Abstract
The development of COVID-19 vaccines is occurring at unprecedented speeds, but require high coverage rates to be successful. This research examines individuals’ psychological beliefs that may act as enablers and barriers to vaccination intentions. Using the health beliefs model as a guide to our conceptual framework, we explore factors influencing vaccine hesitancy and health beliefs regarding risks and severity of the disease, along with individual variables such as income, age, religion, altruism, and collectivism. A questionnaire using newly created measures for various antecedents provided 4303 usable responses from Australia, Canada, England, New Zealand, and the United States. A factor analytic and structural equation model indicates that trust in vaccine approval, the perceived effectiveness of the vaccine for protecting others, and conspiracy beliefs are the most significant drivers of intentions to vaccinate. Older people, those seeking employment, and those who have received a recent influenza vaccine are more likely to be vaccinated against COVID-19. The findings have implications for improving communication strategies targeting individuals about the merits of vaccination, particularly focusing on younger individuals and expanded message framing to include altruistic considerations, and to improve government transparency regarding the effectiveness and side effects of vaccines.
Keywords: COVID-19, Vaccination hesitancy, Health beliefs model, Conspiracy beliefs, Immunization, Structural equation model
1. Introduction
COVID-19 vaccines are being developed at unprecedented speeds, with novel partnerships between private, public, philanthropic, and civil society organizations [1]. High vaccine uptake rates are required for COVID-19 vaccination programs to be successful and achieve herd immunity objectives. [2] Vaccine hesitancy, defined as a “delay in acceptance or refusal of vaccines despite availability of vaccination services” [3] represents a significant barrier to the success of any vaccination program. Several factors contributing to vaccine hesitancy have been identified, with the majority of concerns relating to fear of side effects, distrust in the vaccine, vaccine related risks and the perceived effectiveness of the vaccine. These concerns can be influenced and amplified through anti-vaccination reporting [4]. Various theories are provided in the literature to explain how individuals decide to engage in a health action after assessing the threat posed by the disease itself alongside vaccine related concerns, for example the Health Beliefs Model (HBM) [5], [6]. However, vaccine hesitancy and acceptance of vaccines as a health behaviour vary over time, place, and even individual vaccines [2], [7]. This warrants a separate empirical investigation of barriers to COVID-19 vaccination uptake rather than drawing on generalizations from other vaccine contexts [4], [8]. The objective of the current research is to identify and quantify the effect of various enablers and barriers to higher vaccination uptake from a broad psychological perspective in the context of COVID-19.
2. Psychological enablers and barriers to vaccination uptake
2.1. Vaccine related perceptions
A range of side effects are associated with vaccinations, some based on science, while others are purely speculative, coincidental, or unsubstantiated, all of which can negatively affect immunization coverage [9]. The development and approval of COVID-19 vaccinations has occurred at an unprecedented speed [1], [10] resulting in concerns about unknown vaccine side-effects. Indeed, historical examples exist where adverse reactions were only identified after widespread vaccine use [1]. Distinguishing between adverse outcomes from a disease and those caused by a corresponding vaccine is complicated. This is particularly true in the case of COVID-19 as it remains widely circulating in communities where immunization programs are being deployed [1].
Public confidence in vaccines is positively (negatively) driven by the (mis)trust that individuals hold in public health and government authorities to recommend safe and effective vaccines [2], [11]. Assurances from government and healthcare providers are essential to vaccination uptake [12], [13], [14], particularly where anxiety about the nature of the illness is significant [15]. However, health information is increasingly obtained from other sources, including the Internet and social media, allowing claims of vaccine injury to disseminate more quickly and widely [2], [13], [16]. This also includes information relating to anti-vaccine conspiracy theories, which have been shown to significantly reduce vaccine uptake [17], [18], [19], including in the case of COVID-19 [20].
Barriers relating to the inconvenience of vaccinating (e.g., access, cost, time) have also been shown to negatively impact vaccination uptake [21], [22], [23], [24]. Whilst pharmaceutical companies and governments might improve vaccine convenience, individuals may hold different perceptions about such solutions. For example, Liao et al. [21] showed preferences for vaccination to occur at a mobile station relative to designated clinic locations, and for walk-in based options rather than appointment-based arrangements. Availability has also been considered in terms of cost, but only found to contribute to vaccination delay for a small minority of the population [22]. Conversely, Sun et al. [23] reported preferences for more expensive vaccines among affluent individuals with higher levels of education or income, suggesting that individuals may use price as a signal to the quality of the vaccine offered.
Several studies cite vaccine efficacy as the most important attribute compared to other concerns such as side-effects and price [24], [25]. To be effective, vaccination programs require a majority of individuals to participate. However, some studies have identified “free-riding” individuals who derive benefits from vaccination programs by allowing others to participate and reduce a disease to an acceptable level, thus avoiding their own need to be vaccinated [26]. Whilst Hershey et al. [26] report the existence of free-riding behaviors, the authors also identified individuals motivated by altruistic considerations, whilst others based their decision on matching what the majority of others do (i.e., “bandwagoning”).
2.2. Disease-related perceptions
Consistent with the HBM [5], [6], it is anticipated that individuals will evaluate the threat of COVID-19 with respect to their perceived susceptibility to infection and the perceived severity of the disease against vaccine-related barriers. In terms of threat, COVID-19 spreads primarily from respiratory droplets of infected individuals in enclosed spaces with infection resulting in symptoms that include fever, dry and persistent cough, muscle ache, headache, fatigue, diarrhea, nausea, and loss of appetite [27]. Severe symptoms include hypoxia and respiratory distress, whilst other patients have developed kidney or pancreatic injury, a complete loss of taste or smell, or experienced coagulopathy or thrombotic events [10]. Many virus-positive individuals, however, are asymptomatic or exhibit minor cold like symptoms. Complicating threat perceptions, many believe that COVID-19 is only fatal to those already at risk, particularly the elderly with underlying comorbidities [10]. This is despite people of all ages and healthy individuals having died from the disease or experiencing a reduced quality of life. Such high levels of complacency imply lower levels of engagement in vaccination decisions and likely lower uptake in vaccination behaviour [11].
2.3. Individual differences and control variables
Various control variables are used in the literature to explain vaccination uptake. Vaccination uptake is reported to be significantly higher among older individuals [11], [24], [28], more important among males [28], but with higher vaccination rates among females, as well as those living in urban and high income areas [24]. Vaccination rates have also been found to vary by country, with vaccine hesitancy higher among European countries [28]. Finally, Grabenstein’s [29] review of disease outbreaks among religious communities indicated that most declines in immunization reflected concerns about vaccine safety or personal beliefs, rather than theologically based objections.
3. Theoretical framework
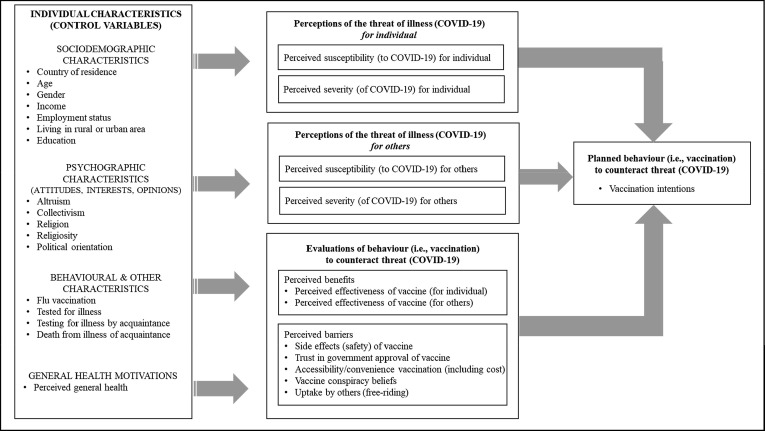
Our conceptual framework of vaccine acceptance and hesitancy has five major elements drawn from the literature (Fig. 1 ) and based on the health beliefs model (HBM). The first element of this framework, the focal dependent variable, is the behavioral intentions among individuals to have a COVID-19 vaccine. Whilst it is consistent with HBM to focus on value expectancy, our focus on behavioral intentions as a dependent variable overlaps with theories of reasoned action and planned behavior (TPB) [30]. Specifically, such intentions are driven by various beliefs about attributes describing benefits and costs associated with the behavior. Studies of intentions and behaviors employing these theories have been undertaken in various health-related domains, including in the context of alcohol consumption [31] and smoking [32], and in studies of vaccination, such as in the contexts of HPV [33] and influenza [34]. In our study, the HBM guides our choice in the inclusion and structure of the key constructs driving such behavioral intentions.
Fig. 1.
Conceptual Framework.
As our first set of independent variables, and consistent with the HBM and vaccine hesitancy, we include beliefs about the benefits and barriers associated with vaccination itself. We consider barriers relating to perceptions around safety, trust in the development and approval of the vaccine, its accessibility and convenience, and conspiracy beliefs regarding the vaccine. In terms of perceived benefits, we include an individuals’ assessment of the perceived effectiveness of the vaccine for themselves. We extend the HBM to include perceptions about perceived vaccine efficacy for others in the community, which are likely to drive vaccination intentions through altruistic motivations and social norms [26]. We also consider how each of these independent variables impacting vaccination intentions are moderated by the country in which an individual resides.
Our second set of independent variables examine beliefs about the threat of disease itself. As per the HBM, this consists of an individual’s perceived susceptibility to contracting a disease and severity of the disease [6]. Once again, we extend the HBM model to include beliefs about disease severity and susceptibility for others in the community. We believe this is an important extension to the HBM model in the context of vaccination, where the goal of ones’ individual vaccination behavior is to provide individual protection, but also others to prevent the spread of the disease. This is likely to be particularly important during a global pandemic in the presence of goals to achieve herd immunity. Again, we investigate whether these effects differ across countries by introducing moderating terms for each.
Finally, we examine the role of various control variables that have been offered as explanatory variables in the HBM and immunization literature, including age, gender, income, education, political, and religious beliefs. We also include reflective measures of a person’s altruistic and collectivist beliefs as additional control variables.
4. Methodology
4.1. Instrument development
The empirical assessment of our framework involved an online questionnaire utilizing a range of reflective measures for each latent construct adapted from previous literature (see Table 1 ). With respect to perceptions of susceptibility to and severity of the disease, items were adapted from existing empirical applications of the HBM [35], [36], [37] and tailored to the COVID-19 context. Some items were further improved with respect to ambiguity, particularly distinguishing the measures to consider whether the perceived threat related to an individual or others in the community. Several items used in previous literature on vaccine related beliefs were adapted for the current context [4], [18], [19], [30], [35], [36], [38], [39], [40], [41]. Again, items were re-written to measure an individual’s perception about COVID-19 vaccination being effective for themselves, but also effective in protecting others. Further, some wording was simplified for a general audience, such as replacing the word “efficacy” with “effectiveness” [40]. With respect to measuring trust, items were adapted from those used in the context of perceived risks relating to electromagnetic fields from mobile phone antennas and adapted to measure the trust placed in government vaccination approval [41]. Each measurement item was presented in a randomized order and evaluated on a seven-point Likert scale ranging from strongly disagree (1) to strongly agree (7).
Table 1.
Cited Sources Used in Construction of Reflective Measures.
| PERCEPTIONS OF THREAT OF ILLNESS (COVID-19) | Items adapted from | Vaccination context | Subjects |
|---|---|---|---|
| Perceived Disease Severity (for individual) |
|
|
|
|
|
|
|
|
|
|
|
| Perceived Disease Severity (for others) |
|
|
|
|
|
|
|
| Perceived Susceptibility to COVID-19 (for individual) |
|
|
|
| Perceived Susceptibility to COVID-19 (for others) | new items | ||
| EVALUATIONS OF BEHAVIOR (VACCINATION) TO COUNTERACT THREAT OF ILLNESS (COVID-19) | Items adapted from | Vaccination context | Subjects |
| Conspiracy Beliefs about Vaccination |
|
|
|
|
|
|
|
| Perceived C-19 Vaccine Availability |
|
|
|
|
|
|
|
|
|
|
|
| Perceived side-effects of C-19 Vaccine |
|
|
|
| Trust in government approval of C-19 vaccine |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Perceived Ability to Free-Ride | new items | ||
| Perceived Effectiveness of COVID-19 Vaccination (for individual) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Perceived Effectiveness of C-19 Vaccination (for others) |
|
|
|
|
|
|
|
* Tested in non vaccine context of mobile phone antennas.
5. Results
5.1. Sample
Respondents were recruited via an international online panel company (Quality Online Research, QoR) that emailed invitations to two proprietary consumer panel members (QoR in Australia; Cint’s in other countries). Panel members are recruited online and offline to match the population in each country.2 Qualified respondents were adults, living in one of five countries: Australia (39%), the United States (21%), Canada (16%), England (12%) or New Zealand (11%). The chosen countries were selected for benchmarking purposes because they had a strong cultural resemblance (including language spoken) to the country that the study originated (Australia), but had different experiences of the spread of COVID-19. This explains why the majority of respondents were Australian. Quotas were also applied within each country to reflect age, gender, and geographic distributions. Stratified sampling was also employed to ensure a minimal number of respondents came from rural regions in each geographic district, thereby requiring more respondents of all ages and genders from rural areas – and therefore larger samples overall – from persons living in the United States and Canada. A breakdown of these quotas and country-level population census figures used to construct them are available from the authors upon request.
Following data cleaning, removing those who had zero variation in their responses or completed the study in less than five minutes, a total of 4303 useable responses were included for analysis. A description of the sample is presented in Table 2 . For each country sample, the distribution of gender and income match those of the population, with the exception of New Zealand and United States where the sample median income bracket was marginally lower than both corresponding population figures. The summary statistics show a higher median adult age for the Australian sample (59.5 years) compared to both the Australian adult population (44.5 years) and the other countries sampled (45.8 years). However, both age and country-of-origin were included as control variables in the empirical model to account for such differences. Similarly, reported differences in income were accounted for by introducing income standardized with respect to the country-level median income. In surveying a higher number of older respondents, the Australian sample had a higher proportion of couples with no children (42%) and a higher proportion of retirees (33%). In contrast, full-time employment rates were higher in the English (46%) and Canadian (48%) samples. The majority of respondents resided in metropolitan areas (42%), with the exception of the US sample, which had a higher proportion of respondents living in a rural area (44%). Religiosity was significantly higher in the United States sample, but lower among English respondents. More than half of the New Zealand sample did not identify with any religion (52%). Those living in the US were also more likely to identify as right wing, whilst Canadians and New Zealanders were, on average, more politically neutral.
Table 2.
Summary statistics of sample by country of origin.
| Control variable | Overall n = 4303 |
AUS (n = 1678) |
NZ (n = 471) |
US (n = 919) |
ENG (n = 540) |
CAN (n = 695) |
|---|---|---|---|---|---|---|
| Country of residence (%) | 100% | 39.0 | 10.9 | 21.4 | 12.5 | 16.2 |
| Female (%)^ | 50.7 | 50.7 (50.7) | 50.5 (50.4) | 50.1 (50.8) | 50.4 (50.6) | 50.8 (50.3) |
| Median adult age in years^ | 49.5 | 55–64 (44.5) | 35–44 (43.8) | 35–44 (44.0) | 35–44 (46.2) | 45–54 (47.0) |
| Median annual income (local currency)^ | – | $42–52 K ($47 K) | $35–40 K ($41 K) | $30–35 K ($39 K) | £20-25 K (£22 K) | $52–65 K ($63 K) |
| Median annual income ($US)^ | $30–38 K ($37 K) | $31–39 K ($35 K) | $24–27 K ($29 K) | $30–35 K ($39 K) | $24–30 K ($26 K) | $42–53 K ($51 K) |
| Type of area residing (%): | ||||||
| Living in a rural area | 30.9 | 25.4 | 26.4 | 43.9 | 29.9 | 30.8 |
| Living in a small metropolitan area | 27.0 | 22.0 | 30.6 | 31.0 | 29.2 | 29.8 |
| Living in large metropolitan area | 42.1 | 52.6 | 43.0 | 25.1 | 40.9 | 39.5 |
| Household type (%): | ||||||
| Couple with no dependent children | 35.1 | 42.2 | 32.6 | 26.4 | 34.4 | 31.7 |
| Family with dependent children | 29.2 | 26.7 | 31.7 | 30.4 | 30.6 | 31.1 |
| Lone person | 20.3 | 20.1 | 16.1 | 20.9 | 18.3 | 24.5 |
| Other household type (e.g., group household) | 15.3 | 11.0 | 19.6 | 22.2 | 16.7 | 12.7 |
| Employment status (%): | ||||||
| Full-time | 37.4 | 31.7 | 39.6 | 34.0 | 45.6 | 47.5 |
| Part-time/casual | 16.3 | 16.9 | 18.9 | 15.5 | 15.9 | 14.5 |
| Unemployed (looking) | 7.4 | 6.6 | 9.4 | 9.0 | 7.1 | 6.1 |
| Unemployed (not looked) | 5.6 | 5.1 | 6.8 | 6.3 | 5.4 | 5.1 |
| Retired | 24.6 | 32.8 | 15.5 | 23.3 | 17.9 | 17.6 |
| Other employment or not stated | 8.8 | 6.9 | 9.8 | 12.0 | 8.0 | 9.2 |
| Highest education qualification (%): | ||||||
| No qualification | 9.2 | 16.2 | 11.1 | 3.5 | 3.7 | 3.0 |
| High school qualification | 21.4 | 13.0 | 33.0 | 26.4 | 22.1 | 26.6 |
| Bachelor degree qualification | 24.7 | 23.6 | 22.6 | 22.4 | 27.1 | 29.8 |
| Postgraduate (Masters, PhD) qualification | 13.6 | 16.9 | 17.0 | 13.2 | 18.5 | 20.3 |
| Other qualification (eg apprenticeship) | 31.1 | 30.3 | 16.4 | 34.5 | 28.6 | 20.3 |
| Control variable | Overall | AUS | NZ | US | ENG | CAN |
| Religion (%): | ||||||
| Catholic | 21.0 | 21.0 | 11.3 | 24.6 | 12.0 | 29.8 |
| Anglican | 9.3 | 13.7 | 8.0 | 0.6 | 18.5 | 3.4 |
| Protestant | 8.7 | 5.8 | 5.0 | 16.0 | 5.7 | 11.4 |
| Baptist | 3.0 | 1.6 | 3.1 | 6.8 | 1.3 | 2.4 |
| Other Christian | 6.4 | 7.4 | 5.9 | 7.0 | 4.8 | 4.4 |
| Buddhism or Hinduism | 3.0 | 3.6 | 4.0 | 1.9 | 2.3 | 2.8 |
| Islam | 2.3 | 1.6 | 1.2 | 2.2 | 6.9 | 1.6 |
| Other religion | 10.5 | 7.9 | 9.7 | 17.2 | 8.2 | 10.6 |
| No religion | 35.9 | 37.5 | 51.8 | 23.6 | 40.3 | 33.7 |
| Religiosity (-1=not at all; +1=very much so) | −0.25 (0.71)# | −0.30 (0.68) | −0.35 (0.71) | −0.04 (0.73) | −0.38 (0.67) | −0.26 (0.70) |
| Political orientation (left-wing=0; right-wing=100) | 52.8 (22.8)# | 53.3 (21.2) | 49.1 (23.1) | 55.3 (26.7) | 53.3 (20.6) | 50.5 (22.1) |
| Flu-vaccination rates (%): | ||||||
| Received flu vaccine in last 12 months | 47.3 | 57.6 | 40.1 | 45.6 | 37.6 | 37.4 |
| Received flu vaccine in last 2 years | 15.2 | 13.3 | 16.3 | 16.6 | 15.0 | 17.6 |
| Received flu vaccine in last 5 years | 9.2 | 7.2 | 11.0 | 11.6 | 9.3 | 9.5 |
| Received flu vaccine more than 5 years ago | 9.0 | 5.7 | 11.0 | 11.5 | 9.6 | 11.7 |
| Never received flu vaccine | 19.2 | 16.3 | 21.4 | 14.6 | 28.5 | 23.9 |
| COVID-19 testing (%): | ||||||
| Individual received positive C-19 test result | 1.8 | 1.0 | 0.2 | 3.8 | 3.1 | 1.0 |
| Individual received negative C-19 test result | 23.3 | 23.2 | 22.3 | 28.9 | 24.3 | 16.3 |
| Individual not been tested for C-19 | 74.9 | 75.9 | 77.5 | 67.2 | 72.6 | 82.7 |
| Know another who has died from C-19 | 7.3 | 3.4 | 2.7 | 13.7 | 13.8 | 6.2 |
| Know another testing positive for C-19, but not died | 10.1 | 3.7 | 4.0 | 20.3 | 17.3 | 10.2 |
| Know another receiving negative C-19 test result | 43.8 | 52.8 | 54.0 | 29.5 | 33.0 | 42.8 |
| Do not know another who has been tested or died | 38.8 | 40.1 | 39.4 | 36.6 | 35.9 | 40.8 |
# Sample standard deviation shown in parentheses.
^ Census results adjusted for inflation shown in parentheses.
Sources (date of Census result available shown in parentheses):
Australian Bureau of Statistics (2016).
Statistics New Zealand (2018).
United States Census Bureau (2010).
Office for National Statistics, United Kingdom (2018).
Statistics Canada (2016).
With respect to flu-vaccination rates, more than half the Australian sample (57%) had received the flu-vaccine in the last 12 months, and also had the highest flu-vaccination rates over the last five years (78%). English and Canadian respondents reported the lowest rates of flu-vaccination with 29% and 24%, respectively, having never received the flu-vaccine. The United States reported the highest rates of flu vaccination uptake, with 15% having never received the flu compared with 29% among respondents living in England, where uptake was the lowest among the countries sampled. Individuals who had been tested for COVID-19 and received positive results were more likely to reside in the United States (3.8%) or England (3.1%), with the lowest rates of a positive result following COVID-19 testing among New Zealanders (0.2%). Overall, a quarter of the sample had received testing for COVID-19, with individual test rates highest in the United States (33%) and lowest in Canada (17%). Those living in the United States or England were more likely to know someone who had died from COVID-19, representing 14% of respondents from each country. Similarly, these countries recorded a higher proportion of respondents who knew of another person who had tested positive for COVID-19. In contrast, more than half of the Australian and New Zealand samples knew someone who had undertaken COVID-19 testing, but returned a negative result.
5.2. Reliability and validity of measures
The first stage of analysis involved exploratory factor analysis (EFA) using principal components analysis with varimax rotation. The final measurement model results reported were based on a confirmatory factor analysis (CFA) using covariance-based modelling. The endogenous variable in the model, intentions to receive the COVID-19 vaccination, was measured using three reflective items, with all factor loadings above the benchmark of 0.707 as reported in Table 3 . The resulting average variance extracted (AVE) of 0.953 of the latent construct exceeded 0.5 to establish convergent validity, whilst both Cronbach Alpha (CA = 0.975) and Composite Reliability (CR = 0.984) exceeded 0.7 to establish reliability [42]. Overall, the latent factor score was significantly different across the five countries sampled (F = 43.75; p < 0.001). Post-hoc contrasts of each country mean against the mean of all other countries combined indicated significantly higher COVID-19 vaccination intentions among Australians (t = 9.551; p < 0.001) and lower intentions among those living in the United States (t = −8.861; p < 0.001). Overall, 66% of the sample agreed that they would receive COVID-19 vaccination, with Australians having the highest rates of intention (73%), followed by individuals living in Canada (66%), England (64%), New Zealand (62%), and the United States (55%). In contrast, 29% and 11% of those from the United States and Australia, respectively, stated an intention not to receive the vaccine.
Table 3.
Factor Loadings and Descriptive Statistics (Endogeneous Variable).
| Sample Mean (Standard Deviation) |
Test of Differences in Means^ |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ENDOGENEOUS VARIABLE | Factor Loading | AUS | NZ | US | ENG | CAN | Overall | F-stat. | p-val | sig. |
| Intention to have C19 vaccination (individual) (CA = 0.975; CR = 0.984; AVE = 0.953) | 5.46 (1.66)a | 5.08 (1.77) | 4.52 (1.96)b | 5.03 (1.88) | 5.11 (1.89) | 5.11 (1.84) | 43.75 | 0.00 | ** | |
| I will certainly have the COVID-19 vaccine when it is approved by Government. | 0.977 | 5.46 (1.69)a | 5.06 (1.82) | 4.49 (2.02)b | 5.01 (1.96) | 5.12 (1.93) | 5.10 (1.89) | 43.82 | 0.00 | ** |
| I will definitely get vaccinated when a COVID-19 vaccine is available. | 0.976 | 5.43 (1.70)a | 5.08 (1.81) | 4.51 (2.04)b | 5.00 (1.97) | 5.09 (1.92) | 5.09 (1.89) | 39.60 | 0.00 | ** |
| When a COVID-19 vaccine is approved by government, I will get vaccinated. | 0.976 | 5.49 (1.67)a | 5.10 (1.80) | 4.55 (2.03)b | 5.06 (1.94) | 5.13 (1.92) | 5.14 (1.87) | 41.98 | 0.00 | ** |
CA = Cronbach Alpha; CR = Composite Reliability; AVE = Average Variance Extracted.
^ Test of differences in means across five countries sampled; */** p < .05/.01. a/b – country mean significantly higher/lower than mean excluding country (p < .05).
The EFA yielded four disease related constructs, seven vaccine hesitancy, and three control variables with reflective measures (general health, altruism, and collectivism) as intended. A total of 58 reflective measurement items were used in the final CFA model, with 12 items removed as their respective factor loadings were below the benchmark of 0.707 or significant cross-loadings were detected. The full list of removed items and their measurement properties are available upon request. The remaining factor loadings and measures of validity and reliability are reported in Tables 4 and 5 for the eleven exogenous variables. Discriminant validity was also established as the squared correlation between any two variables was less than their respective AVEs [42].
Table 4.
Factor Loadings and Descriptive Statistics (Disease Related Variables).
|
Sample Mean (Standard Deviation) |
Differences in Means^ |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| EXOGENEOUS VARIABLES (DISEASE RELATED) | Est λ | AUS | NZ | US | ENG | CAN | Overall | F-stat. | p-val | sig. |
| Perceived Disease Severity (for individual) (CA=0.960; CR=0.974; AVE=0.926) | 5.62 (1.52)a | 5.50 (1.50) | 5.40 (1.74) | 5.17 (1.74)b | 5.48 (1.63) | 5.49 (1.63) | 9.49 | 0.00 | ** | |
| Contracting COVID-19 is not dangerous for people like me (R) | 0.961 | 5.61 (1.57)a | 5.46 (1.56) | 5.43 (1.78) | 5.19 (1.79)b | 5.48 (1.69) | 5.40 (1.68) | 7.69 | 0.00 | ** |
| Contracting COVID-19 is not serious for people like me (R) | 0.963 | 5.62 (1.55)a | 5.52 (1.55) | 5.41 (1.83) | 5.14 (1.80)b | 5.47 (1.69) | 5.40 (1.69) | 10.05 | 0.00 | ** |
| COVID-19 is not a serious illness for people like me (R) | 0.964 | 5.63 (1.57)a | 5.53 (1.56) | 5.37 (1.85) | 5.20 (1.82)b | 5.49 (1.69) | 5.42 (1.70) | 9.14 | 0.00 | ** |
| Perceived Disease Severity (for others) (CA=0.949; CR=0.967; AVE=0.908) | 5.15 (1.47)a | 5.10 (1.46)a | 5.01 (1.61) | 4.55 (1.64)b | 5.12 (1.50)a | 4.95 (1.54) | 18.54 | 0.00 | ** | |
| Contracting COVID-19 would be very dangerous for most people in the community. | 0.948 | 5.08 (1.55)a | 5.00 (1.57) | 4.96 (1.71) | 4.53 (1.73)b | 5.07 (1.61)a | 4.89 (1.64) | 13.97 | 0.00 | ** |
| Getting COVID-19 would be very serious for most people in the community. | 0.957 | 5.18 (1.52)a | 5.14 (1.53)a | 5.02 (1.69) | 4.57 (1.69)b | 5.16 (1.54)a | 4.98 (1.60) | 17.78 | 0.00 | ** |
| COVID-19 would be a very serious illness for most people in the community if they were to contract it. | 0.953 | 5.19 (1.53)a | 5.15 (1.51)a | 5.03 (1.72) | 4.54 (1.73)b | 5.14 (1.57)a | 5.05 (1.61) | 19.33 | 0.00 | ** |
| Perceived Susceptibility to COVID-19 (for individual) (CA=0.888; CR=0.930; AVE=0.816) | 4.14 (1.48)b | 4.05 (1.41)b | 4.44 (1.62)a | 4.51 (1.55)a | 4.35 (1.48) | 4.27 (1.52) | 13.69 | 0.00 | ** | |
| I am far less likely than others to get COVID-19 (R) | 0.916 | 4.26 (1.63) | 4.18 (1.58)b | 4.44 (1.78) | 4.47 (1.69)a | 4.39 (1.62) | 4.33 (1.66) | 4.14 | 0.00 | ** |
| I have an extremely low risk of getting COVID-19 (R) | 0.921 | 4.20 (1.66)b | 4.00 (1.61)b | 4.53 (1.83)a | 4.48 (1.74)a | 4.36 (1.67) | 4.31 (1.71) | 11.80 | 0.00 | ** |
| I am very confident I will not get COVID-19 (R) | 0.872 | 3.97 (1.58)b | 3.96 (1.55)b | 4.37 (1.77)a | 4.59 (1.68)a | 4.31 (1.63) | 4.18 (1.65) | 23.66 | 0.00 | ** |
| Perceived Susceptibility to COVID-19 (for others) (CA=0.947; CR=0.966; AVE=0.904) | 4.05 (1.46)b | 3.83 (1.51)b | 4.67 (1.54)a | 4.80 (1.42)a | 4.51 (1.41)a | 4.32 (1.51) | 63.07 | 0.00 | ** | |
| Many people in the community will get COVID-19. | 0.951 | 3.98 (1.51)b | 3.75 (1.53)b | 4.65 (1.64)a | 4.76 (1.47)a | 4.50 (1.47)a | 4.27 (1.57) | 66.19 | 0.00 | ** |
| I expect many people in the community will contract COVID-19. | 0.954 | 3.98 (1.52)b | 3.77 (1.57)b | 4.62 (1.67)a | 4.78 (1.50)a | 4.44 (1.52)a | 4.26 (1.59) | 60.95 | 0.00 | ** |
| COVID-19 will infect many people in the community. | 0.947 | 4.19 (1.55)b | 3.97 (1.64)b | 4.75 (1.64)a | 4.85 (1.48)a | 4.59 (1.49)a | 4.43 (1.59) | 45.20 | 0.00 | ** |
(R) – item reverse coded; CA = Cronbach Alpha; CR = Composite Reliability; AVE = Average Variance Extracted.
^ Test of differences in means across five countries sampled; */** p < .05/.01. a/b – country mean significantly higher/lower than mean excluding country (p < .05).
Table 5.
Factor loadings and Descriptive Statistics – Vaccine Hesitancy Related Beliefs.
| EXOGENOUS VARIABLES (VACCINE-RELATED) | Est λ | AUS | NZ | US | ENG | CAN | Overall | F-stat.^ |
|---|---|---|---|---|---|---|---|---|
| Ability to Free-Ride (CA = 0.943; CR = 0.963; AVE = 0.897) | 2.38 (1.55)b | 2.70 (1.58) | 2.95 (1.75)a | 2.72 (1.68) | 2.68 (1.68) | 2.62 (1.64) | 21.39** | |
| There is no need for me to have a COVID-19 vaccine if most people in the community get vaccinated. | 0.951 | 2.38 (1.62)b | 2.70 (1.67) | 2.97 (1.89)a | 2.72 (1.76) | 2.71 (1.77) | 2.63 (1.74) | 20.99** |
| If most people in the community get a COVID-19 vaccine, I do not need to be vaccinated. | 0.943 | 2.40 (1.62)b | 2.68 (1.68) | 2.94 (1.86)a | 2.75 (1.80) | 2.68 (1.77) | 2.62 (1.74) | 18.09** |
| I don’t need to get a COVID-19 vaccine if most people in the community have a COVID-19 vaccine. | 0.948 | 2.38 (1.60)b | 2.70 (1.68) | 2.93 (1.87)a | 2.69 (1.74) | 2.65 (1.75) | 2.60 (1.72) | 18.99** |
| Perceived Vaccine Effectiveness (for individual) (CA = 0.90; CR = 0.94; AVE = 0.83) | 4.78 (1.22)a | 4.62 (1.25) | 4.34 (1.45)b | 4.55 (1.41) | 4.62 (1.39) | 4.61 (1.34) | 17.05** | |
| If I get a COVID-19 vaccine, I will not get sick from COVID-19. | 0.887 | 4.44 (1.41)a | 4.34 (1.43) | 4.08 (1.64)b | 4.30 (1.56) | 4.33 (1.54) | 4.32 (1.51) | 8.67** |
| If I have a COVID-19 vaccine, I will be protected from getting C-19. | 0.927 | 4.84 (1.35)a | 4.65 (1.40) | 4.41 (1.63)b | 4.62 (1.56) | 4.66 (1.50) | 4.67 (1.48) | 13.20** |
| A COVID-19 vaccine will prevent me contracting the disease. | 0.919 | 5.06 (1.32)a | 4.87 (1.34) | 4.53 (1.66)b | 4.73 (1.51) | 4.87 (1.54) | 4.85 (1.48) | 21.40** |
| Side-effects of C-19 Vaccine (CA = 0.86; CR = 0.91; AVE = 0.78) | 4.21 (1.55)b | 4.42 (1.45) | 4.52 (1.62)a | 4.30 (1.58) | 4.34 (1.54) | 4.33 (1.56) | 6.45** | |
| I am not worried at all about adverse side-effects of a COVID-19 vaccine (R) | 0.898 | 4.33 (1.75)b | 4.46 (1.66) | 4.63 (1.85)a | 4.41 (1.87) | 4.45 (1.74) | 4.44 (1.78) | 4.49** |
| I think the C-19 vaccine has undergone enough testing to be safe (R) | 0.861 | 3.98 (1.68)b | 4.28 (1.62)a | 4.29 (1.84)a | 3.99 (1.71)b | 4.07 (1.68) | 4.09 (1.72) | 7.05** |
| I am not concerned at all about potential negative long-term side-effects from a COVID-19 vaccine (R) | 0.887 | 4.33 (1.78)b | 4.53 (1.70) | 4.64 (1.87)a | 4.51 (1.80) | 4.50 (1.79) | 4.47 (1.80) | 4.87** |
| Trust in government (CA = 0.97; CR = 0.97; AVE = 0.83) | 5.26 (1.42)a | 5.27 (1.32)a | 4.21 (1.60)b | 4.74 (1.55)b | 4.97 (1.57) | 4.92 (1.55) | 82.02** | |
| The information I receive about vaccines from the government is reliable and trustworthy. | 0.923 | 5.22 (1.50)a | 5.22 (1.47)a | 4.17 (1.78)b | 4.64 (1.68)b | 4.92 (1.66) | 4.87 (1.66) | 71.67** |
| Government will communicate honestly about the possible health effects of a COVID-19 vaccine. | 0.923 | 5.19 (1.57)a | 5.27 (1.48)a | 4.10 (1.84)b | 4.63 (1.80)b | 4.97 (1.72)a | 4.86 (1.73) | 73.58** |
| If a COVID-19 vaccine is found to be a health risk, government will openly and honestly inform the public. | 0.906 | 5.13 (1.59)a | 5.22 (1.49)a | 4.05 (1.87)b | 4.59 (1.76)b | 4.89 (1.75)a | 4.80 (1.75) | 71.18** |
| I trust government to make safety a priority when approving COVID-19 vaccines. | 0.914 | 5.38 (1.54)a | 5.42 (1.46)a | 4.24 (1.88)b | 4.80 (1.81)b | 5.09 (1.73) | 5.02 (1.73) | 78.42** |
| Government has a history of only approving vaccines once they have been proven safe and effective. | 0.858 | 5.37 (1.43)a | 5.24 (1.45)a | 4.41 (1.79)b | 5.03 (1.58) | 4.99 (1.63) | 5.05 (1.61) | 58.12** |
| I have confidence that government approved COVID-19 vaccines will be safe and effective. | 0.915 | 5.25 (1.55)a | 5.18 (1.54)a | 4.29 (1.80)b | 4.76 (1.73)b | 4.99 (1.69) | 4.94 (1.69) | 54.47** |
| I have confidence in the government to properly assess the safety and effectiveness of COVID-19 vaccines. | 0.929 | 5.26 (1.57)a | 5.31 (1.53)a | 4.21 (1.82)b | 4.74 (1.77)b | 4.97 (1.71) | 4.93 (1.72) | 67.17** |
| Conspiracy Beliefs about Vaccination (CA=0.972; CR=0.976; AVE=0.838) | 3.17 (1.50)b | 3.46 (1.52) | 3.77 (1.57)a | 3.52 (1.57) | 3.36 (1.59) | 3.48 (1.56) | 25.43** | |
| Vaccine safety data is often fabricated. | 0.935 | 3.26 (1.67)b | 3.61 (1.69) | 3.76 (1.81)a | 3.46 (1.78) | 3.43 (1.74) | 3.53 (1.74) | 9.47** |
| Immunizing children is harmful and this fact is covered up. | 0.901 | 2.62 (1.64)b | 3.01 (1.69) | 3.38 (1.88)a | 3.14 (1.88) | 3.05 (1.79) | 3.08 (1.79) | 22.34** |
| Pharmaceutical companies cover up the dangers of vaccines. | 0.902 | 3.54 (1.70)b | 3.87 (1.70) | 4.00 (1.82)a | 3.77 (1.71) | 3.56 (1.80)b | 3.83 (1.74) | 9.13** |
| People are deceived about vaccine effectiveness. | 0.921 | 3.29 (1.72)b | 3.65 (1.67) | 3.88 (1.79)a | 3.62 (1.69) | 3.45 (1.76) | 3.66 (1.71) | 13.40** |
| Vaccine effectiveness data is often fabricated. | 0.935 | 3.24 (1.66)b | 3.50 (1.66) | 3.83 (1.77)a | 3.62 (1.75) | 3.42 (1.77) | 3.59 (1.72) | 13.68** |
| People are deceived about vaccine safety. | 0.920 | 3.27 (1.70)b | 3.48 (1.72) | 3.88 (1.79)a | 3.52 (1.75) | 3.50 (1.69) | 3.59 (1.73) | 13.01** |
| The government is trying to cover up the link between vaccines and autism. | 0.895 | 2.76 (1.65)b | 3.00 (1.66) | 3.37 (1.92)a | 3.14 (1.78) | 2.86 (1.77)b | 3.09 (1.75) | 14.60** |
| People don't know the real truth about the dangers of vaccines. | 0.913 | 3.40 (1.76)b | 3.75 (1.79) | 4.04 (1.87)a | 3.84 (1.74) | 3.53 (1.80)b | 3.80 (1.79) | 15.41** |
| Perceived Effectiveness of C-19 Vaccination (for others) (CA=0.941; CR=0.957; AVE=0.849) | 5.38 (1.32)a | 5.12 (1.35) | 4.64 (1.55)b | 5.08 (1.50) | 5.14 (1.50) | 5.12 (1.45) | 39.63** | |
| If I have a COVID-19 vaccine, it will help protect others in my community from COVID-19. | 0.919 | 5.35 (1.41)a | 5.08 (1.51) | 4.64 (1.72)b | 5.07 (1.62) | 5.15 (1.60) | 5.10 (1.57) | 30.98** |
| I can help protect the health of others in my community by having a COVID-19 vaccine. | 0.932 | 5.42 (1.42)a | 5.18 (1.43) | 4.67 (1.72)b | 5.12 (1.62) | 5.21 (1.57) | 5.16 (1.56) | 35.14** |
| If I have a COVID-19 vaccine it will reduce the risk of COVID-19 spreading in my community | 0.920 | 5.39 (1.40)a | 5.15 (1.45) | 4.63 (1.71)b | 5.08 (1.63) | 5.14 (1.60) | 5.12 (1.56) | 36.04** |
| I can help increase the level of COVID-19 immunity in my community by having a COVID-19 vaccine. | 0.916 | 5.36 (1.45)a | 5.08 (1.51) | 4.62 (1.76)b | 5.03 (1.63) | 5.06 (1.66) | 5.08 (1.61) | 32.25** |
| Perceived C-19 Vaccine Availability (CA=0.84; CR=0.90; AVE=0.68) | 5.19 (1.14)a | 4.76 (1.11) | 4.43 (1.35)b | 4.66 (1.26)b | 4.78 (1.25) | 4.72 (1.22) | 70.09** | |
| COVID-19 vaccines will be very affordable for me. | 0.825 | 5.06 (1.45)a | 4.60 (1.44)b | 4.43 (1.68)b | 4.82 (1.59) | 4.84 (1.62) | 4.72 (1.55) | 28.96** |
| It will be easy for me to get a COVID-19 vaccine when one is available. | 0.866 | 5.22 (1.36)a | 4.81 (1.42) | 4.47 (1.65)b | 4.57 (1.59)b | 4.73 (1.53) | 4.71 (1.52) | 50.53** |
| It will be easy for me to find out where I can get a COVID-19 vaccine when one is available. | 0.821 | 5.59 (1.24)a | 5.39 (1.33)a | 4.73 (1.64)b | 4.98 (1.50)b | 5.19 (1.46) | 5.23 (1.44) | 65.65** |
| There will be enough COVID-19 vaccines for everyone who wants one in my community. | 0.771 | 4.91 (1.44)a | 4.25 (1.50)b | 4.10 (1.64)b | 4.25 (1.56)b | 4.35 (1.56) | 4.36 (1.54) | 58.54** |
(R) – item reverse coded; CA = Cronbach Alpha; CR = Composite Reliability; AVE = Average Variance Extracted.
^ Test of differences in means across five countries sampled; */** p < .05/.01. a/b – country mean significantly higher/lower than mean excluding country (p < .05).
Measures of perceived susceptibility to and severity of the COVID-19 for both individuals and others are reported in Table 4. Perceived severity following infection for both individuals and others was significantly higher in the United States and England, whilst significantly higher among Canadians in relation to susceptibility for others only (p < .001). Australians and New Zealanders reported significantly lower rates of perceived susceptibility for both themselves and others (p < .001).
Measures of perceptions relating to the vaccine itself are reported in Table 5. The results indicate that Australians held significantly higher levels of agreement with respect to perceived effectiveness of the vaccine for themselves (Mdiff = 0.251; t = 6.19; p < .001) and for others (Mdiff = 0.382; t = 8.76; p < .001). Those living in the United States were significantly lower in evaluation of the perceived effectiveness of the vaccine for themselves and others (teff_indiv = -5.63; teff_others = −9.22; p < .001). A similar pattern of results emerged for concerns about the potential adverse side effects of the COVID-19 vaccination and vaccine conspiracy beliefs. Differences in trust regarding government approval of COVID-19 vaccines represented the largest source of differences across the five countries (F = 82.02; p < .001). Levels of trust were significantly higher in New Zealand (t = 7.028; p < .001) and Australia (t = 10.01; p < .001), and significantly lower in the United States (t = −14.18; p < .001) and England (t = −2.56; p < .05). Differences in perceived vaccine availability also emerged, with Australians more likely to believe it would be easily available (t = 14.95; p < .001), whilst those in the United States (t = −8.31; p < .001) and England (t = −2.28; p < .05) had significant concerns about vaccine availability. Those living in the United States were significantly more likely to express intentions not to be vaccinated because of “free-riding” (t = 4.446; p < .001); such intentions were significantly lower among Australians (t = -7.021; p < .001). The proportion of those with free-riding intentions ranged from 12% among Australians to as high as 20% in the United States sample.
Measures of altruism, collectivism, and perceived general health were included as control variables in the model of vaccination intentions presented below. Before doing so, the reflective measures were assessed in terms of their reliability and validity. As reported in Table 6 , all factor loadings for the measures of altruism, collectivism, and perceived health were more than 0.71, whilst Cronbach Alpha’s, Composite Reliability and Average Variance Extracted were all above the acceptable benchmarks.
Table 6.
Factor loadings and Descriptive Statistics – Control Variables.
| CONTROL VARIABLE | Est λ | AUS | NZ | US | ENG | CAN | Overall | F-stat.^ |
|---|---|---|---|---|---|---|---|---|
| Altruism (CA = 0.89; CR = 0.92; AVE = 0.75) | 4.97 (1.10) | 4.96 (1.19) | 4.95 (1.30) | 4.85 (1.27) | 5.02 (1.21) | 4.96 (1.20) | 1.70. | |
| I often do things for others more than for myself | 0.871 | 5.01 (1.27) | 5.01 (1.37) | 5.00 (1.52) | 4.80 (1.51)b | 5.03 (1.37) | 4.99 (1.39) | 2.86* |
| I tend to put people first, then myself | 0.876 | 4.98 (1.27) | 4.96 (1.38) | 4.99 (1.53) | 4.87 (1.44) | 5.01 (1.41) | 4.97 (1.38) | 0.85. |
| I often think about other people when I am doing something even for me | 0.744 | 5.07 (1.20) | 5.05 (1.36) | 5.03 (1.45) | 4.99 (1.38) | 5.19 (1.31) | 5.07 (1.32) | 2.05. |
| I often help others at the expense of my own personal well-being | 0.851 | 4.80 (1.32) | 4.80 (1.37) | 4.79 (1.54) | 4.73 (1.50) | 4.87 (1.44) | 4.80 (1.42) | 0.82. |
| Collectivism (CA = 0.91; CR = 0.93; AVE = 0.78) | 5.67 (1.01)a | 5.55 (1.09) | 5.43 (1.24)b | 5.39 (1.12)b | 5.66 (1.02)a | 5.57 (1.09) | 12.93** | |
| I think it is important to do things for “the greater good” | 0.883 | 5.75 (1.13)a | 5.67 (1.20) | 5.47 (1.44)b | 5.49 (1.29)b | 5.76 (1.13)a | 5.65 (1.14) | 10.69** |
| Doing things for “the greater good” is important to me. | 0.877 | 5.65 (1.14)a | 5.53 (1.22) | 5.41 (1.45)b | 5.32 (1.33)b | 5.65 (1.20)a | 5.54 (1.26) | 8.56** |
| The well-being of those outside my family is important to me. | 0.815 | 5.52 (1.15)a | 5.38 (1.29) | 5.38 (1.39) | 5.27 (1.30)b | 5.62 (1.14)a | 5.46 (1.24) | 9.97** |
| Doing things for other people in the community should be encouraged | 0.832 | 5.75 (1.06)a | 5.63 (1.17) | 5.47 (1.39)b | 5.50 (1.26)b | 5.61 (1.19) | 5.62 (1.20) | 11.83** |
| Perceived General Health (CA = 0.96; CR = 0.97; AVE = 0.92) | 4.62 (1.50) | 4.80 (1.46)a | 4.54 (1.62)b | 4.54 (1.58) | 4.71 (1.52) | 4.63 (1.54) | 3.19*. | |
| I consider myself to be in very good health. | 0.962 | 4.64(1.56) | 4.78(1.50) a | 4.56(1.74) | 4.57(1.69) | 4.74(1.59) | 4.65(1.61) | 2.41*. |
| My general health is excellent. | 0.955 | 4.58(1.56) | 4.80(1.55) a | 4.46(1.76) b | 4.49(1.67) | 4.68(1.59) | 4.58(1.62) | 4.57** |
| I am a very healthy individual. | 0.958 | 4.64(1.53) | 4.81(1.50) | 4.60(1.70) | 4.57(1.61) | 4.72(1.58) | 4.65(1.58) | 2.20 . |
(R) – item reverse coded; CA = Cronbach Alpha; CR = Composite Reliability; AVE = Average Variance Extracted.
^ Test of differences in means across five countries sampled; */** p < .05/.01. a/b – country mean significantly higher/lower than mean excluding country (p < .05).
5.3. Model results
A structural model predicting self-reported vaccination intentions was estimated using a covariance based approach. The normed fit index was 0.959 above a value of 0.9 indicating acceptable levels of incremental fit [43]. The standardized root mean square residual was 0.012, significantly below the suggested benchmark of 0.08 [43]. The Variance Inflation Factors for the structural model components were below the recommended thresholds of 3.3, indicating that our findings are not affected by multicollinearity. The R-square was 0.670 and adjusted R-square was 0.661. All parameter estimates of path relationships for the exogenous variables were significant at the 0.01 level (see Table 7 ), whilst the country-level estimates of the exogeneous variables determined from the inclusion of interaction terms between country and perceptions of the disease and vaccination in the same model are also reported in Table 7. Finally, taken from the same model, but reported separately for convenience, several control variables were also significant (see Table 8 ).
Table 7.
Model Estimates (Exogenous Variables).
|
Aggregate |
AUS |
NZ |
US |
ENG |
CAN |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est (SE) | Std. Est. | Est (SE) | Std. Est. | Est (SE) | Std. Est. | Est (SE) | Std. Est. | Est (SE) | Std. Est. | Est (SE) | Std. Est. | ^ | |
| Perceptions about the threat of illness for individual | |||||||||||||
| SEVi | 0.101 (0.019)** | 0.055** | 0.114 (0.024)** | 0.060** | 0.076 (0.032)* . | 0.048* | 0.057 (0.026)* . | 0.040* . | 0.078 (0.029)** | 0.048** | 0.180 (0.027)** | 0.079** | C |
| RISKi | 0.064 (0.019)** | 0.035** | 0.079 (0.024)** | 0.041** | 0.072 (0.032)* . | 0.037* | 0.061 (0.026)* . | 0.034* . | 0.069 (0.031)* . | 0.037* . | 0.039 (0.028) . | 0.026 . | |
| Perceptions about the threat of illness for others | |||||||||||||
| SEVo | 0.182 (0.019)** | 0.099** | 0.131 (0.024)** | 0.079** | 0.166 (0.033)** | 0.095** | 0.313 (0.027)** | 0.142** | 0.209 (0.029)** | 0.107** | 0.091 (0.028)* . | 0.072* . | Uc |
| RISKo | 0.145 (0.019)** | 0.079** | 0.055 (0.024)* . | 0.044* . | 0.222 (0.031)** | 0.101** | 0.188 (0.027)** | 0.093** | 0.186 (0.032)** | 0.091** | 0.074 (0.028)** | 0.066** | a |
| Evaluation of behaviour to counteract threat | |||||||||||||
| Perceived benefits of vaccination | |||||||||||||
| EFFi | 0.367 (0.018)** | 0.200** | 0.343 (0.023)** | 0.191** | 0.390 (0.030)** | 0.207** | 0.446 (0.025)** | 0.227** | 0.359 (0.028)** | 0.198** | 0.297 (0.027)** | 0.177** | Uc |
| EFFo | 0.599 (0.018)** | 0.327** | 0.612 (0.024)** | 0.332** | 0.545 (0.031)** | 0.312** | 0.578 (0.025)** | 0.319** | 0.622 (0.028)** | 0.334** | 0.638 (0.027)** | 0.338** | |
| Perceived barriers to vaccination | |||||||||||||
| TRUST | 0.764 (0.020)** | 0.416** | 0.708 (0.025)** | 0.395** | 0.757 (0.036)** | 0.414** | 0.734 (0.027)** | 0.405** | 0.784 (0.031)** | 0.422** | 0.837 (0.029)** | 0.444** | |
| AVAIL | 0.271 (0.019)** | 0.148** | 0.249 (0.025)** | 0.139** | 0.246 (0.033)** | 0.141** | 0.357 (0.026)** | 0.179** | 0.240 (0.030)** | 0.139** | 0.263 (0.028)** | 0.142** | U |
| SIDE | 0.383 (0.019)** | 0.209** | 0.342 (0.024)** | 0.193** | 0.373 (0.032)** | 0.206** | 0.477 (0.027)** | 0.241** | 0.379 (0.030)** | 0.208** | 0.344 (0.028)** | 0.197** | U |
| CONSP | -0.454 (0.020)** | -0.247** | -0.413 (0.024)** | -0.231** | -0.481 (0.032)** | -0.255** | -0.439 (0.027)** | -0.242** | -0.519 (0.031)** | -0.266** | -0.418 (0.028)** | -0.241** | |
| FREE | -0.490 (0.019)** | -0.267** | -0.529 (0.024)** | -0.282** | -0.495 (0.031)** | -0.269** | -0.479 (0.026)** | -0.263** | -0.503 (0.030)** | -0.271** | -0.444 (0.027)** | -0.250** | |
SEVi/SEVo = Perceived disease severity (for individual/for others); RISKi/RISKo = Perceived susceptibility to COVID-19 (for individual/for others).
EFFi/EFFo = Perceived effectiveness of C-19 Vaccination (for individual/for others); TRUST = Trust in government approval of C-19 vaccine.
AVAIL = Perceived C-19 vaccine availability; SIDE = perceived side effects of C-19 Vaccine; CONSP = Conspiracy beliefs about vaccination; FREE = perceived ability to free-ride.
Est. refers to unstandardized estimates; SE refers to Standard Error of Estimate; Std. Est refers to standardized estimate.
^ Upper/lower case denotes country estimate significantly higher/lower (p < .05).;
*/** p < .05/.01.
Table 8.
Model Estimates (Control Variables).
| Individual Characteristic | Est B. | S.E. | Std. Est. | Est./SE | p-val. | Sig. |
|---|---|---|---|---|---|---|
| Intercept (Intention to Vaccinate) | 4.813 | 0.093 | – | 51.772 | 0.000 | ** |
| Residing in Australia | 0.051 | 0.032 | 0.020 | 1.585 | 0.113 | |
| Residing in New Zealand | 0.052 | 0.050 | 0.015 | 1.037 | 0.300 | |
| Residing in United States | −0.160 | 0.041 | −0.053 | −3.878 | 0.000 | ** |
| Residing in England | 0.005 | 0.048 | 0.001 | 0.103 | 0.918 | |
| Residing in Canada | 0.052 | 0.043 | 0.017 | 1.216 | 0.224 | |
| General Healthiness of Individual | −0.017 | 0.017 | −0.009 | −1.001 | 0.317 | |
| Altruism | 0.112 | 0.017 | 0.061 | 6.569 | 0.000 | ** |
| Collectivism | 0.172 | 0.017 | 0.094 | 9.971 | 0.000 | ** |
| Age of respondent (in years) | 0.004 | 0.001 | 0.034 | 2.410 | 0.016 | * |
| Male | 0.039 | 0.051 | 0.021 | 0.761 | 0.447 | |
| Age × Male | 0.001 | 0.001 | 0.030 | 1.063 | 0.288 | |
| Living in rural area | 0.002 | 0.025 | 0.001 | 0.061 | 0.951 | |
| Living in small metropolitan area | 0.029 | 0.025 | 0.013 | 1.145 | 0.252 | |
| Living in large metropolitan area | −0.031 | 0.025 | −0.014 | −1.240 | 0.215 | |
| Household type - Couple, no dependent children | −0.016 | 0.028 | −0.006 | −0.562 | 0.574 | |
| Household type - Family, with dependent children | −0.028 | 0.029 | −0.010 | −0.973 | 0.331 | |
| Household type - Lone person | 0.014 | 0.019 | 0.007 | 0.756 | 0.450 | |
| Other household type (e.g., group household) | 0.030 | 0.025 | 0.009 | 1.184 | 0.236 | |
| Full-time employed | 0.056 | 0.035 | 0.019 | 1.589 | 0.112 | |
| Part-time/casual employed | −0.023 | 0.039 | −0.006 | −0.581 | 0.561 | |
| Unemployed (seeking employment) | 0.113 | 0.055 | 0.025 | 2.074 | 0.038 | * |
| Unemployed (not seeking employment) | −0.174 | 0.062 | −0.036 | −2.821 | 0.005 | ** |
| Retired | 0.057 | 0.045 | 0.017 | 1.265 | 0.206 | |
| Other employment (e.g., student) | −0.029 | 0.047 | −0.019 | −0.614 | 0.539 | |
| Standardized income (wrt. country median income) | 0.021 | 0.019 | 0.012 | 1.114 | 0.265 | |
| Political orientation (left wing = 0; right wing = 100) | 0.001 | 0.001 | 0.007 | 0.698 | 0.485 | |
| Religiosity (-1 = Not at all; +1 = Very) | 0.019 | 0.019 | 0.015 | 0.997 | 0.319 | |
| Catholic | 0.041 | 0.044 | 0.016 | 0.929 | 0.353 | |
| Anglican | −0.023 | 0.061 | −0.007 | −0.374 | 0.708 | |
| Protestant | −0.090 | 0.065 | −0.029 | −1.398 | 0.162 | |
| Baptist | −0.044 | 0.117 | −0.012 | −0.382 | 0.703 | |
| Other Christian | −0.026 | 0.068 | −0.008 | −0.381 | 0.703 | |
| Buddhism or Hinduism | −0.031 | 0.106 | −0.009 | −0.295 | 0.768 | |
| Islam | 0.229 | 0.135 | 0.063 | 1.699 | 0.089 | |
| Other religion | −0.058 | 0.056 | −0.019 | −1.027 | 0.304 | |
| No religion | 0.002 | 0.082 | 0.005 | 0.025 | 0.980 | |
| No education qualification | −0.033 | 0.049 | −0.011 | −0.675 | 0.500 | |
| High school qualification | −0.020 | 0.034 | −0.008 | −0.592 | 0.554 | |
| Bachelor degree qualification | 0.082 | 0.033 | 0.033 | 2.476 | 0.013 | * |
| Postgraduate (Masters, PhD) qualification | 0.050 | 0.041 | 0.018 | 1.202 | 0.229 | |
| Other education | −0.079 | 0.039 | −0.032 | −2.013 | 0.044 | * |
| Individual received positive C19 test result | −0.046 | 0.088 | −0.012 | −0.523 | 0.601 | |
| Individual received negative C19 test result | 0.067 | 0.049 | 0.031 | 1.358 | 0.174 | |
| Never been tested for C-19 | −0.021 | 0.069 | −0.019 | −0.307 | 0.759 | |
| Know of another who has died from C19 | 0.015 | 0.055 | 0.005 | 0.276 | 0.782 | |
| Know another who tested positive for C19 but not died | 0.002 | 0.043 | 0.001 | 0.054 | 0.957 | |
| Know another who has received negative C19 test result | −0.003 | 0.033 | −0.002 | −0.103 | 0.918 | |
| Do not know of another who has been tested or died | −0.014 | 0.044 | −0.004 | −0.321 | 0.749 | |
| Received flu vaccine in last 12 months | 0.236 | 0.030 | 0.098 | 7.866 | 0.000 | ** |
| Received flu vaccine in last 2 years | 0.152 | 0.039 | 0.049 | 3.904 | 0.000 | ** |
| Received flu vaccine in last 5 years | 0.068 | 0.047 | 0.019 | 1.453 | 0.146 | |
| Received flu vaccine more than 5 years ago | −0.133 | 0.048 | −0.038 | −2.793 | 0.005 | ** |
| Never received flu vaccine | −0.323 | 0.041 | −0.128 | −7.878 | 0.000 | ** |
Est = unstandardized estimate; SE = Standard error of estimate; Std. Est = standardized estimate.
*/** p < .05/.01.
The model estimates indicate vaccination intention will be significantly higher among individuals who perceive that COVID-19 is a serious disease for themselves (β = 0.101; p < .001) and for others (β = 0.182; p < .001). In contrast, the perceived susceptibility to infection is predicted to have a lower, but significant impact on intentions to vaccinate for assessments made about the infection likelihood for individuals (β = 0.064; p < .001) and for others (β = 0.145; p < .001). The results show that perceptions about severity of and susceptibility to infection relating to others is more significant in explaining vaccination intentions than the same assessment applied to an individual themselves.
All seven vaccine hesitancy beliefs were significant in explaining intentions to vaccinate, with the largest effect related to trust in the government to approve a safe and effective COVID-19 vaccine (β = 0.764; p < .001). In contrast, vaccine uptake was predicted to be significantly lower among those holding free-riding intentions (β = -0.490; p < .001), followed by those holding conspiracy beliefs about vaccinations (β = -0.454; p < .001). The least significant variable related to the impact of perceived availability of the vaccine (β = 0.271; p < .001). Finally, the model showed a distinction between the role of perceived effectiveness of the vaccine in relation to individuals (β = 0.367) and the community (β = 0.599), with the later a more significant predictor of vaccination intentions (p < .001).
Each of the 11 main effects relating to perceptions of the disease and vaccination were accompanied by moderating effects to detect significant differences in the impact that each variable had across the five countries sampled. The significance of the moderating effects are noted in the final column of Table 7, with the resulting overall parameter estimate for each country and its significance presented in the preceding columns. The results indicate that the effects for four of the latent variables on intentions (SEVo, EFFi, AVAIL, SIDE) are significantly greater among those residing in the United States (p < .01). On the other hand, Canadians revealed significantly weaker effects relating to perceptions of disease severity for individuals, disease severity for others, and vaccine effectiveness for themselves as predictors of overall vaccination intentions (p < .01). The moderating effects of country for five of the eleven variables were not significant; that is, the impacts of perceptions relating to perceived risk of infection for individuals, ability to free-ride, conspiracy beliefs, vaccine effectiveness for others, and trust in government approval on vaccination intentions are found to not significantly differ across any of the five countries sampled.
With respect to control variables, the impact of individuals holding collectivist beliefs (β = 0.172; p < .001) and the impact of altruistic beliefs on COVID-19 vaccination intentions (β = 0.112; p < .001), both positively impacted vaccination intentions significantly. Vaccination intentions are predicted to be significantly higher among older individuals (β = 0.004; p < .05), but differences in relation to gender (p = .252) were not detected; and the interaction between gender and age was also not significant (p = .288). Controlling for age and other differences across the sample, only individuals in the United States were predicted to have significantly lower rates of vaccination intention compared to those living in the other countries sampled (β = −0.160; p < .01). Those unemployed, but seeking employment, held significantly higher vaccination intentions (β = 0.113; p < .05), whilst those unemployed, but not actively seeking work had significantly lower intentions to be vaccinated (β = −0.174; p < .01). With respect to education, only those holding a Bachelor degree or above were significantly higher in their stated intentions to vaccinate (β = 0.082; p < .01). Past influenza vaccination behaviour was a strong predictor of COVID-19 vaccination intentions, with those having received the flu vaccine in the last year (β = 0.236; p < .001) or last two years (β = 0.152; p < .001) more likely to vaccinate; those who had received the flu vaccine more than five years ago (β = −0.133; p < .01) or not at all (β = −0.323; p < .001) had significantly lower intentions to receive a COVID-19 vaccine. Finally, a range of control variables had no significant effect with respect to explaining vaccination intentions, including whether an individual lived in rural or metropolitan area, household type, income, political orientation, religion and religiosity, and whether they knew someone who had been tested for COVID-19 or had died from the disease.
6. Discussion
The objective of our research was to determine an individual’s perceptions about disease related threats and beliefs and how dimensions of vaccine hesitancy would affect COVID-19 vaccination intentions. The most significant predictor of vaccination intentions was perceived trust in the government approval of COVID-19 vaccines, followed by perceptions of vaccine effectiveness in protecting others, ability to forgo vaccination by relying on the uptake of others (free-riding), vaccine conspiracy beliefs, perceived side effects, perceived effectiveness for individuals, and perceived availability.
The results show that reassuring information from governments regarding the safety and effectiveness of COVID-19 vaccines and their approval are critical to vaccine uptake. Indeed, the model results indicate that levels of trust in the government to be transparent and follow appropriate vaccine approval processes was found to be the most important factor in driving vaccination intentions among the 11 HBM constructs examined. Information is also a mechanism to reduce decision uncertainty and fosters positive beliefs about other dimensions of the HBM model, including beliefs about the trust, effectiveness, and availability of COVID-19 vaccination. Similarly, accurate and credible information are important to correct beliefs relating to vaccination conspiracies. Our model predicts that intentions relating to vaccination uptake can be significantly improved by addressing these concerns. The current research, however, is unclear about the medium and message content to deliver such assurances. Philip et al. [44] suggests that modern digital communication strategies are one avenue to promote vaccination coverage, whilst more personalized forms of information from healthcare providers have been shown to be most effective, particularly among parents [14]. As such, future research would be beneficial to understand the appropriate strategy to deliver trusted information to strengthen perceptions of vaccine effectiveness and safety. However, engaging with people holding anti-vaccination beliefs through targeted communications is difficult owing to confirmation bias, where information countering existing views is rejected, but information fitting with existing views is more accepted [45]. French et al. [45] recommends that a more effective approach is to provide a combination of positive messaging emphasizing protection of the individual, family, and community, whilst communicating the losses associated with vaccine avoidance (including death, poor health, inability to travel, etc.).
Targeting particular groups with effective messaging can be informed by a range of socio-demographic variables found to be significant in the model. Whilst previous literature motivated several segmentation variables for inclusion, such as gender or income, many of these were not significant in predicting COVID-19 vaccine uptake. Other control variables, however, were significant. For example, those unemployed, but (not) seeking employment, were more (less) likely to be vaccinated. One explanation for this is that potential employees may use vaccination as a signal of their availability for the workforce relative to non-vaccinated individuals [46]. Indeed, several employers have publicly stated that they would not employ those who have not been vaccinated, although the legalities of doing so are unclear [47].
The model also indicates that younger people have significantly lower vaccination intentions than older people. Whilst younger people tend to have higher propensities for risk [48], another explanation is that older people may perceive themselves to be at greater risk of comorbidities. Nonetheless, an individual’s perceived general health was not significant in predicting vaccination uptake. As such, information targeted at young people should highlight the disease risks for healthy individuals and the role they play in protecting others in the community, whilst promoting the economic and social benefits that can occur once the spread of the disease is contained.
A critical contribution of our model of vaccination intentions is the distinction we make between an individuals’ assessment about factors relating to threats to themselves from threats to others. Interestingly, consideration of others with respect to the threat of the disease were stronger in explaining vaccination uptake than those relating to the individual (βdiff = 0.081; t = 4.26; p < .001). Similarly, vaccine effectiveness was stronger in explaining vaccination uptake than those relating to the individual (βdiff = 0.232; t = 12.89; p < .001). Likewise, individuals with stronger collectivist beliefs as well as altruistic beliefs outside of the context of COVID-19 had stronger vaccination intentions (βdiff = 0.060; t = 3.53; p < .001). Overall, these results suggest that decisions based on altruism and social norms are essential factors in explaining vaccination intentions. This appears a fruitful avenue for messaging to promote vaccine uptake for “the greater good” rather than solely for individualistically motivated reasons. It is also noted, however, higher vaccination uptake by others negatively impacted vaccination intentions, with around 15% of individuals indicating they would engage in free-riding behavior.
A notable finding is that the prior receipt of the flu vaccine was a significant predictor of vaccination intentions for COVID-19. The result may reflect those individuals with a behavioral tendency to accept vaccinations in general.3 Conversely, it also indicates that those who have not been vaccinated in other domains may be less inclined to receive vaccination for COVID-19. One limitation of our finding, however, is that we included a measure of vaccination behavior in one context (i.e., flu). Future research could ascertain the generalizability of the result by examining prior behaviors in other contexts (e.g., chickenpox; rubella; HPV) as predictors of COVID-19 vaccination intentions.
The study finds few differences in COVID-19 vaccination intentions across the sampled countries after controlling for individual differences, such as age and measures of altruism, as well as differences in psychological beliefs about the vaccine and disease, with one exception: those living in the United States had a significantly lower predicted vaccination uptake compared with those living in the four other countries surveyed, despite having the highest number of deaths from COVID-19. Our findings indicate little difference in vaccine intentions among individuals living in countries that have successfully mitigated the spread of the disease, such as Australia and New Zealand, compared with individuals living in other countries struggling to contain the pandemic, particularly those living in England. The model indicates that an individual’s vaccination intentions are largely made irrespective of macro-context reflected in the current or previous rates of COVID-19 infection that they experience, but instead falls to an assessment of the severity and risk of the diseases’ potential to affect themselves and their community.
Finally, the model reveals that some of the effects of variables predicting dimensions of the vaccine hesitancy model and health beliefs model are significantly amplified or reduced in some countries, as noted in the detection of significant moderating effects of country level indicators. In particular, the results indicate that for those living in the United States with stronger perceptions relating to the threat of COVID-19 for others, vaccine effectiveness for individuals, and weaker perceptions about the availability and side effects of the vaccine are more likely to hold stronger intentions to vaccinate than those with the same perceptions residing in other countries. Among Canadians, perceptions relating to disease severity (for others) and vaccine effectiveness had a weaker effect on vaccination intentions, whilst among Australians the role of perceived risk of infection (for others) similarly had a weaker effect on vaccination intentions relative to its estimated effect in other countries. There were no moderating effects by country relating to perception of infection risk for individuals, ability to free ride, conspiracy beliefs, effectiveness of vaccination for others or trust in government on vaccination intentions. The presence or absence of moderating effects, however, differs from the findings found in relation to how countries differ significantly in the extent to which these perceptions are held in their communities. As noted in Table 4, Table 5, Australians, on average, tend to be in more agreement about the severity and risks of the disease, as well as the effectiveness, availability, and minimal side effects of COVID-19 vaccinations, whilst the United States tend to be hold perceptions that are in stark contrast about the risks of the disease and benefits of vaccination. In turn, the results indicate that some countries will face stronger forms of resistance to vaccine uptake than others given the significant differences in perceptions that exist and their role as barriers to vaccination intentions.
6.1. Limitations and future research
Several additional factors could be explored to improve our model of vaccine uptake. For example, the model overlooks questions relating to vaccine delivery. Vaccination delivery predominantly occurs via an oral tablet or by injection, the latter being the only form of COVID-19 vaccination delivery currently available. Much of the population has an aversion to injections. For parents, observing their own child’s fear of needles or pain following vaccination can be most disturbing [16]. In other research, subjects evaluating hypothetical COVID-19 vaccination options showed a significant preference for oral vaccination as compared to injection [49]. In turn, the model of COVID-19 vaccination may require adjustment if oral vaccination options become available.
Our research also is silent on parent decisions about vaccination for their children, although households with dependent children were shown to have lower, but not significant differences in predicted rates of COVID-19 vaccination uptake. Nonetheless, parents may make different COVID-19 vaccination decisions for themselves compared to their children, such as a greater emphasis on side effects as shown in previous research [16], [25]. In turn, future research to understand how the model performs or requires adaptation to understand decisions by parents to vaccinate their child against COVID-19 would be beneficial.
Even within the same population, factors affecting vaccination can vary over time. Vaccination against COVID-19 remains in its infancy so perceptions around effectiveness, side effects, availability, and trust are likely to alter in the future as more robust evidence on such dimensions becomes available. In other research, for example, van der Weerd et al. [11] found that trust in the government was high, but decreased over time, whilst perceived levels of vulnerability and intention to adopt protective measures increased. As noted, the Australian sample was skewed to be over-representative of older Australians. Hence, whilst the present study considers differences across several Western nations and accounts for the distribution of various control factors (e.g., age; gender) in the model, it is limited by being cross-sectional in its design and inability to comment on experiences from many other countries. As such, generalizability of the findings offered in this study is encouraged for future research.
A major limitation of the present study is that vaccination intentions were measured as a self-reported assessment rather than an objective observation of vaccination behavior. Presently, no such data on vaccination behavior exists in relation to COVID-19 for countries where vaccination programs are in their early stages or remain at low levels. As such, our empirical results present important insights into the factors and individual characteristics driving vaccination intentions in the event of other data being presently unavailable. In addition, as the research is conducted in the context of COVID-19, it would be worthwhile to examine the conceptual framework, as well as the reliability and validity of scales employed, in understanding drivers of vaccination intentions in other contexts, such as hepatitis B, HPV, chickenpox, and pneumococcal disease [4], [50].
7. Conclusion
The COVID-19 pandemic continues as a global crisis with enormous social and economic costs, with successful vaccination programs foreseen as one of the most important long-term tools for countries around the world to navigate the crisis [1]. Our research demonstrates that COVID-19 vaccination intentions are influenced by the trust they place in the approval of the vaccine and its effectiveness for themselves, but are also highly influenced by an individual’s assessment of the effectiveness of vaccination and threats pertaining to others in the community. It also indicates that various cohorts based on age, employment, and flu vaccination uptake, will differ in their participation in a COVID-19 vaccination program. The results also show rates of intentions for vaccination uptake, as well as the levels and effects of various drivers of uptake significantly differ across the countries sampled. This was found to be particularly true of results relating to the United States. Such findings offer a critical understanding for those working on related problems of vaccination coverage from both a theoretical and practice perspective, but particularly for those challenged with implementing one of the most important vaccination programs in human history.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
For further information about QoR and its panel see https://www.qor.com.au/copy-of-contact.
We thank an anonymous reviewer for suggesting this interpretation of the result.
References
- 1.Kochhar S., Salmon D.A. Planning for COVID-19 vaccines safety surveillance. Vaccine. 2020;38(40):6194–6198. doi: 10.1016/j.vaccine.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dubé E., Vivion M., MacDonald N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Exp Revew Vacc. 2015;14(1):99–117. doi: 10.1586/14760584.2015.964212. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Report of the SAGE working Group on vaccine hesitancy; 2014. http://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf.
- 4.Larson H.J., Jarrett C., Schulz W.S., Chaudhuri M., Zhou Y., Dube E., et al. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33(34):4165–4175. doi: 10.1016/j.vaccine.2015.04.037. [DOI] [PubMed] [Google Scholar]
- 5.Hochbaum G.M. US Department of Health, Education, and Welfare, Public Health Service, Bureau of State Services, Division of Special Health Services, Tuberculosis Program; 1958. Public participation in medical screening programs: A socio-psychological study. [Google Scholar]
- 6.Janz N.K., Becker M.H. The health belief model: A decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 7.Bedford H., Attwell K., Danchin M., Marshall H., Corben P., Leask J. Vaccine hesitancy, refusal and access barriers: The need for clarity in terminology. Vaccine. 2018;36(44):6556–6558. doi: 10.1016/j.vaccine.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Thomson A., Robinson K., Vallée-Tourangeau G. The 5As: A practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016;34(8):1018–1024. doi: 10.1016/j.vaccine.2015.11.065. [DOI] [PubMed] [Google Scholar]
- 9.Dubov A., Phung C. Nudges or mandates? The ethics of mandatory flu vaccination. Vaccine. 2015;33(22):2530–2535. doi: 10.1016/j.vaccine.2015.03.048. [DOI] [PubMed] [Google Scholar]
- 10.Alexandrova R., Beykov P., Vassilev D., Jukić M., Podlipnik Č. The virus that shook the world: questions and answers about SARS-CoV-2 and COVID-19. Biotechnol Biotechnol Equip. 2021;35(1):74–102. [Google Scholar]
- 11.van der Weerd W., Timmermans D.R., Beaujean D.J., Oudhoff J., van Steenbergen J.E. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in the Netherlands. BMC Public Health. 2011 Dec 1;11(1):575. doi: 10.1186/1471-2458-11-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paulussen T.G.W., Hoekstra F., Lanting C.I., et al. Determinants of Dutch parents’ decision to vaccinate their child. Vaccine. 2006;24:644–651. doi: 10.1016/j.vaccine.2005.08.053. [DOI] [PubMed] [Google Scholar]
- 13.Downs J.S., de Bruin W.B., Fischhoff B. Parents’ vaccination comprehension and decisions. Vaccine. 2008;26(12):1595–1607. doi: 10.1016/j.vaccine.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 14.Gellin B.G., Maibach E.W., Marcuse E.K. Do parents understand immunizations? A national telephone survey. Pediatrics. 2000;106(5):1097–1102. doi: 10.1542/peds.106.5.1097. [DOI] [PubMed] [Google Scholar]
- 15.Barton B.L., Burke P.F., Waller D.S. Effects of anxiety on preferences for generic medicines in Australia. Health Promot Int. 2020 doi: 10.1093/heapro/daaa034. [DOI] [PubMed] [Google Scholar]
- 16.Salmon D.A., Dudley M.Z., Glanz J.M., Omer S.B. Vaccine hesitancy: causes, consequences, and a call to action. Vaccine. 2015 Nov;27(33):D66–D71. doi: 10.1016/j.vaccine.2015.09.035. [DOI] [PubMed] [Google Scholar]
- 17.Poland G.A., Jacobson R.M. The age-old struggle against the antivaccinationists. N Engl J Med. 2011;364(2):97–99. doi: 10.1056/NEJMp1010594. [DOI] [PubMed] [Google Scholar]
- 18.Jolley D, Douglas K. The effects of anti-vaccine conspiracy theories on vaccination intentions. Available from: www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0089177 [Accessed 4 Jan 2020]. [DOI] [PMC free article] [PubMed]
- 19.Shapiro G.K., Holding A., Perez S., Amsel R., Rosberger Z. Validation of the vaccine conspiracy beliefs scale. Papillomav Res. 2016 Dec;1(2):167–172. doi: 10.1016/j.pvr.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bertin P., Nera K., Delouvée S. Conspiracy Beliefs, Rejection of Vaccination, and Support for hydroxychloroquine: A Conceptual Replication-Extension in the COVID-19 Pandemic Context. Front Psychol. 2020 Sep;18(11):2471. doi: 10.3389/fpsyg.2020.565128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liao Q., Ng T.W.Y., Cowling B.J. What influenza vaccination programmes are preferred by healthcare personnel? A discrete choice experiment. Vaccine. 2020;38(29):4557–4563. doi: 10.1016/j.vaccine.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith P.J., Humiston S.G., Parnell T., Vannice K.S., Salmon D.A. The association between intentional delay of vaccine administration and timely childhood vaccination coverage. Public Health Rep. 2010;125(4):534–541. doi: 10.1177/003335491012500408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sun X., Wagner A.L., Ji J., Huang Z., Zikmund-Fisher B.J., Boulton M.L., et al. A conjoint analysis of stated vaccine preferences in Shanghai. Vaccine. 2020;38(6):1520–1525. doi: 10.1016/j.vaccine.2019.11.062. [DOI] [PubMed] [Google Scholar]
- 24.Guo N.a., Zhang G., Zhu D., Wang J., Shi L. The effects of convenience and quality on the demand for vaccination: Results from a discrete choice experiment. Vaccine. 2017;35(21):2848–2854. doi: 10.1016/j.vaccine.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 25.Verelst F., Kessels R., Delva W., Beutels P., Willem L. Drivers of vaccine decision-making in South Africa: a discrete choice experiment. Vaccine. 2019;37(15):2079–2089. doi: 10.1016/j.vaccine.2019.02.056. [DOI] [PubMed] [Google Scholar]
- 26.Hershey J.C., Asch D.A., Thumasathit T., Meszaros J., Waters V.V. The roles of altruism, free riding, and bandwagoning in vaccination decisions. Organ Behav Hum Decis Process. 1994;59(2):177–187. [Google Scholar]
- 27.Vetter P., Vu D.L., L'Huillier A.G., Schibler M., Kaiser L., Jacquerioz F. Clinical features of covid-19. BMJ. 2020;369 doi: 10.1136/bmj.m1470. [DOI] [PubMed] [Google Scholar]
- 28.Larson H.J., de Figueiredo A., Xiahong Z., Schulz W.S., Verger P., Johnston I.G., et al. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grabenstein J.D. What the world's religions teach, applied to vaccines and immune globulins. Vaccine. 2013;31(16):2011–2023. doi: 10.1016/j.vaccine.2013.02.026. [DOI] [PubMed] [Google Scholar]
- 30.Fishbein M., Ajzen I. Addison-Wesley; New York: 1975. Attitude, intention and behavior. [Google Scholar]
- 31.Schlegel R.P., DAvernas J.R., Zanna M.P., DeCourville N.H., Manske S.R. Problem drinking: A problem for the Theory of Reasoned Action? 1. J Appl Soc Psychol. 1992;22(5):358–385. [Google Scholar]
- 32.Godin Gaston, Valois Pierre, Lepage Linda, Desharnais Raymond. Predictors of smoking behaviour: an application of Ajzen's theory of planned behaviour. Br J Addict. 1992;87(9):1335–1343. doi: 10.1111/j.1360-0443.1992.tb02742.x. [DOI] [PubMed] [Google Scholar]
- 33.Gerend M.A., Shepherd J.E. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med. 2012;44(2):171–180. doi: 10.1007/s12160-012-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wu A.M.S., Lau J.T.F., Ma Y.-L., Cheng K.-M., Lau M.M.C. A longitudinal study using parental cognitions based on the theory of planned behavior to predict childhood influenza vaccination. J Infect Public Health. 2020;13(7):970–979. doi: 10.1016/j.jiph.2020.04.009. [DOI] [PubMed] [Google Scholar]
- 35.Corace K., Prematunge C., McCarthy A., Nair R.C., Roth V., Hayes T., et al. Predicting influenza vaccination uptake among health care workers: what are the key motivators? Am J Infect Control. 2013;41(8):679–684. doi: 10.1016/j.ajic.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 36.Santos A.J., Kislaya I., Machado A., Nunes B. Beliefs and attitudes towards the influenza vaccine in high-risk individuals. Epidemiol Infect. 2017;145(9):1786–1796. doi: 10.1017/S0950268817000814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adams A., Hall M., Fulghum J. Utilizing the health belief model to assess vaccine acceptance of patients on hemodialysis. Nephrol Nurs J. 2014;41(4) [PubMed] [Google Scholar]
- 38.Coe A.B., Gatewood S.B.S., Moczygemba L.R., Goode J.-V. The use of the health belief model to assess predictors of intent to receive the novel (2009) H1N1 influenza vaccine. Innovat Pharm. 2012 Jan 1;3(2) doi: 10.24926/iip.v3i2.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wong L.P., Alias H., Wong P.-F., Lee H.Y., AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Human Vacc Immunotherap. 2020;16(9):2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shapiro G.K., Tatar O., Dube E., Amsel R., Knauper B., Naz A., et al. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine. 2018;36(5):660–667. doi: 10.1016/j.vaccine.2017.12.043. [DOI] [PubMed] [Google Scholar]
- 41.Siegrist M., Earle T.C., Gutscher H. Test of a trust and confidence model in the applied context of electromagnetic field (EMF) risks. Risk Anal Int J. 2003;23(4):705–716. doi: 10.1111/1539-6924.00349. [DOI] [PubMed] [Google Scholar]
- 42.Fornell C., Larcker D.F. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18(1):39–50. [Google Scholar]
- 43.Hu L.-T., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Eq Model Multidiscip J. 1999;6(1):1–55. [Google Scholar]
- 44.Philip R.K., Shapiro M., Paterson P., Glismann S., Van Damme P. Is it time for vaccination to “Go Viral”? Pediatr Infect Dis J. 2016 Dec 1;35(12):1343–1349. doi: 10.1097/INF.0000000000001321. [DOI] [PubMed] [Google Scholar]
- 45.French J., Deshpande S., Evans W., Obregon R. Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. Int J Environ Res Public Health. 2020 Jan;17(16):5893. doi: 10.3390/ijerph17165893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Spence M. Competitive and optimal responses to signals: An analysis of efficiency and distribution. J Econ Theory. 1974;7(3):296–332. [Google Scholar]
- 47.Mitchell Irwin. No vaccine, no job? Can employers insist their staff take the Covid-19 vaccine? Lexology, January 19, 2021. Accessed February 1st 2021 from: https://www.lexology.com/library/detail.aspx?g=ea9f03de-9ec3-410b-a020-29d248e154ab.
- 48.Burke P.F. Seeking simplicity in complexity: The relative value of ease of use (EOU)-based product differentiation. J Prod Innov Manage. 2013;30(6):1227–1241. [Google Scholar]
- 49.Borriello A., Master D., Pellegrini A., Rose J.M. Preferences for a COVID-19 vaccine in Australia. Vaccine. 2021;39(3):473–479. doi: 10.1016/j.vaccine.2020.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Glanz J.M., McClure D.L., O’Leary S.T., Narwaney K.J., Magid D.J., Daley M.F., et al. Parental decline of pneumococcal vaccination and risk of pneumococcal related disease in children. Vaccine. 2011;29(5):994–999. doi: 10.1016/j.vaccine.2010.11.085. [DOI] [PMC free article] [PubMed] [Google Scholar]