Abstract
Once COVID-19 vaccines are approved for children < 12 years of age, high pediatric vaccination coverage will be needed to help minimize the public health threat from the SARS-CoV-2 epidemic. We conducted an online survey of 1,119 parents and caregivers of children ≤ 12 years in New York City from March 9 to April 11, 2021. Among parents surveyed, 61.9% reported plans to vaccinate their youngest child for COVID-19, 14.8% said they do not plan to vaccinate their child and 23.3% were unsure. Female and non-Hispanic Black parents were least likely to report plans to vaccinate their children. Safety, effectiveness and perceptions that children do not need vaccination were the primary reasons for vaccine hesitancy/resistance. Parents who have or will vaccinate themselves were significantly more likely to report they would vaccinate their children. Efforts to increase awareness about vaccine safety and education about the importance of vaccinating children are needed.
1. Introduction
As of July 2021, vaccines to prevent SARs-COV-2 infection (COVID-19) have not yet been approved for use in children younger than 12 years of age in the United States (US). Clinical trials in younger pediatric populations are underway and approval for vaccines in children<12 years is expected before the end of 2021 [1]. Once COVID-19 vaccination is available for children, acceptability among parents will be critical for protecting them from infection and for mitigating the public health threat posed by COVID-19 [2].
While children may be a lower risk for infection and severe disease [2], over 4 million children in the US have been diagnosed with COVID-19 since the start of the epidemic and more than 300 have died [3]. In addition, some infected children have serious complications, including multi‐inflammatory syndrome in children (MIS‐C), and they also experience long-COVID with persistent symptoms similar to adults [4], [5].
Preventing COVID-19 in children is of critical importance not only for the individual health benefits but also because it will contribute to stopping the spread of infections in communities and households. Although children appear to be less susceptible to infection and to play a smaller role than teenagers and adults in transmission,[2] outbreaks have been reported from schools and daycare facilities[6], [7] and age-appropriate social distancing measures continue to be recommended for children.[8] High coverage of COVID-19 vaccination among children will help stop transmission and will allow for safe return to normal activities, including fully opening schools.[9]
Whether parents of children < 12 years will accept COVID-19 vaccination for their children remains an important question. Since the approval in early May 2021 of COVID-19 vaccines for adolescents 12–15 years, only 24.9% of that age group had been vaccinated as of July 2021.[10] Overcoming vaccine hesitancy among parents will be a critical issue for ensuring high uptake of vaccination coverage. Vaccine hesitancy or the delayed acceptance or refusal to vaccinate is complex, may vary over time, particularly for parents depending on the age of their child, and is often connected with misunderstandings about vaccine safety and efficacy.[11], [12] Prior to the COVID-19 epidemic, a study of vaccine hesitancy found that 6.1% of US parents reported vaccine hesitancy for routine childhood immunizations and 25.8% for influenza vaccines.[13] Given this evidence, it is important to understand whether parents will be likely to accept COVID-19 vaccination for children when approved.
New York City (NYC) was the epicenter of the US COVID-19 epidemic and continues to have high levels of community transmission.[10] It is the most densely populated city in the US and also one of the most racially and ethnicity diverse. Since the start of the epidemic, more than 87,000 children in NYC have been diagnosed with COVID-19[3] and, in an analysis of NYC testing data, school aged children 5–14 years who were tested for SARS-CoV-2 had the highest sero-prevalence of any age group.[14] We surveyed NYC parents and caregivers of children ≤ 12 years of age to measure intentions to vaccinate children against COVID-19.
2. Methods
We conducted an online non-probability survey of English and Spanish speaking parents and caregivers (‘parents’) in NYC to measure intentions to vaccinate their youngest child when a pediatric COVID-19 vaccine is available (n = 1,119). Eligible participants were adults ≥ 18 years who identified as primary caregivers of a child ≤ 12 years of age. Recruitment was conducted through a Qualtrics panel with data collected from March 9 through April 11, 2021. We followed the American Association for Public Opinion Research (AAPOR) guidelines for quota-based sampling[15] and used 2019 Census data for NYC to calculate survey weights based on race, ethnicity, sex, education and borough.[16] The protocol was approved by the CUNY School of Public Health and Health Policy institutional review board.
The study outcome was the proportion of parents reporting intentions to vaccinate the youngest child in their household against COVID-19. Parents were asked “when a vaccine to prevent COVID-19 is approved for children, would you want your child to receive the vaccine” (responses: “yes”, “no”, “unsure”). Parents responding “no” or “unsure” were considered vaccine hesitant/resistant and were asked, “why do you not want your child to receive the COVID-19 vaccine?” with multiple response options. Parents reported demographics and household characteristics, and whether they had received or planned to get the COVID-19 vaccine themselves (response options included already received COVID-19 vaccination, plan to receive when available, unsure, will not get the vaccine and prefer not to answer).
Survey weights were applied to all analyses to generate prevalence estimates. Descriptive statistics (unweighted counts and weighted percentages) are presented for the sample. Prevalence of parental plans to vaccinate children (yes, no, unsure) were compared by sample characteristics using Rao adjusted Pearson chi-squared tests. Poisson regression models with robust standard errors were fitted to estimate prevalence ratios (PR) and confidence intervals (CI) comparing parents planning to vaccinate to those responding “no” or “unsure” (combined); models were adjusted for demographic and household characteristics. Parents’ own COVID-19 vaccination status was examined by grouping together parents who responded that they had already been vaccinated with those who planned to get the vaccine, and those responding that they were unsure or preferred not to answer (parents reporting they would not get vaccinated were examined as their own group). We measured the association between parental vaccine status with reported intentions to vaccinate children using Rao adjusted Pearson chi-squared tests to compare proportions. Analyses were conducted in SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
3. Results
Among NYC parents, 61.9% reported intentions to vaccinate their youngest child against COVID-19 (median child age: 4.7 years), 14.8% said they will not vaccinate their child and 23.3% were unsure (Table 1 ). The most commonly cited concerns among vaccine hesitant parents (those reporting they would not vaccinate their child or were unsure) were safety and effectiveness which was reported by 81.2%, and there were significant differences by race/ethnicity. Whereas 88.4% of Hispanic parents, 85.1% of non-Hispanic Black parents and 82.3% of Asian parents who were vaccine hesitant reported safety and effectiveness concerns, only 60.7% of non-Hispanic white vaccine-hesitant parents reported this concern (p = 0.01). In addition to safety concerns, 21.7% of vaccine hesitant parents reported that they believe children are at low risk for COVID-19 and don’t need vaccination; 16.6% and 9.5% of vaccine hesitant parents reported medical and religious or philosophical reasons, respectively, and 2.7% reported ‘other’ reasons.
Table 1.
Intentions among NYC parents to vaccinate children ≤ 12 years against COVID-19 according to parent and child characteristics – March 9-April 11, 2021.
| When a COVID-19 vaccine available for children, will you want your child to be vaccinated |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NYC sample |
Yes |
No |
Unsure |
p-valueŦ | Adjusted prevalence ratios |
|||||||
| Characteristics | N | %* | %^ | 95% CI | % | 95% CI | % | 95% CI | aPR | 95 %CI | p-value | |
| Total sample | 1119 | 100.0 | 61.9 | 56.6–67.1 | 14.8 | 11.1–18.6 | 23.3 | 18.4–28.3 | ||||
| Child age | ||||||||||||
| Median age, years (IQR) | 4.7 (2.0–8.5) | 4.9 (2.2–8.5) | 5.6 (2.1–8.6) | 3.5 (1.4–8.2) | <0.01 | |||||||
| <24 months | 195 | 18.4 | 55.4 | 41.0–69.7 | 14.8 | 4.4–25.3 | 29.8 | 14.6–45.0 | 0.59 | 1.00 | ref | – |
| 2–6 years | 460 | 41.1 | 64.2 | 56.5–71.8 | 12.5 | 7.8–17.1 | 23.3 | 16.1–30.6 | 1.04 | 0.82–1.31 | 0.76 | |
| 7–12 years | 464 | 40.5 | 62.4 | 54.8–70.1 | 17.2 | 10.9–23.5 | 20.4 | 13.8–27.0 | 1.03 | 0.81–1.30 | 0.81 | |
| Child sex | ||||||||||||
| Male | 558 | 50.8 | 62.8 | 54.8–70.9 | 12.4 | 6.6–18.1 | 24.8 | 17.2–32.4 | 0.09 | 1.00 | ref | – |
| Female | 555 | 48.7 | 61.6 | 54.7–68.4 | 17.1 | 12.2–22.0 | 21.4 | 14.9–27.9 | 0.99 | 0.87–1.14 | 0.93 | |
| Missing§ | 6 | 0.5 | ||||||||||
| Child race/ethnicity** | ||||||||||||
| Non-Hispanic Black | 162 | 18.4 | 45.8 | 36.2–55.4 | 23.2 | 15.7–30.8 | 31.0 | 22.3–39.7 | <0.01 | |||
| Asian | 100 | 12.8 | 67.9 | 55.8–80.0 | 5.0 | 0.9–9.1 | 27.1 | 15.2–39.0 | ||||
| Non-Hispanic White | 517 | 31.7 | 86.6 | 82.5–90.8 | 7.2 | 4.4–10.1 | 6.1 | 2.8–9.4 | ||||
| Hispanic | 294 | 29.3 | 44.8 | 32.1–57.4 | 19.6 | 9.5–29.8 | 35.6 | 22.5–48.8 | ||||
| Non-Hispanic Other § | 46 | 7.6 | ||||||||||
| Parent age | ||||||||||||
| 18–29 years | 165 | 23.2 | 40.9 | 28.0–53.9 | 19.0 | 7.5–30.5 | 40.1 | 25.5–54.6 | <0.01 | 0.87 | 0.61–1.24 | 0.44 |
| 30–44 years | 830 | 67.4 | 69.1 | 63.9–74.2 | 12.7 | 9.2–16.3 | 18.2 | 13.7–22.7 | 1.01 | 0.81–1.26 | 0.94 | |
| 45 + years | 124 | 9.4 | 61.7 | 48.7–74.6 | 19.4 | 8.5–30.3 | 19.0 | 9.2–28.7 | 1.00 | ref | – | |
| Parent sex | ||||||||||||
| Male | 626 | 40.7 | 83.3 | 78.3–88.2 | 6.6 | 3.8–9.5 | 10.1 | 5.8–14.5 | <0.01 | 1.00 | ref | – |
| Female | 490 | 59.0 | 47.2 | 39.8–54.7 | 20.4 | 14.4–26.3 | 32.4 | 24.9–39.9 | 0.72 | 0.61–0.85 | <0.0001 | |
| Transgender/other§# | 3 | 0.3 | ||||||||||
| Parent race/ethnicity | ||||||||||||
| Non-Hispanic Black | 176 | 20.9 | 47.3 | 38.2–56.4 | 23.4 | 16.1–30.8 | 29.3 | 21.2–37.3 | <0.01 | 0.79 | 0.63–0.99 | 0.04 |
| Asian | 113 | 14.2 | 67.4 | 56.1–78.8 | 5.0 | 1.2–8.9 | 27.5 | 16.3–38.7 | 1.05 | 0.84–1.32 | 0.66 | |
| Non-Hispanic White | 510 | 31.1 | 86.2 | 82.0–90.4 | 7.6 | 4.7–10.5 | 6.2 | 2.9–9.6 | 1.00 | ref | – | |
| Hispanic | 292 | 29.2 | 47.0 | 33.8–60.2 | 19.2 | 9.0–29.4 | 33.8 | 20.4–47.2 | 0.80 | 0.61–1.05 | 0.10 | |
| Non-Hispanic Other | 28 | 4.7 | 40.7 | 16.8–64.6 | 26.7 | 3.5–50.0 | 32.6 | 11.2–53.9 | 0.72 | 0.41–1.26 | 0.25 | |
| Child has health insurance | ||||||||||||
| Yes | 1018 | 91.3 | 61.0 | 55.5–66.6 | 15.2 | 11.2–19.2 | 23.8 | 18.5–29.1 | 0.14 | 0.99 | 0.81–1.20 | 0.90 |
| No | 89 | 6.3 | 78.5 | 67.3–89.7 | 11.6 | 2.8–20.5 | 9.9 | 2.0–17.7 | 1.00 | ref | – | |
| Don't know | 12 | 2.4 | ||||||||||
| Child attending in person school/daycare ≥ 1 day per week | ||||||||||||
| Yes | 628 | 50.7 | 71.5 | 64.4–78.5 | 11.8 | 7.6–16.0 | 16.7 | 10.0–23.5 | <0.01 | 1.23 | 1.05–1.45 | 0.01 |
| No | 482 | 48.3 | 52.5 | 44.9–60.1 | 18.0 | 11.7–24.2 | 29.5 | 22.2–36.9 | 1.00 | ref | – | |
| Don't know§ | 9 | 1.0 | ||||||||||
| Number of children ≤ 12 years in household | ||||||||||||
| 1 | 514 | 49.4 | 55.8 | 48.6–62.9 | 14.4 | 10.0–18.8 | 29.8 | 22.7–36.9 | 0.07 | 1.00 | ref | – |
| 2 | 494 | 40.2 | 70.0 | 61.2–78.8 | 13.6 | 7.4–19.8 | 16.4 | 8.2–24.7 | 1.06 | 0.89–1.26 | 0.50 | |
| 3 or more | 111 | 10.4 | 59.3 | 42.1–76.4 | 21.4 | 5.0–37.9 | 19.3 | 8.6–29.9 | 1.04 | 0.77–1.42 | 0.80 | |
| Parent education (highest completed) | ||||||||||||
| High school or less | 145 | 30.0 | 46.9 | 34.6–59.2 | 19.2 | 9.5–29.0 | 33.9 | 21.4–46.3 | <0.01 | 0.90 | 0.69–1.16 | 0.40 |
| Some college/tech school | 193 | 30.3 | 57.6 | 47.9–67.2 | 15.1 | 8.4–21.8 | 27.4 | 18.3–36.4 | 0.94 | 0.81–1.10 | 0.80 | |
| Completed college or more | 761 | 38.4 | 76.1 | 72.2–80.1 | 11.4 | 8.5–14.3 | 12.5 | 9.4–15.6 | 1.00 | ref | – | |
| Missing§ | 20 | 1.4 | ||||||||||
| Household income (USD) | ||||||||||||
| <$25,000 | 106 | 15.1 | 52.0 | 36.8–67.2 | 16.7 | 8.7–24.6 | 31.3 | 16.8–45.9 | <0.01 | 0.74 | 0.53–1.03 | 0.08 |
| $25,000-$49,999 | 157 | 20.8 | 38.3 | 26.0–50.7 | 22.3 | 11.0–33.7 | 39.4 | 25.2–53.5 | 0.98 | 0.86–1.13 | 0.82 | |
| $50,000-$99,999 | 275 | 26.8 | 62.5 | 52.2–72.8 | 15.2 | 7.0–23.3 | 22.3 | 13.3–31.3 | 1.13 | 0.80–1.60 | 0.48 | |
| ≥$100,000 | 554 | 31.7 | 82.1 | 77.3–86.8 | 8.9 | 4.8–13.1 | 9.0 | 6.0–12.1 | 1.00 | ref | – | |
| Missing§ | 27 | 5.6 | ||||||||||
| NYC borough | ||||||||||||
| Bronx | 278 | 13.7 | 48.3 | 38.6–57.9 | 21.9 | 14.3–29.4 | 29.9 | 20.4–39.3 | <0.01 | 0.84 | 0.66–1.06 | 0.14 |
| Brooklyn | 360 | 31.7 | 63.1 | 55.1–71.1 | 17.6 | 11.2–24.0 | 19.3 | 12.3–26.3 | 0.92 | 0.79–1.06 | 0.26 | |
| Manhattan | 240 | 14.9 | 83.7 | 75.4–92.1 | 5.1 | 1.0–9.1 | 11.2 | 3.4–18.9 | 1.00 | ref | – | |
| Staten Island | 46 | 8.0 | 57.6 | 32.4–82.9 | 7.3 | 0.4–14.1 | 35.1 | 8.4–61.8 | 0.85 | 0.60–1.21 | 0.36 | |
| Queens | 195 | 31.6 | 57.3 | 46.1–68.5 | 15.4 | 6.6–24.2 | 27.3 | 16.9–37.7 | 1.01 | 0.81–1.25 | 0.95 | |
Abbreviations: CI = confidence interval; IQR = interquartile range; USD = US dollars.
*Survey weights applied to sample to represent NYC population of parents by race, ethnicity, sex, education and region.
^Weighted percentages are prevalence estimates of NYC parents reporting vaccination plans for their youngest child.
Ŧp-values from Rao adjusted Pearson Chi-squared tests to compare expected to observed frequencies among groups by characteristic for parent’s willingness to vaccinate their youngest child (i.e. whether willing to vaccinate youngest child differed by sex of the child, etc.).
§Categories are not presented in the table as they yielded unreliable standard error estimates.
**Child’s race/ethnicity excluded from adjusted models due to collinearity with parent’s race/ethnicity.
#Parents identifying as transgender were grouped according to their identified gender.
In adjusted models, parents of children attending in-person school or daycare were more likely to report intentions to vaccinate (aPR: 1.23;95% confidence interval (CI): 1.05–1.45) (Table 1). Female (aPR: 0.72;95% CI: 0.61–0.85) and non-Hispanic Black parents (aPR: 0.79, 95 %CI: 0.63–0.99) were less likely to report plans to vaccinate their children.
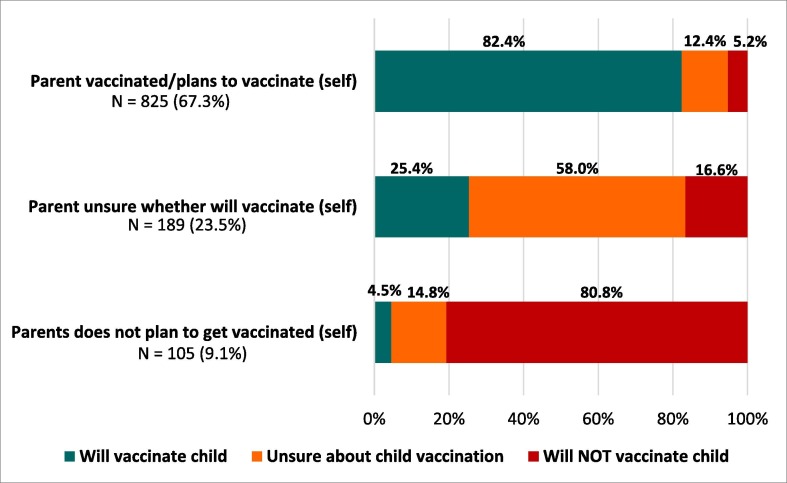
Among parents, 20.2% had received and 47.1% planned to receive COVID-19 vaccination themselves, 20.6% were unsure, 9.1% reported not planning to receive it and 3.0% declined to answer. Most parents (82.4%) who had been or planned to be vaccinated themselves reported plans to vaccine their youngest child, whereas among parent who were unsure about getting vaccinated or said they did not plan to get vaccinated themselves, only 25.4% and 4.5%, respectively, planned to vaccinate their youngest child (p < 0.0001) (Fig. 1 ).
Fig. 1.
Parental intentions to vaccinate children in NYC against COVID-19 according to parents’ own vaccination status – March 9-April 11, 2021.
4. Discussion
In March 2021, approximately 60% of parents in NYC reported plans to vaccinate children ≤ 12 years against COVID-19 when vaccines are approved for pediatric populations. Among parents expressing vaccine hesitancy, the primary concerns were safety and effectiveness, particularly for non-Hispanic Black and Hispanic parents, as well as perceived lack of need. Female and non-Hispanic Black parents were least likely to report intending to vaccinate their children, and we observed a strong correlation between parental willingness to get vaccinated and reported intentions to vaccinate children. Among NYC parents, 67% reported they had been vaccinated or planned to get vaccinated themselves.
Willingness of parents to vaccinate children when a COVID-19 vaccine is approved for pediatric populations will be crucial for protecting pediatric populations, their communities and households from infection. While trials in younger children have not yet been completed, studies in young adolescents (12–15 years) have shown up to 100% efficacy suggesting that the vaccine will be highly effective.[17] High uptake of efficacious vaccines in pediatric populations may also contribute to lower infections in adults and will help stop community spread, as has been observed with other illnesses.[2] Decreasing risk of infections in children and curtailing transmission of COVID-19, will also have the added benefit of allowing children to return to normal activities, including school and other services and programs, which have been limited during the epidemic causing significant harm to children and parents.[18]
Our findings indicate that while a majority of NYC parents intend to vaccinate their children for COVID-19, roughly 40% will not or are unsure. In order to achieve herd immunity and stop the spread of COVID-19, it is estimated that up to 70% of the population may need to be vaccinated, including children.[19] If vaccine acceptability does not improve, herd immunity may not be reached and COVID-19 may continue circulating among the unvaccinated. In our survey, we found that the most commonly held concerns reported by parents for not wanting to vaccinate their child were safety and efficacy, followed by a perceived lack of need for vaccination of children.
While previous studies of vaccine hesitancy among US parents have found safety to be the most predominant concern[13], [20], a 2019 study found that another reason many parents refuse influenza vaccine for children is lack of agreement that the vaccine is effective.[13] Data from our study suggest that many parents who expressed hesitancy to vaccinate their children for COVID-19 may in part believe that it is unnecessary to protect children from infection and that children are at low risk of severe COVID-19 disease. However, the long-term sequelae of even mild COVID-19 are still being investigated and understood. As with adults with milder illness, children who get SARS-CoV-2 infection may be at increased risk for long-COVID.[5] These findings suggest that greater efforts are needed to help parents understand that vaccines are safe and important for protecting children from COVID-19.
We also identified that female parents and non-Hispanic Black parents in NYC were more likely to report vaccine hesitancy. In a survey conducted across the US at the same time, we had a similar finding, that female parents expressed more hesitancy about COVID-19 vaccination for children compared to male parents.[21] These findings are consistent with surveys asking adults about their own vaccine intentions conducted in 2020, in which women and Black adults in the US were more likely to report vaccine hesitancy compared to other groups.[22], [23] We did not find that lower income and less education were associated with greater vaccine hesitancy among parents in NYC which is somewhat different from our national survey results, and also different from studies of general vaccine hesitancy measured prior to the epidemic.[21], [24] Greater attempts should be undertaken to understand the concerns of mothers and of non-Hispanic Black parents to inform and improve strategies for providing targeted information about the safety and benefits of vaccination to these groups.
Planning for pediatric COVID-19 vaccination roll-out should include strategies to address vaccine hesitancy including public health campaigns to counter misinformation about safety and to provide messaging about the effectiveness and importance of vaccinating children. Another approach that may improve coverage and decrease vaccine hesitancy is distribution of COVID-19 vaccination for children not only through mass vaccination sites but also through pediatricians’ offices as part of primary care. In addition to making vaccines more accessible for parents, previous research has shown high levels of trust between parents and pediatricians [20] who may be able to increase uptake among vaccine hesitant parents.
Our study was unique in examining the concordance between parents’ vaccine intentions for themselves and for their child. We found high agreement showing that parents who do not want to get vaccinated themselves will also likely not vaccinate their children, and that parents who are unsure about getting vaccinated are also unsure about the vaccine for their children. We do not know from our data whether these findings indicate that shifts in parents’ willingness to get vaccinated themselves will lead to acceptance of vaccination for children. Further studies are needed to better understand this finding. This study was limited to parents in NYC and to children ≤ 12 years and may not be generalizable to other areas or adolescents. Data were self-reported and subject to response bias, and our survey was conducted online, excluding parents without internet access.
5. Conclusions
Our study provides important information about parental acceptability of the COVID-19 vaccine for children in the most densely populated and one of the most racially and ethnically diverse cities in the US. Our findings also suggest that pediatric vaccine hesitancy is strongly tied to parental vaccine hesitancy. Targeted interventions are needed to increase uptake of COVID-19 vaccines for children, including educating parents on the safety and importance of COVID-19 vaccination for children.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Centers for Disease Control and Prevention (CDC). Summary Document for Interim Clinical Considerations for use of COVID-19 Vaccines Currently Authorized in the United States. https://www.cdc.gov/vaccines/covid-19/info-by-product/clinical-considerations.html Accessed: May 21, 2021.
- 2.Kao C.M., Orenstein W.A., Anderson E.J. The Importance of Advancing Severe Acute Respiratory Syndrome Coronavirus 2 Vaccines in Children. Clin Infect Dis. 2021;72(3):515–518. doi: 10.1093/cid/ciaa712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amercian Academy of Pediatrics (AAP) and Children's Hospital Association. Children and COVID-19: State Data Report Version: July 8, 2021. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/. Accessed: July 11, 2021.
- 4.Kest H., Kaushik A., DeBruin W., Colletti M., Goldberg D. Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with 2019 Novel Coronavirus (SARS-CoV-2) Infection. Case Rep Pediatr. 2020;2020:1–4. doi: 10.1155/2020/8875987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buonsenso D., Munblit D., De Rose C., et al. Preliminary evidence on long COVID in children. Acta Paediatr. 2021 doi: 10.1111/apa.15870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doyle T., Kendrick K., Troelstrup T., Gumke M., Edwards J., Chapman S., et al. COVID-19 in Primary and Secondary School Settings During the First Semester of School Reopening - Florida, August-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(12):437–441. doi: 10.15585/mmwr.mm7012e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim C., McGee S., Khuntia S., Elnour A., Johnson-Clarke F., Mangla A., et al. Characteristics of COVID-19 Cases and Outbreaks at Child Care Facilities - District of Columbia, July-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(20):744–748. doi: 10.15585/mmwr.mm7020a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CDC. Help Stop the Spread of COVID-19 in Children. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/children/protect-children.html. Accessed May 3, 2021.
- 9.Kamidani S., Rostad C.A., Anderson E.J. COVID-19 vaccine development: a pediatric perspective. Curr Opin Pediatr. 2021;33(1):144–151. doi: 10.1097/MOP.0000000000000978. [DOI] [PubMed] [Google Scholar]
- 10.CDC. COVID Data Tracker: COVID-19 Integrated Country View. https://covid.cdc.gov/covid-data-tracker/#county-view. Accessed July 12, 2021.
- 11.MacDonald NE, Hesitancy SWGoV. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161-4164. [DOI] [PubMed]
- 12.Rosso Annalisa, Massimi Azzurra, Pitini Erica, Nardi Angelo, Baccolini Valentina, Marzuillo Carolina, et al. Factors affecting the vaccination choices of pregnant women for their children: a systematic review of the literature. Hum Vaccin Immunother. 2020;16(8):1969–1980. doi: 10.1080/21645515.2019.1698901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kempe Allison, Saville Alison W., Albertin Christina, Zimet Gregory, Breck Abigail, Helmkamp Laura, et al. Parental Hesitancy About Routine Childhood and Influenza Vaccinations: A National Survey. Pediatrics. 2020;146(1):e20193852. doi: 10.1542/peds.2019-3852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rane MS, Profeta A, Poehlein E, et al. The emergence, surge and subsequent wave of the SARS-CoV-2 pandemic in New York metropolitan area: The view from a major region-wide urgent care provider. medRxiv. 2021. https://www.medrxiv.org/content/10.1101/2021.04.06.21255009v3.full#F4. [DOI] [PMC free article] [PubMed]
- 15.American Association for Public Opinion Research (AAPOR). Standard defintions: final dispositions of case codes and outcome rates for surveys. https://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions20169theditionfinal.pdf. Accessed: January 13, 2021.
- 16.US Census Bureau (USC). Census QuickFacts (2019). Available from: https://www.census.gov/quickfacts/fact/table/US/PST045219. Accessed January 5, 2021.
- 17.Mahase E. Covid-19: Pfizer reports 100% vaccine efficacy in children aged 12 to 15. BMJ. 2021;373 doi: 10.1136/bmj.n881. [DOI] [PubMed] [Google Scholar]
- 18.Patrick SW, Henkhaus LE, Zickafoose JS, et al. Well-being of Parents and Children During the COVID-19 Pandemic: A National Survey. Pediatrics. 2020;146(4). [DOI] [PubMed]
- 19.Kwok Kin On, Lai Florence, Wei Wan In, Wong Samuel Yeung Shan, Tang Julian W.T. Herd immunity - estimating the level required to halt the COVID-19 epidemics in affected countries. J Infect. 2020;80(6):e32–e33. doi: 10.1016/j.jinf.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santibanez TA, Nguyen KH, Greby SM, et al. Parental Vaccine Hesitancy and Childhood Influenza Vaccination. Pediatrics. 2020;146(6) [DOI] [PMC free article] [PubMed]
- 21.Teasdale CA, Borrell LN, Kimball S, et al. Plans to vaccinate children for COVID-19: a survey of US parents. J Pediatr. 2021. Jul 17;S0022-346(21)00688-0.
- 22.Kreps Sarah, Prasad Sandip, Brownstein John S., Hswen Yulin, Garibaldi Brian T., Zhang Baobao, et al. Factors Associated With US Adults' Likelihood of Accepting COVID-19 Vaccination. JAMA Netw Open. 2020;3(10):e2025594. doi: 10.1001/jamanetworkopen.2020.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Latkin CA, Dayton L, Yi G, Colon B, Kong X. Mask usage, social distancing, racial, and gender correlates of COVID-19 vaccine intentions among adults in the US. PloS one. 2021;16(2):e0246970. [DOI] [PMC free article] [PubMed]
- 24.Siddiqui Mariam, Salmon Daniel A., Omer Saad B. Epidemiology of vaccine hesitancy in the United States. Hum Vaccin Immunother. 2013;9(12):2643–2648. doi: 10.4161/hv.27243. [DOI] [PMC free article] [PubMed] [Google Scholar]