Abstract
Background:
There is a lack of information regarding the reasons why patients do not return to sports after an arthroscopic Bankart repair and whether there is a relationship between return to sports and functional outcomes.
Purpose:
To evaluate the reasons why competitive athletes who underwent arthroscopic Bankart repair did not return to sports and whether there was a relationship between returning to sports and postoperative outcome scores and complications.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Of 217 competitive athletes who underwent arthroscopic Bankart repair for isolated anterior glenohumeral instability between June 2014 and December 2017, a total of 208 athletes (96%) were evaluated at minimum 2-year follow-up. Return to sports, the level of sports achieved, and the time between surgery and return to competition were assessed, and patients who did not return to sports were asked to provide the reasons for cessation. The Rowe score and the Athletic Shoulder Outcome Scoring System (ASOSS) were used to assess functional outcomes. Recurrences, reoperations, and complications were also evaluated.
Results:
The mean patient age was 24 years (range, 18-30 years), and the mean follow-up was 44 months (range, 24-90 months). Of the 208 athletes, 73% were able to return to sports (65% returned to their preinjury level), and 27% did not return to sports. Of those who did not return, the most frequent reasons were fear of reinjury (44%), lack of confidence in their shoulder (12%), and concern about a new rehabilitation process in case of recurrence (10%). The Rowe and ASOSS scores showed significant postoperative improvement in all patients (P < .001), with no significant differences between the 2 study groups at the final follow-up. There were 21 recurrences (10%) and 5 complications (2.4%), and 11 patients (5.3%) underwent revision surgery, with no significant differences in these rates between the groups.
Conclusion:
Of patients who did not return to sports, 74% left for a reason independent of shoulder function, with the most frequent causes being fear of reinjury and a concern about new rehabilitation process. Neither outcome scores nor complications varied significantly between patients who returned and those who did not return to sports.
Keywords: glenohumeral instability, return to sports, Bankart, athletes
Glenohumeral instability is a frequent problem among young competitive athletes, especially those involved in contact and overhead sports such as handball, baseball, and martial arts. 5,11 Anterior glenohumeral instability is the main cause of sports absenteeism after shoulder injuries and may leave the athlete out of competition for 6 to 8 months. 5,11
The treatment of choice in competitive athletes without significant bony defects is arthroscopic capsulolabral repair (Bankart procedure). 13,26 In general, Bankart repair is associated with excellent outcome scores and a low complication rate. 12,18 However, studies have reported return to play rates ranging between 48% and 100%. 1,15,25 Because sports training as well as competition is a major activity or focus of interest among most young competitive athletes, such highly variable rates pose a relevant clinical problem. 1,15,25
Although numerous studies have evaluated return to sports results after Bankart repair, the only commonly evaluated variables are the rate of return to sports, the level achieved by athletes after surgery, and the time elapsed between the procedure and return to competition. 1,15,16 However, the reasons why patients do not return to sports have been scarcely addressed in the literature.
The purpose of this study was to evaluate the reasons why competitive athletes treated using an arthroscopic Bankart repair did not return to sports and whether there was a relationship between the rate of return to sports and the postoperative patient outcomes. We hypothesized that most athletes who did not return to sports would have reasons independent of their shoulder function and that outcome scores and complications would not vary significantly between athletes who returned and those who did not.
Methods
This was a retrospective comparative cohort study. The study protocol was approved by the local ethics committee of our institution, and all patients provided written informed consent to participate in this investigation.
A total of 280 competitive athletes underwent arthroscopic Bankart repair for isolated anterior instability at our institution between June 2014 and December 2017. The inclusion criteria for this study were participation in competitive athletics, age <30 years, and at least 1 instability episode (defined as a subluxation or dislocation with spontaneous reduction or complete dislocation requiring a reduction) as an indication for Bankart repair.
Exclusion criteria were large bony Bankart lesions (bony defects >20% on the anteroinferior portion of the glenoid), engaging Hill-Sachs lesions, humeral avulsion of the glenohumeral ligament lesions, associated superior labral anterior-posterior lesions, posterior labral tears, rotator cuff injuries, previous surgery on the same shoulder, anterior or inferior hyperlaxity, and multidirectional instability.
Evaluation
Preoperative and postoperative evaluations consisted of patient-reported outcome measures and a physical examination performed by a shoulder fellow who did not participate in the surgical procedure (I.P.). Instability was evaluated using apprehension and relocation tests performed at the preoperative evaluation and at the last follow-up. Anterior hyperlaxity was defined as external rotation >90° with arms at the side (reaching in the frontal plane), and inferior laxity was determined through use of the Gagey hyperabduction test. 7,10
Radiography and magnetic resonance imaging were performed in all patients preoperatively. If, during these studies, bony defects were suspected, computed tomography was ordered to evaluate the magnitude of defects. Patients were considered competitive athletes if they fulfilled all 4 criteria of Araújo and Scharhag 3 : (1) training in sports aiming to improve their performance; (2) actively participating in sports competitions; (3) formally registered in a local, regional, or national sports federation as a competitor; and (4) having sports training and competition as their major activity or focus of interest. Patients who did not fulfill these criteria were considered recreational athletes.
The distinctive types of shoulder-dependent sports were subdivided in an analog manner according to Allain et al 2 : noncollision/nonoverhead sports, high-impact/collision sports, overhead sports, and martial arts sports.
Pre- and postoperatively, patients completed the Rowe score 22 and the Athletic Shoulder Outcome Scoring System (ASOSS). 23 The ASOSS measures subjective, shoulder-dependent, sport-specific perceptions of pain, instability, muscular strength and endurance, intensity, and proficiency level, with percentage scores compared with conditions before injury (defined as 100%). Clinical outcomes were also assessed using the minimal clinically important difference (MCID) for the Rowe score, defined as an increase from baseline of at least 9.7 points. 20
Patients were contacted by telephone and then examined at a minimum follow-up of 24 months. Postoperatively, patients were asked whether they had been able to practice sports again and whether they had been able to perform their sports at the same level as before the injury. Patients who did not return to sports were asked to give their reasons for cessation. The determination of recurrences was made via a review of the electronic clinical records of the patients and an interview with and physical examination of the patients at the last follow-up visit. We defined recurrence as the presence of dislocation or a subluxation event that limited activities or sports.
Surgical Technique
The surgical technique for all cases in this series was an anterior arthroscopic stabilization performed with the patient in the lateral decubitus position under combined general endotracheal and regional anesthesia. All athletes underwent primary arthroscopic anterior glenohumeral stabilization surgery for anterior shoulder instability that entailed a knotted anchor technique using simple sliding knots. The labral edge was debrided after complete liberation and release of the capsulolabral ligament beyond the 6-o’clock position. Then, the anterior and inferior glenoid rim and neck were lightly abraded using a shaver. Typically, 3 anchors with No. 2 nonabsorbable sutures (CrossFT; ConMed) were placed on the cartilage edge of the glenoid surface (mean, 3.2 anchors; range, 2-4 anchors). The first anchor was placed in the inferior area of the anterior glenoid rim below the 5-o’clock position. Additional anchors were placed in a similar manner at both the 3- and the 4-o’clock positions. Capsular plication was performed, starting 1 hour inferior to the anchor placement and lateral depending on capsular laxity, between 5 and 15 mm, to create superior tensioning of the inferior glenohumeral ligament and eliminate inferior capsular redundancy. Once the sutures were placed in the correct position, they were secured using sliding knots. No patients in this series were treated using a posterior-inferior capsulolabral repair, rotator interval closure, superior labral anterior-posterior lesion repair, or remplissage.
Rehabilitation
A standardized postoperative physical therapy and rehabilitation program was used. The arm was supported in a sling for 4 weeks. After 1 week, patients began supervised gentle physical therapy consisting of gradual passive range of motion (ROM). Active-assisted ROM exercises were started 2 weeks after surgery. When the patient could perform active forward elevation above the shoulder level, strengthening exercises were started. Running was authorized at 8 weeks. Return to sports was allowed when the patient was pain-free without apprehension, full shoulder ROM had been achieved, and shoulder strength was the near the same as before the injury.
Statistical Analysis
Continuous variables are expressed as means and standard deviations, and results were compared between groups using the t test or Mann-Whitney U test if there were nonnormal distributions. The normality of distribution was tested using the Shapiro-Wilk test. Categorical variables are presented as absolute and relative frequencies. To compare the proportions of the categorical variables between the groups, the chi-square test or the Fisher exact test was used according to the assumptions. The statistical analysis was performed using STATA MP Version 14 (Stata Corporation). Statistical significance was set at P < .05.
Results
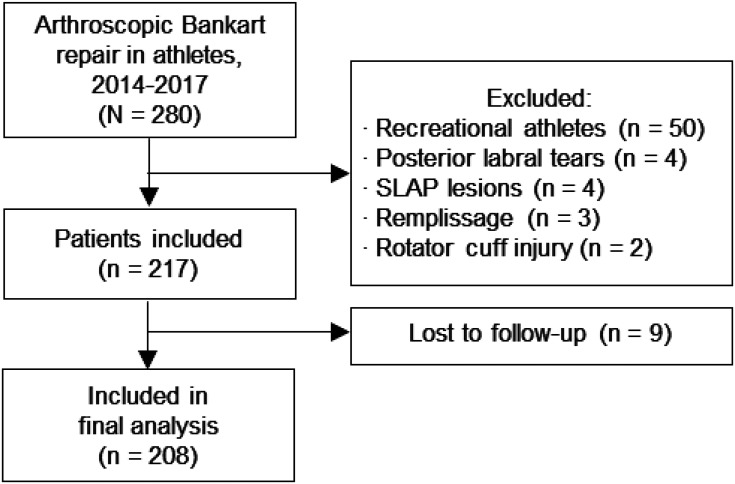
A total of 63 patients was excluded because they did not meet the inclusion criteria, and 9 patients were lost to follow-up. Thus, the final analysis entailed 208 patients (96% follow-up) (Figure 1).
Figure 1.
Flow diagram of the included patients. SLAP, superior labral anterior-posterior.
The mean follow-up was 44 months (range, 24-90 months). The study included 176 male athletes (85%) and 32 female athletes (15%). The mean age of the 208 patients at the time of surgery was 24 years (range, 18-30 years). Of the 208 arthroscopic stabilizations, 120 (58%) involved the dominant arm. Comparative details of patients who returned and did not return to sports are summarized in Table 1.
TABLE 1.
Patient Characteristics a
| Variable | Returned to Sports (n = 151) |
Did Not Return (n = 57) |
P Value |
|---|---|---|---|
| Age, y, mean (range) | 23.9 (17-30) | 24.7 (16-30) | .54 b |
| Dominant arm affected | 87 (58) | 33 (58) | .85 c |
| Follow-up, mo | 40 ± 18 | 38 ± 17 | .80 b |
| Competitive athlete | 80 (53) | 29 (51) | .80 c |
| Sport type | |||
| Noncollision/nonoverhead | 58 (38.5) | 23 (40.3) | |
| High-impact/collision | 52 (34.5) | 19 (33.3) | |
| Overhead | 35 (23) | 12 (21.3) | |
| Martial arts | 6 (4) | 3 (5) | |
| Preoperative evaluation | |||
| Rowe score | 45 ± 13 | 42 ± 14 | .51 b |
| ASOSS score | 52 ± 3 | 51 ± 5 | .21 b |
| Forward flexion, deg | 166 ± 5 | 169 ± 4 | .19 b |
| External rotation in adduction, deg | 63 ± 3 | 60 ± 4 | .13 b |
a Data are reported as n (%) or mean ± SD unless otherwise indicated. ASOSS, Athletic Shoulder Outcome Scoring System.
b t test.
c χ2 test.
Overall, 151 patients (73%) were able to return to sports, and 136 (65.3%) returned at the same level as before the injury. The mean time to return to sports was 5.4 months (range, 5-7 months). Regarding the reasons for sports cessation, 74% of patients who did not return to sports cited reasons independent of their shoulder function, and 26% of the patients reported not returning for reasons associated with their shoulder disorders. The reasons for sports cessation are reported in Table 2.
TABLE 2.
Reasons Why Patients Did Not Return to Sports (n = 57 Patients)
| Reason for Sports Cessation | n (%) |
|---|---|
| Independent from shoulder function | 42 (74) |
| Fear of reinjury | 25 (44) |
| Concern about new rehabilitation process | 6 (10) |
| Lack of time (family, work, university) | 5 (9) |
| Change in priorities and personal interest | 5 (9) |
| Associated injuries | 1 (2) |
| Dependent on shoulder function | 15 (26) |
| Lack of confidence in their shoulder | 7 (12) |
| Shoulder discomfort with sports | 6 (10) |
| Persistent instability | 1 (2) |
| Pain with sports | 1 (2) |
No significant difference in shoulder ROM was found between preoperative and postoperative results (Table 3). The Rowe score and ASOSS score showed statistical improvement after surgery (P < .001). Specifically, the Rowe score increased from a preoperative mean of 45.1 points to a postoperative mean of 95.2 points (P < .01). We found that 96% (145/151) of athletes returning to sports and 93% (53/57) of athletes not returning to sports achieved a clinically significant improvement that exceeded the MCID for the Rowe score. The ASOSS score improved significantly from a preoperative mean of 52.1 to a postoperative mean of 88.8 (P < .001). The final Rowe score and the final ASOSS score did not change significantly between the groups at the final follow-up (Table 3).
Table 3.
Comparative Outcomes Between Patients Who Returned and Did Not Return to Sports a
| Variable | Returned to Sports (n = 151) |
Did Not Return (n = 57) |
P Value |
|---|---|---|---|
| Change in ASOSS score | 35.7 ± 9 | 37.7 ± 9 | .325 |
| Change in Rowe score | 48.1 ± 11 | 50.1 ± 11 | .472 |
| Postoperative forward flexion, deg | 166.6 ± 4 | 168.3 ± 3.3 | .74 |
| Postoperative external rotation in adduction, deg | 64.2 ± 2.2 | 61.9 ± 2.4 | .11 |
| Recurrences | 16 (10.6) | 5 (8.7) | .697 |
| Complications | 4 (2.6) | 1 (1.8) | .532 |
| Revisions | 8 (5.3) | 3 (5.3) | .896 |
a Values are expressed as n (%) or mean ± SD. ASOSS, Athletic Shoulder Outcome Scoring System.
We noted 21 recurrences (10%) and 5 complications (2.4%). A total of 11 patients (5.3%) underwent revision surgery. Regarding complications, there were 2 cases of biceps tendinitis, 2 cases of subacromial bursitis, and 1 case of postoperative stiffness. In all patients, symptoms resolved via physical therapy. No significant differences were seen in the rate of recurrence, complications, or revision between the groups (Table 3).
Discussion
There were 3 main findings of our study. First, although we found excellent shoulder outcome scores after arthroscopic Bankart repair, a considerable number of athletes did not return to sports. Second, most athletes left sports for a reason independent of shoulder function, with the 2 most frequent reasons being fear of reinjury and concern about a new rehabilitation process in case of recurrence. Third, neither outcome scores nor complications varied significantly between patients who returned to sports and those who did not.
Currently, the majority of the evidence regarding return to sports after arthroscopic Bankart repair has been focused on how many athletes return to sports, the level of competition reattained, and the time elapsed between surgery and return to sports. 1,15,17,18 Memon et al 17 analyzed 34 studies, reporting an 81% pooled rate of return to sports at any level and a 66% rate of return to preinjury level at a mean of 7.9 months. Ialenti et al 15 reported that 90.5% of the athletes returned to sports after arthroscopic Bankart repair and 71% returned to their preinjury level at a mean of 8 months. Kasik et al 16 analyzed adolescent athletes after arthroscopic Bankart repair, showing an 89.2% rate of return to sports at any level, with 79.8% of patients returning to their preinjury levels of competition. Finally, Murphy et al 18 and Harris et al 14 analyzed long-term outcomes of arthroscopic Bankart repair with a minimum of 10- and 5-year follow-up, respectively, and reported return to sports rates of 74% and 77.6%, respectively. Similarly, our results were in line with the reported data, wherein 73% of the patients were able to return to sports and 65.3% returned at the same level as before the injury. The mean time to return to sports was 5.4 months. However, there is a lack of evidence regarding the reasons why some athletes did not return to sports after arthroscopic Bankart repair.
Tjong et al 25 evaluated the factors affecting 25 patients’ decision to not return to sports after an arthroscopic Bankart repair. Those authors reported that the most common reasons for cessation were fear of reinjury, shift in priority, mood, social support, and lack of motivation. Similarly, Plath et al 21 reported that most of their athletes did not return to sports after arthroscopic Bankart repair because of non--shoulder related reasons and because they were concerned about sustaining a further injury to the shoulder. In our series, 74% of the athletes did not return to sports for reasons unrelated to the shoulder. Specifically, when athletes were asked why they did not return to sports, most of them indicated fear of reinjury and concerns about a new rehabilitation process in the event of a new injury. Several studies have highlighted the influence of psychosocial factors on functional outcomes and return to sports after an anterior cruciate ligament (ACL) injury. 4,6,8,9,19,24
A systematic review by Czuppon et al 8 analyzed the variables associated with return to sports after ACL reconstruction, finding that lower kinesiophobia or fear of reinjury, higher athletic confidence, higher preoperative knee self-efficacy, and higher preoperative self-motivation were associated with return to sports. Similarly, a recent systematic review by Ardern et al 4 found that positive psychological responses, including motivation, confidence, and low fear, were associated with a greater likelihood of returning to sports. Finally, a systematic review by Everhart et al 9 revealed that psychological factors, such as self-confidence, optimism, self-motivation, social support, and athletic self-identity, have been predictive of ACL reconstruction outcomes. Overall, all of these studies show that after a severe injury, an athlete must be not only physically but also psychologically ready to return to sports. Consequently, apart from evaluating physical function, it is essential to address other factors such as fear, lack of confidence, and pressure from family and club authorities, which may hinder return to sports after arthroscopic Bankart repair. Shoulder surgeons need to acknowledge that psychosocial factors might play a significant role in determining return to sports outcomes.
Regarding outcome scores, both the Rowe and the ASOSS scores showed excellent postoperative outcomes, and thereby they could not explain why some athletes did not return to sports. This was reflected in our study in 2 ways: first, only 26% of the athletes reported not returning to sports because of shoulder-related causes. Second, the final outcome scores of those who returned to sports compared with those who did not return were similar. The same occurred with complications and reoperations. In our study, 10% of patients had recurrences, 2.4% had complications, and 5.3% underwent revision surgery. We found no significant differences in any of the 3 variables between patients who returned to sports and patients who did not return. We consider that the findings of our study are very relevant because they show that patients who did not return to sports had reasons independent of the shoulder, given that functional outcome scores and complications did not vary significantly between athletes who returned to competition and those who did not.
Limitations
This study has some limitations that should be mentioned. First, it is a retrospective study and has all the inherent limitations of this type of study. Second, all the athletes evaluated were competitive athletes. Although this population was chosen intentionally to homogenize the evaluated cohort, the results obtained may be different for recreational athletes. Third, we did not carry out a subanalysis regarding the relationship between the patients who did not return and the type of sports because we did not have enough patients. It is possible that the percentage of patients who do not return varies according to the demand imposed on the shoulder to practice each sport. However, we believe that this may influence the level of sports achieved more than the overall percentage of return because, as our study and previous studies have demonstrated, the majority of patients who do not return to sports cite reasons independent of the shoulder. Fourth, as this is a retrospective study, it could be subject to a recall bias related to the presence of recurrence because patients’ recollections are not fully reliable, particularly as an event becomes more remote in time.
Conclusion
Although Bankart repair produces excellent outcome scores in competitive athletes, a considerable number of patients do not return to sports. We found that 74% of patients left sports for a reason independent of the shoulder, with the 2 most frequent causes being fear of reinjury and concern about a new rehabilitation process in case of recurrence. Neither outcome scores nor complications varied significantly between patients who returned and those who did not return to sports.
Footnotes
Final revision submitted December 19, 2020; accepted January 21, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Hospital Italiano de Buenos Aires (IRB: 00010193).
References
- 1. Abdul-Rassoul H, Galvin JW, Curry EJ, Simon J, Li X. Return to sport after surgical treatment for anterior shoulder instability: a systematic review. Am J Sports Med. 2019;47(6):1507–1515. [DOI] [PubMed] [Google Scholar]
- 2. Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 1998;80:841–852. [DOI] [PubMed] [Google Scholar]
- 3. Araújo CG, Scharhag J. Athlete: a working definition for medical and health sciences research. Scand J Med Sci Sports. 2016;26(1):4–7. [DOI] [PubMed] [Google Scholar]
- 4. Ardern CL, Taylor NF, Feller JA, et al. A systematic review of the psychological factors associated with returning to sport following injury. Br J Sports Med. 2013;47:1120–1126. [DOI] [PubMed] [Google Scholar]
- 5. Cameron KL, Mauntel TC, Owens BD. The epidemiology of glenohumeral joint instability: incidence, burden, and long-term consequences. Sports Med Arthrosc Rev. 2017;25(3):144–149. [DOI] [PubMed] [Google Scholar]
- 6. Christino MA, Fantry AJ, Vopat BG. Psychological aspects of recovery following anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2015;23:501–509. [DOI] [PubMed] [Google Scholar]
- 7. Coste JS, Jund S, Lemaire M, Pascal B. Evaluation prospective arthroscopique du test de laxité du ligament gléno-huméral inférieur. Rev Chir Orthop. 1999;85:61. [Google Scholar]
- 8. Czuppon S, Racette BA, Klein SE, et al. Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Br J Sports Med. 2014;48:356–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sport Traumatol Arthrosc. 2015;23:752–762. [DOI] [PubMed] [Google Scholar]
- 10. Gagey OJ, Gagey N. The hyperabduction test. J Bone Joint Surg Br. 2001;83:69–74. [DOI] [PubMed] [Google Scholar]
- 11. Galvin JW, Ernat JJ, Waterman BR, Stadecker MJ, Parada SA. The epidemiology and natural history of anterior shoulder instability. Curr Rev Musculoskelet Med. 2017;10(4):411–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gao B, DeFroda S, Bokshan S, et al. Arthroscopic versus open Bankart repairs in recurrent anterior shoulder instability: a systematic review of the association between publication date and postoperative recurrent instability in systematic reviews. Arthroscopy. 2020;36(3):862–871. [DOI] [PubMed] [Google Scholar]
- 13. Gowd AK, Liu JN, Cabarcas BC, et al. Management of recurrent anterior shoulder instability with bipolar bone loss: a systematic review to assess critical bone loss amounts. Am J Sports Med. 2019;47(10):2484–2493. [DOI] [PubMed] [Google Scholar]
- 14. Harris JD, Gupta AK, Mall NA, et al. Long-term outcomes after Bankart shoulder stabilization. Arthroscopy. 2013;29:920–933. [DOI] [PubMed] [Google Scholar]
- 15. Ialenti MN, Mulvihill JD, Feinstein M, Zhang AL, Feeley BT. Return to play following shoulder stabilization: a systematic review and meta-analysis. Orthop J Sports Med. 2017;5(9):2325967117726055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kasik CS, Rosen MR, Saper MG, Zondervan RL. High rate of return to sport in adolescent athletes following anterior shoulder stabilisation: a systematic review. J ISAKOS. 2019;4(1):33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Memon M, Kay J, Cadet ER, et al. Return to sport following arthroscopic Bankart repair: a systematic review. J Shoulder Elbow Surg. 2018;27:1342–1347. [DOI] [PubMed] [Google Scholar]
- 18. Murphy AI, Hurley ET, Hurley DJ, Pauzenberger L, Mullett H. Long-term outcomes of the arthroscopic Bankart repair: a systematic review of studies at 10-year follow-up. J Shoulder Elbow Surg. 2019;28(11):2084–2089. [DOI] [PubMed] [Google Scholar]
- 19. Papadopoulos SD, Tishukov M, Stamou K, et al. Fear of re-injury following ACL reconstruction: an overview. J Res Pract Musculoskelet Syst. 2018;2:124–130. [Google Scholar]
- 20. Park I, Lee JH, Hyun HS, Lee TK, Shin SJ. Minimal clinically important differences in Rowe and Western Ontario Shoulder Instability Index scores after arthroscopic repair of anterior shoulder instability. J Shoulder Elbow Surg. 2018;27(4):579–584. [DOI] [PubMed] [Google Scholar]
- 21. Plath JE, Feucht MJ, Saier T, et al. Sporting activity after arthroscopic Bankart repair for chronic glenohumeral instability. Arthroscopy. 2015;31:1996–2003. [DOI] [PubMed] [Google Scholar]
- 22. Rowe C, Patel D, Southmayd W. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60:1–16. [PubMed] [Google Scholar]
- 23. Stein T, Linke RD, Buckup J, et al. Shoulder sport-specific impairments after arthroscopic Bankart repair: a prospective longitudinal assessment. Am J Sports Med. 2011;39(11):2404–2414. [DOI] [PubMed] [Google Scholar]
- 24. Te Wierike SCM, Van Der Sluis A, Van Den Akker-Scheek I, et al. Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sci Sports. 2013;23:527–540. [DOI] [PubMed] [Google Scholar]
- 25. Tjong VK, Devitt BM, Murnaghan ML, et al. A qualitative investigation of return to sport after arthroscopic Bankart repair: beyond stability. Am J Sports Med. 2015;43:2005–2011. [DOI] [PubMed] [Google Scholar]
- 26. Schrumpf MA, Maak TG, Delos D, et al. The management of anterior glenohumeral instability with and without bone loss: AAOS exhibit selection. J Bone Joint Surg Am. 2014;96(2):e12. [DOI] [PubMed] [Google Scholar]