Abstract
Introduction:
Psychoactive substance use may be risky for adults with functional impairments. This study investigates cannabis use and prescription opioid and tranquilizer/sedative (mis)use among adults aged ≥50 years reporting functional impairments in the U.S.
Methods:
This cross-sectional analysis of adults aged ≥50 years from the 2015–2019 cohorts of the National Survey on Drug Use and Health estimates the prevalence of past-year medical and nonmedical cannabis use, and prescription opioid and tranquilizer/sedative use and misuse, according to the number of functional impairments reported. The adjusted odds of medical and nonmedical use or misuse of each substance in relation to any impairment, number of impairments, and specific impairments were estimated using logistic regression. Analyses were conducted in December 2020.
Results:
Compared with those reporting no impairments, those reporting any impairment were more likely to report use of cannabis and (mis)use of prescription opioids and tranquilizers/sedatives (all p<0.05). Prevalence of (mis)use increased for each drug as number of impairments increased (all p<0.001). Having any impairment was associated with increased odds for medical cannabis use (AOR=2.28, 95% CI=1.57, 3.30) but not nonmedical use, and increased odds for misuse of prescription opioids (AOR=1.62, 95% CI=1.38, 1.91) and tranquilizers/sedatives (AOR=1.59, 95% CI=1.20, 2.11). Impaired thinking was associated with increased odds for use and misuse of each substance, and impaired ability to do errands was associated with increased odds for prescription opioid misuse (AOR=1.34, 95% CI=1.01, 1.78).
Conclusions:
Prescription drug misuse is linked to functional impairments among adults aged ≥50 years and may pose a potential risk for this vulnerable population.
INTRODUCTION
Among non-institutionalized people in the U.S., >40 million have a functional disability.1 Functional limitations in performing activities of daily living or instrumental activities of daily living are associated with the presence of chronic conditions2 and increased likelihood of institutionalization and healthcare use.3,4 Although previous studies examined psychoactive substance use patterns among adults with multiple chronic conditions,5 few focused on functional limitations. Disabilities are often related to uncontrolled chronic pain, psychological distress, or social isolation, which are also potential drivers for substance use.6,7 A previous study found disability status was correlated with prescription drug misuse,8 but a more current and nuanced characterization of psychoactive substance use among adults with functional limitations is needed.
The purpose of this study is to estimate the odds of medical and nonmedical cannabis use, and use and misuse of prescription opioids and tranquilizers/sedatives, among adults aged ≥50 years in the U.S. reporting a functional impairment, according to both number and type of impairment. Given that psychoactive substance use could be risky for older adults with impairments, findings could inform the scope of problematic substance use in this population.
METHODS
Study Sample
This study analyzed data from participants aged ≥50 years from the 2015–2019 National Survey on Drug Use and Health, an annual cross-sectional nationally representative sample of non-institutionalized individuals.9 Each year, a separate probability sample of individuals was obtained. Surveys were administered via computer-assisted interviewing and audio computer-assisted self-interviewing.
Measures
Participants were asked about demographic characteristics and use of cannabis or prescription opioids or tranquilizers/sedatives in the past year. Those reporting cannabis use were asked if it was recommended by a doctor and those reporting opioid or tranquilizer/sedative use were asked about misuse. Misuse was defined as using in any way not directed by a doctor, including use without a prescription, use in greater amounts, more often, or longer than instructed to take them, or use in any other way a doctor did not direct. Participants were asked whether they have: (1) serious difficulty concentrating, remembering, or making decisions because of a physical, mental or emotional condition; (2) serious difficulty walking or climbing stairs; (3) difficulty dressing or bathing; and (4) difficulty running errands alone such as visiting a doctors’ office or shopping because of a physical, mental or emotional condition.
Statistical Analysis
Prevalence of reporting any impairment and number of impairments according to past-year use of cannabis (medical and nonmedical) and prescription opioids and prescription tranquilizers/sedatives (medical use and misuse) was estimated. Adjusted odds of impairment in relation to past-year use for each drug as dependent variables was performed using logistic regression. AORs were derived from models controlling survey year, demographics, insurance status, and past-year major depression. Any impairment was examined as an independent variable, followed by number of impairments, and by individual impairments. Sensitivity tests were used to test these associations among those aged ≥65 years. Weights were used to account for complex survey design, selection probability, non-response, and population distribution. This secondary analysis was exempt from IRB review.
RESULTS
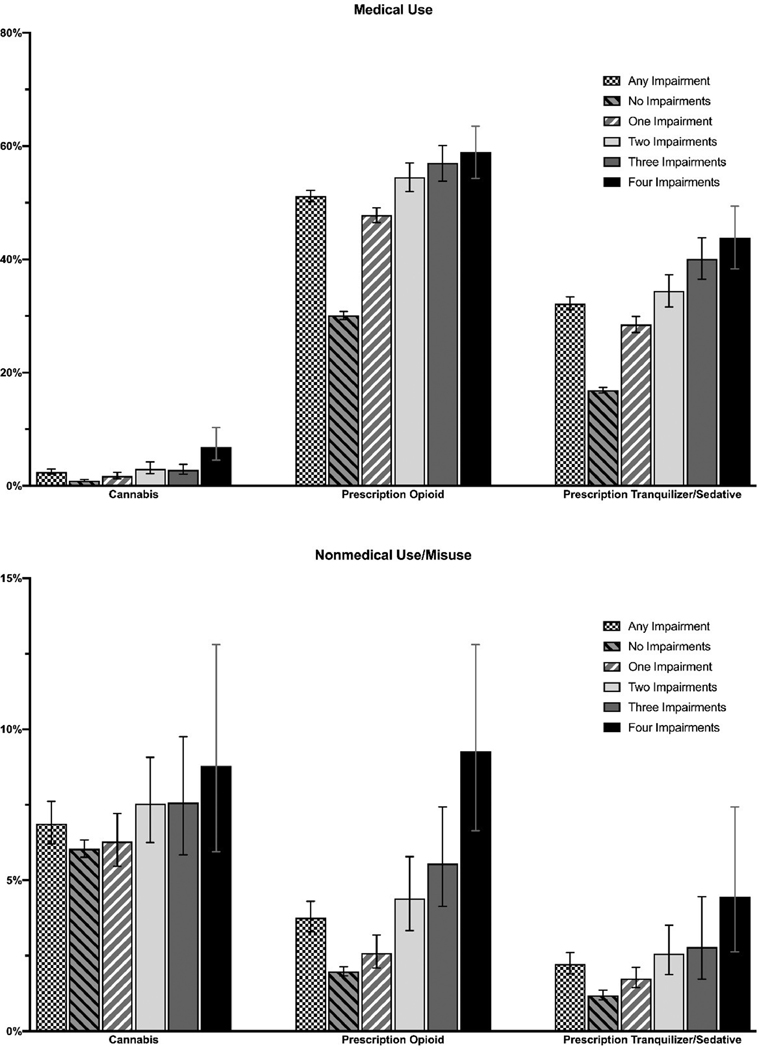
Sample characteristics by number of impairments are presented in Appendix Table 1. Figure 1 depicts the estimated prevalence of past-year use of the 3 drugs among those reporting any impairment and according to number of impairments. Compared with those reporting no impairments, those reporting any impairment were more likely to report use of cannabis (medical use: 2.5% vs 0.9%, nonmedical use: 6.9% vs 6.0%), opioids (medical use: 51.2% vs. 30.1%, misuse: 3.8% vs 2.0%), and tranquilizers/sedatives (medical use: 32.2% vs 16.9%, misuse: 2.2% vs 1.2%) (all p<0.05). The prevalence of (mis)use of each drug increased as the number of impairments increased (all p<0.001).
Figure 1.
Prevalence of past-year cannabis and prescription drug medical use and nonmedical/misuse by number of functional impairments.
Table 1 shows having any impairment was associated with increased odds for medical cannabis use (AOR=2.28, 95% CI=1.57, 3.30), and medical prescription opioid use (AOR=2.23, 95% CI=2.09, 2.38) and tranquilizer/sedative use (AOR=2.02, 95% CI=1.88, 2.17). With respect to number of impairments, there was a dose–response-like association with more impairments being associated with higher odds of use of each drug. Reporting any impairment was not associated with nonmedical cannabis use, but it was associated with higher odds for misuse of prescription opioids (AOR=1.62, 95% CI=1.38, 1.91) and tranquilizers/sedatives (AOR=1.59, 95% CI=1.20, 2.11). Regarding number of impairments, there was a dose–response-like association with more impairments associated with higher odds for opioid misuse. Impaired thinking and walking in particular were associated with increased odds of medical use of all drug classes. Impaired thinking was associated with increased odds for nonmedical use or misuse of each drug and difficulty running errands was associated with decreased odds for nonmedical cannabis use and increased odds for opioid misuse. Sensitivity tests (Appendix Table 2) for those aged ≥65 years yielded similar results, but with some associations attenuated.
Table 1.
Impairment in Relation to Past-Year Drug Use and Misuse Among Adults Age ≥50 Years
| Variable | Cannabis AORb (95% CI) | Opioids AOR (95% CI) | Prescription Tranquilizers/Sedativesa AOR (95% CI) |
|---|---|---|---|
| Medical use | |||
| Any impairment | |||
| No | 1.00 | 1.00 | 1.00 |
| Yes | 2.28 (1.57, 3.30) | 2.23 (2.09, 2.38) | 2.02 (1.88, 2.17) |
| Number of impairments | |||
| None | 1.00 | 1.00 | 1.00 |
| 1 | 1.88 (1.23, 2.87) | 2.03 (1.90, 2.18) | 1.80 (1.65, 1.96) |
| 2 | 2.90 (1.74, 4.81) | 2.50 (2.23, 2.80) | 2.18 (1.92, 2.48) |
| 3 | 2.39 (1.45, 3.94) | 2.78 (2.38, 3.25) | 2.78 (2.28, 3.37) |
| 4 | 4.46 (2.62, 7.59) | 2.67 (2.20, 3.24) | 2.84 (2.23, 3.61) |
| Specific impairments | |||
| Thinking | 1.77 (1.22, 2.56) | 1.20 (1.09, 1.32) | 1.69 (1.51, 1.88) |
| Walking | 1.74 (1.20, 2.51) | 2.14 (1.98, 2.31) | 1.53 (1.40, 1.67) |
| Dressing | 1.09 (0.71, 1.68) | 1.24 (1.10, 1.40) | 1.18 (0.96, 1.45) |
| Errands | 1.30 (0.83, 2.03) | 1.11 (1.01, 1.21) | 1.28 (1.07, 1.52) |
| Nonmedical use/Misuse | |||
| Any impairment | |||
| No | 1.00 | 1.00 | 1.00 |
| Yes | 1.09 (0.95, 1.24) | 1.62 (1.38, 1.91) | 1.59 (1.20, 2.11) |
| Number of impairments | |||
| None | 1.00 | 1.00 | 1.00 |
| 1 | 1.08 (0.93, 1.26) | 1.28 (1.03, 1.59) | 1.44 (1.07, 1.95) |
| 2 | 1.17 (0.93, 1.48) | 1.96 (1.43, 2.67) | 1.79 (1.19, 2.70) |
| 3 | 1.05 (0.77, 1.43) | 2.21 (1.46, 3.34) | 1.74 (0.91, 3.30) |
| 4 | 0.89 (0.55, 1.45) | 3.11 (2.13, 4.54) | 2.14 (1.21, 3.81) |
| Specific impairments | |||
| Thinking | 1.27 (1.06, 1.54) | 1.45 (1.15, 1.83) | 1.88 (1.27, 2.78) |
| Walking | 0.99 (0.83, 1.19) | 1.21 (0.96, 1.53) | 1.26 (0.92, 1.73) |
| Dressing | 1.10 (0.80, 1.52) | 1.39 (0.98, 1.95) | 0.80 (0.46, 1.41) |
| Errands | 0.82 (0.69, 0.97) | 1.34 (1.01, 1.78) | 1.15 (0.78, 1.71) |
Tranquilizers include benzodiazepines and muscle relaxants, and sedatives include zolpidem, eszopiclone, and zaleplon products. benzodiazepines: flurazepam, temazepam, and triazolam; and barbiturates.
Adjusted for year, age (50‒64 vs ≥65 years), sex, race/ethnicity, family income, marital status, education, insurance, and past-year major depression.
DISCUSSION
These findings suggest that functional impairments among adults aged ≥50 years are associated with greater odds of use and misuse of prescription opioids and tranquilizers/sedatives. This implies that functional impairments may precipitate an increase in these prescribed drugs with increasing burden of impairments while placing them at risk for misuse. This is important as prescription psychoactive drugs pose risks and in particular tranquilizers/sedatives should be avoided in older adults.11 Prescription opioid and benzodiazepine misuse can be dangerous among this demographic regarding an increased risk for falls, exacerbation of chronic diseases, and overdose.10
However, the increased misuse of prescription drugs may reflect undertreated symptoms. For example, among adults aged ≥50 years, the primary motive for opioid misuse is for pain relief12 and tranquilizer/sedative misuse is for undertreated insomnia and anxiety.13 Older adults who misuse psychoactive medications are more likely to rely on physician sources for them compared with younger adults.14,15 Likewise, research suggests that cannabis is primarily used by older adults to self-treat pain, insomnia, or anxiety.16 This study found that medical cannabis was associated with any and increasing number of impairments, but nonmedical use was not, suggesting adults aged ≥50 years with functional limitations are typically not using cannabis unless directed by a doctor.
Concerning specific impairments, older adults with impaired thinking were at greater odds of reporting the use of each of the three substances for both medical and nonmedical use. Again, this association may be related to their psychoactive properties, though the research connecting these substances to long-term cognitive decline is less established.17–19 There was an association between impaired ability to run errands and increased odds for opioid misuse, which may be due to undertreated chronic pain.12 These results highlight the need for better comprehensive screening, evaluation, and treatment for pain, anxiety, and insomnia for adults aged ≥50 years with functional impairments.
Limitations
This study has limitations. The National Survey on Drug Use and Health is cross-sectional and cannot establish temporality. Although the questions asked regarding impairment may be a proxy for impairments in activities of daily living /instrumental activities of daily living,8 they do not directly measure these; however, they capture important components of functioning. Future research focused on psychoactive substance use among people with functional limitations should use more commonly used measures of function. Finally, the National Survey on Drug Use and Health samples community-dwelling populations and does not include institutionalized adults.
CONCLUSIONS
This study provides national estimates of cannabis use and prescription opioid and tranquilizer/sedative (mis)use among adults aged ≥50 years with functional impairments. Although medically recommended cannabis, opioids, and tranquilizers/sedatives were associated with functional impairments, prescription drug misuse was also. Further research is needed to minimize the risks of psychoactive substance use in this population.
Supplementary Material
ACKNOWLEDGMENTS
This research was supported by grants through the National Institute on Drug Abuse: R01DA044207 (Palamar) and K23DA043651 (Han). NIH provided financial support for the project and the preparation of the manuscript but did not have a role in the design of the study, the analysis of the data, the writing of the manuscript, or the decision to submit the present research.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.U.S. Census Bureau. Disability characteristics from the 2018 American Community Survey. https://data.census.gov/cedsci/table?t=Disability&tid=ACSST1Y2018.S1810. Accessed November 15, 2020.
- 2.Jindai K, Nielson CM, Vorderstrasse BA, Quiñones AR. Multimorbidity and functional limitations among adults 65 or older, NHANES 2005–2012. Prev Chronic Dis. 2016;13:160174. 10.5888/pcd13.160174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greiner MA, Qualls LG, Iwata I, et al. Predicting nursing home placement among home- and community-based services program participants. Am J Manag Care. 2014;20(12):e535–e536. [PubMed] [Google Scholar]
- 4.Gaugler JE, Duval S, Anderson KA, Kane RL. Predicting nursing home admission in the U.S.: a meta-analysis. BMC Geriatr. 2007;7:13. 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Han BH, Ko R, Palamar JJ. Substance use by adults with medical multimorbidity in the United States, 2015‒2016. J Gen Intern Med. 2019;34(8):1394–1396. 10.1007/s11606-019-04980-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown RL. Functional limitation, pain, and alcohol use: exploring gender differences in the mediating role of depressive symptoms. J Stud Alcohol Drugs. 2015;76(5):809–817. 10.15288/jsad.2015.76.809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Backe IF, Patil GG, Nes RB, Clench-Aas J. The relationship between physical functional limitations, and psychological distress: considering a possible mediating role of pain, social support and sense of mastery. SSM Popul Health. 2017;4:153–163. 10.1016/j.ssmph.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ford JA, Hinojosa MS, Nicholson HL. Disability status and prescription drug misuse among U.S. adults. Addict Behav. 2018;85:64–69. 10.1016/j.addbeh.2018.05.019. [DOI] [PubMed] [Google Scholar]
- 9.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20–07-01–001, NSDUH Series H-55). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data. Accessed November 15, 2020. [Google Scholar]
- 10.Han BH, Moore AA. Prevention and screening of unhealthy substance use by older adults. Clin Geriatr Med. 2018;34(1):117–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674–694. 10.1111/jgs.15767. [DOI] [PubMed] [Google Scholar]
- 12.Schepis TS, Wastila L, Ammerman B, McCabe VV, McCabe SE. Prescription opioid misuse motives in US older adults. Pain Med. 2020;21(10):2237–2243. 10.1093/pm/pnz304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schepis TS, Wastila L, McCabe SE. Prescription tranquilizer/sedative misuse motives across the U.S. population. J Addict Med. In press. Online September 8, 2020. 10.1097/adm.0000000000000736. [DOI] [Google Scholar]
- 14.Schepis TS, McCabe SE, Teter CJ. Sources of opioid medication for misuse in older adults: results from a nationally representative survey. Pain. 2018;159(8):1543–1549. 10.1097/j.pain.0000000000001241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schepis TS, McCabe SE. Prescription tranquilizer/sedative sources for misuse in older adults. Subst Use Misuse. 2019;54(11):1908–1912. 10.1080/10826084.2019.1613434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang KH, Kaufmann CN, Nafsu R, et al. Cannabis: an emerging treatment for common symptoms in older adults. J Am Geriatr Soc. 2021;69(1):91–97. 10.1111/jgs.16833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dublin S, Walker RL, Gray SL, et al. Prescription opioids and risk of dementia or cognitive decline: a prospective cohort study. J Am Geriatr Soc. 2015;63(8):1519–1526. 10.1111/jgs.13562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Picton JD, Marino AB, Nealy KL. Benzodiazepine use and cognitive decline in the elderly. Am J Health Syst Pharm. 2018;75(1):e6–e12. 10.2146/ajhp160381. [DOI] [PubMed] [Google Scholar]
- 19.Pocuca N, Walter TJ, Minassian A, Young JW, Geyer MA, Perry W. The effects of cannabis use on cognitive function in healthy aging: a systematic scoping review. Arch Clin Neuropsychol. In press. Online November 7, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.