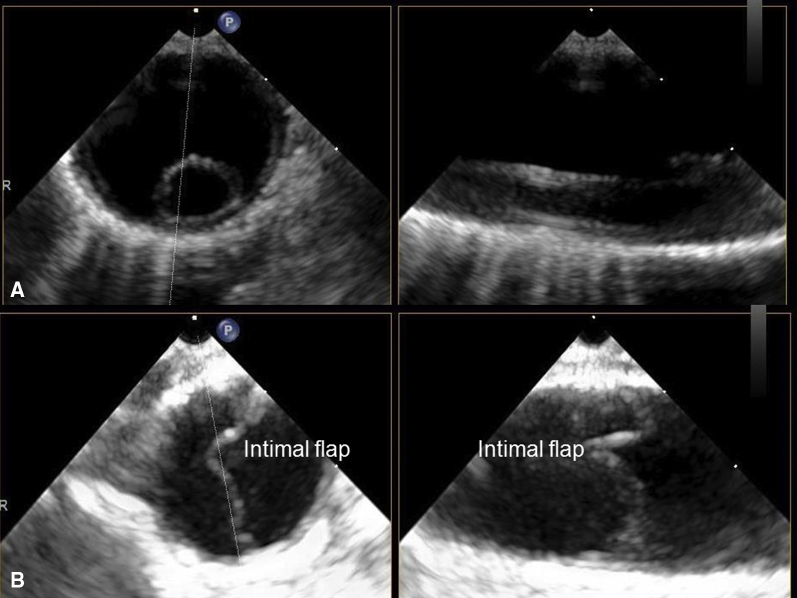
Thrombus cast (A) and type B aortic dissection and intimal flap (B).
Central Message.
All physicians dealing with patients on extracorporeal membrane oxygenation must pay attention to the arterial cannula position.
See Commentaries on pages 88 and 90.
Extracorporeal membrane oxygenation (ECMO) is a valuable, life-saving modality for patients in shock. Some complications associated with ECMO are well known. We describe a case of simultaneous aortic thrombosis and acute type B aortic dissection (AD) caused by an arterial cannula placed in the descending aorta.
Clinical Summary
A 49-year-old woman with a previous mitral commissurotomy via thoracotomy was admitted to another hospital due to heart failure, severe mixed rheumatic mitral disease, and left ventricular ejection function of 45% with normal right ventricular function. Coronary angiography showed normal coronary arteries.
She underwent redo mechanical mitral valve replacement and maze procedure for atrial fibrillation. At surgery, the right ventricle was lacerated on entry. She was sent to the intensive care unit with high-dose inotropic and vasopressor supports. She remained hemodynamically unstable and the next day was taken back to the operating room to relieve tamponade, and an intra-aortic balloon pump was inserted. Hemodynamic instability persisted; therefore, central venoarterial (VA)-ECMO was initiated with cannulas in the right atrium, ascending aorta, and right superior pulmonary vein for venting.
Her coronary arteries were reassessed and were widely patent. Transesophageal echocardiography showed no evidence of ascending or descending AD and thrombosis. She was transferred to our hospital for ongoing care.
Chest radiograph on arrival showed the tip of the aortic cannula in the descending aorta (Figure 1). Her heart improved and 6 days later she was successfully decannulated. The aortic EOPA (Medtronic Corp, Minneapolis, Minn) cannula had been placed in the distal ascending aorta and placed deeply to the transition zone so that the tip was indeed in the descending aorta. The cannulation technique and methods of confirmation of positioning performed at another hospital were not described in the operative note.
Figure 1.
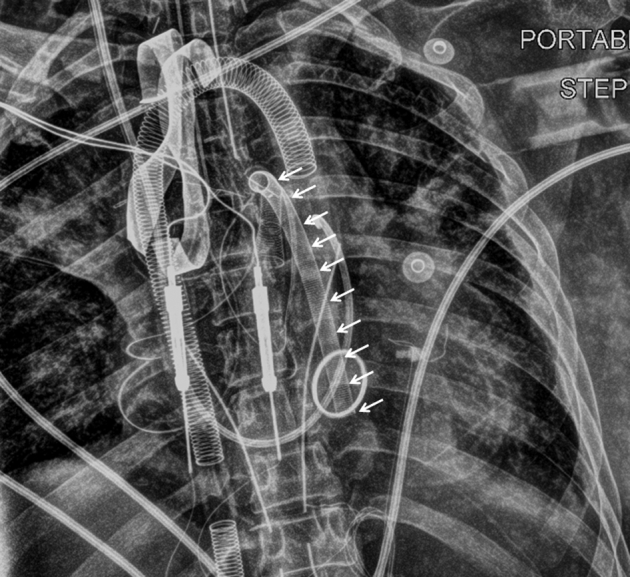
Chest radiograph on admission to our hospital. The patient was intubated and supported on both central extracorporeal membrane oxygenation and intra-aortic balloon pump. White arrows indicate the entire arterial cannula placed in the descending aorta. A mechanical mitral valve is also seen at the tip of the cannula.
While the patient was on ECMO, activated partial thromboplastin time was maintained between 40 and 60 seconds. Postoperatively, her creatinine rose from 92 to 280 mmol/dL. Transesophageal echocardiography revealed a thrombotic cast where the aortic cannula was along with an intimal flap suggestive of type B AD (Figure 2, A and B and see Video 1). Abdominal ultrasound confirmed that the intimal flap was confined to the thorax. Computed tomography was not used due to the elevated creatinine and further damage related to contrast. Computed tomography of the brain revealed a cerebral infarct in the posterior limb of the right middle cerebral artery without evidence of hemorrhage. Anticoagulation was initiated, and medical management for the type B AD was commenced. She was discharged from the hospital with normal cardiac, renal, and neurologic recovery.
Video 1.

Summary of our case report including aortic cannulation and imaging findings. Video available at: https://www.jtcvs.org/article/S2666-2507(20)30645-3/fulltext.
Figure 2.
Postoperative transesophageal echocardiography shows (A) thrombus cast where the arterial cannula is in the descending aorta and (B) type B aortic dissection and intimal flap confirmed by the short- and long-axial views. The intimal flap is confined to thorax and not observed at the site of the aortic cannulation (ascending aorta). The intimal flap does not cover the visceral arteries, either.
Discussion
Peripheral VA-ECMO has been preferred to central VA-ECMO because of its easy and quick institution, less invasiveness, and no need for surgical exposure of the heart and great vessels.1 Peripheral VA-ECMO has been associated with a significant reduction in the risk for bleeding, continuous venovenous hemofiltration, and requirement of any blood production compared with central VA-ECMO.2 Incidence rates of stroke and 30-day mortality between both central and peripheral ECMO are not statistically significant different. In terms of vascular complications, central ECMO is beneficial over peripheral ECMO.1 Despite these studies, central ECMO is often used in postcardiotomy shock because the heart and great vessels are already exposed and the cannulas are already there.
There are life-threatening issues associated with ECMO.3 Although activated partial thromboplastin time, activated clotting time, or international normalized ratio were maintained appropriately in those cases, a fatal thrombosis formed. The incidence rate of iatrogenic type A AD associated with aortic cannulation was reported to be 0.048% (5/10,360).4 Our case showed both thrombosis and acute type B AD due to an arterial cannula placed in the descending aorta.
We assume that jet injury from the tip of the cannula being directly against the aortic wall and relative stagnant retrograde flow or the long thrombotic surface around the long arterial cannula caused the 2 critical complications. Given that the patient had open heart surgery, the acute cerebral infarction may have been primary or secondary to embolism of a small embolic thrombus from the cannula or even aortic atherosclerotic debris from the retrograde aorta to cerebral perfusion, given the tip of the cannula was in the descending aorta.
Care taken in the placement of the aortic cannula may prevent complications that may be life-threatening. The cannula tip must be kept in the ascending aorta or proximal arch to allow for antegrade flow of blood and not be advanced too far so that the amount of thrombotic material in the bloodstream is at a minimum. Maintaining antegrade flow will also diminish potential atherosclerotic debris, often starting in the aortic arch, being embolized to the brain.
Footnotes
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Supplementary Data
Summary of our case report including aortic cannulation and imaging findings. Video available at: https://www.jtcvs.org/article/S2666-2507(20)30645-3/fulltext.
References
- 1.Ranney D.N., Benrashid E., Meza J.M., Keenan J.E., Bonadonna D.K., Bartz R. Central cannulation as a variable alternative to peripheral cannulation in extracorporeal membrane oxygenation. Semin Thorac Surg. 2017;29:188–195. doi: 10.1053/j.semtcvs.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 2.Raffa G.M., Kowalewski M., Brodie D., Ogino M., Whitman G., Meani P. Meta-analysis of peripheral or central extracorporeal membrane oxygenation in postcardiotomy and non-postcardiotomy shock. Ann Thorac Surg. 2019;107:311–321. doi: 10.1016/j.athoracsur.2018.05.063. [DOI] [PubMed] [Google Scholar]
- 3.Burrell A.J.C., Bennett V., Serra A.L., Pellegrino V.A., Romero L., Fan E., for the international ECMO Network (ECMONet) Venoarterial extracorporeal membrane oxygenation: a systemic review of selection criteria, outcome measures and definitions of complications. J Crit Care. 2019;53:32–37. doi: 10.1016/j.jcrc.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 4.Narayan P., Angelini G.D., Bryan A.J. Iatrogenic intraoperative type A aortic dissection following cardiac surgery. Asian Cardiovasc Thorac Ann. 2015;23:31–35. doi: 10.1177/0218492314531140. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Summary of our case report including aortic cannulation and imaging findings. Video available at: https://www.jtcvs.org/article/S2666-2507(20)30645-3/fulltext.