Background
There are approximately 5200 community hospitals in the United States. About 1300 of them are investor-owned, for-profit hospitals whose owners are corporations, groups of physicians, or other private entities. Private equity firms use capital from individuals and institutions to invest in organizations. They are increasingly buying hospitals, which they typically plan to sell for a profit within 3 to 7 years after acquisition (1, 2). A recent study evaluated changes in hospital income, use, and quality associated with private equity acquisitions between 2005–2017 (2).
Objective
To compare acute care hospitals owned by private equity firms with similarly sized and located hospitals not owned by private equity firms.
Methods and Findings
We used merger and acquisition reports by Irving Levin Associates and public information to identify 130 hospitals under private equity control in 2018. We then identified all 2868 hospitals that had a full year of data in the 2018 Medicare Cost Report, extracted information on size (1 to 49 beds, 50 to 450 beds, and ≥451 beds), and assigned the hospitals to health care markets (hospital referral regions) using The Dartmouth Atlas of Health Care. We used health care markets and size groups to identify 688 hospitals that we could match to a private equity hospital. Within matched groups, there were 1 to 56 matched control hospitals per private equity hospital, with a median of 8 control hospitals and an interquartile range of 10. We assigned each private equity hospital a weight of 1 and assigned its matched hospitals weights that summed to 1. We used these weights in all analyses.
We compared private equity hospitals with their matched hospitals on location, financial characteristics, and patient experience. Hospital characteristics were identified from the Medicare cost report after transforming (winsorizing) values outside the 95th and 5th percentiles to limit the effect of extreme outliers (3). We used the rurality score from the Rural-Urban Commuting Areas geographic taxonomy, version 3.10, to classify ZIP codes from 1 (metropolitan) to 10 (rural). We used 2017 median household income by ZIP code from The Dartmouth Atlas of Health Care. Scores were collected from the Hospital Consumer Assessment of Healthcare Providers and Systems survey, which contains patient perspectives of their hospital experience. It has often been called a patient satisfaction score and ranges from 0 (lowest) to 100 (highest) (4).
Mean values were compared between the groups, allowing for correlation in hospital characteristics, by using a linear regression model with private equity status as the key independent variable, conditional on hospital referral region. We controlled for total hospital beds in analyses involving cost report outcomes. We clustered SEs at the hospital referral region level. For outcomes expressed in ratios, we modeled the numerator as the outcome and adjusted for the denominator by including it as an independent variable, along with hospital beds and hospital referral region (5).
Results
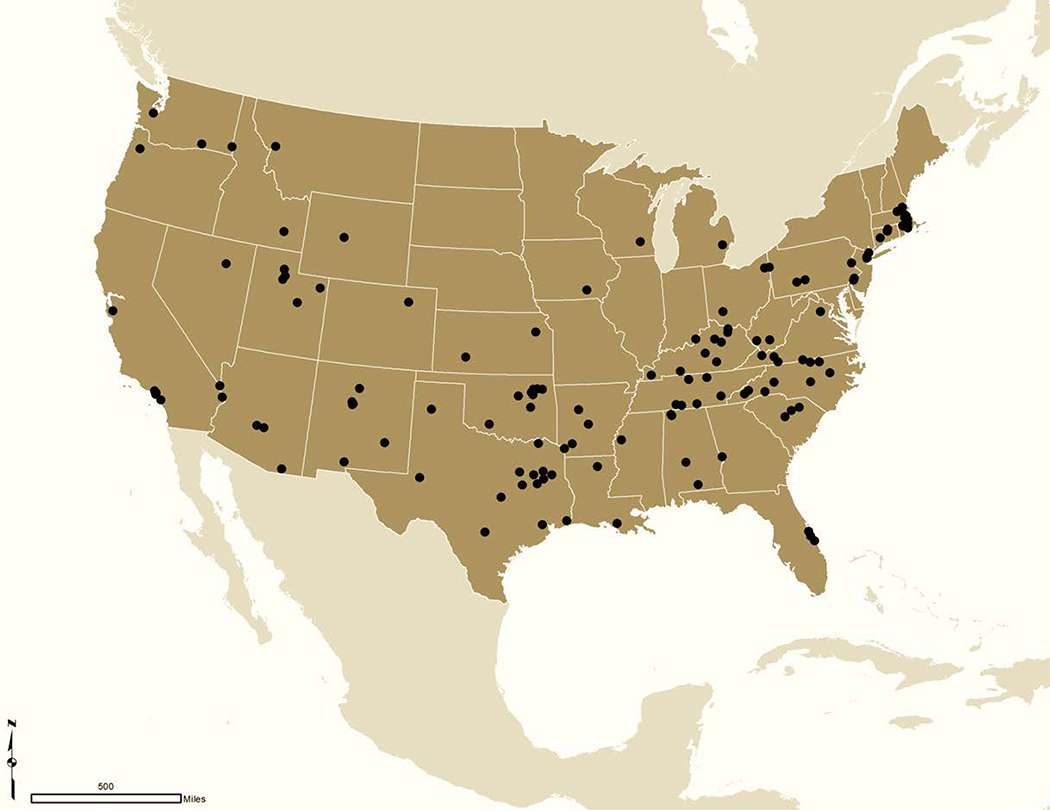
Most hospitals in this study were in the South (Figure) and were medium sized (Table). When compared with their matched hospitals, private equity hospitals on average had a higher rurality score, were located in a ZIP code with a lower median household income, had a slightly lower patient experience score, had fewer patients discharged per year, and had fewer full-time equivalent employees per occupied bed (Table). Private equity hospitals did not differ from their matched hospitals on net income per patient discharged, total inpatient charge per inpatient day, total charge-to-cost ratio, or Medicare and Medicaid shares of patients discharged.
Figure.
Map of private equity–owned hospitals in 2018.
Using Medicare cost reports, the addresses for the 130 private equity–owned hospitals in 2018 were identified. There were no hospitals located in Hawaii or Alaska.
Table.
Characteristics of Private Equity–Owned Hospitals and Control Hospitals*
| Characteristic | Private Equity–Owned Hospitals (n = 130) | Control Hospitals (n = 688) | Adjusted Difference (95% CI) | P Value† |
|---|---|---|---|---|
| Geographic region, % | ||||
| South | 53 | 54 | – | – |
| West | 24 | 23 | – | – |
| Northeast | 17 | 17 | – | – |
| Midwest | 6 | 7 | – | – |
| Hospital size, % | ||||
| Small (≤49 beds) | 7 | 7 | – | – |
| Medium (50–450 beds) | 91 | 91 | – | – |
| Large (≥451 beds) | 2 | 2 | – | – |
| Mean rurality score (SD)‡ | 2.70 (2.16) | 2.28 (2.14) | 0.42 (0.01 to 0.83) | 0.043 |
| Mean hospital ZIP code median household income (SD), $ | 45 389 (16 614) | 50 112 (24 472) | −4723 (−9455 to 9) | 0.050 |
| Mean patient experience score (SD)§ | 85.47 (3.74) | 88.19 (3.05) | −2.68 (−3.56 to −1.80) | <0.001 |
| Mean total patients discharged (SD), n | 5764 (4719) | 8453 (6660) | −1839 (−2364 to −1313) | <0.001 |
| Mean net income (SD), million $|| | 5.1 (16.5) | 15.1 (28.1) | −2.3 (−5.4 to 0.8) | 0.149 |
| Mean net income per patient discharged (SD), $ | 1030.3 (3453.2) | 1038.2 (6499.0) | −7.9¶ | – |
| Mean total inpatient charges (SD), million $** | 307.7 (355.2) | 423.2 (468.2) | 22.3 (−16.6 to 61.2) | 0.26 |
| Mean total inpatient charges per day (SD), $ | 9194.7 (4110.9) | 8825.6 (5498.3) | 369.1¶ | – |
| Mean total charges (SD), million $†† | 621.5 (562.8) | 877.2 (802.8) | 9.3 (−68.5 to 87.2) | 0.81 |
| Mean total charge-to-cost ratio (SD) | 5.8 (2.0) | 4.8 (2.4) | 1.0¶ | – |
| Mean Medicare patients discharged (SD), n‡‡ | 1958.5 (1603.0) | 2709.8 (2150.1) | 36.0 (−97.3 to 169.3) | 0.59 |
| Mean Medicare share of patients discharged (SD), % | 36.1 (10.3) | 34.4 (10.6) | 1.7¶ | – |
| Mean Medicaid patients discharged (SD), n§§ | 591.5 (756.4) | 763.8 (890.5) | 1.8 (−146.3 to 149.9) | 0.98 |
| Mean Medicaid share of patients discharged (SD), % | 11.1 (9.9) | 10.2 (11.1) | 0.9¶ | – |
| Mean full-time equivalent employees (SD), n|||| | 667.8 (487.5) | 1077.9 (899.2) | −164.9 (−250.6 to −79.1) | <0.001 |
| Mean full-time equivalent employees per occupied bed (SD), n | 12.6 (5.4) | 14.5 (10.9) | −1.9¶ | – |
Private equity–owned hospitals were matched to control hospitals on hospital referral region and size bin using exact matching in R MatchIt (R Foundation). We assigned control hospitals weights that summed to 1 (1/number of control hospitals). Hospital referral region was separated by geographic region for the purpose of this table.
To compare acute care hospitals owned by private equity firms with similarly sized and located hospitals not owned by private equity firms and to accommodate correlation within hospital referral region, we used a linear regression model with the variable of interest as the dependent variable and private equity ownership status as the independent variable, conditional on hospital referral region. We clustered SEs at the hospital referral region level.
Rurality codes range from metropolitan (1) to highly rural (10). These codes come from the Rural-Urban Commuting Areas geographic taxonomy, version 3.10.
The patient experience score refers to the Hospital Consumer Assessment of Healthcare Providers and Systems linear score.
We modeled total net income as the outcome and adjusted for total discharges, total beds, and hospital referral region.
Value is a ratio difference.
We modeled total inpatient charges as the outcome and adjusted for total inpatient days, total beds, and hospital referral region.
We modeled total charges as the outcome and adjusted for total costs, total beds, and hospital referral region.
We modeled total Medicare discharges as the outcome and adjusted for total discharges, total beds, and hospital referral region.
We modeled total Medicaid discharges as the outcome and adjusted for total discharges, total beds, and hospital referral region.
We modeled total full-time equivalent employees as the outcome and adjusted for occupied beds (total patient days/365), total beds, and hospital referral region.
Discussion
In this comparison of characteristics between hospitals owned by private equity and those not owned by private equity in 2018, private equity hospitals were on average located in lower-income, more-rural areas and had fewer patients discharged and employees per bed, although several economic outcomes were similar. Some of these differences may be due to unobserved factors, such as private equity–owned hospitals being located in less metropolitan areas with different populations and socioeconomic conditions than more metropolitan areas, and it is unknown whether these differences are attributable to the private equity acquisition itself. A separate question is whether private equity–owned hospitals differ from other hospitals in ways that negatively affect patient care. Fewer full-time–equivalent employees per occupied bed and lower average patient experience scores among private equity–owned hospitals raise concern. These measures, however, do not fully capture quality of care, and the potential effect of private equity on quality and other outcomes was outside the scope of this cross-sectional analysis. Therefore, additional research is necessary to identify and characterize the mechanisms underlying these differences.
Acknowledgments
Grant Support: By grant DP5-OD024564 from the Office of the Director, National Institutes of Health (National Institutes of Health Director’s Early Independence Award to Dr. Song).
Footnotes
Disclosures: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M20-1361.
Reproducible Research Statement: Study protocol: Not available. Statistical code: Available from Mr. Bruch, jbruch@g.harvard.edu. Data set: Data on total acquisitions by private equity firm are available from Mr. Bruch (jbruch@g.harvard.edu).
Contributor Information
Joseph Bruch, Harvard T.H. Chan School of Public Health; Boston, Massachusetts.
Dan Zeltzer, The Eitan Berglas School of Economics, Tel Aviv University; Tel Aviv, Israel.
Zirui Song, Harvard Medical School and Massachusetts General Hospital; Boston, Massachusetts.
References
- 1.Casalino LP, Saiani R, Bhidya S, et al. Private equity acquisition of physician practices. Ann Intern Med. 2019;170:114–115. [PMID: 30615785] doi: 10.7326/M18-2363 [DOI] [PubMed] [Google Scholar]
- 2.Bruch JD, Gondi S, Song Z. Changes in hospital income, use, and quality associated with private equity acquisition. JAMA Intern Med. 2020. November 1;180(11):1428–1435. [PMID: 32833006] doi: 10.1001/jamainternmed.2020.3552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coomer NM, Ingber MJ, Coots L, et al. Using Medicare Cost Reports to Calculate Costs for Post-Acute Care Claims. RTI Press; 2017. [PubMed] [Google Scholar]
- 4.Centers for Medicare & Medicaid Services. HCAHPS: patients’ perspectives of care survey. Accessed at www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS on 6 March 2020.
- 5.Bollen KA, Ward S. Ratio variables in aggregate data analysis: their uses, problems, and alternatives. Sociol Methods Res. 1979;7:431–450. doi: 10.1177/004912417900700405 [DOI] [Google Scholar]