Abstract
Aim
Amidst COVID-19 pandemic, the health care delivery in India faces major challenges owing to the overwhelming hospitals, exhausted healthcare workers, and shortage of crucial medical supplies such as ventilators and oxygen. The study aims to propose a novel successful interventional home care model, the Virtual COVID In-Patient (VCIP) care for effective COVID management.
Methods
The Covid-19 positive patients enrolled in VCIP were chosen for the study. A 24/7 active multidisciplinary WhatsApp group was created for each patient, for remote monitoring of temperature, blood pressure, blood glucose, respiratory and pulse rate along with the symptoms. Advice on sleep and exercises were given along with the medication via video-audio consultations. Lab facility was provided at the doorstep. Training on various devices, medications including steroids, delivering subcutaneous injections etc were given via video platforms.
Results
Among the 220 patients who availed the VCIP facility, only two were hospitalized, yielding a 99.5 % success rate in preventing hospitalizations and patients enrolled have been immensely satisfied with their experience.
Conclusions
With similar pandemics anticipated in near future, VCIP model may be considered for successful domiciliary treatment and overcoming the challenges.
Keywords: Virtual covid IP, Injections, Home care, Steroids, Diabetes, COVID-19
1. Introduction
As of June 16, 2021, there have been 175, 987, 176 confirmed cases of SARS-CoV-2 viral infection (COVID-19) globally, resulting in 3,811,561 deaths. 3, 77,031 of these deaths have occurred in India. The health authorities in India have become desperate as hospitals are overwhelmed, healthcare workers have become exhausted, and the shortage of crucial supplies such as ventilators and oxygen have posed extraordinary challenges in the delivery of healthcare [[1], [2], [3]]. Here, we describe a program that we have developed termed as the Virtual COVID Inpatient (VCIP) care. We have found this program a successful one and hence we are sharing with others on an urgent basis.
VCIP may be a valuable model for other providers to deliver inpatient-level care in the patient's home virtually both during the COVID-19 pandemic and in future epidemics of highly transmissible diseases.
Telemedicine is defined as the use of telecommunication equipment for the provision of healthcare including telephone and video communication equipment and is fundamental to the VCIP program [[4], [5], [6]], Given the high risk of transmission, telemedicine can be favourable in minimizing the need for direct contact with the patients especially during national lockdown during Covid-19 pandemic [7,8]. Virtual consultations and telemedicine can overcome physical barriers in providing access to high-quality healthcare [[9], [10], [11]].
The Diabetes Tele Management System (DTMS®) is a telemedicine-based outpatient follow-up program for the comprehensive management of diabetes that has been a crucial part of diabetes care at Jothydev's Diabetes Research Centre since 1997 [12]. The program has five major components: a customized electronic medical record (EMR) software with different user interfaces; a decision support system provided by the multidisciplinary team of doctors, nurses, dietitians, diabetes educators and psychologists; telecommunication with patients using telephone, e-mail, and internet communication using a secure website; telemedicine-enabled diabetes empowerment, education, and troubleshooting customized to the patient's individual needs; and a program to ensure adherence to complex regimens by linking the program directly to the pharmacy [12]. The experience gained and the proven benefits from DTMS® over the past 24 years inspired the team at Jothydev's Diabetes Research Centre to take VCIP care from a concept to reality [[13], [14], [15]].
It is well-documented that diabetes is one of the key risk factors for poor out comes in COVID-19, regardless of the age and type [[16], [17], [18], [19], [20]]. New onset hyperglycemia and steroid induced hyperglycemia are also recognised as potential factors contributing to severity of COVID [[21], [22], [23], [24], [25], [26], [27], [28], [29]]. We were inspired to develop a novel, systematic, patient-centered approach for the successful treatment of COVID-19 at home in patients with diabetes.
Since September 2020, Jothydev's Diabetes Research Centre (Kerala, India) has been practising the concept of VCIP, wherein the consenting patient will remain in their home and consult the physician and his or her team via audio-video consultations to treat COVID-19 in a manner similar to inpatient care. While the widely prevalent home-based care that is currently available is often limited to monitoring of vital signs, the VCIP program described here involves active therapeutic intervention.
In this article, we detail the concept behind VCIP, a targeted virtual in-patient approach for providing effective treatment and delivering expert health care to improve the access to health care during this pandemic.
2. Materials and methods
2.1. Workflow of VCIP
2.1.1. Initial step towards VCIP
Initial process of VCIP started from March to June 2020 with the conduction of weekly webinars for large groups of patients at a time (n = 500–1000). The webinars focused on teaching patients with diabetes the precautions to be taken to prevent COVID-19 and the importance of aggressively controlling diabetes. Most of the patients who enrolled in our telemedicine program and familiar with using telemedicine were encouraged to enroll in the VCIP program if diagnosed with COVID-19. As the pandemic progressed, a core follow-up team was created including doctors, nurses, diabetes educators and dietitian and was trained in COVID-19 care to prepare for virtual consultation and follow-up. Frequent meetings were organised for the team to create awareness on the COVID-19 care updates.
2.1.2. Initiation of VCIP
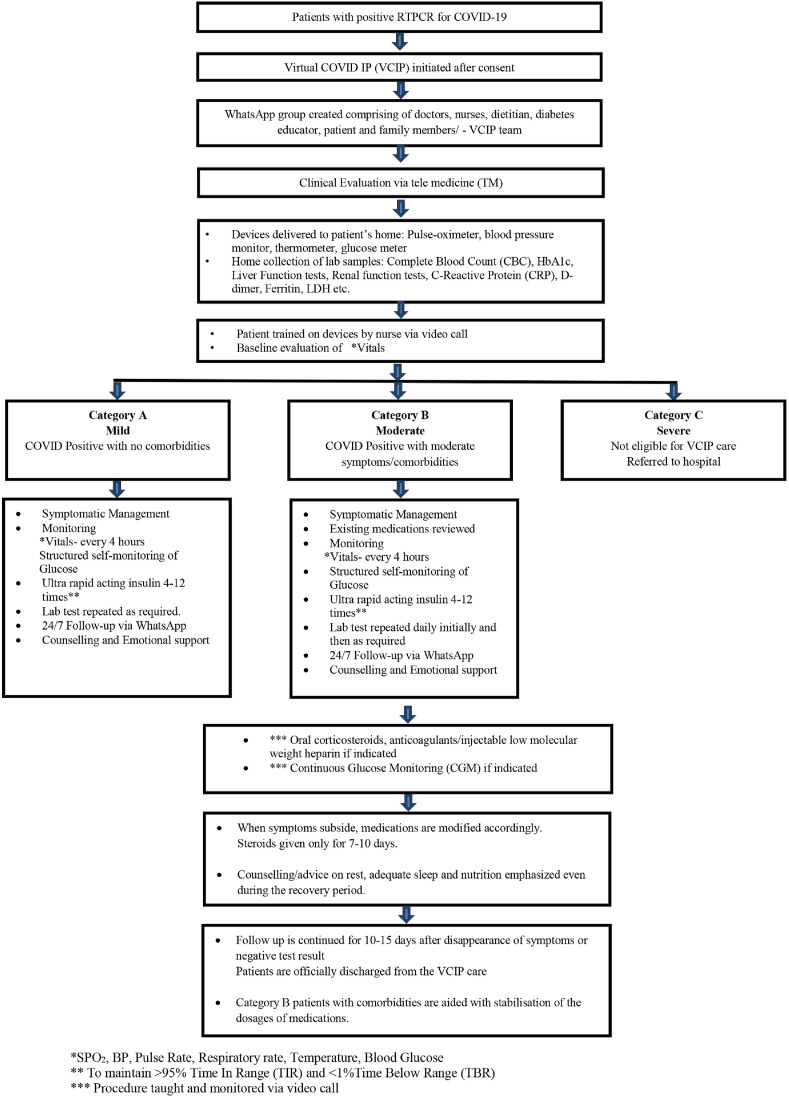
Patients tested positive for COVID-19 interested in enrolling with VCIP were briefed on the VCIP protocol by the HCP team. The patients were enrolled and managed under VCIP only if they contacted us fairly early, preferably within the first day of onset of symptoms and late within 3 days. After obtaining consent from the patient, a dedicated WhatsApp group was initiated (Fig. 1 ) and set as the primary platform because most patients were familiar with its use and no additional training is required. WhatsApp group comprised of the HCP team (5 doctors, 5 nurses, a dietitian, a diabetes educator and a psychologist) along with the patient and his or her family members. For each patient, there was a primary physician and a nurse in charge from the day of admission to discharge. The duty was rotated among different physicians, nurses and other healthcare professionals. During the initial consultation, the physician along with the nurse performed an all-inclusive clinical evaluation including a detailed history and risk assessment via telemedicine, gathering the details on clinical symptoms, time of onset of symptoms, existing comorbidities and details of medications and all other supporting parameters that form the rationale indicators of the triage (Category A, B or C).
Fig. 1.
Workflow of VCIP.
The devices necessary for home monitoring, including pulse-oximeter, blood pressure monitor, thermometer, and glucometer, were delivered directly to the homes of the patients who were under home quarantine for those not having it. Virtual training for the patients and their families on the use of these devices to self-monitor vital signs was provided by a nurse either via WhatsApp or Zoom, as per the patient's choice. Medications were also delivered as per the requirement. Laboratory sample collection was arranged daily or every other day depending on the severity of illness. Home lab tests were performed by local accredited laboratories equipped with standardized equipment and machines and widened with chains all over the country which ensures accuracy in results. Five to six reliable laboratories, well facilitated with all protective gears used to visit the houses for phlebotomy. RT-PCR or antigen test were also managed at home in a similar way.
The potential therapies that might be needed throughout the illness, such as insulin, steroids, and low-molecular weight heparin, were reviewed with the patients and their caregivers at the beginning of their illness. Continuous glucose monitoring (CGM) was also reviewed. The goal was to familiarize families with these therapies early, at a time when the patient was relatively stable, so that the anxiety associated with worsening the severity of the disease would not impair the learning process at the time when they became necessary.
Some patients enrolled in the program were living remotely at the time they contracted COVID-19. In addition to monitoring the basic vital signs, the patient's general wellbeing and overall health status was evaluated. Advice on sleep and exercise was also given. Many patients suffered from significant stress and exacerbation of underlying anxiety and depression due to the fear of dying, restriction in movement due to quarantine, and copious sources of incorrect and misleading information about COVID-19, treatment, and outcomes. Psychotherapeutic counselling was additionally given via audio/video consultation for emotional support and to treat the anxiety and stress.
2.1.3. Virtual IP treatment
The baseline evaluation of vital sign parameters (SpO2, blood pressure, respiratory rate, temperature, and blood glucose) and biochemical parameters (Urine and Blood analysis- Complete Blood Count (CBC), HbA1c, Liver Function tests, Renal function tests, C-Reactive Protein (CRP), D-dimer, Ferritin, LDH) were reviewed by the VCIP team.
The patients were then categorized based on the severity and lab test results as given below:
-
●
Category A - Mild- SARS-CoV-2 positive with mild symptoms (Low-grade fever, mild sore throat, cough, rhinitis, diarrhoea) and no comorbidities.
-
●
Category B - Moderate- SARS-CoV-2 positive with moderate symptoms (High-grade fever, severe sore throat, and cough), comorbidities, or age >60 or pregnant women, or serial elevation of inflammatory markers; Respiratory rate ≥24 breaths per minute, and SpO2 <94 % at room air.
-
●
Category C – Severe-SARS-CoV-2 positive with comorbidities and low saturation (SPO2<90 %) or Respiratory rate >30 breaths/min.
Patients in Category C were not eligible for VCIP treatment and were immediately hospitalized.
The patients were closely monitored for symptoms along with vital status measurements like pulse rate, respiratory rate (more than 30 indicate severe illness), blood pressure and oxygen saturation to assess the severity of the illness and plan treatment accordingly.
Tests like blood sugar, renal function test, and liver function tests were included to identify and assess the severity of comorbidities. In addition to the basic blood investigations inflammatory markers like CRP, serum ferritin, LDH, D-dimer were examined to identify the risk of progression of the disease quite reasonably. The blood report was interpreted with the day of onset of symptoms to gather optimal information.
In patients with any clinical features suggestive of onset of pulmonary phase like a return of fever after day 5, the persistence of high temperature beyond 5–7 days, cough with shortness of breath, drop in saturation after 6 min walk, chest pain etc even minor alterations in blood parameters like progressive rise in CRP, ferritin, LDH or rise in NLR, D-Dimer above 500 ng/ml etc dexamethasone was started even if saturation was above 94 % at room temperature with close monitoring of blood sugars. Enoxaparin subcutaneous injections were started at home after ruling out contraindications in all patients with D-Dimer above 1000 and even in some patients with D-Dimer above 500 ng/ml based on clinical judgement.
The decision to start corticosteroids, enoxaparin or oral rivoroxaban was made depending on the lab parameters and self-reported vital parameters. It was ensured that corticosteroids and anti-coagulants were initiated at the right time: never too early or too late. Probably only four medications such as paracetamol, H2 blocker, anticoagulant and corticosteroids are required to treat the symptoms and prevent COVID from developing into a moderate or severe form. The most important parameter is to address comorbidities including diabetes, hypertension, coronary artery disease etc, which need to be aggressively managed in the absence of which the patients will succumb to COVID 19.
VCIP intended to address the second phase early and avoid saturation drop requiring hospitalization and oxygen therapy or thrombotic complications. rt or isCGM or structured SMBG was used in patients in whom steroids were started and used short-acting insulin such as Ultra rapid acting aspart (Fiasp) to keep blood glucose under 150–180 mg (customised) round the clock. Secondary infections were monitored with observing symptoms and by using investigation like procalcitonin in indicated cases. Blood parameters were sequentially checked to assess progression. ECG at home, CPK MB and TROP T was performed in patients with alterations in pulse rate or suspected cardiac involvement. In affordable patients, we used an Apple watch to monitor rhythm. Chest X-ray were not done in the majority of patients undergoing treatment at home.
2.1.4. Management of category A patients
COVID positive patients with no or mild symptoms including low-grade fever, mild sore throat, cough, rhinitis, diarrhoea and with no comorbidities were categorized as Category A. Patients were managed by symptomatic treatment with antipyretic (paracetamol) for fever and pain, adequate nutrition along with vitamin D, C and zinc supplements and appropriate hydration. Remote monitoring of BP, pulse rate and SpO2 every 4 h, temperature every 6 h and blood glucose were advised in real-time with the HCP team in the WhatsApp group via audio-video call or text message. A doctor and nurse in the team were assigned 24/7 duty to ensure continuing care. Laboratory tests were performed daily or less frequently as warranted.
2.1.5. Management of category B patients
COVID positive patients with more severe symptoms, comorbidities such as obesity, diabetes or hypertension, age >60 years, and pregnant women were categorized as Category B. All home medications taken by the patient were reviewed by the physician and the doses were modified if needed during the first virtual consultation. Preliminary management was similar to Category A patients with symptomatic treatment with antipyretic, Vitamin D, Vitamin C, zinc supplements and appropriate nutrition and hydration as required. Patients who developed abdominal discomfort as suspected could be due to Vitamin C/zinc which were relieved with withdrawal of these medications but continued Vitamin D. With the amendment in the guidelines, we have discontinued the use of regular vitamin C and zinc in the protocol. Vital parameters including BP, pulse rate, SpO2 every 4 h, respiratory rate, temperature every 6 h and blood glucose (Fasting, pre- and post-meal for patients with diabetes or structured self-monitoring of blood glucose (SMBG) as indicated) are closely monitored, given the possible risk of progressing to a more severe form of the disease. For patients with diabetes on insulin, dosages were titrated based on SMBG values or RT-CGM/isCGM. Laboratory tests were collected as described above.
2.1.6. Management of category C patients
COVID patients in severe condition with comorbidities and low oxygen saturation (SPO2<90 %) or respiratory rate >30breaths/min were categorized as Category C. Category C patients were immediately directed to a nearby hospital with oxygen and ICU availability.
2.2. Subsequent management of COVID
The patients were closely monitored for signs or symptoms of disease progression. If the oxygen saturation was downtrending or inflammatory markers were rising, steroids (Dexamethasone 4mg/6 mg (once daily), 0.15 mg/kg/dose PO every 24 h for 10 days; max: 6 mg daily was initiated and dosages of which were modified if required. Home therapy with corticosteroids was limited to 7–10 days duration. In certain high-risk individuals with laboratory parameters concerning for thrombosis, low molecular weight heparin therapy was initiated. Instruction on its administration was reviewed by the trained nurses in the team via video at the time of initiation.
For patients with diabetes started on steroids, more frequent monitoring blood glucose was advised. CGM was the preferred modality to examine trends of glucose levels in order to make informed quick treatment decisions and to avoid hypoglycemia. In these situations, a ready to use continuous glucose sensor was delivered at home of patients and the training on placement and operation of the CGM sensor was given via video consultation.
Ultra-fast acting analog insulin such as Faster-acting insulin Aspart (Fiasp) was given for pre-meal and multiple correction boluses. The newer analogues were faster in onset and with shorter duration of action making this the insulin of choice in special circumstances where the patients themselves are managing insulin administration. Given the flexibility, it can be taken immediately before a meal or even up to 20 min after starting a meal if necessary. Maximizing time-in-target-range for patients with diabetes on high dose dexamethasone therapy decreases likelihood of further steroid-related complications such as secondary infections or mucormycosis.
On day 7–10, RT-PCR/Rapid Antigen Test (RAT) was repeated. If the result was negative, the patient is advised to continue rest, be on constant follow up via WhatsApp and be in quarantine for an additional 7 days. If positive or symptoms persist, the VCIP management continues until all symptoms subside or the labs return to normal.
3. Results
3.1. Patient outcomes
Our experience with 220 patients showed successful prevention of hospitalization for nearly all patients. The treatment was initiated only for our already registered patients with diabetes, but with variants too emerging, almost all the family members were affected and hence ended up managing the entire family as well, many of them without diabetes. The baseline values for CRP, Ferritin, D-dimer and LDH were found to be normal for most of the patients. For those patients with serial elevation of one or more of these parameters, home interventions were advised but not hospitalized. Patients with as high as 100.4 mg/L for CRP, 1338 ng/ml for Ferritin, 381 U/L for LDH, 1750 ng/mL for D-dimer are managed at home with interventions but not requiring oxygen, continued in VCIP. With the continuous management of COVID-19 via VCIP, the values were brought back to acceptable levels in most patients within a week or two. The use of CGM for 14 days at home care setting successfully maintained 90–95 % Time-in-Range and less than 1 % Time-below-range in all patients. Patients were monitored for 10–15 days after the disappearance of symptoms or a negative COVID test to evaluate for persistent symptoms or complications. Home medication doses were adjusted to achieve adequate control of comorbidities after COVID symptoms had resolved (Table 1 ). There were a wide range of post-COVID-19 symptoms and illnesses experienced by our patients such as severe headache, generalized itching, fatigue, urticaria, exacerbation of sinusitis, and insomnia were common post COVID. Some patients who experienced more severe complications such as atrial fibrillation and ventricular ectopics picked up in Apple watch ECG were referred to Cardiologist for evaluation. The arrythmias disappeared spontaneously with clinical improvement in majority of the patients.
Table 1.
Baseline characteristics of patients, presence of comorbidities and progression of disease and medications.
| Total no. of patients | 220 |
|---|---|
| Sex | |
| Female | 132 |
| Male | 88 |
| Average Age | 48 |
| A Category | 66 |
| B Category | 154 |
| C Category | 0 |
| No. of patients hospitalized after enrolled in VCIP | 2 |
| Presence of Comorbidities | 154 |
| Diabetes | 107 |
| Prediabetes | 15 |
| HTN | 30 |
| Dyslipidemia | 109 |
| Asthma | 2 |
| Chronic Liver Disease | 1 |
| Progression of disease and medications | |
| Patients progressed from A to B | 0 |
| Patients progressed from B to C | 1 |
| No. of patients on steroids in Category A (4 mg OD 7 days) | 1 |
| No. of patients on LMWH in Category A (0.4 ml OD Sc 7 days) | 9 |
| No. of patients on steroids in Category B (4 mg BD for 7 days) | 6 |
| No. of patients on steroids in Category B (4 mg BD for 7 days) | 57 |
| No. of patients on LMWH in Category B (0.4 ml OD for 7 days) | 92 |
There were only 2 instances of hospitalization for patients enrolled in the VCIP. The first one, due to the impending fear of death. Despite having all the lab parameters normal, the patient went for a chest X-ray in a hospital nearby. Notwithstanding the normal x-ray and lab parameters, the patient got admitted there. The second one, due to intolerance to oral corticosteroids. This patient had ulcerative colitis along with peptic ulcer and could not tolerate oral steroids. With the subsequent deterioration of symptoms and lab values, the patient was immediately referred to the hospital for intravenous steroid administration. We acknowledge here that patients who cannot tolerate oral steroids is a contraindication to be managed in VCIP.
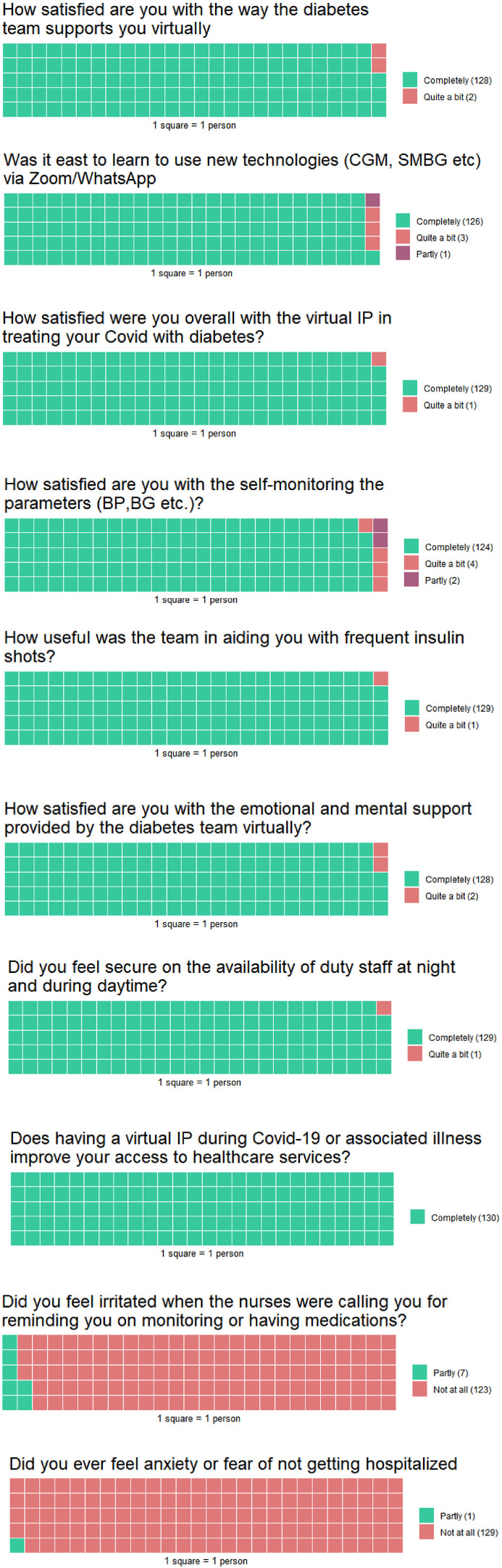
The VCIP team emphasized the importance of adequate sleep, nutrition and rest throughout the illness and recovery period, which is easier to achieve at home than in the hospital setting. VCIP program was designed with the assumption that COVID-19 is a treatable illness that can be managed symptomatically in some patients or with the addition of corticosteroids and anticoagulants at the right time when indicated. We have gathered evidence over the past several months that appropriate home treatment with these medications, and symptomatic management with paracetamol, antihistamine, and betadine gargles, can help patients avoid the need for inpatient care provided the co-morbidities are intensively managed. None of the patients were treated with antiviral medications. The patients expressed a high level of satisfaction (Fig. 2 ). The difference between VCIP and conventional domestic care and VCIP and hospital care is also mentioned (Table 2 , Table 3 ). The preliminary results were published at the ATTD [30].
Fig. 2.
Waffle Chart shows response to VCIP performance assessment questionnaire.
Table 2.
Difference between VCIP and conventional domestic care.
| Virtual COVID IP | Conventional Domestic Care |
|---|---|
| Monitor all the five vital parameters (SpO2, Blood pressure, respiratory rate, temperature and blood glucose) | Usually, temperature and blood oxygen levels are monitored. |
| Medicines given: Paracetamol, Vitamins, Corticosteroids and LMWH (at the right time for right duration) | Medicines given: Paracetamol and Vitamins |
| Treatment is started at home itself before clinical deterioration | Patients hospitalized only when there is an onset of symptoms like breathlessness, low blood oxygen level when already it could be late |
| Patients are empowered for SMBG and very frequent injections of rapid acting analog insulin to keep time in target above 90 % | Only infrequent SMBG is being advised. |
| In eligible patients advanced devices such as Continuous Glucose Monitoring Guardian Connect, Apple watch ECG etc are being utilized | Not applicable |
| Group of 5 nurses and 5 doctors taking care of around 20 patients at a time | A systematic or structured approach is not being practiced |
| Investigation of parameters are executed at home itself at required frequency | No lab investigations performed for patients diagnosed with COVID 19 |
| Patients are frequently monitored for symptoms and changes in parameters by healthcare professional | Attention is paid only when symptoms severity is progressing |
| Effective intervention starts at the earliest | The effective intervention starts at a later stage |
| Cost effective intervention to prevent development of complications | Costly compared to VCIP |
Table 3.
Difference between VCIP and hospital care.
| Parameter | VCIP | Hospital Care |
|---|---|---|
| Mental Status | More relaxed in the home environment | Significantly more anxious, distressed |
| Disease transmission | Absolutely no chance of disease transmission to HCP | Obviously more chance of transmission |
| Nosocomial infections | Not applicable | Chances are more in the hospital environment |
| Comorbid illnesses | More frequent monitoring of blood pressure, blood sugar and other vitals possible in the home environment | Speciality care possible in the hospital but with restrictions imposed by COVID protocol |
| Infrastructure | Not applicable in the home environment | Use of PPE Kit, room sanitization etc. |
| Efficacy of communication | More effective via the video without PPE Kit and mask | Less effective when dressed in PPE kits. |
| Addressing anxiety and stress | Involving a multidisciplinary team including a psychologist Easy and effective via telemedicine video consultations |
Isolation in hospital environment further increases anxiety. |
| Diabetes Management | More frequent injections of Rapid acting insulin and significantly more chances of patients reaching glucose targets | Less likely chances of more frequent injections due to the restrictions imposed by the pandemic and the overwhelmed hospital staff |
| Overall Cost | Lower compared to hospitalization | 20 times more costly |
4. Discussion
VCIP has allowed for the provision of inpatient-level care in the patient's home during the pandemic. With social distancing and quarantine orders in place, and hospitals being overwhelmed with patients, this allows a subset of patients with mild-to-moderate disease to be managed at home and reduce the spread of the virus. With appropriate staffing, this is a replicable model in which steroids can be initiated at an appropriate time to prevent progression of moderate COVID-19 to severe disease.
The set goals of VCIP such as to avoid hospitalization, reduce cost, intervene with medications before hypoxia develops to prevent oxygen supplementation, ventilator, and to train team members to have the expertise to manage comorbidities or symptoms of COVID-19 infection such as uncontrolled hyper- or hypoglycemia, hypertension, tachycardia, insomnia, and anxiety and to feel comfortable managing the patients’ ongoing questions and concerns were accomplished. Among the 220 patients who availed the VCIP facility, only one was hospitalized, yielding a 99.5 % success rate in preventing hospitalization. Indeed, the patient who was hospitalized likely could have continued to be managed at home from a medical perspective.
4.1. Merits of VCIP
-
1.
A hospitalization for 10–14 days is 20 times as expensive as VCIP management for the same period. Treating patients in their homes at minimal costs decreases the burden on local hospitals and keeps beds available for sicker patients.
-
2.
Virtual consultations do not require personal protective equipment (PPE), including masks, which helps to preserve PPE for healthcare providers who need it.
-
3.
Personalized individualized care is possible as the patients are followed by the same team throughout their illness.
-
4.
Treatment in their own homes can reduce anxiety and stress in patients, and psychotherapeutic counselling is included as part of the program.
-
5.
Intensive diabetes monitoring with frequent correctional boluses of insulin are easier to achieve outside the hospital setting, where there are resource limitations due to the pandemic.
-
6.
DKA, CAM, secondary bacterial infections, nosocomial infections etc. are almost completely preventable in this model involving COVID HCP team and the empowered patients.
4.2. Challenges of VCIP
Though VCIP successfully managed the mild and moderate COVID-19 cases that presented, there were some unanticipated challenges seen.
-
1.
The frequent monitoring required was sometimes overwhelming to families, especially if the entire household had fallen ill, and there was a large burden of reminder calls that fell to the VCIP team. At times, patients/relatives were unable to be contacted.
-
2.
Patients must have a very high level of confidence in the medical team and cooperation with medical advice is essential.
-
3.
If there is a surge in the number of cases, there may not be adequate medical staff to perform home phlebotomy visits.
-
4.
Corticosteroids and anticoagulant injections were given at home which otherwise is carried out only in a hospital setting. A well trained HCP team is a prerequisite to ensure error free execution.
-
5.
Patients must be literate in order to self-monitor and follow instructions texted by the medical team.
-
6.
Patients must have uninterrupted internet connectivity.
-
7.
Around-the-clock staffing of the line by a trained physician and nurse is required, mimicking the hospital environment, which may be difficult to achieve in the outpatient setting.
-
8.
There is an inherent security risk to consultation via virtual platforms given that sensitive medical information is being collected.
-
9.
Though the patients are officially discharged in two weeks, most of them continued contacting us for post COVID symptoms such as cough, breathlessness, tiredness, giddiness etc. which we managed to give advice for another 2–3 weeks.
4.3. Future area of research
-
1.
Studies should be conducted to determine the optimal doctor-patient and nurse-patient ratios for such a program so that providers do not become overwhelmed.
-
2.
The training regimen for healthcare providers must be optimized for a larger number of healthcare providers on use of the technology and appropriate code of conduct in these unusual circumstances.
-
3.
Evaluate the efficacy of this monitoring program in identifying patients at risk of progressing to severe disease. In the 220 patients who have been studied thus far, none progressed to the hypoxemia or respiratory distress, and so this algorithm must be studied in a larger population.
5. Conclusion
Covid Virtual IP demonstrated 99.5 % success in preventing hospitalizations and patients enrolled have been immensely satisfied with their experience. In contrast to conventional home-based care, this program includes a well-structured protocol for empowering patients to self-monitor. High-level interventions can be delivered that are otherwise only being carried out in the hospitalized setting. As we expect that COVID-19 will continue to cause havoc in the coming years, and with the anticipation of similar pandemics in the near future, this model needs to be considered for delivery on a larger scale. This could prevent hospitals from being overwhelmed by patients with mild to moderate illness and could save millions of lives. We have shown that inpatient-level care can be delivered virtually in a convenient, safe, and effective way to deliver quality targeted disease management and can improve access to a subset of the population. The limitations of this model, especially that it requires a motivated, educated patient population with reliable internet access, do limit its replicability in some settings.
Acknowledgements
We acknowledge our patients with diabetes and their relatives with or without diabetes who had complete confidence in us for accepting the treatment via telemedicine. We also sincerely thank Ms. Jayasree Ajith and the entire hospital staff for their tireless efforts during the ongoing pandemic.
References
- 1.Pal R., Yadav U. COVID-19 pandemic in India: present scenario and a steep climb ahead. J Prim Care Community Health. 2020;11 doi: 10.1177/2150132720939402. 2150132720939402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu Q., Luo D., Haase J.E., Guo Q., Wang X.Q., Liu S. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health. 2020;8(6):e790–e798. doi: 10.1016/S2214-109X(20)30204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mareiniss D.P. The impending storm: COVID-19, pandemics and our overwhelmed emergency departments. Am J Emerg Med. 2020;38(6):1293–1294. doi: 10.1016/j.ajem.2020.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dasgupta A., Deb S. Telemedicine: a new horizon in public health in India. Indian J Community Med. 2008;33(1):3–8. doi: 10.4103/0970-0218.39234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kirsh S., Su G.L., Sales A., Jain R. Access to outpatient specialty care: solutions from an integrated health care system. Am J Med Qual. 2015;30(1):88–90. doi: 10.1177/1062860614542844. [DOI] [PubMed] [Google Scholar]
- 6.Serper M., Volk M.L. Current and future applications of telemedicine to optimize the delivery of care in chronic liver disease. Clin Gastroenterol Hepatol. 2018;16(2):157–161. doi: 10.1016/j.cgh.2017.10.004. e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shokri T., Lighthall J.G. Telemedicine in the era of the COVID-19 pandemic: implications in facial plastic surgery. Facial Plast Surg Aesthet Med. 2020;22(3):155–156. doi: 10.1089/fpsam.2020.0163. [DOI] [PubMed] [Google Scholar]
- 8.Ghosh A., Gupta R., Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: guidelines for physicians. Diabetes Metab Syndr. 2020;14(4):273–276. doi: 10.1016/j.dsx.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gajarawala S.N., Pelkowski J.N. Telehealth benefits and barriers. J Nurse Pract. 2021;17(2):218–221. doi: 10.1016/j.nurpra.2020.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bokolo Anthony J. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7):132. doi: 10.1007/s10916-020-01596-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Misra A. Majorly resurgent and uncontrolled diabetes during COVID19 era, and in the future can Be contained in India. Diabetes Metab Syndr. 2021:102142. doi: 10.1016/j.dsx.2021.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kesavadev J., Saboo B., Shankar A., Krishnan G., Jothydev S. Telemedicine for diabetes care: an Indian perspective - feasibility and efficacy. Indian J Endocrinol Metab. 2015;19(6):764–769. doi: 10.4103/2230-8210.167560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kesavadev J., Shankar A., Pillai P.B.S., Krishnan G., Jothydev S. Cost-effective use of telemedicine and self-monitoring of blood glucose via diabetes Tele management system (DTMS) to achieve target glycosylated hemoglobin values without serious symptomatic hypoglycemia in 1,000 subjects with type 2 diabetes mellitus-A retrospective study. Diabetes Technol Therapeut. 2012;14(9):772–776. doi: 10.1089/dia.2012.0088. [DOI] [PubMed] [Google Scholar]
- 14.Kesavadev J., Shankar A., Ashok A.D., Srinivas S., Ajai N.A., Sanal G. Our first 825 T2DM patients on 14-day factory-calibrated glucose monitoring system: clinical utility and challenges. J Diabetes Sci Technol. 2018;12(1):230–231. doi: 10.1177/1932296817717504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kesavadev J., Vigersky R., Shin J., Pillai P.B.S., Shankar A., Sanal G. Assessing the therapeutic utility of professional continuous glucose monitoring in type 2 diabetes across various therapies: a retrospective evaluation. Adv Ther. 2017;34(8):1918–1927. doi: 10.1007/s12325-017-0576-x. [DOI] [PubMed] [Google Scholar]
- 16.Kar P. Partha Kar: Covid-19—we must keep faith in our experts. Bmj. 2020;368:m1143. doi: 10.1136/bmj.m1143. [DOI] [PubMed] [Google Scholar]
- 17.Corona G., Pizzocaro A., Vena W., Rastrelli G., Semeraro F., Isidori A.M. Diabetes is most important cause for mortality in COVID-19 hospitalized patients: systematic review and meta-analysis. Rev Endocr Metab Disord. 2021;22(2):275–296. doi: 10.1007/s11154-021-09630-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Riddle M.C., Buse J.B., Franks P.W., Knowler W.C., Ratner R.E., Selvin E. COVID-19 in people with diabetes: urgently needed lessons from early reports. Diabetes Care. 2020;43(7):1378–1381. doi: 10.2337/dci20-0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holman N., Knighton P., Kar P., O'Keefe J., Curley M., Weaver A. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020;8(10):823–833. doi: 10.1016/S2213-8587(20)30271-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Woolcott O.O., Castilla-Bancayán J.P. The effect of age on the association between diabetes and mortality in adult patients with COVID-19 in Mexico. Sci Rep. 2021;11(1):8386. doi: 10.1038/s41598-021-88014-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gianchandani R., Esfandiari N.H., Ang L., Iyengar J., Knotts S., Choksi P. Managing hyperglycemia in the COVID-19 inflammatory storm. Diabetes. 2020;69(10):2048–2053. doi: 10.2337/dbi20-0022. [DOI] [PubMed] [Google Scholar]
- 22.Yang J.-K., Jin J.-M., Liu S., Bai P., He W., Wu F. New onset COVID-19–related diabetes: an indicator of mortality. medRxiv. 2020 doi: 10.1101/2020.04.08.20058040. [DOI] [Google Scholar]
- 23.Lim S., Bae J.H., Kwon H.-S., Nauck M.A. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021;17(1):11–30. doi: 10.1038/s41574-020-00435-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bode B., Garrett V., Messler J., McFarland R., Crowe J., Booth R. Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States. J Diabetes Sci Technol. 2020;14(4):813–821. doi: 10.1177/1932296820924469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sardu C., D'Onofrio N., Balestrieri M.L., Barbieri M., Rizzo M.R., Messina V. Hyperglycaemia on admission to hospital and COVID-19. Diabetologia. 2020;63(11):2486–2487. doi: 10.1007/s00125-020-05216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chee Y.J., Ng S.J.H., Yeoh E. Diabetic ketoacidosis precipitated by Covid-19 in a patient with newly diagnosed diabetes mellitus. Diabetes Res Clin Pract. 2020;164:108166. doi: 10.1016/j.diabres.2020.108166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singh A.K., Singh R. Hyperglycemia without diabetes and new-onset diabetes are both associated with poorer outcomes in COVID-19. Diabetes Res Clin Pract. 2020;167:108382. doi: 10.1016/j.diabres.2020.108382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta Y., Goyal A., Kubihal S., Golla K.K., Tandon N. A guidance on diagnosis and management of hyperglycemia at COVID care facilities in India. Diabetes Metab Syndr. 2021;15(1):407–413. doi: 10.1016/j.dsx.2021.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Raju R., V P., Biatris P.S. J SJUC. Therapeutic role of corticosteroids in COVID-19: a systematic review of registered clinical trials. Futur J Pharm Sci. 2021;7(1):67. doi: 10.1186/s43094-021-00217-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kesavadev J., Shankar A., Unes Y., Shijin S., Manoj A., Rajalakshmi S. ATTD 2021 invited speaker abstracts. Diabetes Technol Therapeut. 2021;23(S2) doi: 10.1089/dia.2021.2525.abstracts. A-1-A-206. [DOI] [PubMed] [Google Scholar]