Abstract
The COVID-19 crisis represents a global health concern, including mental health. Regarding the necessity to assess anxiety related to COVID-19, a scale was developed (Ahorsu et al., 2020). The goal of the present study was to validate the Fear of COVID-19 Scale (FCV-19S) in French (official language in 29 countries), and investigate its relationship with indicators of affective disturbances. The sample comprised 316 participants (271 females) recruited online during the French lockdown. They were from several regions of France. The FCV-19S underwent a forward-backward translation procedure. Its psychometric properties were evaluated with the confirmatory factor analysis (CFA). The French FCV-19S demonstrated a stable unidimensional structure with robust psychometric properties (strong internal consistency, good convergent and divergent validity, and good test-retest validity). With its robust psychometric properties in assessing the unidimensional construct of the fear of COVID-19, this scale will help to provide a better understanding of the relationship between emotions and psychological or psychiatric disorders during the pandemics in French-speaking countries.
Keywords: COVID-19, Fear, Fear of COVID-19 Scale, Mental health, Scale development, French validation
Background
During the last quarter of 2019 and in the beginning of 2020, a new and highly contagious disease — coronavirus disease-2019 (COVID-19) — spread worldwide. To date (end of May 2021), this pandemic has infected over 171.47 million people and caused over 3.56 million deaths among more vulnerable individuals (Worldometer, 2021). At the time of writing, there had been over 5.6 million confirmed cases and over 109,000 deaths in France. The crisis caused by COVID-19 is a virologic and infectious problem. If a large part of the contamination leads to asymptomatic or paucisymptomatic cases, some infected individuals will experience serious complications. These complications can be serious and can cause respiratory, inflammatory, and neurological problems (Wu et al., 2020). To deal with the intense spread of the virus at the beginning of 2020, the French government first isolated individuals who had COVID-19. Meetings of more than 5000 people were then prohibited on February 23, 2020. Finally, France went into a national lockdown between March 17 and May 11, 2020. Since then, a second partial lockdown (with schools remaining open) was implemented on October 30, 2020. The spread of COVID-19 also has an emotional dimension and could also lead to a “pandemic fear.” For many years, epidemics and their associated protective measures such as lockdowns and quarantining have been known for their effects on mental health (Brooks et al., 2020; Rogers et al., 2020). One of the major effects is the increase in stress levels and negative affects such as fear (Centers for Disease Control and Prevention, 2020). In addition, ambiguous or even false information about factors related to the COVID-19 (e.g., transmission, incubation period, infection, and mortality rates) can lead to insecurity and fear in the population (Ornell et al., 2020). In such a context, individuals naturally began to be worried about COVID-19, especially of being in contact with individuals who are possibly affected by the COVID-19 (Lin, 2020).
All of these negative emotional reactions can have a negative effect on mental health that could evolve into severe disorders including depression, anxiety, paranoia, psychotic episodes, and (in extreme situations) suicide (Griffiths & Mamun, 2020; Mamun et al., 2021). Such abnormal affective states can result in irrational processing of information related to the pandemic (Gunnell et al., 2020). Mental health conditions also tend to last longer (e.g., possibly 6 months after the end of the disease) and are associated with a greater prevalence (Brooks et al., 2020; Ornell et al., 2020; Shultz et al., 2016). It has also been suggested that the “second wave” of COVID-19 will be more about mental health (World Health Organization [WHO], 2020). Indeed, beyond the re-emergence of the virus in a population a few months apart, public health systems could be faced with the delayed consequences of the pandemic on mental health (Carbone, 2020).
Recently, a self-report psychometric tool — the Fear of COVID-19 Scale (FCV-19S) — was developed to assess the level of fear of COVID-19 among individuals in the general population (Ahorsu et al., 2020). The tool was developed based on the review and assessment of 30 other “fear scales” (e.g., fear of cancer, fear of crime, fear of missing out in social media use). The most relevant and salient items were selected resulting in 28 relevant items. These items were then reduced to 17 after examination by experts in general health, mental health, and virology. Supplementary steps led to the development of a 10-item scale that was then tested and validated among 717 Iranian participants in the Persian language. After testing the psychometric properties of the scale (e.g., exploratory factor analysis, correlation analyses), only seven of the 10 items were retained in the final scale. Since then, it has been translated, validated, and used in many countries including versions in Arabic (Alyami et al., 2020), Amharic (Elemo et al., 2020), Bangla (Mamun et al., 2021; Sakib et al., 2020), Chinese (Chang et al., 2020), [Cuban] Spanish (Broche-Pérez et al., 2020), English (Winter et al., 2020), Greek (Tsipropoulou et al., 2020), Indian (Doshi et al., 2020; Revathishree et al., 2020), Israeli (Bitan et al., 2020), Italian (Soraci et al., 2020), Japanese (Masuyama et al., 2020; Wakashima et al., 2020), Kazakh (Konstantinov et al., 2020), Malay (Pang et al., 2020), [Mexican] Spanish (García-Reyna et al., 2020), Pakistani (Mahmood et al., 2020), Peruvian [Spanish] (Huarcaya-Victoria et al., 2020), Polish (Sigorski et al., 2020), Russian (Reznik et al., 2020; Yehudai et al., 2020), Spanish (Martínez-Lorca et al., 2020), Taiwanese (Chang et al., 2020), and Turkish (Kaya et al., 2020). A growing body of research is now using this scale to investigate the consequence of the COVID-19 pandemic on psychological well-being (e.g., Mamun et al., 2021; Perz et al., 2020; Rahman et al., 2020; Satici et al., 2020; Sigorski et al., 2020).
However, it has not been translated and validated in French, the official language in 29 countries worldwide. Considering the need for identifying and preventing the mental health consequences associated with the pandemic, the authors adapted and validated the French version of the Fear of COVID-19 Scale. This will provide a good basis on which to understand the psychiatric and psychological consequences of the COVID-19 in French-speaking countries. The first aim of the present study was to adapt the items of FCV-19S into French. For this, a standard translation and back translation with native speakers was conducted. The second aim was to investigate the factor structure of the French version of the scale, and to examine if the one-factor solution was found among French-speaking individuals. Furthermore, because the main issue of the mental health–related consequences to the pandemic concerns fear and anxiety, the relationship between the fear of the COVID-19 and markers of emotion functioning was evaluated. More specifically, the correlations between the self-perception of vulnerability to illness and fear of COVID-19 were investigated. Due to the unavailability of the Perceived Vulnerability to Disease Scale in French, a standard translation and validation was also conducted. As the emotion of fear appears to be central in this pandemic, and in order to better assess the vulnerability of individuals to anxiety and fear symptoms related to COVID-19, individuals’ trait emotions were also assessed. Positive correlations were expected between negative emotions and scores on the FCV-19S, as well as negative associations with positive emotions. Finally, based on the extant literature elsewhere, it has been shown that the pandemic has led to the emergence of mental health disturbances (Carbone, 2020; Carre et al., 2020; Pakpour & Griffiths, 2020; Raony et al., 2020; Rogers et al., 2020; Taquet et al., 2020; Torales et al., 2020). Therefore, the present study also investigated the relationship between the FCV-19S and symptoms of anxiety and depression. Positive correlations between fear of COVID-19, anxiety, and depression were expected.
Methods
Participants and Procedure
A total of 471 participants took part in an online survey (between April and May 2020) during the lockdown period in France (which started on March 17 and ended May 11, 2020). The final sample comprised 316 French participants (271 women, 85%) because those who did not complete all the survey questions were removed from the final analysis. Participants were aged between 16 and 77 years (M=35.55 years, SD=14.27). Participants had to indicate their mother tongue at the start of the study. For those who did not report French as their mother tongue, they were asked to indicate their level of verbal fluency (e.g., high level or very high level of understanding the French language). All were French native speakers or fluent in the French language. Participants were volunteers and recruited through online advertisement on social media (e.g., Facebook, Twitter) and institutional mailing lists of universities. Convenience sampling was utilized to collect the data. All the participants completed and signed a consent form prior to data collection.
Ethical Standards
All procedures complied with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Additionally, the study was approved by the research team’s university ethics committee (CER-flash-2020-283).
Measures
Demographic questions were asked including gender, age, education, occupation, and history of their psychological problems (e.g., depression, anxious disorders), and consumption of psychoactive substances (e.g., nicotine, alcohol, recreational and illicit drugs). The survey also included several psychometric instruments that assessed affective components. Descriptive statistics and reliability coefficients are shown in Table 1.
Table 1.
Descriptive statistics and correlations with the French Fear of COVID-19 Scale
| Variables | Mean (± S.D.) | Cronbach’s a [95% CI] | McDonald’s ω | Correlation (r) with French FCV-19S | p-values |
|---|---|---|---|---|---|
| STAI Y-A | 46.24 (13.90) | .95 [.94, .96] | .96 | .49 | <0.001 |
| STAI Y-B | 46.12 (11.82) | .93 [.92, .94] | .94 | .33 | <0.001 |
| HADS-Anxiety | 8.53 (4.47) | .83 [.8, .86] | .84 | .50 | <0.001 |
| HADS-Depression | 6.34 (4.31) | .81 [.78, .84] | .82 | .40 | <0.001 |
| PVDS-Germ aversion | 4.27 (1.21) | .76 [.72, .8] | .76 | .43 | <0.001 |
| PVDS-Perceived infectability | 3.92 (1.26) | .77 [.73, .81] | .78 | .27 | <0.001 |
| PVDS-Perceived vulnerability to disease | 4.12 (1.07) | .82 [.79, .85] | .83 | .48 | <0.001 |
| DES-IV–Joy | 10.47 (2.62) | .85 [.82, .88] | .86 | −.29 | <0.001 |
| DES-IV–Interest | 10.40 (2.10) | .54 [.44, .62] | .58 | −.19 | <0.001 |
| DES-IV–Anger | 7.30 (3.01) | .79 [.75, .83] | .79 | .33 | <0.001 |
| DES-IV–Disgust | 6.25 (2.47) | .60 [.52, .67] | .65 | .35 | <0.001 |
| DES-IV–Fear | 6.40 (3.01) | .84 [.81, .87] | .85 | .58 | <0.001 |
| DES-IV–Sadness | 8.31 (2.98) | .85 [.78, .85] | .86 | .37 | <0.001 |
STAI-Y-A and STAI-B, State (Y-A) and Trait (Y-B) Anxiety Inventory; HADS, Hospital and Anxiety Depression Scale; PVDS, Perceived Vulnerability to Disease Scale; DES-IV, Differential Emotions Scale
The Fear of COVID-19 Scale (FCV-19S)
The 7-item French version of the Fear of COVID-19 Scale (Ahorsu et al., 2020) was used to assess the extent of fear of COVID-19. Participants provide ratings on a 5-point Likert type scale ranging from 1 (Strongly disagree) to 7 (Strongly agree). The higher the score, the greater the fear of COVID-19. Following general guidelines for cross-cultural adaptation (Guillemin et al., 1993), the original items of the FCV-19S were translated from English to French by two French native speakers. A committee comprising two experts established a preliminary version of the French FCV-19S based on these translations. This preliminary version was then translated from French to English (i.e., back-translation) by an English native speaker. Finally, the committee revised the preliminary version of the FCV-19S based on the translations and back translations (see Appendix A for the items). Example items include “I am most afraid of coronavirus-19” and “It makes me uncomfortable to think about the coronavirus-19”.
Statistical Analysis
Analyses of the Factor Structure of the FCV-19S
As the FCV-19s has previously been validated in several contexts (at least 11 languages), a previously been validated in several contexts was performed to verify the factor structure of the scale2. Data were continuous but not normal. Therefore, the weighted least estimator (WLS) was used to decrease risk of type I error (Brown, 2015). In the CFA analysis, goodness of fit was evaluated using the chi-square test. However, because the χ2 test is highly affected by sample size (Bentler & Bonett, 1980), we also considered the relative χ2 (ratio χ2/df), which is less influenced by sample size. The acceptable relative χ2 range is from less than two (Ullman, 2006) to less than five (Schumacker & Lomax, 2010). In addition, commonly applied goodness-of-fit indices were also examined: the Comparative Fit Index (CFI; Bentler, 1990), the Tucker-Lewis Index (TLI; Tucker & Lewis, 1973), and the root mean square error of approximation (RMSEA, Steiger, 1998). Good fit was indicated by a non-significant chi-square test, CFI and TLI values ≥.95 (for good, ≥.90 for acceptable) and RMSEA ≤0.06 (for good, acceptable fit if ≤ .08) with 95% confidence interval (Hu & Bentler, 1999). Analyses of data should not only be based on fit indices. Close inspection of parameter estimates (e.g., factor loadings, cross-loadings) may also reveal relevant information about the model (Morin et al., 2020).
Reliability
Reliability was assessed with Cronbach’s alpha using the commonly reported cut-off values of .70 and .80 (Nunnally, 1978). However, in the case of a factor only including a few items, values between .60 and .70 are considered acceptable (Hair, Black, Babin, & Anderson, 2014). The 95% confidence interval for each Cronbach’s alpha was also calculated. Moreover, given risks of biases using Cronbach’s alpha, additional evidence of reliability was calculated in the form of a McDonald’s omega coefficient (Bollen, 1980; Raykov, 2001).
Convergent and Divergent Validity
The convergent and divergent validity investigated by correlations with the various validity measures on the whole sample (n=316). Effect sizes were evaluated according to Cohen’s standards (1988): correlations of r=.10 to .30 were considered small, .30 to .50 were considered medium, and ≥ .50 were considered large. A positive correlation was expected between the French FCV-19S total score and the STAI-A and STAI- B, the HADS (anxiety, depression, and total) scores, and with germ aversion, perceived infectability and perceived vulnerability to infectious disease. Positive correlations with disgust, shame, sadness, contempt, fear, and anger were also expected. Negative correlations with joy and interest were also expected.
Test-Retest Reliability
Eighty-six participants (81 women and 5 men) completed the French FCV-19S again 6 weeks after first completing it. Their mean age was 31.48 years (SD=12.02). The test-retest reliability was assessed with intra-class coefficient and its 95% confidence interval.
All analyses were performed using R version 3.6.1 (R Core Team, 2019). Several R packages (psy, psych, mice, and lavaan especially for CFA and SEM analyses) were used. Statistical tests were considered significant at p<.05. Pre-registration, materials, data, and scripts are referenced on the Open Science Framework (URL blinded for anonymous peer review).
Results
Confirmatory Factor Analysis of the FCV19-S
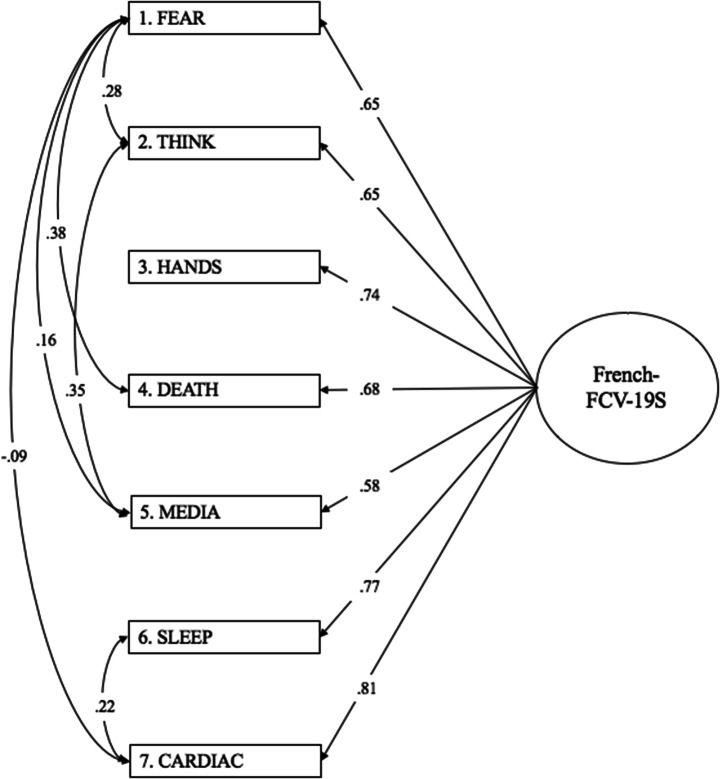
The one-factor model of the FCV19-S arising from the literature yielded the following indices: χ2(14)=79.69, p<.001; relative χ2=5.69, RMSEA=.122 (95% CI [.097, .149], CFI=.726, TLI =.589, SRMR=.201. These results indicate that the goodness of fit was not optimal. In an effort to make the more optimal model for the data, the modification indices (MIs) were considered. Each modification was assessed by a comparison between the two models to choose the best. It was found that the inter-item correlations in the final one-factor model (Fig. 1) yielded the following indices: χ2(8)=5.164, p=.740; relative χ2=0.65, RMSEA=.000 (95% CI [.000, .048]), CFI=1.000, TLI=1.031, SRMR=.017. This one-factor model presented satisfactory internal consistency (Cronbach’s alpha=.87, 95% CI= [.85, .89], and the omega coefficient was .85). Standardized factor loadings indicated that all items appropriately reflected the unidimensional structure.
Fig. 1.
Factorial structure of the French version of the Fear of Covid-19 Scale
Convergent and Divergent Validity
The French FCV-19S total score correlated positively with all expected variables, especially with the DES-IV subscale of fear (Table 1). The French FCV-19S total score correlated negatively with joy and interest (Table 1). These results indicated a good convergent and divergent validity. Predictive SEM was also conducted to examine the variables in the FCV-19S model. Fit indices were satisfactory (χ2[86]=235.52, p<.001; relative χ2=2.74, RMSEA=.074 (90% CI [.063, .086], CFI=.797, TLI =.734, SRMR=.065). Apart from the HADS-Anxiety score (p=.134), and the differential trait emotions (assessed by the DES-IV) of joy (p=.931), interest (p=.257), and sadness (p=.206), all other markers of emotion functioning were statistically significant. Concerning the emotional traits, the fear of the COVID was negatively predicted by anger (p=.021), and positively predicted by disgust (p<.001). State anxiety (p<.001) and depressive symptoms (HADS-Depression, p=.045) positively predicted the FCV-19S score. Scores concerning trait anxiety (p=.006), germ aversion (p<.001), and perceived infectability (p<.001) negatively predicted the FCV-19S score.
Test-Retest Reliability
The mean French FCV-19S total scores for the group of the re-test, at the initial testing (t1) and following a 6-week interval (t2), are displayed in Table 2. The intra-class correlation coefficient (ICC)3 revealed good test-retest reliability for between the test and the re-test assessments (ICC=.76, ICC 95% CI =[.66; .84], F(85,86)=7.38, p<.001).
Table 2.
Scores on the French Fear of Covid-19 Scale for the whole sample and the subsample (test-retest)
| Whole sample CFA N = 316) |
Group R (T1)a (n = 86) |
Group R (T2) (n = 86) |
|
|---|---|---|---|
| FCV-19S | 15.82 (6.19) | 14.74 (5.63) | 14.03 (4.69) |
aT1 refers to the score obtained at the initial time of testing; T2 refers to scores obtained following a 6-week interval
FCV-19S, Fear of Covid-19 Scale; CFA, confirmatory factorial analysis; Group R, Group for the Retest
Discussion
The aim of the present study was to evaluate the psychometric properties of the Fear of COVID-19 Scale among the French population. As in the original study, the French version demonstrates a stable unidimensional structure with robust psychometric properties. In particular, there was (i) strong internal consistency (as demonstrated by the very good Cronbach’s alpha and McDonald’s omega); (ii) acceptable construct validity (as demonstrated by the CFA); (iii) confirmed unidimensional structure as demonstrated by the CFA (see also supplementary materials); (iv) good convergent (especially shown by the large and positive correlation with the feeling of fear); (v) good divergent validity (as shown by the negative correlation with the feeling of joy), tested by predictive SEM; (vi) and good test-retest reliability (as demonstrated by the intra-class coefficient).
As in a previous validation study (Soraci et al., 2020), although we did not include formal diagnoses concerning disorders (e.g., generalized anxiety disorders, depression), the French FCV-19S total score was positively correlated with anxiety and depression. This is in line with previous studies highlighting that long period of infectious pandemic can affect individuals’ mental health (Duncan et al., 2009; Pappas et al. 2009). The French FCV-19S total score was also strongly and positively correlated with intense negative feelings including fear, anger, and disgust. These results are of particular interest as a further investigation of the individuals’ negative emotional feelings, and deepen the understanding of psychiatric and psychological consequences of a pandemic.
As highlighted in “Background,” many mental health problems can arise at a distance from the presence of the virus and health measures (Ornell et al., 2020; Rogers et al., 2020). In addition, one or more new acute waves of COVID-19 are feared in France, as in other countries, in the absence of a disappearance of the virus or the availability of a vaccine. For this reason, the availability of a tool such as the FCS-19S appears relevant. It can be used in the screening of the most severe affective disturbances related to the pandemic, and at a distance from the virologic peaks.
Although a lot of uncertainty still remains concerning COVID-19 and its trajectories in the potential waves of the pandemic, it is strongly believed that individuals’ mental health and well-being has suffered directly or indirectly since the beginning of the outbreak (Kontoangelos et al., 2020; Ornell et al., 2020; Taylor et al., 2020). More specifically, due to contamination or societal interventions (e.g., physical distancing, lockdown, etc.), the following waves of the pandemic may impact on mental health. It has been suggested that the “second wave of COVID-19” could be a wave of mental health issues (Brooks et al., 2020; Carbone, 2020; Taquet et al., 2020). Beyond hypochondriasis attitudes and intolerance to uncertainty, this global crisis could generate radical reactions or beliefs harmful at individual or interpersonal levels (e.g., suicide attempts, opposition to future treatments or vaccination). This could be the consequence of high levels of fear which affect beliefs and behaviors (Coelho et al., 2020; Erku et al., 2020; Gunnell et al., 2020; Lee & Crunk, 2020). In fact, the development of such a tool in French would provide the opportunity for French-speaking epidemiological studies linking mental health and the COVID-19 crisis (Wathelet et al., 2020). From an interventional point of view, psychoeducation and management concerning the exacerbated symptoms of fear (anxiety) related to the disease of COVID19 are needed.
This study has some limitations. First, the sample was modestly sized (although sufficient to test the psychometric properties of the French FCV-19S) and comprised a majority of females leading to the impossibility to test gender differences. Further investigations on bigger and more representative gender-balanced samples are needed to replicate preliminary results provided by the present study and the association between the French FCV-19S and age. It also appears relevant to investigate the extent in which “underlying medical conditions associated with a higher risk of death from COVID-19 (e.g., diabetes, hypertension, coronary heart disease, pre-existing respiratory conditions) may experience increased levels of COVID-19 fear” (Soraci et al., 2020, p.7). In addition, in view of the global phenomenon of the pandemic, and the international dissemination of this assessment tool, an analysis of population invariance would appear relevant to the cross-cultural stability of the scale.
In conclusion, the French FCV-19S demonstrated good and robust psychometric properties to assess the unidimensional construct of the fear of COVID-19 among French-speaking participants. In short, the French FCV-19S is a reliable, stable, and valid tool for assessing the severity of the fear of COVID-19. This scale can be used to better investigate the relationship between emotions and psychiatric and psychological disorders during the COVID-19 pandemic.
Appendix 1 The seven items of the French Fear of COVID-19 Scale (Ahorsu et al., 2020)
|
Items (French translation) | |
|
Item 1. I am most afraid of coronavirus-19. (J’ai très peur du Covid-19.) | |
|
Item 2. It makes me uncomfortable to think about the coronavirus-19. (Penser au Covid-19 me rend mal à l'aise.) | |
|
Item 3. My hands become clammy when I think about coronavirus-19. (J'ai les mains moites quand je pense au Covid-19.) | |
|
Item 4. I am afraid of losing my life because of coronavirus-19. (J'ai peur de mourir à cause du Covid-19.) | |
|
Item 5. When watching news and stories about coronavirus-19 on social media, I become nervous and anxious. (En regardant les nouvelles sur le Covid-19 dans les réseaux sociaux, je deviens nerveux (se) ou anxieux (se).) | |
|
Item 6. I cannot sleep because I’m worrying about getting coronavirus-19. (Je ne peux pas dormir car je suis inquiet(e) d'attraper le Covid-19.) | |
|
Item 7. My heart races or palpitates when I think about getting coronavirus-19. (Mon rythme cardiaque accélère ou j'ai de palpitations lorsque je pense au Covid-19.) |
Differential Emotions Scale IV (DES-IV)
The DES-IV is a 36-item scale that assesses individuals’ trait emotions (i.e., individuals’ frequent experiences of discrete emotions in their daily life) on 12 dimensions developed by Izard et al. (1993; French version: Ricard-St-Aubin et al., 2010). Each of the 12 dimensions is assessed by three items. Participants are asked to rate how often they feel the emotions in their daily life on a 5-point Likert type scale from 1 (Rarely or never) to 5 (Very often). The higher the score, the greater individuals feel the associated emotions. Positive emotions refer to joy, seeking-interest, and surprise whereas negative emotions refer to anger, disgust, contempt, fear, guilt, shame, shyness, sadness, and self-hostility1. Example items include “In your everyday life, how often do you feel yelling at someone or banging something?” (anger) and “In your everyday life, how often do you feel satisfied about something?” (joy). The scale had acceptable reliability in the present study (Table 1).
The Hospital Anxiety and Depression Scale (HADS)
The HADS (Zigmond & Snaith, 1983; French version: Razavi et al., 1989) was used to assess the level of depression among participants. Participants provide ratings on a 4-point Likert type scale ranging from 0 to 3. The HADS contains two sub-scales of seven items, one for anxiety and one for depression. Example items include “I feel tense or ‘wound up’” (anxiety) and “I still enjoy the things I used to enjoy” (depression). The HADS is scored by summing the rating for the 14 items yielding a total score that can range from 0 to 42, and by summing the rating for the seven items of each subscale. The subscales yield separate scores for anxiety and depression that range from 0 to 21. The scale had acceptable reliability in the present study (Table 1).
Spielberger’s State-Trait Anxiety Inventory (STAI)
The STAI state (STAI-A) and trait (STAI-B) assess two dimensions of anxiety (Spielberger et al., 1983; French version: Bruchon-Schweitzer and Paulhan, 1993). The STAI-A and the STAI-B comprise a 20-item scale. Example items include “I feel nervous and restless” and “I feel like a failure.” Participants provide ratings on a 4-point Likert type scale. Assessment of state anxiety asks participants to describe how they feel “right now, at this moment.” In contrast, trait anxiety asks participants to describe how they feel “in general.” Each scale is scored by summing the rating for the 20 items to give a score that can range from 20 to 80. The scales had acceptable reliability in the present study (Table 1).
Perceived Vulnerability to Disease Scale (PVDS)
The PVDS (Duncan et al., 2009) is a 15-item scale that assesses self-perception of vulnerability to infectious disease specifically perceived infectability (7-item subscale) and germ aversion (8-item subscale). Participants respond to each item on a 7-point scale Likert type scale from 1 (strongly disagree) to 7 (strongly agree) with approximately half of the items reverse-scored. Example items include “In general, I am very susceptible to colds, flu and other infectious diseases” (perceived infectability) and “I prefer to wash my hands pretty soon after shaking someone’ hand” (germ aversion). A higher score indicates greater perceived infectability, germ aversion, and perceived vulnerability to disease (as a whole). As it was the first time the PVDS had been used in French, it was translated and its factorial structure was evaluated. Details of this are shown in Appendix B. These scales had acceptable reliability in the present study (alphas are displayed in Table 1).
Appendix 2 Details about the adaptation of the Perceived Vulnerability to Disease Scale (PVDS) in French
The scale was translated into French using the same procedure (outlined in the “Measures” section) as that of the French Fear of COVID-19 Scale (FCV19-S). The French Perceived Vulnerability to Disease Scale (PVDS, see Table 3 for the items.) was used for the first time in the present study; therefore, a confirmatory factor analysis (CFA) was carried out. Results of the CFA (χ2[64]=53.302; relative χ2=0.83, p=.82, RMSEA=.00 [95% CI .00, .02], CFI=1.00, TLI =1.02, SRMR=.05) indicated the scale as valid and reliable for assessing perceived infectability and germ aversion. Moreover, analysis (χ2[68]=77.53; relative χ2=1.14, p=.20, RMSEA=.02 [95% CI .00, .04], CFI=.99, TLI =.98, SRMR=0.07) also indicated that the perceived infectability and germ aversion scales can be used together as a unidimensional perceived vulnerability scale.
Table 3.
The items of the Perceived Vulnerability to Disease Scale (Duncan et al., 2009) and their French translation
|
Items (French translation) | |
|
Item 1. It really bothers me when people sneeze without covering their mouths. (Cela me dérange beaucoup lorsque les gens éternuent sans se couvrir la bouche.) | |
|
Item 2. If an illness is ‘going around’, I will get it. (Si une maladie ‘circule’, je l’aurai.) | |
|
Item 3. I am comfortable sharing a water bottle with a friend. (Cela ne me dérange pas de partager ma bouteille avec un ami.) | |
|
Item 4. I do not like to write with a pencil someone else has obviously chewed on. (Je n’aime pas écrire avec un stylo que quelqu’un d’autre a de toute évidence mâchouillé.) | |
|
Item 5. My past experiences make me believe I am not likely to get sick even when my friends are sick. (D’après mes expériences précédentes, je sais que je suis moins susceptible de tomber malade même si mes amis le sont.) | |
|
Item 6. I have an history of susceptibility to infectious disease. (J’ai des prédispositions au développement de maladies infectieuses.) | |
|
Item 7. I prefer to wash my hands pretty soon after shaking someone’s hand. (Je préfère me laver les mains assez rapidement après avoir serré la main de quelqu’un.) | |
|
Item 8. In general, I am very susceptible to colds, flu and other infectious diseases. (En général, je suis très sujet(te) aux rhumes, grippes et autres maladies infectieuses. | |
|
Item 9. I dislike wearing used clothes because you do not know what the last person who wore it was like. (Je n’aime pas porter des vêtements d’occasion car on ne sait pas à quoi la personne qui les as | |
| portés ressemblait.) | |
|
Item 10. I am more likely than the people around me to catch an infectious disease. (Je suis plus susceptible que les personnes qui m’entourent d’attraper une maladie infectieuse.) | |
|
Item 11. My hands do not feel dirty after touching money. (Je n’ai pas l’impression d’avoir les mains sales après avoir touché de l’argent.) | |
|
Item 12. I am unlikely to catch a cold, flu or other illness, even if it is ‘going around’. (Il est peu probable que j’attrape un rhume, une grippe ou une autre maladie même si celle-ci circule activement.) | |
|
Item 13. It does not make me anxious to be around sick people. (Je ne suis pas anxieux(se) si je suis entouré(e) de personnes malades.) | |
|
Item 14. My immune system protects me from most illnesses that other people get. (Mon système immunitaire me protège de la plupart des maladies dont souffrent les autres personnes.) | |
|
Item 15. I avoid using public telephones because of the risk that I may catch something from the previous user. (J’évite d’utiliser les téléphones publics (ou celui de quelqu’un d’autre que je ne connais pas) car je risque d’être contaminé(e)par les microbes de l’utilisateur précédent.) |
Note that the items 2, 5, 6, 8, 10, 12, and 14 belong to the perceived infectability factor whereas the items 1, 3, 4, 7, 9, 11, 13, and 15 belong to the germ aversion factor
Author Contribution
A. Carre (AC) and M. Mailliez (MM) designed the study. Material preparation and data collection were performed by MM and AC. Analysis was performed MM and supervised by AC. The first draft of the manuscript was written by MM and then shared with M.D. Griffiths (MDG) and AC for critical analysis and re-writing of the manuscript. The manuscript then went through a number of iterations. Finally, the three authors read and approved the manuscript.
Declarations
Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ahorsu, D. K., Lin, C.-Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (2020). The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction. 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed]
- Alyami M, Henning M, Krägeloh CU, Alyami H. Psychometric evaluation of the Arabic version of the fear of COVID-19 scale. International Journal of Mental Health and Addiction. 2020;16:1–14. doi: 10.1007/s11469-020-00316-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbisch D, Koenig KL, Shih FY. Is there a case for quarantine ? Perspectives from SARS to Ebola. Disaster Medicine and Public Health Preparedness. 2015;9(5):547–553. doi: 10.1017/dmp.2015.38. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037//0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88(3):588–606. doi: 10.1037/0033-2909.88.3.588. [DOI] [Google Scholar]
- Bitan, D. T., Grossman-Giron, A., Bloch, Y., Mayer, Y., Shiffman, N., & Mendlovic, S. (2020). Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Research, 289, 113100. 10.1016/j.psychres.2020.113100. [DOI] [PMC free article] [PubMed]
- Bollen KA. Issues in the comparative measurement of political democracy. American Sociological Review. 1980;45(3):370–390. doi: 10.2307/2095172. [DOI] [Google Scholar]
- Broche-Pérez, Y., Fernández-Fleites, Z., Jiménez-Puig, E., Fernández-Castillo, E., & Rodríguez-Martin, B. C. (2020). Gender and fear of COVID-19 in a Cuban population sample. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00343-8. [DOI] [PMC free article] [PubMed]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, T. A. (2015). Confirmatory factor analysis for applied research. Guilford Publications.
- Bruchon-Schweitzer, M., & Paulhan, I. (1993). Manuel Francais de l’échelle d’anxiété-trait et d’anxiété -état de Spielberger.
- Carbone SR. Flattening the curve of mental ill-health: The importance of primary prevention in managing the mental health impacts of COVID-19. Mental Health & Prevention. 2020;19:200185. doi: 10.1016/j.mhp.2020.200185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carre, A., Luquiens, A., Metral, M., & Morvan, Y. (2020). Covid-19: Quelles conséquences sur la santé mentale ? The Conversation. http://theconversation.com/covid-19-quelles-consequences-sur-la-sante-mentale-137242.
- CDC Centers for Disease Control and Prevention (2020). Coronavirus disease 2019 (COVID-19). Centers for Disease Control and Prevention. Retrieved November 23, 2020, from: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html.
- Chang, K.-C., Hou, W.-L., Pakpour, A. H., Lin, C.-Y., & Griffiths, M. D. (2020). Psychometric testing of three COVID-19-related scales among people with mental lllness. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00361-6. [DOI] [PMC free article] [PubMed]
- Coelho CM, Suttiwan P, Arato N, Zsido AN. On the nature of fear and anxiety triggered by COVID-19. Frontiers in Psychology. 2020;11:581314. doi: 10.3389/fpsyg.2020.581314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Core Team, R. (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing https://www.Rproject.org/.
- Doshi, D., Karunakar, P., Sukhabogi, J. R., Prasanna, J. S., & Mahajan, S. V. (2020). Assessing coronavirus fear in Indian population using the Fear of COVID-19 Scale. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00332-x. [DOI] [PMC free article] [PubMed]
- Duncan LA, Schaller M, Park JH. Perceived vulnerability to disease : Development and validation of a 15-item self-report instrument. Personality and Individual Differences. 2009;47(6):5411546–5411546. doi: 10.1016/j.paid.2009.05.001. [DOI] [Google Scholar]
- Elemo, A. S., Satici, S. A. & Griffiths, M. D. (2020). The Fear of COVID-19 Scale: Psychometric properties of the Ethiopian Amharic version. International Journal of Mental Health and Addiction, in press. [DOI] [PMC free article] [PubMed]
- Erku DA, Belachew SA, Abrha S, Sinnollareddy M, Thomas J, Steadman KJ, Tesfaye WH. When fear and misinformation go viral: Pharmacists’ role in deterring medication misinformation during the « infodemic » surrounding COVID-19. Research in Social and Administrative Pharmacy. 2020;17:1954–1963. doi: 10.1016/j.sapharm.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Reyna, B., Castillo-García, G. D., Barbosa-Camacho, F. J., Cervantes-Cardona, G. A., Cervantes-Pérez, E., Torres-Mendoza, B. M., Fuentes-Orozco, C., Pintor-Belmontes, K. J., Guzmán-Ramírez, B. G., Hernández-Bernal, A., González-Ojeda, A., & Cervantes-Guevara, G. (2020). Fear of COVID-19 Scale for hospital staff in regional hospitals in Mexico: A brief report. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00413-x.
- Griffiths, M. D. & Mamun, M. A. (2020). COVID-19 suicidal behavior among couples and suicide pacts: Case study evidence from press reports. Psychiatry Research, 289, 113105. 10.1016/j.psychres.2020.113105 [DOI] [PubMed]
- Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health- related quality of life measures: Literature review and proposed guidelines. Journal of Clinical Epidemiology. 1993;46(12):1417–1432. doi: 10.1016/0895-4356(93)90142-n. [DOI] [PubMed] [Google Scholar]
- Gunnell, D., Appleby, L., Arensman, E., Hawton, K., John, A., Kapur, N., Khan, M., O’Connor, R. C., Pirkis, J., Appleby, L., Arensman, E., Caine, E. D., Chan, L. F., Chang, S.-S., Chen, Y.-Y., Christensen, H., Dandona, R., Eddleston, M., Erlangsen, A., et al. (2020). Suicide risk and prevention during the COVID-19 pandemic. The Lancet Psychiatry. Advance online publication. 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed]
- Hair, J. F., Babin, B. J., Anderson, R. E., & Black, W. C. (2014). Multivariate data analysis (7th ed.). Cengage Learning. 10.1002/9781119409137.ch4.
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Huarcaya-Victoria, J., Villarreal-Zegarra, D., Podestà, A., & Luna-Cuadros, M. A. (2020). Psychometric properties of a Spanish version of the Fear of COVID-19 Scale in general population of Lima, Peru. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00354-5. [DOI] [PMC free article] [PubMed]
- Izard CE, Libero DZ, Putnam P, Haynes OM. Stability of emotion experiences and their relations to traits of personality. Journal of Personality and Social Psychology. 1993;64(5):847–860. doi: 10.1037/0022-3514.64.5.847. [DOI] [PubMed] [Google Scholar]
- Kaya S, Uzdil Z, Cakiroğlu FP. Evaluation of the effects of fear and anxiety on nutrition during the COVID-19 pandemic in Turkey. Public Health Nutrition. 2020;24:282–289. doi: 10.1017/S1368980020003845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konstantinov, V., Berdenova, S., Satkangulova, G., Reznik, A., & Isralowitz, R. (2020). COVID-19 impact on Kazakhstan University student fear, mental health, and substance use. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00412-y. [DOI] [PMC free article] [PubMed]
- Kontoangelos K, Economou M, Papageorgiou C. Mental health effects of COVID-19 pandemia: A review of clinical and psychological traits. Psychiatry Investigation. 2020;17(6):491–505. doi: 10.30773/pi.2020.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SA, Crunk EA. Fear and psychopathology during the COVID-19 crisis: Neuroticism, hypochondriasis, reassurance-seeking, and coronaphobia as fear factors. OMEGA - Journal of Death and Dying. 2020;0030222820949350:003022282094935. doi: 10.1177/0030222820949350. [DOI] [PubMed] [Google Scholar]
- Lin C-Y. Social reaction toward the 2019 novel coronavirus (COVID-19) Social Health and Behavior. 2020;3(1):1. doi: 10.4103/SHB.SHB_11_20. [DOI] [Google Scholar]
- Mahmood, Q. K., Jafree, S. R., & Qureshi, W. A. (2020). The psychometric validation of FCV-19S in Urdu and socio-demographic association with fear in the people of the Khyber Pakhtunkhwa (KPK) province in Pakistan. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00371-4. [DOI] [PMC free article] [PubMed]
- Mamun MA, Sakib N, Gozal D, Bhuiyan AI, Hossain S, Bodrud-Doza M, Al Mamun F, Hosen I, Safiq MB, Abdullah AH, Sarker MA, Rayhan I, Sikder MT, Muhit M, Lin C-Y, Griffiths MD, Pakpour AH. The COVID-19 pandemic and serious psychological consequences in Bangladesh: A population-based nationwide study. Journal of Affective Disorders. 2021;279:462–472. doi: 10.1016/j.jad.2020.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez-Lorca M, Martínez-Lorca A, Criado-Álvarez JJ, Armesilla MDC, Latorre JM. The Fear of COVID-19 scale : Validation in Spanish university students. Psychiatry Research. 2020;293:113350. doi: 10.1016/j.psychres.2020.113350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masuyama, A., Shinkawa, H., & Kubo, T. (2020). Validation and psychometric properties of the Japanese version of the Fear of COVID-19 Scale among adolescents. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00368-z. [DOI] [PMC free article] [PubMed]
- Morin, A. J. S., Myers, N. D., & Lee, S. (2020). Modern factor analytic techniques. In G. Tenenbaum & R. C. Eklund (Eds.), Handbook of sport psychology (pp. 1044–1073). John Wiley & Sons. 10.1002/9781119568124.ch51.
- Nunnally, J. C. (1978). Psychometric theory (2nd ed.). McGraw-Hill.
- Ornell F, Schuch JB, Sordi AO, Kessler FHP, Ornell F, Schuch JB, Sordi AO, Kessler FHP. “Pandemic fear” and COVID-19: Mental health burden and strategies. Brazilian Journal of Psychiatry. 2020;42(3):232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pakpour AH, Griffiths MD. The fear of COVID-19 and its role in preventive behaviors. Journal of Concurrent Disorders. 2020;2(1):58–63. doi: 10.54127/WCIC8036. [DOI] [Google Scholar]
- Pang, N. T. P., Kamu, A., Hambali, N. L. B., Mun, H. C., Kassim, M. A., Mohamed, N. H., Ayu, F., Rahim, S. S. S. A., Omar, A., & Jeffree, M. S. (2020). Malay version of the Fear of COVID-19 Scale : Validity and reliability. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00355-4. [DOI] [PMC free article] [PubMed]
- Pappas, G., Kiriaze, I. J., Giannakis, P., & Falagas, M. E. (2009). Psychosocial consequences of infectious diseases. Clinical Microbiology and Infection, 15(8), 743–747. 10.1111/j.1469-0691.2009.02947.x. [DOI] [PMC free article] [PubMed]
- Perz, C. A., Lang, B. A., & Harrington, R. (2020). Validation of the Fear of COVID-19 Scale in a US College sample. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00356-3. [DOI] [PMC free article] [PubMed]
- Rahman MA, Hoque N, Alif SM, Salehin M, Islam SMS, Banik B, Sharif A, Nazim NB, Sultana F, Cross W. Factors associated with psychological distress, fear and coping strategies during the COVID-19 pandemic in Australia. Globalization and Health. 2020;16:95. doi: 10.1186/s12992-020-00624-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raony Í, de Figueiredo CS, Pandolfo P, Giestal-de-Araujo E, Oliveira-Silva Bomfim P, Savino W. Psycho-neuroendocrine-immune interactions in COVID-19 : Potential impacts on mental health. Frontiers in Immunology. 2020;11:1170. doi: 10.3389/fimmu.2020.01170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raykov T. Estimation of congeneric scale reliability using covariance structure analysis with nonlinear constraints. British Journal of Mathematical and Statistical Psychology. 2001;54(2):315–323. doi: 10.1348/000711001159582. [DOI] [PubMed] [Google Scholar]
- Razavi, D., Delvaux, N., Farvacques, C., & Robaye, E. (1989). Validation de la version française du HADS dans une population de patients cancéreux hospitalisés [Validation of the French version of the Hospital Anxiety and Depression Scale (HADS) in a population of hospitalized cancer patients]. Revue de Psychologie Appliquée, 39(4), 295–307.
- Revathishree, K., Shyam Sudhakar, S., Indu, R., & Srinivasan, K. (2020). Covid-19 demographics from a tertiary care center: Does it depreciate quality-of-life? Indian Journal of Otolaryngology and Head & Neck Surgery. Advance online publication. 10.1007/s12070-020-02144-w. [DOI] [PMC free article] [PubMed]
- Reznik, A., Gritsenko, V., Konstantinov, V., Khamenka, N., & Isralowitz, R. (2020). COVID-19 fear in Eastern Europe: Validation of the Fear of COVID-19 Scale. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00283-3. [DOI] [PMC free article] [PubMed]
- Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, Zandi MS, Lewis G, David AS. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. The Lancet Psychiatry. 2020;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakib, N., Bhuiyan, A. K. M. I., Hossain, S., Al Mamun, F., Hosen, I., Abdullah, A. H., Sarker, M. A., Mohiuddin, M. S., Rayhan, I., Hossain, M., Sikder, M. T., Gozal, D., Muhit, M., Islam, S. M. S., Griffiths, M. D., Pakpour, A. H., & Mamun, M. A. (2020). Psychometric validation of the Bangla Fear of COVID-19 Scale: Confirmatory factor analysis and Rasch analysis. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00289-x. [DOI] [PMC free article] [PubMed]
- Satici, B., Gocet-Tekin, E., Deniz, M. E., & Satici, S. A. (2020). Adaptation of the Fear of COVID-19 Scale: Its association with psychological distress and life satisfaction in Turkey. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00294-0. [DOI] [PMC free article] [PubMed]
- Schumacker, R. E., & Lomax, R. G. (2010). A beginner’s Guide to structural equation Modeling (2nd ed.). Taylor & Francis.
- Shultz, J. M., Cooper, J. L., Baingana, F., Oquendo, M. A., Espinel, Z., Althouse, B. M., Marcelin, L. H., Towers, S., Espinola, M., McCoy, C. B., Mazurik, L., Wainberg, M. L., Neria, Y., & Rechkemmer, A. (2016). The role of fear-related behaviors in the 2013–2016 West Africa ebola virus disease outbreak. Current Psychiatry Reports, 18(11), 104. 10.1007/s11920-016-0741-y. [DOI] [PMC free article] [PubMed]
- Sigorski D, Sobczuk P, Osmola M, Kuć K, Walerzak A, Wilk M, Ciszewski T, Kopeć S, Hryń K, Rutkowski P, Stec R, Szczylik C, Bodnar L. Impact of COVID-19 on anxiety levels among patients with cancer actively treated with systemic therapy. ESMO Open. 2020;5(5):e000970. doi: 10.1136/esmoopen-2020-000970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soraci, P., Ferrari, A., Abbiati, F. A., Del Fante, E., De Pace, R., Urso, A., & Griffiths, M. D. (2020). Validation and psychometric evaluation of the Italian version of the Fear of COVID-19 Scale. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00277-1. [DOI] [PMC free article] [PubMed]
- Spielberger, C. D., Gorsuch, R. L., Lushene, R., Vagg, P. R., & Jacobs, G. A. (1983). Manual for the state-trait anxiety inventory. Consulting Psychologists Press.
- Steiger JH. A note on multiple sample extensions of the RMSEA fit index. Structural Equation Modeling. 1998;5(4):411–419. doi: 10.1080/10705519809540115. [DOI] [Google Scholar]
- Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62354 COVID-19 cases in the USA. The Lancet Psychiatry. 2020;8:130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Landry CA, Paluszek MM, Rachor GS, Asmundson GJG. Worry, avoidance, and coping during the COVID-19 pandemic: A comprehensive network analysis. Journal of Anxiety Disorders. 2020;76:102327. doi: 10.1016/j.janxdis.2020.102327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry. 2020;66:317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Tsipropoulou, V., Nikopoulou, V. A., Holeva, V., Nasika, Z., Diakogiannis, I., Sakka, S., Kostikidou, S., Varvara, C., Spyridopoulou, E., & Parlapani, E. (2020). Psychometric properties of the Greek version of FCV-19S. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00319-8. [DOI] [PMC free article] [PubMed]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38(1):1–10. doi: 10.1007/BF02291170. [DOI] [Google Scholar]
- Tzur Bitan D, Grossman-Giron A, Bloch Y, Mayer Y, Shiffman N, Mendlovic S. Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Research. 2020;289:113100. doi: 10.1016/j.psychres.2020.113100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman JB. Structural equation modeling: Reviewing the basics and moving forward. Journal of Personality Assessment. 2006;87(1):35–50. doi: 10.1207/s15327752jpa8701_03. [DOI] [PubMed] [Google Scholar]
- Wakashima K, Asai K, Kobayashi D, Koiwa K, Kamoshida S, Sakuraba M. The Japanese version of the Fear of COVID-19 Scale: Reliability, validity, and relation to coping behavior. PLoS One. 2020;15(11):e0241958. doi: 10.1371/journal.pone.0241958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, Debien C, Molenda S, Horn M, Grandgenèvre P, Notredame C-E, D’Hondt F. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Network Open. 2020;3(10):e2025591. doi: 10.1001/jamanetworkopen.2020.25591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winter, T., Riordan, B. C., Pakpour, A. H., Griffiths, M. D., Mason, A., Poulgrain, J. W., & Scarf, D. (2020). Evaluation of the English version of the Fear of COVID-19 Scale and its relationship with behavior change and political beliefs. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00342-9. [DOI] [PMC free article] [PubMed]
- World Health Organization (2020). Mental health and COVID-19. Retrieved November 23, 2020, from: https://www.who.int/teams/mental-health-and-substance-use/covid-19.
- Worldometer (2020). Coronavirus cases. Retrieved November 23, 2020, from: https://www.worldometers.info/coronavirus/
- Wu, Y., Xu, X., Chen, Z., Duan, J., Hashimoto, K., Yang, L., Liu, C., & Yang, C. (2020). Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain, Behavior, and Immunity, 87, 18–22. 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed]
- Yehudai, M., Bender, S., Gritsenko, V., Konstantinov, V., Reznik, A., & Isralowitz, R. (2020). COVID-19 fear, mental health, and substance misuse conditions among university social work students in Israel and Russia. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00360-7. [DOI] [PMC free article] [PubMed]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]