Abstract
Reactive oxygen species (ROS) generated at low levels during mitochondrial respiration have key roles in several signaling pathways. Oxidative stress (OS) arises when the generation of ROS exceeds the cell’s antioxidant scavenging ability and leads to cell damage. Physiological ROS production in spermatozoa regulates essential functional characteristics such as motility, capacitation, acrosome reaction, hyperactivation, and sperm-oocyte fusion. OS can have detrimental effects on sperm function through lipid peroxidation, protein damage, and DNA strand breakage, which can eventually affect the fertility of an individual. Substantial evidence in the literature indicates that spermatozoa experiencing OS during in vitro manipulation procedures in human- and animal-assisted reproduction are increasingly associated with iatrogenic ROS production and eventual impairment of sperm function. Although a direct association between sperm OS and human assisted reproductive techniques (ART) outcomes after in vitro fertilization (IVF) and/or intracytoplasmic sperm injection (ICSI) is still a matter of debate, studies in animal models provide enough evidence on the adverse effects of sperm OS in vitro and defective fertilization and embryo development. This review summarized the literature on sperm OS in vitro, its effects on functional ability and embryo development, and the approaches that have been proposed to reduce iatrogenic sperm damage and altered embryonic development.
Keywords: spermatozoa, male infertility, oxidative stress, assisted reproductive technologies, embryo development
1. Introduction
Infertility, defined by the World Health Organization (WHO), as the inability to achieve pregnancy within 12 months of regular unprotected sexual intercourse, affects approximately 15% of couples, out of which a male factor is responsible for approximately half of the cases [1,2]. The causes of male infertility are numerous, and includes genetic causes such as Y-chromosome deletions in severe oligozoospermic and non-obstructive azoospermic men, varicocele, infections of the male reproductive tract, presence of anti-sperm antibodies, non-obstructive and obstructive azoospermia, and hypogonadism [3]. About 15% of infertile men have unexplained infertility as no defects are observed after routine semen analysis [4]. Moreover, 30–50% of male infertility cases are idiopathic as routine semen analysis has no identifiable etiology, and a female factor seems to be absent [5,6,7]. Indeed, the incidence of male infertility oscillates in a wide range (5–35%) due to multifactorial differences among the patient’s populations [8,9].
Although it is widely accepted that a semen profile based on sperm number, motility, and morphology according to the WHO is fundamental in the evaluation and treatment of the infertile couple, its predictive value on the fertilizing ability, either in vivo or in vitro, is limited. Oxidative stress (OS) and sperm DNA damage have shown a strong association with several forms of male infertility. In fact, about 30–80% of infertile men have elevated levels of reactive oxygen species (ROS) and lower antioxidant capacity in their ejaculate [10,11,12]. Hence, the term Male Oxidative Stress Infertility (MOSI) has been recently introduced to describe infertile men with abnormal semen characteristics and OS, including many patients previously classified as infertile idiopathic males [13]. Indeed, controlled production of ROS in spermatozoa has a physiological role in redox signaling and drives fundamental events in spermatozoa such as the activation of motility, transient sperm-oviduct adhesion, capacitation, hyperactivation, acrosome reaction, and sperm oocyte fusion [14,15,16,17,18]. On the other hand, when semen ROS levels exceed the antioxidant’s defense, a status of oxidative stress is generated. OS plays a crucial role in a wide range of diseases, including infertility, and is also clearly influenced by environmental and lifestyle factors. It may impair not only female and male reproductive health but also exert epigenetic effects on the offspring [19]. Spermatozoa are vulnerable to OS due to their high content of polyunsaturated fatty acids (PUFA), deficiencies in intracellular antioxidant enzymes, and limited DNA repair ability. ROS cause impairment in male fertility by damaging the sperm membrane via lipid peroxidation with consequent reduction of sperm motility, sperm-oocyte fusion [20,21], and the sperm DNA integrity, thus compromising the paternal genomic contribution to the embryo [22,23,24,25]. Sperm DNA damage, in most cases is believed to be oxidative in nature and associated with reduced fertilization rates, impaired preimplantation development, increased incidence of miscarriage, and fetal loss [11,26,27,28,29,30,31]. Although several mechanisms are known to induce DNA damage during spermatogenesis and epididymal maturation, sperm DNA can also be damaged post-ejaculation.
ART outcome, including fertilization and clinical pregnancy rates, are influenced by multiple factors, among which sperm OS plays a significant role. Sperm oxidative DNA damage, if left unrepaired after fertilization, can compromise embryo development or transmit genetic mutations to the offspring [9]. During in vitro handling, spermatozoa experience altered microenvironments, shearing forces, and a wide spectrum of exogenous factors which are different from the specific physicochemical microenvironments they sequentially encounter during their journey within the female reproductive tract. The regulation of ROS levels within physiological concentrations during sperm handling in ART represents a crucial factor in optimizing its clinical efficiency. The laboratory interventions such as sperm handling, washing techniques, and cryopreservation could generate or increase the status of OS in spermatozoa, and this could be a concern, especially when ROS levels and/or DNA damage in the basal semen are elevated.
This manuscript aims to review the literature on sperm OS during in vitro handling in ART, its effects on sperm function and embryo development, and the remedies that have been proposed to reduce iatrogenic sperm damage and impairment of embryo development.
2. Sources of ROS in Spermatozoa
Various sources in spermatozoa produce ROS such as superoxide (O2•−) [22,32], hydrogen peroxide (H2O2) [22], nitric oxide [33], and peroxynitrite [34]. Mitochondria represent one of the main ROS sources in spermatozoa [18]. Production of mitochondrial ROS is due to the leakage of electrons from the electron transport chain (ETC), which are then accepted by molecular oxygen (O2) producing O2•− [35,36]. ROS also results from the mitochondrial apoptotic pathway, which has been reported to be activated by the dysfunction of the phosphoinositide signaling pathway [37]. Moreover, mitochondrial membranes are rich in PUFA that represent preferential substrates for ROS, triggering lipid peroxidation and the generation of highly reactive lipid aldehydes. These covalently bind to ETC proteins, reinforcing the production of mitochondrial ROS in a self-perpetuating cycle, and compromise both the competence and the DNA integrity of the spermatozoa [38,39,40]. The fact that unesterified unsaturated fatty acids are powerful ROS inducers in human spermatozoa also indicates a role for lipoxygenase in this process [41].
Several lines of evidence in different species support the role of the hexose monophosphate shunt pathway in ROS generation by spermatozoa [42,43]. In human spermatozoa, ROS production has been highly correlated with the presence of glucose-6-phosphate-dehydrogenase, a key enzyme in the control of hexose monophosphate shunt activity [44]. Among NADPH oxidases involved in ROS production in phagocytes [45], a novel isoform of NADPH oxidase 5 (NOX5) localized in the membrane, activated by binding of calcium ions (Ca2+) and involved in the production of O2•− and H2O2, has been detected in the acrosome, neck, and tail of human spermatozoa [46,47]. Nitric oxide synthase and other non-enzymatic mechanisms have also been proposed to participate in the production of nitric oxide [48,49].
3. Roles of ROS in Sperm Physiology
Ejaculated spermatozoa move along the female reproductive tract until they reach the oviductal ampulla to fertilize the oocyte. Redox signaling through the production of low levels of ROS is involved in several sperm physiological processes such as transient sperm-oviduct adhesion, capacitation, hyperactivation, acrosome reaction, and the membrane fusion with the oocyte. The two main events that orchestrate the physiological changes associated with sperm capacitation are the activation of Src family kinases with the consequent inhibition of serine/threonine (Ser/Thr) phosphatases and the activation of the cAMP pathways by bicarbonate and Ca2+. Downstream changes such as the increase in intracellular pH and membrane hyperpolarization have been hypothesized to increase intracellular Ca2+ through the modulation of specific sperm channels. Such an increase is essential for inducing sperm hyperactivation, acrosome reaction, and developing the ability to fertilize the oocyte [50]. Redox regulation of the thiol groups of cysteine residues is necessary to regulate different sperm proteins associated with capacitation [51]. In several species, spermatozoa transiently adhere to the epithelial cells lining the isthmic portion of the oviductal epithelium [52]. This adhesion selects high-quality spermatozoa and maintains their fertilizing ability until periovulatory release, which allows their migration toward the oviductal ampulla for fertilization [53]. Several pieces of evidence indicate that selected spermatozoa are not capacitated, and that capacitation allows their release from the oviductal reservoir. The quantity of sperm surface thiols has been shown to increase during capacitation [51], and the level of thiols in sperm-surface proteins modulates the ability of bovine spermatozoa to adhere to and be released from the oviduct in vitro and their capacitation status [15,17].
Concentrations of O2•−, H2O2, nitric oxide, and peroxynitrite are progressively increased during the entire course of capacitation [32,54]. An early event of capacitation regulated by ROS is the activation of adenylate cyclase by O2•− and nitric oxide, which drives the increase of intracellular cyclic adenosine monophosphate (cAMP), followed by the activation of protein kinase A (PKA), which is essential for the tyrosine phosphorylation of target proteins [55,56]. Later capacitation molecular events in which specific ROS are implicated include the mitogen-activated protein kinase (MEK), extracellular-regulated kinase (ERK), phosphoinositide-3 kinase/Akt (PI3K/Akt) pathways, and tyrosine phosphorylation [57,58,59,60].
Hyperactivation, a high amplitude, increased lateral head displacement, asymmetric flagellar movement, is part of capacitation and is required for successful sperm passage through the cumulus oophorus and the zona pellucida and for fertilization. This motility change depends on ROS-mediated tyrosine phosphorylation of flagellar proteins, and the simple exposure of capacitating spermatozoa to ROS increases hyperactivation [61,62].
The increase of membrane fluidity needed for induction of acrosome reaction and sperm-oocyte fusion is influenced by ROS. In fact, exposure of spermatozoa from several species to exogenous H2O2 was shown to induce both the acrosome reaction and the sperm-oocyte fusion [63,64,65]. In particular, exposure of human spermatozoa to H2O2 induces the acrosome reaction whereas, this is inhibited by the addition of catalase [66,67].
4. Effects of Oxidative Stress on Sperm Function
Spermatozoa are vulnerable to OS due to their high content of PUFA, deficiencies in intracellular antioxidant enzymes, and limited DNA repair ability. In particular, the high content of PUFA in the sperm plasma membrane regulates membrane fluidity but also represents a preferential substrate for ROS attack. In fact, lipid peroxidation of the sperm plasma membrane PUFA has been the first oxidative damage recognized in male infertility [22,68]. The highly reactive lipid aldehydes produced by peroxidation form adducts with proteins and DNA and induce sperm mitochondrial dysfunction through binding to ETC proteins. This reinforces the production of mitochondrial ROS and compromises both the competence and the DNA integrity of the spermatozoa [38,39,40], causing mutations in the sperm genome [9]. The generation of 4-hydroxynonenal-protein adducts has been associated with loss of membrane integrity, motility, and reduced fertility [69].
5. Origin and Consequences of DNA Damage in Ejaculated Spermatozoa
Three main mechanisms are currently considered for the induction of DNA damage in spermatozoa: abortive apoptosis during spermatogenesis [70], defective protamination during spermiogenesis, defective epididymal microenvironment, and OS. Among these, OS is considered to be the major cause of spermatozoa [24]. In fact, high ROS levels and decreased total antioxidant capacity are closely correlated to increased sperm DNA damage in infertile men [71,72,73,74]. ROS can directly damage DNA, generating oxidized DNA adducts such as 8-hydroxy-2-deoxyguanosine (8-OHdG), 1,N6-ethenoadenosine, and 1,N6-ethenoguanosine. In particular, 8-OHdG, caused by hydroxyl radicals, represents the most frequently generated adduct and is assessed as a marker of DNA oxidative damage in several studies [25,75].
Defective protamination renders the spermatozoa highly susceptible to oxidative DNA damage and DNA fragmentation [75]. DNA bases in the nucleus and mitochondria can also be deaminated, nitrated, or oxidated by nitric oxide [76]. 8OHdG is highly mutagenic if left unrepaired; it forms a stable base pair with adenine, resulting in G:C to T:A transversion mutations following DNA replication [77]. A critical enzyme of the base excision repair pathway, 8-oxoguanine DNA glycosylase 1 (OGG1), localized both in the mitochondria and nucleus of mature human spermatozoa, is able to excise 8OHdG, allowing the creation of an apurinic site and extracellular release of the adduct. However, human spermatozoa have a truncated base excision repair pathway as they lack the downstream components, apurinic endonuclease 1 (APE1), and X-ray repair complementing defective repair in Chinese hamster cells 1 (XRCC1) [78]. During oogenesis, the oocyte accumulates mRNA’s and proteins involved in base excision repair [79,80], and the apurinic sites in the sperm DNA can be repaired following fertilization by the zygote before the S-phase of the first mitotic division [81,82,83]. Although a remarkable acceleration of 8OHdG repair by the base excision repair pathway has been reported in the mouse oocyte following fertilization, OGG1 expression seems particularly low compared to male germ cells [77]. Therefore, spermatozoa carrying high levels of 8OHdG at the time of fertilization can undergo an incomplete DNA repair in the zygote, and this may impair the preimplantation embryo development [84] and fetal growth [85]. In addition, incomplete repair of sperm 8OHdG lesions has been linked to defects in offspring, including cancer and reduced lifespan [86,87]. Spermatozoa may also carry single- and double-strand DNA breaks (DSB), and the significance of the different methods to evaluate sperm DNA fragmentation has been recently reviewed elsewhere [88,89]. Oocytes should be able to repair such damage as they are equipped with components of DSB DNA repair, single-strand break (SSB) repair, and nucleotide-excision repair (NER) pathways [86]. However, female age has been shown to affect oocyte DNA repair pathways [90,91]. Further, detrimental effects of age have been reported on the DNA repair capacity of oocytes after IVF with X- irradiated sperm [92].
6. ROS Producers in Semen
The human ejaculate comprises mature and immature spermatozoa, germ cells, leukocytes, macrophages, and epithelial cells suspended in the seminal plasma. The main ROS producers in semen are leukocytes and immature spermatozoa. Peroxidase-containing leukocytes include macrophages (20–30%) and polymorphonuclear leukocytes (50–60%) and among them, neutrophils, which enter the semen in an activated state, are the most powerful ROS producers [93]. Seminal plasma antioxidants protect spermatozoa against the deleterious action of ROS generated by leukocytes [94], but in cases of infection or inflammation, the concentration of peroxidase-positive leukocytes can be ≥ 1 × 106/mL, leading to leukocytospermia. In such conditions, peroxidase-positive leukocytes have been reported to produce 100-folds more ROS than under normal physiological conditions, and the antioxidant protection of seminal plasma becomes insufficient, leading to OS [95,96,97,98]. Although the association of leukocytospermia with male fertility in vitro is still under debate, the persistence of leukocyte contamination after removal of seminal plasma during sperm manipulation in ART has been reported to decrease the fertilization rates [98,99].
Leukocytes produce ROS much higher than spermatozoa, but their level in human semen is extremely low, and selection techniques such as density gradient centrifugation (DGC) are able to remove leukocytes from sperm suspensions. Spermatozoa and specific sperm subpopulations with enhanced ability to produce ROS are of concern once they are separated from seminal plasma and subjected to laboratory interventions. Although it would be important to determine which spermatozoon produces more ROS, these reactive molecules are extremely short-lived (10−9 s) and, most redox-sensitive probes measure OS rather than ROS directly [25].
A series of studies suggested a relationship between retention of the cytoplasmic droplet and human sperm membrane peroxidative damage using creatinine kinase (CK) and glucose-6-phosphate dehydrogenase (G6PDH) as markers of cytoplasm retention [100,101,102,103]. Gomez and collaborators [44] demonstrated an enhanced ROS production in human spermatozoa recovered from the low-density fraction after Percoll DGC characterized by large midpieces and high content of cytoplasmic enzymes. As G6PDH is required for the reduction of NADP+ to NADPH, it has been proposed to be involved in ROS production through membrane NADPH oxidase [104,105,106]. The enhanced ROS production by immature spermatozoa has been suggested to induce an OS in neighboring mature spermatozoa during their transit in the epididymis [44,107,108]. Koppers and collaborators reported that poorly motile and dysfunctional spermatozoa from the low-density region of Percoll gradients had an increased content of unsaturated fatty acids compared to motile and functional spermatozoa recovered from the high-density region, and this caused increased spontaneous production of mitochondrial ROS and consequent oxidative DNA damage in the mitochondria and nucleus [109]. Dysfunctional spermatozoa were characterized by the presence of excess residual cytoplasm, poor protamination, and retention of histones and have been suggested to result from defective differentiation during spermiogenesis [109]. Several studies showed a positive correlation between abnormal sperm morphology, ROS production, and DNA damage [93,107,110,111]. Moreover, an increased expression of the main isoform of NADPH oxidase (NOX), NOX5, an active membrane-bound generator of ROS in spermatozoa, has been reported in both teratozoospermic [112] and asthenozoospermic human ejaculates [44]. Positive correlations found between sperm morphological abnormalities, histone persistency, and lipid peroxidation indicate that abnormal spermatozoa with excessive histones and relaxed chromatin produce a higher amount of H2O2 [113]. The fact that the percentage of sperm persistent histones had an adverse effect on embryo development and clinical pregnancy outcomes is another indication of the incidence of sperm OS in such impairments [113].
The presence of an elevated fraction of dead spermatozoa is of concern during sperm manipulation and especially during cryopreservation in ART. Dead spermatozoa are generally considered high ROS producers [114] though their contribution to semen ROS generation can vary according to the species. The production of H2O2 by dead equine spermatozoa has been reported to be five-fold higher than in live spermatozoa [115]. Dead spermatozoa have been suggested to represent the major ROS producers through an aromatic L-amino acid oxidase (LAAO) pathway in bull semen [116]. In boars, the presence of dead spermatozoa in semen before and during freezing increased the production of ROS and sperm DNA fragmentation (SDF) in cryo-survived gametes [117]. L-amino acid oxidases have been reported in bull, ram, and stallion, and its activity is increased following sperm death [116,117,118,119,120]. Exposure of this enzyme to aromatic L-amino acids present in cryo-diluents and extenders upon loss of sperm membrane integrity promotes their deamination and the production of H2O2. Viable spermatozoa can therefore undergo a ROS-induced death promoting, in turn, the loss of viability in the remaining live cells [116,120]. Human spermatozoa containing LAAO are capable of inducing sperm capacitation and acrosomal exocytosis, but in contrast to bull and ram spermatozoa, LAAO activity is completely absent in nonviable human spermatozoa due to its rapid leakage after the loss of membrane integrity [121].
7. ART Procedures That Generate Sperm Oxidative Stress
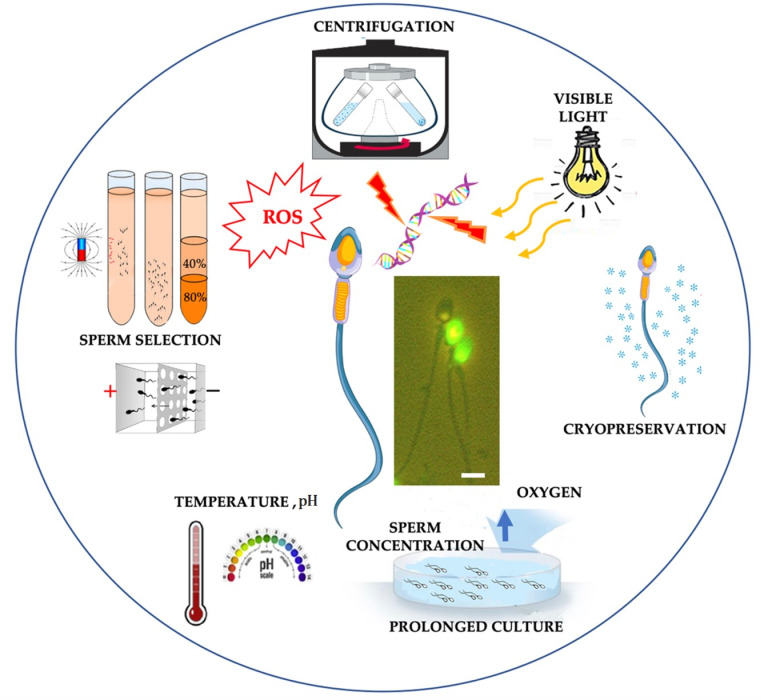
Spermatozoa are subjected to a wide range of in vitro manipulations during ART in both human and domestic animals. In a typical ART setting, the potential sources of oxidative stress in vitro include endogenous and exogenous factors. Although gametes themselves have the potential to generate ROS, OS during ART could also arise from several exogenous factors such as exposure to visible light, centrifugation, cryopreservation, culture media, O2 tension, pH, and temperature (Figure 1).
Figure 1.
Factors inducing oxidative stress during sperm manipulation in ART. Central micrographs: TUNEL-labeled human sperm. Bar, 5 μm. Sperm drawing is modified from https://www.vecteezy.com/vector-art/1434164-human-sperm-or-spermatozoa-cell-structure (accessed date 3 March 2021).
In vitro manipulation of sperm primarily involves the separation of cells from the seminal plasma that contains several protective enzymatic and non-enzymatic antioxidants and low molecular weight compounds exerting powerful antioxidant activity [122,123]. On the other hand, as the main sources of intracellular ROS in semen are leukocytes [124,125,126] and immature sperm with abnormal head morphology and cytoplasmic retention [44,70], removal of these ROS sources through sperm selection can reduce SDF and other oxidative damage.
Whole semen can be subjected to several sperm selection procedures. The most commonly applied are swim-up techniques and centrifugation through discontinuous density gradients of silane-coated silica colloidal particles. Swim-up can be performed from the whole semen or a pellet obtained through centrifugation, through stratification of a medium containing bicarbonate and albumin, in which motile sperm migrate.
Several factors could generate OS during the swim-up from a pellet. In fact, (1) the seminal plasma antioxidants are removed as semen is mixed with culture medium; (2) the shearing forces induced on spermatozoa and cells during centrifugation result in the production of ROS [125]; (3) before migration, spermatozoa remain tightly packed for a variable time in the pellet along with leukocytes and abnormal spermatozoa which are both ROS producers. The level of ROS generation is dependent on the severity and duration of exposure to centrifugation force [127,128]. Preparation techniques involving the centrifugation of unfractionated sperm suspensions, such as simple washings or swim-up from the pellet, have been associated with a sudden burst of ROS production, reduced motility, and impaired sperm-oocyte fusion in the zona-free hamster oocyte penetration test [125,129]. Therefore, it has been suggested to adopt sperm-selection techniques in which centrifugation is only applied after the sperm motile fraction has been selected, as in the swim-up from semen and gradient centrifugation procedures.
Several studies assessed the effects of DGC on DNA oxidative damage analyzing SDF through TUNEL and the formation of the DNA-base adduct 8-hydroxy-2′-deoxyguanosine. Aitken et al. showed that a majority of TUNEL and 8OHdG positive cells were dead both before and after Percoll and Puresperm, and DGC positively selected motile and viable cells, reducing the proportion of TUNEL-positive cells. However, DGC increased the fraction of viable cells with high levels of 8OHdG both in a patient and donor population, leading to an increase of viable TUNEL-positive sperm only in the former [25]. Such effects were attributed to ROS production during centrifugation through the dense gradient rather than to the simple act of centrifugation that can also increase ROS generation [125,129]. Iwasaki and Gagnon [130] showed a four- to five-fold increase of ROS in Percoll-washed spermatozoa compared to the original semen sample, whereas a reduction of ROS was reported in spermatozoa recovered after DGC in SpermGrad™ [131], and a lack of increase in sperm DNA damage was reported after centrifugation in PureCeption™ and Isolate™ [132]. Zhao et al. reported a significant reduction of ROS and SDF after the selection of normozoospermic samples through PureCeptionTM density gradient centrifugation or swim-up [133].
The induction of oxidative DNA damage in PureSperm recovered spermatozoa was demonstrated to depend on the simple exposure to the density medium and not associated with generalized oxidative stress. Contaminating metals found in Percoll, PureSperm, and other commercial density media have been suggested to promote ROS generation in the immediate vicinity of DNA, and the addition of EDTA to PureSperm fully reversed its ability to induce oxidative DNA damage [134]. Muratori and collaborators reported that PureSperm centrifugation increased the percentage of DNA fragmented spermatozoa in about 50% of subjects studied, while a reduction was observed in the remaining ones. Interestingly, the patients with PureSperm-induced DNA oxidation had a 50% lower chance of achieving pregnancy after IVF/ICSI [135], even though no differences were found after basal semen analysis. In a subsequent paper, the effects of DGC and swim-up selection on the TUNEL positive live and dead fractions were evaluated in male partners of infertile couples, which did not show any differences in average pre- and post-selection SDF values but again a different behavior according to the sample. The analysis of single samples revealed that in some subjects, both selection methods induced SDF, whereas in other subjects, the opposite finding was observed. The analysis of viable-DNA fragmented sperm allowed the identification of additional subjects undergoing DNA damage during selection with respect to conventional methods revealing total SDF. Moreover, under these conditions, the increase of both total and viable SDF (p = 0.047) in samples processed by DGC was higher than swim-up of good quality semen samples and about equal to swim-up selection in case of poor-quality samples [136]. Although ROS were not assessed in these studies, the occurrence of DNA fragmentation in spermatozoa after ejaculation is generally considered a result of OS.
Apparently, controversial findings of studies aimed to evaluate the effects of discontinuous gradient centrifugation on ROS production and/or DNA damage could be explained by the particular gradient used, presence of metal contamination, and chelating agents in diluting media, as well as by semen quality and patient age.
More advanced sperm selection techniques, including magnetic cell sorting (MACS) with annexin V conjugated beads, intracytoplasmic morphologically selected sperm injection (IMSI), and physiological ICSI using hyaluronic acid binding (PICSI), have been proposed to select high-quality spermatozoa with intact chromatin [137,138,139,140]. However, the additional value of such selection procedures on ART outcome is still debated [141,142], and importantly, these techniques require longer culture or handling time, pH, and temperature variations, and exposure to visible light under the microscope which could induce OS and consequent DNA damage.
Ashgar et al. developed a centrifugation-free and flow-free microfluidic platform where spermatozoa from whole semen migrate against gravity through 3, 5, or 8 μm pores carbonate filters [143]. Human semen processed through the platform had decreased ROS generation and SDF compared to parallel spermatozoa recovered through swim-up from pellet [143]. Ebner and collaborators found a 90% reduction of SDF after a centrifugation-free selection in special chambers, Zech-selectors, whereas no reduction was achieved after DGC [144]. Other studies evaluated the efficiency of methods based on sperm electric charge in selecting DNA fragmentation-free spermatozoa. A significant reduction of SDF through a Zeta potential selection on spermatozoa recovered by DGC compared to DGC alone has been recently reported [145]. An electrophoresis method developed to select high-quality human spermatozoa on the basis of their high negative charge [146] was shown to efficiently select spermatozoa without oxidative DNA damage in contrast to Percoll DGC that increase such damage compared to neat semen [147]. In addition, Simon and collaborators showed that DGC increased the fraction of positively charged and decreased that of negatively charged human spermatozoa compared to neat semen [148].
Several studies showed that prolonged sperm incubation in culture media leads to OS, SDF, and DNA oxidation in human and animal models [38,148,149,150,151]. Incubation of spermatozoa from healthy donors after selection through swim-up from pellet led to a reduction in motility and increased ROS levels starting from 6 h and reaching a peak at 48 and 24 h, respectively [152]. Other studies found significant changes at earlier incubation times. In a study on 24 normozoospermic and 20 oligozoospermic patients, washed spermatozoa in 75% of the patients decreased total and progressive motility and increased lipid peroxidation and SDF during incubation for 6 h. [153]. Nabi and collaborators found an increased SDF in spermatozoa selected through swim-up from whole semen during incubation for 3 h (from 4.38% at 0 h to about 11% at 3 h) [154]. Sperm concentration during in vitro manipulation also affects viability, ROS levels, and SDF in different species. Post-thaw incubation of ram spermatozoa at 6 to 100 × 106/mL for 6 h resulted in an increase of SDF, with lower sperm concentrations being safer in this respect. The increase of SDF also depended on individual ram semen [155]. The sperm concentration during storage of bull semen in a fresh extender also affects the ROS levels, with higher concentrations of spermatozoa (5 × 106 per 0.25 mL artificial insemination dose) exerting detrimental effects on sperm cell viability and increased OS compared to lower sperm concentrations [156]. In our lab, incubation of washed human spermatozoa from seven normozoospermic patients at serial dilutions ranging from 5 to 100 × 106/mL in Sydney IVF Gamete Buffer for 3 h at 37 °C led to increased SDF and oxidative DNA damage except for concentrations of 5–10 × 106/mL (Gualtieri and Talevi, unpublished data).
The effects of prolonged incubation on ROS production could also depend on the specific sperm handling medium used. In fact, incubation of DGC selected human spermatozoa for 3 h in four commercial sperm-washing buffers resulted in different levels of ROS production, sperm viability, and capacitation-associated tyrosine phosphorylation and membrane reorganization. Impairment of sperm function can occur in media with high ROS in response to OS, and in media with very low levels of ROS in which reductive stress can prevent the ROS-induced capacitation events in spermatozoa [157]. Measurements of oxidation-reduction potential (ORP) of sperm processing media using male infertility oxidative system (MiOXSYS) showed values ranging from a condition of reductive stress in freezing media designed to counteract the OS induced by cryopreservation to a condition of OS in sperm washing media. Such measurements could help to define the correct values of sperm processing media to ensure the development of ROS-induced physiological events without introducing an OS during sperm preparation [158].
Oxygen tension during sperm media incubation could also influence the levels of ROS and their beneficial or detrimental effects on spermatozoa. Although spermatozoa are generally incubated in 20% O2, samples with high ROS levels could benefit from reduced O2 tensions. In fact, no differences in sperm function were detected for normozoospermic sperm samples after incubation under 5 versus 20% O2, whereas 5% O2 incubation was found beneficial for oligozoospermic samples that are known to have higher levels of ROS than fertile samples [159].
Moreover, incubation of spermatozoa in whole semen or after washing/selection at 37 °C accelerates the DNA damage compared to room temperature. In fact, incubation of fresh liquified semen for 1 h at 37 °C has been reported to significantly increase phosphatidyl serine translocation and TUNEL positivity compared to parallel samples maintained at 34 and 25 °C [160], whereas incubation of DGC and swim-up selected spermatozoa at 37 °C increases the oxidative damage that can be minimized storing samples at room temperature [161,162].
Exposure of cells to light, especially to short wavelengths in the UV range but also to violet-blue wavelengths, is considered potentially harmful in terms of ROS production and DNA damage. Phototoxicity depends on the wavelength, photon concentration, and also on the cell type, and transmitted light microscopy is generally regarded as poorly phototoxic to cells [163,164,165]. Although the exposure of gametes and embryos to light during microscope observation is generally reported as a potential exogenous source of ROS production [166,167], specific studies on the detrimental effects caused by exposure of spermatozoa to light are lacking. On the other hand, photo-modulation with visible light at different wavelengths has been used to increase sperm hyperactivation and fertilizing potential of human and animal spermatozoa, leading to intracellular Ca2+ rise and a controlled mitochondrial ROS production without affecting the DNA [168,169,170].
Sperm cryopreservation is routinely used in human ART and in the preservation and transport of male gametes in most domestic species. However, several studies in human and domestic animals indicate that cryopreservation reduces sperm viability and can impair sperm motility, mitochondrial activity, chromatin integrity, and reproductive potential in surviving cells [114,171,172,173,174].
Although the high number and quality of gametes present in good-quality ejaculates make survival rates acceptable, spermatozoa in poor-quality ejaculates can be more susceptible to cryoinjuries impairing the recovery of viable spermatozoa after thawing in severely oligozoospermic patients [175]. In fact, impairment of sperm motility, DNA integrity, and sperm competence, as a result of cryopreservation, has been reported, especially in subfertile and infertile men [176,177,178]. There is a general agreement on the contribution of OS as the main factor accounting for the reduced survival and competence of cryopreserved spermatozoa in supporting fertilization and embryo development, especially in non-human mammals [85,150,179,180]. Hence, several studies have been addressed to understand the causes and remedies of cryopreservation-associated sperm damage and the effects of pre- or post-treatment with antioxidants on the improvement of cryopreserved spermatozoa in infertile patients and in animal species prone to cryodamage. The most commonly assessed damages considered are DNA fragmentation and oxidation, ROS levels, and collapse of inner mitochondrial membrane potential [181]. Mitochondria are thought to be central in triggering the OS associated with sperm cryopreservation and opening of the mitochondrial permeability transition pore in response to the increase of intracellular Ca2+ brought about by permeant cryoprotectants has been proposed to represent the main mechanism in this respect (see [182] and references therein for review).
8. Effects of Sperm OS on Embryo Development
Studies have ascertained that OS in spermatozoa can substantially contribute to the poor embryo development in experimental animal models [180,183,184] as well as in humans undergoing ART [185] (Table 1). The most predominant consequence of OS on spermatozoa is DNA damage. Therefore, most of the studies in the literature have correlated the embryonic response to the sperm OS with reference to the sperm DNA damage. The response to the entry of spermatozoa carrying DNA damage to the ooplasm during fertilization can have various consequences [81,82,186,187,188,189]. Depending on the extent of sperm DNA damage, the oocyte can repair the damage in spermatozoa and lead to a healthy embryo; it can successfully fertilize with the development of the defective embryo, or it may lead to fertilization failure or embryo arrest [190]. Simões et al. have demonstrated that elevated endogenous oxidative stress and DNA damage in bovine spermatozoa give rise to blastocysts with a high percentage of apoptotic cells [191]. Similar observations were made in studies in which OS was exogenously induced. Bittner et al. observed that the spermatozoa exposed to H2O2 resulted in embryos carrying high DNA damage at the early cleavage stage as well as blastocyst stage [184]. De Castro et al. reported a dose-dependent decrease in cleavage and blastocyst rates when H2O2 exposed bull spermatozoa were used for in vitro fertilization [183]. In vitro exogenous OS, induced through xanthine/xanthine oxidase system, has been shown to decrease frozen–thawed bull sperm motility, increase SDF, reduce fertilization rates, and reduce blastocyst rates and quality. Pre-treatment with zinc, d-aspartate, and co-enzyme Q10 before exogenous OS was able to prevent these effects [179]. Lane et al. have reported that inducing oxidative stress in mouse spermatozoa using H2O2 can cause oxidative damage to sperm, which not only reduced the developmental potential of preimplantation stage embryos but also decreased their implantation potential. The OS in spermatozoa appeared to have a sex-specific effect on the growth of offspring and their metabolic function. Further, female offspring had metabolic disturbances such as glucose intolerance and increased levels of adipose tissues [85]. Wyck et al. have demonstrated that the sperm OS can impair the epigenetic reprograming in early cattle embryos due to impaired active DNA demethylation on male pronucleus, which can potentially contribute to defective embryo development and poor embryo quality [19]. Rhesus embryos produced from sperm with ROS exposure prior to fertilization exhibit early cleavage abnormalities and a delayed start of first cytokinesis compared to control embryos [192]. Few clinical studies have tried to establish the relationship between basal OS in spermatozoa/seminal plasma and the reproductive outcome in clinical settings. Elevated ROS in seminal plasma has a negative correlation with fertilization rate in IVF and ICSI [193]. Similarly, excessive ROS in semen was found to reduce the fertilization rate, embryo quality, and live birth rate [194]. Further, Ghaleno et al. have shown that high levels of both sperm intracellular H2O2 and O2•− in ICSI patients have a deleterious effect on sperm mitochondrial membrane potential; however, only H2O2 may interfere in pronuclear formation [185]. Further, oxidative DNA damage in human spermatozoa can influence time to pregnancy since an inverse relationship between sperm DNA oxidation and monthly fecundity rate was observed in a naturally conceiving population [195]. In contrast to these observations, Pujol et al. did not find any significant relationship between embryo quality and OS levels in the ejaculate. Hence, these authors have not recommended the routine OS measurement in fresh ejaculate for all patients, especially when the oocytes for the ART cycle come from women younger than 35 years of age [196].
Table 1.
Effects of endogenous, experimentally induced, and art-associated oxidative stress on sperm function, embryo development, and reproductive outcome.
| Oxidative Stress | ART Treatment | Species | Subjects or Samples | Experimental Groups | Adverse Effects: Sperm Function |
Adverse Effects: Embryo Development |
Antioxidant (Effect) | Refs |
|---|---|---|---|---|---|---|---|---|
| Endogenous | NA | Human | First pregnancy— | High vs. low 8OHdG | NA | Natural conception rate ↓ | NA | [195] |
| planning males | ||||||||
| Endogenous | ICSI | Human | Fresh semen | High vs. low ROS | Viability ↓ | Fertilization rate ↓ | NA | [194] |
| Motility ↓ | Pregnancy rate ↓ | |||||||
| Morphology ↓ | ||||||||
| DNA integrity ↓ (TUNEL) | ||||||||
| Endogenous | IVF/ICSI | Human | Fresh semen | High vs. low ROS | Vitality ↓ | Fertilization rate ↓ | NA | [193] |
| Membrane integrity ↓ | ||||||||
| Morphology ↓ | ||||||||
| Endogenous | Washing/IVF | Bovine | F/T semen | High vs. low TBARS | DNA integrity↓ (SCSA) | Cleavage ↓ | ||
| bull semen | Blastocyst DNA fragm. ↑ | NA | [191] | |||||
| (TUNEL) | ||||||||
| Endogenous | Swim-up/ICSI | Human | Fresh semen | High vs. low ROS | ΔΨm ↓ | NA | [185] | |
| High H2O2 vs. high O2•− | ΔΨm ↓ | 2 pronuclei rate ↓ | ||||||
| Endogenous | Swim-up/ICSI | Human | F/T semen | High vs. low O2•− | NA | None | NA | [196] |
| ICSI donor oocytes | ||||||||
| Endogenous | NA | Human | Fresh semen | Idiopathic recurrent | Motility ↓ | Recurrent pregnancy loss | NA | [198] |
| pregnancy loss male | Lipid peroxidation ↑ (TBARS) | |||||||
| partners vs. fertile men | Protein carbonylation ↑ | |||||||
| Histone retention (ABS) ↑ | ||||||||
| Endogenous | NA | Human | Fresh semen | Idiopathic recurrent | Motility ↓ | Recurrent pregnancy loss | NA | [197] |
| pregnancy loss male | ROS ↑ (luminol) | |||||||
| partners vs. fertile men | TAC ↓ | |||||||
| DNA integrity↓ (SCSA, TUNEL) | ||||||||
| Ind. (H2O2) | Culture 1h/IVF | Mouse | Fresh semen | H2O2 vs. medium | ROS ↑ (carboxy-DCFDA) | 8-cell rate ↓ | NA | [85] |
| Mitochondrial ROS ↑(MSR) | Blastocyst rate ↓ | |||||||
| Lipid peroxidation ↑(4-HNE) | Implantation rate ↓ | |||||||
| Fetal weight ↓ | ||||||||
| Fetal:placental ratio ↓ | ||||||||
| Crown-rump length ↓ | ||||||||
| Female offspring health ↓ | ||||||||
| Ind. (H2O2) | Culture 1h/IVF | Bovine | F/T semen | H2O2 vs. medium | Motility ↓ | Cleavage ↓ | NA | [19] |
| DNA integrity ↓(SCSA) | Blastocyst rate ↓ | |||||||
| Active DNA demethylation | ||||||||
| paternal pronucleus ↓ | ||||||||
| Ind. (X-XO) | Culture 2h/ICSI | Rhesus | F/T semen | X-XO vs. medium | Motility ↓ | Cleavage ↓ | NA | [192] |
| Delayed first cytokinesis ↑ | ||||||||
| Blastocyst rate ↓ | ||||||||
| Ind. (H2O2) | Culture 1h/IVF | Bovine | F/T semen | H2O2 vs. medium | Motility ↓ | Cleavage ↓ | NA | [183] |
| ROS↑ (CellROX™) | Blastocyst rate ↓ | |||||||
| DNA integrity↓ (AO) | ||||||||
| Ind. (X-XO) | Culture 3h/IVF | Bovine | F/T semen | X-XO vs. medium vs | Motility ↓ | Cleavage ↓ | Zn, D-asp, CoQ10 | [179] |
| antioxidants + X-XO | DNA integrity↓ (TUNEL) | 8-cell rate ↓ | (protection) | |||||
| Blastocyst rate ↓ | ||||||||
| Blastocyst DNA fragm. ↑ | ||||||||
| (TUNEL) | ||||||||
| Ind. (H2O2) | Culture 1h/IVF | Bovine | F/T semen | H2O2 vs. medium | Motility ↓ | Delayed first cleavage ↑ | NA | [184] |
| DNA integrity↓ (SCSA) | Cleavage ↓ | |||||||
| Blastocyst rate ↓ | ||||||||
| Blastocyst DNA fragm. ↑ | ||||||||
| (Comet, TUNEL) | ||||||||
| Ext. culture | Culture 3h/IVF | Bovine | F/T semen | Antioxidants | Motility 1 h ↑ | Cleavage ↑ | Zn, D-asp, CoQ10 | [150] |
| vs medium | DNA integrity 3 h ↑ (TUNEL) | 8-cell rate ↑ | (protection) | |||||
| Blastocyst rate ↑ | ||||||||
| Blastocyst DNA fragm. ↓ | ||||||||
| (TUNEL) | ||||||||
| DGC + mEP | IVF/ICSI | Human | Fresh semen | DGC vs. fresh semen | Neg. charged sperm (NCS) ↓ | NCS ↑: IVF fertilization rate ↑ | NA | [148] |
| Pos. charged sperm (PCS) ↑ | NCS ↑: blastocyst rate ↑ | |||||||
| NCS: DNA integrity (TUNEL) ↑ | NCS ↑: implantation rate ↑ | |||||||
| PCS: DNA integrity (TUNEL) ↓ | NCS ↑: clin. preg. rate ↑ | |||||||
| NCS ↑: Histone retention (ABS) ↑ | ||||||||
| DGC | IVF | Bovine | F/T semen | DGC + cushioning | ROS (DCHF-DA): no differences | Fertilization rate ↓ | NA | [199] |
| vs DGC | Motility: no differences | Cleavage ↓ | ||||||
| Immobiliz. | Mouse oocyte | Human | Fresh semen | PVP vs. HA vs | ORP: PVP < HA < medium | MOAT: no differences | NA | [203] |
| activation | medium | |||||||
| (MOAT) | ||||||||
| Cryopr. | IVF | Mouse | Fresh and | F/T vs. fresh semen | DNA integrity ↓ (SCSA) | 2-cell embryos ↓ | NA | [205] |
| F/T semen | Blastocyst rate ↓ | |||||||
| Cryopr. | ICSI normal | Human | Fresh and | F/T vs. fresh semen | NA | ICSI defective oocytes: | NA | [204] |
| and defective | F/T semen | Day 2, 3 embryo quality ↓ | ||||||
| oocytes | Blastocyst rate ↓ | |||||||
| Cryopr. | ICSI | Bovine | F/T semen | No GSH vs. post-thaw | Motility ↓ | Cleavage rate ↓ | GSH | [206] |
| GSH treatment | ΔΨm ↓ | Blastocyst rate ↓ | (protection) | |||||
| ATP ↓ | ||||||||
| Sex sorting | IVF | Bovine | F/T semen | Post- vs. pre-sorting | Motility ↓ | Cleavage rate ↓ | [208] | |
| Hyperactivation ↓ | 4-cell rate ↓ | |||||||
| Survival ↓ | Blastocyst rate ↓ | |||||||
| (Extent is bull specific) | Embryo survival ↓ (extent is | |||||||
| bull specific) | ||||||||
| Sex sorting | IVF | Bovine | F/T semen | Washing/fertilization | MDA↓ | Cleavage rate ↑ | Vitamin C or | [209] |
| with vs. without | Viability ↑ | Lyc: Blastocyst rate ↑ | Lycopene | |||||
| Vitamin C (VC) or Lycopene (Lyc) |
Apoptosis (Annexin V) ↓ | (protection) | ||||||
| ΔΨm ↑ (VC: extent bull specific) |
Effects of endogenous, experimentally induced (Ind.), and ART-associated oxidative stress on sperm function, embryo development, and reproductive outcome. ABS, aniline blue staining; AO, acridine orange staining; carboxy-DCFDA, 5- and 6-carboxy-2’,7’-dichlorofluorescein diacetate; CoQ10, coenzyme Q10; Cryopr., cryopreservation; D-asp, D-aspartate; DCHF-DA, 2ʹ,7ʹ-dichlorofluorescin diacetate; DGC, density gradient centrifugation; ΔΨm, inner mitochondrial membrane potential; Ext., extended; Fragm., fragmentation; GSH, reduced L-glutathione; HA, hyaluronic acid; 4-HNE, 4-hydroxynonenal; Immobiliz., immobilization; MDA, malondialdehyde; mEP, micro-electrophoresis; MSR, MitoSOX™ Red; NA, not applicable; 8OHdG, 8-hydroxy-2′-deoxyguanosine; ORP, oxidation-reduction potential; ROS, reactive oxygen species; SCSA, sperm chromatin structure assay; TBARS, thiobarbituric acid reactive substances assay; TAC, total antioxidant capacity; Zn, zinc; ↑, increase; ↓, decrease.
Oxidative stress-induced protein damage in sperm is expected to be implicated in embryo degeneration at a progressive phase of pregnancy, which could lead to pregnancy loss. Levels of SDF, ROS, and total antioxidant capacity (TAC) have significant correlations with recurrent spontaneous miscarriage. The increase in SDF, along with the increase of free radicals and reduction of total antioxidants in semen, has increased the frequency of repeated miscarriages [197]. It has been suggested that histone-carrying sites for oxidative modification such as arginine and lysine might be responsible for disturbing the paternal epigenomic control during early stages of embryonic differentiation, leading to pregnancy loss [198].
Fewer studies were focused on the effects of OS induced by specific sperm manipulations during ART on embryo development. Simon and collaborators showed that selection of human spermatozoa through DGC increased the fraction of positively charged and decreased that of negatively charged spermatozoa compared to neat semen. The negatively charged fraction was relatively free of DNA damage and positively associated with increased fertilization and blastocyst rates. In addition, embryos generated by patients with a higher fraction of negatively charged spermatozoa had better implantation and clinical pregnancy rates [148].
A recent study assessed the effects of cushioned centrifugation of frozen–thawed bull spermatozoa using a commercial colloidal iodixanol-based solution (Cushion Fluid, Minitube®, Tiefenbach, Germany) on fertilization and embryo development. The addition of cushion fluid at the bottom of a Percoll gradient before centrifugation (C1), as well as during washing of recovered spermatozoa (C1–2), or exclusively at washing (C2), was compared with Percoll centrifugation without a cushion fluid (C). ROS levels in C and C1 were comparable and were significantly lower than in C1–2 and C2 treatments. Interestingly, cushioned Percoll centrifugation (C1) produced higher fertilization, cleavage, and blastocyst rates compared to conventional Percoll centrifugation (C) [199].
Conflicting results have been reported on the effects of sperm selection through hyaluronic acid compared to polyvinylpyrrolidone (PVP) prior to ICSI on ART outcome [138,200,201,202]. Although measurements of oxidation-reduction potential (ORP) of human spermatozoa treated with PVP, hyaluronic acid, or medium indicate that PVP provides higher antioxidative protection, exposure of human spermatozoa to the different handling media do not affect mouse oocyte activation, and injection of the three media in parthenogenetically activated mouse oocytes had no effects on embryo development [203].
Spontaneous OS during culture was investigated in human spermatozoa and in bovine frozen-thawed spermatozoa. In both species, culture for 6 and 3 h, respectively, decreased total and progressive motility and increased lipid peroxidation and SDF, and such effects were prevented by supplementation of sperm media with zinc, d-aspartate, and co-enzyme Q10 [150,153]. Moreover, in the bovine, blastocyst rate was found to be significantly higher in oocytes fertilized by treated spermatozoa, and these blastocysts harbored a significantly lower percentage of apoptotic cells compared to parallel spermatozoa incubated in the medium alone [150].
More studies are available in the literature on the detrimental effects of sperm cryopreservation on embryo development after IVF or ICSI. An interesting study considered the effects of cryopreserved versus fresh human spermatozoa on embryo development after ICSI in normal or dysmorphic oocytes. A negative influence of sperm cryopreservation on the quality of cleavage stage embryos and on blastocyst rates was only detected when one oocyte defect was present, suggesting that healthy oocytes can better repair damaged paternal DNA [204]. Mouse sperm cryopreservation increases SDF and affects embryo development according to the specific cryopreservation procedures adopted [205]. In bovine, treatment of frozen–thawed spermatozoa with GSH before ICSI improved the rates of embryos reaching the 4–8-cell stage and blastocyst stage [206].
Sperm sorting, a valuable technique for selecting desired sex in domestic animals, is associated with increased OS and SDF [207]. Bovine embryos derived from sex-sorted spermatozoa had an increased incidence of arrest at the 4-cell stage, and reduced survival and blastocyst rates [208]. Supplementation of vitamin C or lycopene in washing and fertilization medium improves the fertilization, cleavage, and blastocyst rates of oocytes inseminated with sex-sorted bull sperm [209].
9. Conclusions
Several ART manipulations have the potential to induce an ex novo OS in spermatozoa. The individual semen characteristics can influence the degree of OS during sperm in vitro manipulations. Although routinely used sperm selection methods can enhance the recovery of spermatozoa with higher DNA integrity compared to the neat semen, an enhancement of DNA fragmentation or oxidation can be found in some individuals. The induction of OS and the consequent enhancement of DNA damage could be minimized using advanced selection procedures such as microelectrophoresis, Zeta potential, and microfluidic methods. However, such technologies still remain rarely applied in clinics.
Despite substantial evidence in human and animal models that clearly indicate that sperm OS exerts detrimental effects on embryo development, fetal growth, and postnatal health, studies addressing the effects of specific in vitro manipulations on sperm OS and its consequences on embryo development and ART outcome are limited. Treatment with specific antioxidants in vitro could prevent the impairment of sperm function and competence induced by ART manipulations. However, their application in the clinical practice is still limited and should be introduced, taking into account the extent of OS caused by the specific ART procedures and the need for a personalized treatment according to the semen characteristics of the patient. Indeed, the prevention of OS could be needed in some patients in whom ROS production exceeds semen antioxidants’ defenses, whereas it could be dangerous in patients with low ROS levels. This could lead to a reductive stress condition that suppresses the physiological redox signaling needed for sperm capacitation, hyperactivation, acrosome reaction, and sperm–oocyte fusion.
During the next few years, the increase of success rate and safety of ART will require further research to develop and individualize more adequate techniques to avoid the iatrogenic causes of sperm OS and its short- and long-term consequences on the reproductive outcome.
Author Contributions
Conceptualization, R.G., G.K., V.B., S.K.A., and R.T.; data curation, R.G., G.K., V.B., S.L., F.D.R., S.K.A. and R.T.; writing—original draft preparation, R.G., G.K., S.K.A. and R.T.; writing—review and editing, R.G. and R.T.; supervision, R.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Agarwal A., Mulgund A., Hamada A., Chyatte M.R. A unique view on male infertility around the globe. Reprod. Biol. Endocrinol. 2015;13:37. doi: 10.1186/s12958-015-0032-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO Laboratory Manual for the Examination and Processing of Human Semen. 5th ed. World Health Organization; Geneva, Switzerland: 2010. [Google Scholar]
- 3.Agarwal A., Baskaran S., Parekh N., Cho C.L., Henkel R., Vij S., Arafa M., Panner Selvam M.K., Shah R. Male infertility. Lancet. 2021;397:319–333. doi: 10.1016/S0140-6736(20)32667-2. [DOI] [PubMed] [Google Scholar]
- 4.Hamada A., Esteves S.C., Nizza M., Agarwal A. Unexplained male infertility: Diagnosis and management. Int. Braz. J. Urol. 2012;38:576–594. doi: 10.1590/S1677-55382012000500002. [DOI] [PubMed] [Google Scholar]
- 5.Jungwirth A., Diemer T., Kopa Z., Krausz C., Minhas S., Tournaye H. EAU Guidelines on Male Infertility. European Association of Urology; Arnhem, The Netherlands: 2018. [Google Scholar]
- 6.de Kretser D.M. Male infertility. Lancet. 1997;349:787–790. doi: 10.1016/S0140-6736(96)08341-9. [DOI] [PubMed] [Google Scholar]
- 7.Hamada A., Esteves S.C., Agarwal A. Unexplained male infertility: Potential causes and management. Hum. Androl. 2011;1:2–16. doi: 10.1097/01.XHA.0000397686.82729.09. [DOI] [Google Scholar]
- 8.Aitken R.J. The male is significantly implicated as the cause of unexplained infertility. Semin. Reprod. Med. 2020;38:3–20. doi: 10.1055/s-0040-1718941. [DOI] [PubMed] [Google Scholar]
- 9.Aitken R.J., Baker M.A. The role of genetics and oxidative stress in the etiology of male infertility—A unifying hypothesis? Front. Endocrinol. 2020;11:581838. doi: 10.3389/fendo.2020.581838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shekarriz M., Thomas A.J., Jr., Agarwal A. Incidence and level of seminal reactive oxygen species in normal men. Urology. 1995;45:103–107. doi: 10.1016/S0090-4295(95)97088-6. [DOI] [PubMed] [Google Scholar]
- 11.Bisht S., Faiq M., Tolahunase M., Dada R. Oxidative stress and male infertility. Nat. Rev. Urol. 2017;14:470–485. doi: 10.1038/nrurol.2017.69. [DOI] [PubMed] [Google Scholar]
- 12.Agarwal A., Rana M., Qiu E., Al Bunni H., Bui A.D., Henkel R. Role of oxidative stress, infection and inflammation in male infertility. Andrologia. 2018;50:e13126. doi: 10.1111/and.13126. [DOI] [PubMed] [Google Scholar]
- 13.Agarwal A., Parekh N., Panner Selvam M.K., Henkel R., Shah R., Homa S.T., Ramasamy R., Ko E., Tremellen K., Esteves S., et al. Male oxidative stress infertility (MOSI): Proposed terminology and clinical practice guidelines for management of idiopathic male infertility. World J. Mens. Health. 2019;37:296–312. doi: 10.5534/wjmh.190055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Lamirande E., Gagnon C. Impact of reactive oxygen species on spermatozoa: A balancing act between beneficial and detrimental effects. Hum. Reprod. 1995;10:15–21. doi: 10.1093/humrep/10.suppl_1.15. [DOI] [PubMed] [Google Scholar]
- 15.Talevi R., Zagami M., Castaldo M., Gualtieri R. Redox regulation of sperm surface thiols modulates adhesion to the fallopian tube epithelium. Biol. Reprod. 2007;76:728–735. doi: 10.1095/biolreprod.106.056028. [DOI] [PubMed] [Google Scholar]
- 16.Starkov A.A. The role of mitochondria in reactive oxygen species metabolism and signaling. Ann. N. Y. Acad. Sci. USA. 2008;1147:37–52. doi: 10.1196/annals.1427.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gualtieri R., Mollo V., Duma G., Talevi R. Redox control of surface protein sulphhydryls in bovine spermatozoa reversibly modulates sperm adhesion to the oviductal epithelium and capacitation. Reproduction. 2009;138:33–43. doi: 10.1530/REP-08-0514. [DOI] [PubMed] [Google Scholar]
- 18.Aitken R.J. Reactive oxygen species as mediators of sperm capacitation and pathological damage. Mol. Reprod. Dev. 2017;84:1039–1052. doi: 10.1002/mrd.22871. [DOI] [PubMed] [Google Scholar]
- 19.Wyck S., Herrera C., Requena C.E., Bittner L., Hajkova P., Bollwein H., Santoro R. Oxidative stress in sperm affects the epigenetic reprogramming in early embryonic development. Epigenetics Chromatin. 2018;11:60. doi: 10.1186/s13072-018-0224-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agarwal A., Saleh R.A., Bedaiwy M.A. Role of reactive oxygen species in the pathophysiology of human reproduction. Fertil. Steril. 2003;79:829–843. doi: 10.1016/S0015-0282(02)04948-8. [DOI] [PubMed] [Google Scholar]
- 21.Aitken R.J., Clarkson J.S., Fishel S. Generation of reactive oxygen species, lipid peroxidation and human sperm function. Biol. Reprod. 1989;40:183–197. doi: 10.1095/biolreprod41.1.183. [DOI] [PubMed] [Google Scholar]
- 22.Alvarez J.G., Touchstone J.C., Blasco L., Storey B.T. Spontaneous lipid peroxidation and production of hydrogen peroxide and superoxide in human spermatozoa. Superoxide dismutase as major enzyme protectant against oxygen toxicity. J. Androl. 1987;8:338–348. doi: 10.1002/j.1939-4640.1987.tb00973.x. [DOI] [PubMed] [Google Scholar]
- 23.Hughes C.M., Lewis S.E.M., McKelvey-Martin V.J., Thompson W. A comparison of baseline and induced DNA damage in human spermatozoa from fertile and infertile men using a modified comet assay. Mol. Hum. Reprod. 1996;2:613–620. doi: 10.1093/molehr/2.8.613. [DOI] [PubMed] [Google Scholar]
- 24.Aitken R.J., De Iuliis G.N. On the possible origins of DNA damage in human spermatozoa. Mol. Hum. Reprod. 2010;16:3–13. doi: 10.1093/molehr/gap059. [DOI] [PubMed] [Google Scholar]
- 25.Aitken R.J., De Iuliis G.N., Finnie J.M., Hedges A., McLachlan R.I. Analysis of the relationships between oxidative stress, DNA damage and sperm vitality in a patient population: Development of diagnostic criteria. Hum. Reprod. 2010;25:2415–2426. doi: 10.1093/humrep/deq214. [DOI] [PubMed] [Google Scholar]
- 26.Borini A., Tarozzi N., Bizzaro D., Bonu M.A., Fava L., Flamigni C., Coticchio G. Sperm DNA fragmentation: Paternal effect on early post-implantation embryo development in ART. Hum. Reprod. 2006;21:2876–2881. doi: 10.1093/humrep/del251. [DOI] [PubMed] [Google Scholar]
- 27.Tarozzi N., Bizzaro D., Flamigni C., Borini A. Clinical relevance of sperm DNA damage in assisted reproduction. Reprod. Biomed. Online. 2007;14:746–757. doi: 10.1016/S1472-6483(10)60678-5. [DOI] [PubMed] [Google Scholar]
- 28.Tremellen K. Oxidative stress and male infertility—A clinical perspective. Hum. Reprod. Update. 2008;14:243–258. doi: 10.1093/humupd/dmn004. [DOI] [PubMed] [Google Scholar]
- 29.Zhao J., Zhang Q., Wang Y., Li Y. Whether sperm deoxyribonucleic acid fragmentation has an effect on pregnancy and miscarriage after invitro fertilization/intracytoplasmic sperm injection: A systematic review and meta-analysis. Fertil. Steril. 2014;102:998–1005.e8. doi: 10.1016/j.fertnstert.2014.06.033. [DOI] [PubMed] [Google Scholar]
- 30.Osman A., Alsomait H., Seshadri S., El-Toukhy T., Khalaf Y. The effect of sperm DNA fragmentation on live birth rate after IVF or ICSI: A systematic review and meta-analysis. Reprod. Biomed. Online. 2015;30:120–127. doi: 10.1016/j.rbmo.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 31.Simon L., Zini A., Dyachenko A., Ciampi A., Carrell D.T. A systematic review and meta-analysis to determine the effect of sperm DNA damage on in vitro fertilization and intracytoplasmic sperm injection outcome. Asian J. Androl. 2017;19:80–90. doi: 10.4103/1008-682X.182822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Lamirande E., Gagnon C. Capacitation-associated production of superoxide anion by human spermatozoa. Free Radic. Biol. Med. 1995;18:487–495. doi: 10.1016/0891-5849(94)00169-K. [DOI] [PubMed] [Google Scholar]
- 33.Herrero M.B., de Lamirande E., Gagnon C. Nitric oxide is a signaling molecule in spermatozoa. Curr. Pharm. Des. 2003;9:419–425. doi: 10.2174/1381612033391720. [DOI] [PubMed] [Google Scholar]
- 34.Herrero M.B., de Lamirande E., Gagnon C. Tyrosine nitration in human spermatozoa: A physiological function of peroxynitrite, the reaction product of nitric oxide and superoxide. Mol. Hum. Reprod. 2001;7:913–921. doi: 10.1093/molehr/7.10.913. [DOI] [PubMed] [Google Scholar]
- 35.Koppers A.J., De Iuliis G.N., Finnie J.M., McLaughlin E.A., Aitken R.J. Significance of mitochondrial reactive oxygen species in the generation of oxidative stress in spermatozoa. J. Clin. Endocrinol. Metab. 2008;93:3199–3207. doi: 10.1210/jc.2007-2616. [DOI] [PubMed] [Google Scholar]
- 36.Murphy M.P. How mitochondria produce reactive oxygen species. Biochem. J. 2009;417:1–13. doi: 10.1042/BJ20081386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koppers A.J., Mitchell L.A., Wang P., Lin M., Aitken R.J. Phosphoinositide 3-kinase signalling pathway involvement in a truncated apoptotic cascade associated with motility loss and oxidative DNA damage in human spermatozoa. Biochem. J. 2011;436:687–698. doi: 10.1042/BJ20110114. [DOI] [PubMed] [Google Scholar]
- 38.Aitken R.J., Gibb Z., Mitchell L.A., Lambourne S.R., Connaughton H.S., De Iuliis G.N. Sperm motility is lost in vitro as a consequence of mitochondrial free radical production and the generation of electrophilic aldehydes but can be significantly rescued by the presence of nucleophilic thiols. Biol. Reprod. 2012;87:110. doi: 10.1095/biolreprod.112.102020. [DOI] [PubMed] [Google Scholar]
- 39.Aitken R.J., Whiting S., De Iuliis G.N., McClymont S., Mitchell L.A., Baker M.A. Electrophilic aldehydes generated by sperm metabolism activate mitochondrial reactive oxygen species generation and apoptosis by targeting succinate dehydrogenase. J. Biol. Chem. 2012;287:33048–33060. doi: 10.1074/jbc.M112.366690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aitken R.J., Drevet J.R. The importance of oxidative stress in determining the functionality of mammalian spermatozoa: A two-edged sword. Antioxidants. 2020;9:111. doi: 10.3390/antiox9020111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Walters J.L.H., De Iuliis G.N., Dun M.D., Aitken R.J., McLaughlin E.A., Nixon B., Bromfield E.G. Pharmacological inhibition of arachidonate 15-lipoxygenase protects human spermatozoa against oxidative stress. Biol. Reprod. 2018;98:784–794. doi: 10.1093/biolre/ioy058. [DOI] [PubMed] [Google Scholar]
- 42.Niwa K., Iritani A. Effect of various hexoses on sperm capacitation and penetration of rat eggs in vitro. J. Reprod. Fertil. 1978;53:267–271. doi: 10.1530/jrf.0.0530267. [DOI] [PubMed] [Google Scholar]
- 43.Urner F., Sakkas D. Involvement of the pentose phosphate pathway and redox regulation in fertilization in the mouse. Mol. Reprod. Dev. 2005;70:494–503. doi: 10.1002/mrd.20222. [DOI] [PubMed] [Google Scholar]
- 44.Gomez E., Buckingham D.W., Brindle J., Lanzafame F., Irvine D.S., Aitken R.J. Development of an image analysis system to monitor the retention of residual cytoplasm by human spermatozoa: Correlation with biochemical markers of the cytoplasmic space, oxidative stress and sperm function. J. Androl. 1996;17:276–287. [PubMed] [Google Scholar]
- 45.Panday A., Sahoo M.K., Osorio D., Batra S. NADPH oxidases: An overview from structure to innate immunity-associated pathologies. Cell. Mol. Immunol. 2015;12:5–23. doi: 10.1038/cmi.2014.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Musset B., Clark R.A., DeCoursey T.E., Petheo G.L., Geiszt M., Chen Y., Cornell J.E., Eddy C.A., Brzyski R.G., El Jamali A. NOX5 in human spermatozoa: Expression, function, and regulation. J. Biol. Chem. 2012;287:9376–9388. doi: 10.1074/jbc.M111.314955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vatannejad A., Tavilani H., Sadeghi M.R., Karimi M., Lakpour N., Amanpour S., Shabani Nashtaei M., Doosti M. Evaluation of the NOX5 protein expression and oxidative stress in sperm from asthenozoospermic men compared to normozoospermic men. J. Endocrinol. Invest. 2019;42:1181–1189. doi: 10.1007/s40618-019-01035-4. [DOI] [PubMed] [Google Scholar]
- 48.O’Flaherty C., de Lamirande E., Gagnon C. Phosphorylation of the Arginine-X-X-(Serine/Threonine) motif in human sperm proteins during capacitation: Modulation and protein kinase A dependency. Mol. Hum. Reprod. 2004;10:355–363. doi: 10.1093/molehr/gah046. [DOI] [PubMed] [Google Scholar]
- 49.Aitken R.J., Ryan A.L., Baker M.A., McLaughlin E.A. Redox activity associated with the maturation and capacitation of mammalian spermatozoa. Free Radic. Biol. Med. 2004;36:994–1010. doi: 10.1016/j.freeradbiomed.2004.01.017. [DOI] [PubMed] [Google Scholar]
- 50.Gervasi M.G., Visconti P.E. Chang’s meaning of capacitation: A molecular perspective. Mol. Reprod. Dev. 2016;83:860–874. doi: 10.1002/mrd.22663. [DOI] [PubMed] [Google Scholar]
- 51.O’Flaherty C. Redox regulation of mammalian sperm capacitation. Asian J. Androl. 2015;17:583–590. doi: 10.4103/1008-682X.153303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Talevi R., Gualtieri R. Molecules involved in sperm-oviduct adhesion and release. Theriogenology. 2010;73:796–801. doi: 10.1016/j.theriogenology.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 53.Gualtieri R., Talevi R. Selection of highly fertilization-competent bovine spermatozoa through adhesion to the Fallopian tube epithelium in vitro. Reproduction. 2003;125:251–258. doi: 10.1530/rep.0.1250251. [DOI] [PubMed] [Google Scholar]
- 54.Herrero M.B., de Lamirande E., Gagnon C. Nitric oxide regulates human sperm capacitation and protein-tyrosine phosphorylation in vitro. Biol. Reprod. 1999;61:575–581. doi: 10.1095/biolreprod61.3.575. [DOI] [PubMed] [Google Scholar]
- 55.Leclerc P., de Lamirande E., Gagnon C. Cyclic adenosine 3’,5’monophosphate-dependent regulation of protein tyrosine phosphorylation in relation to human sperm capacitation and motility. Biol. Reprod. 1996;55:684–692. doi: 10.1095/biolreprod55.3.684. [DOI] [PubMed] [Google Scholar]
- 56.Herrero M.B., Chatterjee S., Lefièvre L., de Lamirande E., Gagnon C. Nitric oxide interacts with the cAMP pathway to modulate capacitation of human spermatozoa. Free Radic. Biol. Med. 2000;29:522–536. doi: 10.1016/S0891-5849(00)00339-7. [DOI] [PubMed] [Google Scholar]
- 57.O’Flaherty C., de Lamirande E., Gagnon C. Reactive oxygen species and protein kinases modulate the level of phospho-MEK-like proteins during human sperm capacitation. Biol. Reprod. 2005;73:94–105. doi: 10.1095/biolreprod.104.038794. [DOI] [PubMed] [Google Scholar]
- 58.O’Flaherty C., de Lamirande E., Gagnon C. Reactive oxygen species modulate independent protein phosphorylation pathways during human sperm capacitation. Free Radic. Biol. Med. 2006;40:1045–1055. doi: 10.1016/j.freeradbiomed.2005.10.055. [DOI] [PubMed] [Google Scholar]
- 59.O’Flaherty C., de Lamirande E., Gagnon C. Positive role of reactive oxygen species in mammalian sperm capacitation: Triggering and modulation of phosphorylation events. Free Radic. Biol. Med. 2006;41:528–540. doi: 10.1016/j.freeradbiomed.2006.04.027. [DOI] [PubMed] [Google Scholar]
- 60.Luconi M., Barni T., Vannelli G.B., Krausz C., Marra F., Benedetti P.A., Evangelista V., Francavilla S., Properzi G., Forti G., et al. Extracellular signal-regulated kinases modulate capacitation of human spermatozoa. Biol. Reprod. 1998;58:1476–1489. doi: 10.1095/biolreprod58.6.1476. [DOI] [PubMed] [Google Scholar]
- 61.de Lamirande E., Gagnon C. A positive role for the superoxide anion in triggering hyperactivation and capacitation of human spermatozoa. Int. J. Androl. 1993;16:21–25. doi: 10.1111/j.1365-2605.1993.tb01148.x. [DOI] [PubMed] [Google Scholar]
- 62.de Lamirande E., Gagnon C. Human sperm hyperactivation and capacitation as parts of an oxidative process. Free Radic. Biol. Med. 1993;14:157–166. doi: 10.1016/0891-5849(93)90006-G. [DOI] [PubMed] [Google Scholar]
- 63.Bize I., Santander G., Cabello P., Driscoll D., Sharpe C. Hydrogen peroxide is involved in hamster sperm capacitation in vitro. Biol. Reprod. 1991;44:389403. doi: 10.1095/biolreprod44.3.398. [DOI] [PubMed] [Google Scholar]
- 64.Aitken R.J., Paterson M., Fisher H., Buckingham D.W., van Duin M. Redox regulation of tyrosine phosphorylation in human spermatozoa and its role in the control of human sperm function. J. Cell. Sci. 1995;108:2017–2025. doi: 10.1242/jcs.108.5.2017. [DOI] [PubMed] [Google Scholar]
- 65.Rivlin J., Mendel J., Rubinstein S., Etkovitz N., Breitbart H. Role of hydrogen peroxide in sperm capacitation and acrosome reaction. Biol. Reprod. 2004;70:518–522. doi: 10.1095/biolreprod.103.020487. [DOI] [PubMed] [Google Scholar]
- 66.Griveau J.F., Renard P., Le Lannou D. An in vitro promoting role for hydrogen peroxide in human sperm capacitation. Int. J. Androl. 1994;17:300–307. doi: 10.1111/j.1365-2605.1994.tb01260.x. [DOI] [PubMed] [Google Scholar]
- 67.Oehninger S., Blackmore P., Mahony M., Hodgen G. Effects of hydrogen peroxide on human spermatozoa. J. Assist. Reprod. Genet. 1995;12:41–47. doi: 10.1007/BF02214128. [DOI] [PubMed] [Google Scholar]
- 68.Jones R., Mann T., Sherins R. Peroxidative breakdown of phospholipids in human spermatozoa, spermicidal properties of fatty acid peroxides, and protective action of seminal plasma. Fertil. Steril. 1979;31:531–537. doi: 10.1016/S0015-0282(16)43999-3. [DOI] [PubMed] [Google Scholar]
- 69.Nowicka-Bauer K., Nixon B. Molecular changes induced by oxidative stress that impair human sperm motility. Antioxidants. 2020;9:134. doi: 10.3390/antiox9020134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sakkas D., Seli E., Bizzaro D., Tarozzi N., Manicardi G.C. Abnormal spermatozoa in the ejaculate: Abortive apoptosis and faulty nuclear remodelling during spermatogenesis. Reprod. Biomed. Online. 2003;7:428–432. doi: 10.1016/S1472-6483(10)61886-X. [DOI] [PubMed] [Google Scholar]
- 71.Atig F., Raffa M., Ali H.B., Abdelhamid K., Saad A., Ajina M. Altered antioxidant status and increased lipid per-oxidation in seminal plasma of tunisian infertile men. Int. J. Biol. Sci. 2012;8:139–149. doi: 10.7150/ijbs.8.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Aktan G., Doğru-Abbasoğlu S., Küçükgergin C., Kadıoğlu A., Ozdemirler-Erata G., Koçak-Toker N. Mystery of idiopathic male infertility: Is oxidative stress an actual risk? Fertil. Steril. 2013;99:1211–1215. doi: 10.1016/j.fertnstert.2012.11.045. [DOI] [PubMed] [Google Scholar]
- 73.Shamsi M.B., Kumar R., Malhotra N., Singh N., Mittal S., Upadhyay A.D., Dada R. Chromosomal aberrations, Yq microdeletion, and sperm DNA fragmentation in infertile men opting for assisted reproduction. Mol. Reprod. Dev. 2012;79:637–650. doi: 10.1002/mrd.22072. [DOI] [PubMed] [Google Scholar]
- 74.Guz J., Gackowski D., Foksinski M., Rozalski R., Zarakowska E., Siomek A., Szpila A., Kotzbach M., Kotzbach R., Olinski R. Comparison of oxidative stress/DNA damage in semen and blood of fertile and infertile men. PLoS ONE. 2013;8:e68490. doi: 10.1371/journal.pone.0068490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.De Iuliis G.N., Thomson L.K., Mitchell L.A., Finnie J.M., Koppers A.J., Hedges A., Nixon B., Aitken R.J. DNA damage in human spermatozoa is highly correlated with the efficiency of chromatin remodeling and the formation of 8-hydroxy-2’-deoxyguanosine, a marker of oxidative stress. Biol. Reprod. 2009;81:517–524. doi: 10.1095/biolreprod.109.076836. [DOI] [PubMed] [Google Scholar]
- 76.Doshi S.B., Khullar K., Sharma R.K., Agarwal A. Role of reactive nitrogen species in male infertility. Reprod. Biol. Endocrinol. 2012;10:109. doi: 10.1186/1477-7827-10-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lord T., Aitken R.J. Fertilization stimulates 8-hydroxy-2’-deoxyguanosine repair and antioxidant activity to prevent mutagenesis in the embryo. Dev. Biol. 2015;406:1–13. doi: 10.1016/j.ydbio.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 78.Smith T.B., Dun M.D., Smith N.D., Curry B.J., Connaughton H.S., Aitken R.J. The presence of a truncated base excision repair pathway in human spermatozoa that is mediated by OGG1. J. Cell Sci. 2013;126:1488–1497. doi: 10.1242/jcs.121657. [DOI] [PubMed] [Google Scholar]
- 79.Zheng P., Schramm R.D., Latham K.E. Developmental regulation and in vitro culture effects on expression of DNA repair and cell cycle checkpoint control genes in rhesus monkey oocytes and embryos. Biol. Reprod. 2005;72:1359–1369. doi: 10.1095/biolreprod.104.039073. [DOI] [PubMed] [Google Scholar]
- 80.Menezo Y., Jr., Russo G., Tosti E., El Mouatassim S., Benkhalifa M. Expression profile of genes coding for DNA repair in human oocytes using pangenomic microarrays, with a special focus on ROS linked decays. J. Assist. Reprod. Genet. 2007;24:513–520. doi: 10.1007/s10815-007-9167-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shimura T., Inoue M., Taga M., Shiraishi K., Uematsu N., Takei N., Yuan Z.M., Shinohara T., Niwa O. p53-dependent S-phase damage checkpoint and pronuclear cross talk in mouse zygotes with X-irradiated sperm. Mol. Cell. Biol. 2002;22:2220–2228. doi: 10.1128/MCB.22.7.2220-2228.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Adiga S.K., Toyoshima M., Shiraishi K., Shimura T., Takeda J., Taga M., Nagai H., Kumar P., Niwa O. p21 provides stage specific DNA damage control to preimplantation embryos. Oncogene. 2007;26:6141–6149. doi: 10.1038/sj.onc.1210444. [DOI] [PubMed] [Google Scholar]
- 83.Gawecka J.E., Marh J., Ortega M., Yamauchi Y., Ward M.A., Ward W.S. Mouse zygotes respond to severe sperm DNA damage by delaying paternal DNA replication and embryonic development. PLoS ONE. 2013;8:e56385. doi: 10.1371/journal.pone.0056385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Khokhlova E.V., Fesenko Z.S., Sopova J.V., Leonova E.I. Features of DNA repair in the early stages of mammalian embryonic development. Genes. 2020;11:1138. doi: 10.3390/genes11101138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lane M., McPherson N.O., Fullston T., Spillane M., Sandeman L., Kang W.X., Zander-Fox D.L. Oxidative stress in mouse sperm impairs embryo development, fetal growth and alters adiposity and glucose regulation in female offspring. PLoS ONE. 2014;9:e100832. doi: 10.1371/journal.pone.0100832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kumar S.B., Chawla B., Bisht S., Yadav R.K., Dada R. Tobacco use increases oxidative DNA damage in sperm—Possible etiology of childhood cancer. Asian. Pac. J. Cancer Prev. 2015;16:6967–6972. doi: 10.7314/APJCP.2015.16.16.6967. [DOI] [PubMed] [Google Scholar]
- 87.Aitken R.J., De Iuliis G.N., McLachlan R.I. Biological and clinical significance of DNA damage in the male germ line. Int. J. Androl. 2009;32:46–56. doi: 10.1111/j.1365-2605.2008.00943.x. [DOI] [PubMed] [Google Scholar]
- 88.Cissen M., Wely M.V., Scholten I., Mansell S., Bruin J.P., Mol B.W., Braat D., Repping S., Hamer G. Measuring sperm DNA fragmentation and clinical outcomes of medically assisted reproduction: A systematic review and meta-analysis. PLoS ONE. 2016;11:e0165125. doi: 10.1371/journal.pone.0165125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Agarwal A., Majzoub A., Baskaran S., Panner Selvam M.K., Cho C.L., Henkel R., Finelli R., Leisegang K., Sengupta P., Barbarosie C., et al. Sperm DNA fragmentation: A new guideline for clinicians. World J. Mens. Health. 2020;38:412–471. doi: 10.5534/wjmh.200128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Titus S., Li F., Stobezki R., Akula K., Unsal E., Jeong K., Dickler M., Robson M., Moy F., Goswami S. Impairment of BRCA1-related DNA double-strand break repair leads to ovarian aging in mice and humans. Sci. Transl. Med. 2013;5:172ra121. doi: 10.1126/scitranslmed.3004925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Oktay K., Turan V., Titus S., Stobezki R., Liu L. BRCA mutations, DNA repair deficiency, and ovarian aging. Biol. Reprod. 2015;93:1–10. doi: 10.1095/biolreprod.115.132290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Horta F., Catt S., Ramachandran P., Vollenhoven B., Temple-Smith P. Female ageing affects the DNA repair capacity of oocytes in IVF using a controlled model of sperm DNA damage in mice. Hum. Reprod. 2020;35:529–544. doi: 10.1093/humrep/dez308. [DOI] [PubMed] [Google Scholar]
- 93.Agarwal A., Virk G., Ong C., du Plessis S.S. Effect of oxidative stress on male reproduction. World J. Mens. Health. 2014;32:1. doi: 10.5534/wjmh.2014.32.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Aitken R.J., West K., Buckingham D. Leukocytic infiltration into the human ejaculate and its association with semen quality, oxidative stress, and sperm function. J. Androl. 1994;15:343–352. [PubMed] [Google Scholar]
- 95.Henkel R.R. Leukocytes and oxidative stress: Dilemma for sperm function and male fertility. Asian J. Androl. 2011;13:43–52. doi: 10.1038/aja.2010.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sandoval J.S., Raburn D., Muasher S. Leukocytospermia: Overview of diagnosis, implications, and management of a controversial finding. Middle East Fertil. Soc. J. 2013;18:129–134. doi: 10.1016/j.mefs.2013.02.004. [DOI] [Google Scholar]
- 97.Jung J.H., Kim M.H., Kim J., Baik S.K., Koh S.B., Park H.J., Seo J.T. Treatment of leukocytospermia in male infertility: A systematic review. World J. Mens. Health. 2016;34:165–172. doi: 10.5534/wjmh.2016.34.3.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Saleh R.A., Agarwal A., Kandirali E., Sharma R.K., Thomas A.J., Nada E.A., Evenson D.P., Alvarez J.G. Leukocytospermia is associated with increased reactive oxygen species production by human spermatozoa. Fertil. Steril. 2002;78:1215–1224. doi: 10.1016/S0015-0282(02)04237-1. [DOI] [PubMed] [Google Scholar]
- 99.Castellini C., D’Andrea S., Martorella A., Minaldi E., Necozione S., Francavilla F., Francavilla S., Barbonetti A. Relationship between leukocytospermia, reproductive potential after assisted reproductive technology, and sperm parameters: A systematic review and meta-analysis of case-control studies. Andrology. 2020;8:125–135. doi: 10.1111/andr.12662. [DOI] [PubMed] [Google Scholar]
- 100.Huszar G., Corrales M., Vigue L. Correlation between sperm creatine phosphokinase activity and sperm concentrations in normospermic and oligospermic men. Gamete Res. 1988;19:67–75. doi: 10.1002/mrd.1120190107. [DOI] [PubMed] [Google Scholar]
- 101.Huszar G., Vigue L., Corrales M. Sperm creatine phosphokinase activity as a measure of sperm quality in normospermic, variablespermic, and oligospermic men. Biol. Reprod. 1988;38:1061–1066. doi: 10.1095/biolreprod38.5.1061. [DOI] [PubMed] [Google Scholar]
- 102.Huszar G., Vigue L., Corrales M. Sperm creatine kinase activity in fertile and infertile oligospermic men. J. Androl. 1990;11:40–46. [PubMed] [Google Scholar]
- 103.Aitken J., Krausz C., Buckingham D. Relationships between biochemical markers for residual sperm cytoplasm, reactive oxygen species generation, and the presence of leukocytes and precursor germ cells in human sperm suspensions. Mol. Reprod. Dev. 1994;39:268–279. doi: 10.1002/mrd.1080390304. [DOI] [PubMed] [Google Scholar]
- 104.Aitken R.J., Fisher H.M., Fulton N., Gomez E., Knox W., Lewis B., Irvine S. Reactive oxygen species generation by human spermatozoa is induced by exogenous NADPH and inhibited by the flavoprotein inhibitors diphenylene iodonium and quinacrine. Mol. Reprod. Dev. 1997;47:468–482. doi: 10.1002/(SICI)1098-2795(199708)47:4<468::AID-MRD14>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 105.Donà G., Fiore C., Andrisani A., Ambrosini G., Brunati A., Ragazzi E., Armanini D., Bordin L., Clari G. Evaluation of correct endogenous reactive oxygen species content for human sperm capacitation and involvement of the NADPH oxidase system. Hum. Reprod. 2011;26:3264–3273. doi: 10.1093/humrep/der321. [DOI] [PubMed] [Google Scholar]
- 106.Williams A.C., Ford W.C. Functional significance of the pentose phosphate pathway and glutathione reductase in the antioxidant defenses of human sperm. Biol. Reprod. 2004;71:1309–1316. doi: 10.1095/biolreprod.104.028407. [DOI] [PubMed] [Google Scholar]
- 107.Gil-Guzman E., Ollero M., Lopez M.C., Sharma R.K., Alvarez J.G., Thomas A.J., Jr., Agarwal A. Differential production of reactive oxygen species by subsets of human spermatozoa at different stages of maturation. Hum. Reprod. 2001;16:1922–1930. doi: 10.1093/humrep/16.9.1922. [DOI] [PubMed] [Google Scholar]
- 108.Ollero M., Gil-Guzman E., Lopez M.C., Sharma R.K., Agarwal A., Larson K., Evenson D., Thomas A.J., Jr., Alvarez J.G. Characterization of subsets of human spermatozoa at different stages of maturation: Implications in the diagnosis and treatment of male infertility. Hum. Reprod. 2001;16:1912–1921. doi: 10.1093/humrep/16.9.1912. [DOI] [PubMed] [Google Scholar]
- 109.Koppers A.J., Garg M.L., Aitken R.J. Stimulation of mitochondrial reactive oxygen species production by unesterified, unsaturated fatty acids in defective human spermatozoa. Free Radic. Biol. Med. 2010;48:112–119. doi: 10.1016/j.freeradbiomed.2009.10.033. [DOI] [PubMed] [Google Scholar]
- 110.Keshtgar S., Fanaei H., Bahmanpour S., Azad F., Ghannadi A., Kazeroni M. In vitro effects of α-tocopherol on teratozoospermic semen samples. Andrologia. 2012;44:721–727. doi: 10.1111/j.1439-0272.2011.01256.x. [DOI] [PubMed] [Google Scholar]
- 111.Rengan A.K., Agarwal A., van der Linde M., du Plessis S.S. An investigation of excess residual cytoplasm in human spermatozoa and its distinction from the cytoplasmic droplet. Reprod. Biol. Endocrinol. 2012;10:92. doi: 10.1186/1477-7827-10-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ghani E., Keshtgar S., Habibagahi M., Ghannadi A., Kazeroni M. Expression of NOX5 in human teratozoospermia compared to normozoospermia. Andrologia. 2013;45:351–356. doi: 10.1111/and.12023. [DOI] [PubMed] [Google Scholar]
- 113.Simon L., Liu L., Murphy K., Ge S., Hotaling J., Aston K.I., Emery B., Carrell D.T. Comparative analysis of three sperm DNA damage assays and sperm nuclear protein content in couples undergoing assisted reproduction treatment. Hum. Reprod. 2014;29:904–917. doi: 10.1093/humrep/deu040. [DOI] [PubMed] [Google Scholar]
- 114.Kumar A., Prasad J.K., Srivastava N., Ghosh S.K. Strategies to minimize various stress-related freeze-thaw damages during conventional cryopreservation of mammalian spermatozoa. Biopreserv. Biobank. 2019;17:603–612. doi: 10.1089/bio.2019.0037. [DOI] [PubMed] [Google Scholar]
- 115.Ball B.A., Vo A.T., Baumber J. Generation of reactive oxygen species by equine spermatozoa. Am. J. Vet. Res. 2001;62:508–515. doi: 10.2460/ajvr.2001.62.508. [DOI] [PubMed] [Google Scholar]
- 116.Upreti G.C., Jensen K., Munday R., Duganzich D.M., Vishwanath R., Smith J.F. Studies on aromatic amino acid oxidase activity in ram spermatozoa: Role of pyruvate as an antioxidant. Anim. Reprod. Sci. 1998;51:275–287. doi: 10.1016/S0378-4320(98)00082-7. [DOI] [PubMed] [Google Scholar]
- 117.Roca J., Martinez-Alborcia M.J., Gil M.A., Parrilla I., Martinez E.A. Dead spermatozoa in raw semen samples impair in vitro fertilization outcomes of frozen-thawed spermatozoa. Fertil. Steril. 2013;100:875–881. doi: 10.1016/j.fertnstert.2013.05.020. [DOI] [PubMed] [Google Scholar]
- 118.Shannon P., Curson B. Toxic effect and action of dead sperm on diluted bovine semen. J. Dairy Sci. 1972;55:614–620. doi: 10.3168/jds.S0022-0302(72)85544-9. [DOI] [PubMed] [Google Scholar]
- 119.Shannon P., Curson B. Site of aromatic L-amino acid oxidase in dead bovine spermatozoa and determination of between-bull differences in the percentage of dead spermatozoa by oxidase activity. J. Reprod. Fertil. 1982;64:469–473. doi: 10.1530/jrf.0.0640469. [DOI] [PubMed] [Google Scholar]
- 120.Aitken J.B., Naumovski N., Curry B., Grupen C.G., Gibb Z., Aitken R.J. Characterization of an L-amino acid oxidase in equine spermatozoa. Biol. Reprod. 2015;92:1–13. doi: 10.1095/biolreprod.114.126052. [DOI] [PubMed] [Google Scholar]
- 121.Houston B., Curry B., Aitken R.J. Human spermatozoa possess an IL4I1 l-amino acid oxidase with a potential role in sperm function. Reproduction. 2015;149:587–596. doi: 10.1530/REP-14-0621. [DOI] [PubMed] [Google Scholar]
- 122.Lewis S.E., Sterling E.S., Young I.S., Thompson W. Comparison of individual antioxidants of sperm and seminal plasma in fertile and infertile men. Fertil. Steril. 1997;67:142–147. doi: 10.1016/S0015-0282(97)81871-7. [DOI] [PubMed] [Google Scholar]
- 123.Pahune P.P., Choudhari A.R., Muley P.A. The total antioxidant power of semen and its correlation with the fertility potential of human male subjects. J. Clin. Diagn. Res. 2013;7:991–995. doi: 10.7860/JCDR/2013/4974.3040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Aitken R.J., Clarkson J.S. Cellular basis of defective sperm function and its association with the genesis of reactive oxygen species by human spermatozoa. J. Reprod. Fertil. 1987;81:459–469. doi: 10.1530/jrf.0.0810459. [DOI] [PubMed] [Google Scholar]
- 125.Aitken R.J., Clarkson J.S. Significance of reactive oxygen species and antioxidants in defining the efficacy of sperm preparation techniques. J. Androl. 1988;9:367–376. doi: 10.1002/j.1939-4640.1988.tb01067.x. [DOI] [PubMed] [Google Scholar]
- 126.Sharma R.K., Pasqualotto A.E., Nelson D.R., Thomas A.J., Jr., Agarwal A. Relationship between seminal white blood cell counts and oxidative stress in men treated at an infertility clinic. J. Androl. 2001;22:575–583. [PubMed] [Google Scholar]
- 127.Leahy T., Gadella B.M. Sperm surface changes and physiological consequences induced by sperm handling and storage. Reproduction. 2011;142:759–778. doi: 10.1530/REP-11-0310. [DOI] [PubMed] [Google Scholar]
- 128.Shekarriz M., De Wire D.M., Thomas A.J., Jr., Agarwal A. A method of human semen centrifugation to minimize the iatrogenic sperm injuries caused by reactive oxygen species. Eur. Urol. 1995;28:31–35. doi: 10.1159/000475016. [DOI] [PubMed] [Google Scholar]
- 129.McKinney K.A., Lewis S.E., Thompson W. Reactive oxygen species generation in human sperm: Luminol and lucigenin chemiluminescence probes. Arch. Androl. 1996;36:119–125. doi: 10.3109/01485019608987087. [DOI] [PubMed] [Google Scholar]
- 130.Iwasaki A., Gagnon C. Formation of reactive oxygen species in spermatozoa of infertile patients. Fertil. Steril. 1992;57:409–416. doi: 10.1016/S0015-0282(16)54855-9. [DOI] [PubMed] [Google Scholar]
- 131.Takeshima T., Yumura Y., Kuroda S., Kawahara T., Uemura H., Iwasaki A. Effect of density gradient centrifugation on reactive oxygen species in human semen. Syst. Biol. Reprod. Med. 2017;63:192–198. doi: 10.1080/19396368.2017.1294214. [DOI] [PubMed] [Google Scholar]
- 132.Malvezzi H., Sharma R., Agarwal A., Abuzenadah A.M., Abu-Elmagd M. Sperm quality after density gradient centrifugation with three commercially available media: A controlled trial. Reprod. Biol. Endocrinol. 2014;12:121–127. doi: 10.1186/1477-7827-12-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhao F., Yang Q., Shi S., Luo X., Sun Y. Semen preparation methods and sperm telomere length: Density gradient centrifugation versus the swim up procedure. Sci. Rep. 2016;6:39051–39056. doi: 10.1038/srep39051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Aitken R.J., Finnie J.M., Muscio L., Whiting S., Connaughton H.S., Kuczera L., Rothkirch T.B., De Iuliis G.N. Potential importance of transition metals in the induction of DNA damage by sperm preparation media. Hum. Reprod. 2014;29:2136–2147. doi: 10.1093/humrep/deu204. [DOI] [PubMed] [Google Scholar]
- 135.Muratori M., Tarozzi N., Cambi M., Boni L., Iorio A.L., Passaro C., Luppino B., Nadalini M., Marchiani S., Tamburrino L., et al. Variation of DNA fragmentation levels during density gradient sperm selection for assisted reproduction techniques: A possible new male predictive parameter of pregnancy? Medicine. 2016;95:e3624–e3632. doi: 10.1097/MD.0000000000003624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Muratori M., Tarozzi N., Carpentiero F., Danti S., Perrone F.M., Cambi M., Casini A., Azzari C., Boni L., Maggi M., et al. Sperm selection with density gradient centrifugation and swim up: Effect on DNA fragmentation in viable spermatozoa. Sci. Rep. 2019;9:7492–7502. doi: 10.1038/s41598-019-43981-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Lee T.H., Liu C.H., Shih Y.T., Tsao H.M., Huang C.C., Chen H.H., Lee M.S. Magnetic-activated cell sorting for sperm preparation reduces spermatozoa with apoptotic markers and improves the acrosome reaction in couples with unexplained infertility. Hum. Reprod. 2010;25:839–846. doi: 10.1093/humrep/deq009. [DOI] [PubMed] [Google Scholar]
- 138.Parmegiani L., Cognigni G.E., Bernardi S., Troilo E., Ciampaglia W., Filicori M. ‘Physiologic ICSI’, Hyaluronic acid (HA) favors selection of spermatozoa without DNA fragmentation and with normal nucleus, resulting in improvement of embryo quality. Fertil. Steril. 2010;93:598–604. doi: 10.1016/j.fertnstert.2009.03.033. [DOI] [PubMed] [Google Scholar]
- 139.Hammoud I., Boitrelle F., Ferfouri F., Vialard F., Bergere M., Wainer B., Bailly M., Albert M., Selva J. Selection of normal spermatozoa with a vacuole-free head (x6300) improves selection of spermatozoa with intact DNA in patients with high sperm DNA fragmentation rates. Andrologia. 2013;45:163–170. doi: 10.1111/j.1439-0272.2012.01328.x. [DOI] [PubMed] [Google Scholar]
- 140.Maettner R., Sterzik K., Isachenko V., Strehler E., Rahimi G., Alabart J.L., Sánchez R., Mallmann P., Isachenko E. Quality of human spermatozoa: Relationship between high-magnification sperm morphology and DNA integrity. Andrologia. 2014;46:547–555. doi: 10.1111/and.12114. [DOI] [PubMed] [Google Scholar]
- 141.Rappa K.L., Rodriguez H.F., Hakkarainen G.C., Anchan R.M., Mutter G.L., Asghar W. Sperm processing for advanced reproductive technologies: Where are we today? Biotechnol. Adv. 2016;34:578–587. doi: 10.1016/j.biotechadv.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 142.Bradley C.K., McArthur S.J., Gee A.J., Weiss K.A., Schmidt U., Toogood L. Intervention improves assisted conception intracytoplasmic sperm injection outcomes for patients with high levels of sperm DNA fragmentation: A retrospective analysis. Andrology. 2016;4:903–910. doi: 10.1111/andr.12215. [DOI] [PubMed] [Google Scholar]
- 143.Asghar W., Velasco V., Kingsley J.L., Shoukat M.S., Shafiee H., Anchan R.M., Mutter G.L., Tüzel E., Demirci U. Selection of functional human sperm with higher DNA integrity and fewer reactive oxygen species. Adv. Healthc. Mater. 2014;3:1671–1679. doi: 10.1002/adhm.201400058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ebner T., Shebl O., Moser M., Mayer R.B., Arzt W., Tews G. Easy sperm processing technique allowing exclusive accumulation and later usage of DNA-strandbreak-free spermatozoa. Reprod. Biomed. Online. 2011;22:37–43. doi: 10.1016/j.rbmo.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 145.Duarte C., Núñez V., Wong Y., Vivar C., Benites E., Rodriguez U., Vergara C., Ponce J. Impact of the Z potential technique on reducing the sperm DNA fragmentation index, fertilization rate and embryo development. JBRA Assist Reprod. 2017;21:351–355. doi: 10.5935/1518-0557.20170055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ainsworth C., Nixon B., Aitken R.J. Development of a novel electrophoretic system for the isolation of human spermatozoa. Hum. Reprod. 2005;20:2261–2270. doi: 10.1093/humrep/dei024. [DOI] [PubMed] [Google Scholar]
- 147.Aitken R.J., Hanson A.R., Kuczera L. Electrophoretic sperm isolation: Optimization of electrophoresis conditions and impact on oxidative stress. Hum. Reprod. 2011;26:1955–1964. doi: 10.1093/humrep/der162. [DOI] [PubMed] [Google Scholar]
- 148.Simon L., Murphy K., Aston K.I., Emery B.R., Hotaling J.M., Carrell D.T. Micro-electrophoresis: A noninvasive method of sperm selection based on membrane charge. Fertil. Steril. 2015;103:361–366. doi: 10.1016/j.fertnstert.2014.10.047. [DOI] [PubMed] [Google Scholar]
- 149.Banihani S., Sharma R., Bayachou M., Sabanegh E., Agarwal A. Human sperm DNA oxidation, motility and viability in the presence of L-carnitine during in vitro incubation and centrifugation. Andrologia. 2012;44:505–512. doi: 10.1111/j.1439-0272.2011.01216.x. [DOI] [PubMed] [Google Scholar]
- 150.Gualtieri R., Barbato V., Fiorentino I., Braun S., Rizos D., Longobardi S., Talevi R. Treatment with zinc, d-aspartate, and coenzyme Q10 protects bull sperm against damage and improves their ability to support embryo development. Theriogenology. 2014;82:592–598. doi: 10.1016/j.theriogenology.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 151.Nematollahi S., Mehdizadeh M., Hosseini S., Kashanian M., Amjadi F.S., Salehi M. DNA integrity and methylation changes of mouse spermatozoa following prolonged incubation. Andrologia. 2019;51:e13276. doi: 10.1111/and.13276. [DOI] [PubMed] [Google Scholar]
- 152.Calamera J.C., Fernandez P.J., Buffone M.G., Acosta A.A., Doncel G.F. Effects of long-term in vitro incubation of human spermatozoa: Functional parameters and catalase effect. Andrologia. 2001;33:79–86. doi: 10.1046/j.1439-0272.2001.00409.x. [DOI] [PubMed] [Google Scholar]
- 153.Talevi R., Barbato V., Fiorentino I., Braun S., Longobardi S., Gualtieri R. Protective effects of in vitro treatment with zinc, d-aspartate and coenzyme q10 on human sperm motility, lipid peroxidation and DNA fragmentation. Reprod. Biol. Endocrinol. 2013;11:81–90. doi: 10.1186/1477-7827-11-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Nabi A., Khalili M.A., Halvaei I., Roodbari F. Prolonged incubation of processed human spermatozoa will increase DNA fragmentation. Andrologia. 2014;46:374–379. doi: 10.1111/and.12088. [DOI] [PubMed] [Google Scholar]
- 155.López-Fernández C., Johnston S.D., Fernández J.L., Wilson R.J., Gosálvez J. Fragmentation dynamics of frozen-thawed ram sperm DNA is modulated by sperm concentration. Theriogenology. 2010;74:1362–1370. doi: 10.1016/j.theriogenology.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 156.Murphy C., Fahey A.G., Shafat A., Fair S. Reducing sperm concentration is critical to limiting the oxidative stress challenge in liquid bull semen. J. Dairy Sci. 2013;96:4447–4454. doi: 10.3168/jds.2012-6484. [DOI] [PubMed] [Google Scholar]
- 157.Andrisani A., Donà G., Ambrosini G., Bonanni G., Bragadin M., Cosmi E., Clari G., Armanini D., Bordin L. Effect of various commercial buffers on sperm viability and capacitation. Syst. Biol. Reprod. Med. 2014;60:239–244. doi: 10.3109/19396368.2014.904952. [DOI] [PubMed] [Google Scholar]
- 158.Panner Selvam M.K., Henkel R., Sharma R., Agarwal A. Calibration of redox potential in sperm wash media and evaluation of oxidation-reduction potential values in various assisted reproductive technology culture media using MiOXSYS system. Andrology. 2018;6:293–300. doi: 10.1111/andr.12461. [DOI] [PubMed] [Google Scholar]
- 159.Griveau J.F., Grizard G., Boucher D., Le Lannou D. Influence of oxygen tension on function of isolated spermatozoa from ejaculates of oligozoospermic patients and normozoospermic fertile donors. Hum. Reprod. 1998;13:3108–3113. doi: 10.1093/humrep/13.11.3108. [DOI] [PubMed] [Google Scholar]
- 160.Balasuriya A., Serhal P., Doshi A., Harper J.C. Processes involved in assisted reproduction technologies significantly increase sperm DNA fragmentation and phosphatidylserine translocation. Andrologia. 2014;46:86–97. doi: 10.1111/and.12052. [DOI] [PubMed] [Google Scholar]
- 161.Thijssen A., Klerkx E., Huyser C., Bosmans E., Campo R., Ombelet W. Influence of temperature and sperm preparation on the quality of spermatozoa. Reprod. Biomed. Online. 2014;28:436–442. doi: 10.1016/j.rbmo.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 162.Matsuura R., Takeuchi T., Yoshida A. Preparation and incubation conditions affect the DNA integrity of ejaculated human spermatozoa. Asian J. Androl. 2010;12:753–759. doi: 10.1038/aja.2010.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Parshad R., Taylor W.G., Sanford K.K., Camalier R.F., Gantt R., Tarone R.E. Fluorescent light-induced chromosome damage in human IMR-90 fibroblasts. Role of hydrogen peroxide and related free radicals. Mutat. Res. 1980;73:115–124. doi: 10.1016/0027-5107(80)90140-2. [DOI] [PubMed] [Google Scholar]
- 164.Hockberger P.E., Skimina T.A., Centonze V.E., Lavin C., Chu S., Dadras S., Reddy J.K., White J.G. Activation of flavin-containing oxidases underlies light-induced production of H2O2 in mammalian cells. Proc. Natl. Acad. Sci. USA. 1999;96:6255–6260. doi: 10.1073/pnas.96.11.6255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Batista L.F.Z., Kaina B., Meneghini R., Menck C.F.M. How DNA lesions are turned into powerful killing structures: Insights from UV-induced apoptosis. Mutat. Res. 2009;681:197–208. doi: 10.1016/j.mrrev.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 166.Agarwal A., Durairajanayagam D., du Plessis S.S. Utility of antioxidants during assisted reproductive techniques: An evidence based review. Reprod. Biol. Endocrinol. 2014;12:112. doi: 10.1186/1477-7827-12-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Baldi E., Tamburrino L., Muratori M., Degl’Innocenti S., Marchiani S. Adverse effects of in vitro manipulation of spermatozoa. Anim. Reprod. Sci. 2020;220:106314. doi: 10.1016/j.anireprosci.2020.106314. [DOI] [PubMed] [Google Scholar]
- 168.Preece D., Chow K.W., Gomez-Godinez V., Gustafson K., Esener S., Ravida N., Durrant B., Berns M.W. Red light improves spermatozoa motility and does not induce oxidative DNA damage. Sci. Rep. 2017;7:46480. doi: 10.1038/srep46480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Firestone R.S., Esfandiari N., Moskovtsev S.I., Burstein E., Videna G.T., Librach C., Bentov Y., Casper R.F. The effects of low-level laser light exposure on sperm motion characteristics and DNA damage. J. Androl. 2012;33:469–473. doi: 10.2164/jandrol.111.013458. [DOI] [PubMed] [Google Scholar]
- 170.Ríos-Ramírez M., Espinoza J.H., Ruiz-Suárez J.C., Mercado-Uribe H. The effect of green light on the motility of mouse sperm at two different temperatures. Photochem. Photobiol. Sci. 2019;18:2893–2900. doi: 10.1039/C9PP00258H. [DOI] [PubMed] [Google Scholar]
- 171.Abush A., Hauser R., Paz G., Kleiman S.E., Lehavi O., Yavetz H., Yogev L. Thawed human sperm quality is influenced by the volume of the cryopreserved specimen. Fertil. Steril. 2014;101:640–646. doi: 10.1016/j.fertnstert.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 172.Kopeika J., Thornhill A., Khalaf Y. The effect of cryopreservation on the genome of gametes and embryos: Principles of cryobiology and critical appraisal of the evidence. Hum. Reprod. Update. 2015;21:209–227. doi: 10.1093/humupd/dmu063. [DOI] [PubMed] [Google Scholar]
- 173.Najafi A., Asadi E., Moawad A.R., Mikaeili S., Amidi F., Adutwum E., Safa M., Sobhani A.G. Supplementation of freezing and thawing media with brain-derived neurotrophic factor protects human sperm from freeze-thaw-induced damage. Fertil. Steril. 2016;106:1658–1665.e4. doi: 10.1016/j.fertnstert.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 174.Paoli D., Pelloni M., Lenzi A., Lombardo F. Cryopreservation of sperm: Effects on chromatin and strategies to prevent them. Adv. Exp. Med. Biol. 2019;1166:149–167. doi: 10.1007/978-3-030-21664-1_9. [DOI] [PubMed] [Google Scholar]
- 175.Degl’Innocenti S., Filimberti E., Magini A., Krausz C., Lombardi G., Fino M.G., Rastrelli G., Maggi M., Baldi E. Semen cryopreservation for men banking for oligospermia, cancers, and other pathologies: Prediction of post-thaw outcome using basal semen quality. Fertil. Steril. 2013;100:e1–e3. doi: 10.1016/j.fertnstert.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 176.Oehninger S., Duru N.K., Srisombut C., Morshedi M. Assessment of sperm cryodamage and strategies to improve outcome. Mol. Cell. Endocrinol. 2000;169:3–10. doi: 10.1016/S0303-7207(00)00343-9. [DOI] [PubMed] [Google Scholar]
- 177.Kalthur G., Adiga S.K., Upadhya D., Rao S., Kumar P. Effect of cryopreservation on sperm DNA integrity in patients with teratospermia. Fertil. Steril. 2008;89:1723–1727. doi: 10.1016/j.fertnstert.2007.06.087. [DOI] [PubMed] [Google Scholar]
- 178.Brugnon F., Ouchchane L., Pons-Rejraji H., Artonne C., Farigoule M., Janny L. Density gradient centrifugation prior to cryopreservation and hypotaurine supplementation improve post-thaw quality of sperm from infertile men with oligoasthenoteratozoospermia. Hum. Reprod. 2013;28:2045–2057. doi: 10.1093/humrep/det253. [DOI] [PubMed] [Google Scholar]
- 179.Barbato V., Talevi R., Braun S., Merolla A., Sudhakaran S., Longobardi S., Gualtieri R. Supplementation of sperm media with zinc, D-aspartate and co-enzyme Q10 protects bull sperm against exogenous oxidative stress and improves their ability to support embryo development. Zygote. 2017;25:168–175. doi: 10.1017/S0967199416000459. [DOI] [PubMed] [Google Scholar]
- 180.Ribas-Maynou J., Yeste M., Salas-Huetos A. The relationship between sperm oxidative stress alterations and IVF/ICSI outcomes: A systematic review from nonhuman mammals. Biology. 2020;9:178. doi: 10.3390/biology9070178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ezzati M., Shanehbandi D., Hamdi K., Rahbar S., Pashaiasl M. Influence of cryopreservation on structure and function of mammalian spermatozoa: An overview. Cell Tissue Bank. 2020;21:1–15. doi: 10.1007/s10561-019-09797-0. [DOI] [PubMed] [Google Scholar]
- 182.Gualtieri R., Kalthur G., Barbato V., Di Nardo M., Adiga S.K., Talevi R. Mitochondrial dysfunction and oxidative stress caused by cryopreservation in reproductive cells. Antioxidants. 2021;10:337. doi: 10.3390/antiox10030337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.de Castro L.S., de Assis P.M., Siqueira A.F., Hamilton T.R., Mendes C.M., Losano J.D., Nichi M., Visintin J.A., Assumpção M.E. Sperm oxidative stress is detrimental to embryo development: A dose-dependent study model and a new and more sensitive oxidative status evaluation. Oxid. Med. Cell. Longev. 2016;2016:8213071. doi: 10.1155/2016/8213071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Bittner L., Wyck S., Herrera C., Siuda M., Wrenzycki C., van Loon B., Bollwein H. Negative effects of oxidative stress in bovine spermatozoa on in vitro development and DNA integrity of embryos. Reprod. Fertil. Dev. 2018;30:1359–1368. doi: 10.1071/RD17533. [DOI] [PubMed] [Google Scholar]
- 185.Ghaleno L.R., Valojerdi M.R., Hassani F., Chehrazi M., Janzamin E. High level of intracellular sperm oxidative stress negatively influences embryo pronuclear formation after intracytoplasmic sperm injection treatment. Andrologia. 2014;46:1118–1127. doi: 10.1111/and.12202. [DOI] [PubMed] [Google Scholar]
- 186.Adiga S.K., Upadhya D., Kalthur G., Bola Sadashiva S.R., Kumar P. Transgenerational changes in somatic and germ line genetic integrity of first-generation offspring derived from the DNA damaged sperm. Fertil. Steril. 2010;93:2486–2490. doi: 10.1016/j.fertnstert.2009.06.015. [DOI] [PubMed] [Google Scholar]
- 187.Kumar D., Upadhya D., Salian S.R., Rao S.B., Kalthur G., Kumar P., Adiga S.K. The extent of paternal sperm DNA damage influences early post-natal survival of first generation mouse offspring. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013;166:164–167. doi: 10.1016/j.ejogrb.2012.09.021. [DOI] [PubMed] [Google Scholar]
- 188.Uppangala S., Pudakalakatti S., D’souza F., Salian S.R., Kalthur G., Kumar P., Atreya H., Adiga S.K. Influence of sperm DNA damage on human preimplantation embryo metabolism. Reprod. Biol. 2016;16:234–241. doi: 10.1016/j.repbio.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 189.Souza F.D., Asampille G., Uppangala S., Kalthur G., Atreya H.S., Adiga S.K. Sperm-mediated DNA lesions alter metabolite levels in spent embryo culture medium. Reprod. Fertil. Dev. 2019;31:443–450. doi: 10.1071/RD18136. [DOI] [PubMed] [Google Scholar]
- 190.Champroux A., Torres-Carreira J., Gharagozloo P., Drevet J.R., Kocer A. Mammalian sperm nuclear organization: Resiliencies and vulnerabilities. Basic. Clin. Androl. 2016;26:17. doi: 10.1186/s12610-016-0044-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Simões R., Feitosa W.B., Siqueira A.F., Nichi M., Paula-Lopes F.F., Marques M.G., Peres M.A., Barnabe V.H., Visintin J.A., Assumpção M.E. Influence of bovine sperm DNA fragmentation and oxidative stress on early embryo in vitro development outcome. Reproduction. 2013;146:433–441. doi: 10.1530/REP-13-0123. [DOI] [PubMed] [Google Scholar]
- 192.Burruel V., Klooster K., Barker C.M., Pera R.R., Meyers S. Abnormal early cleavage events predict early embryo demise: Sperm oxidative stress and early abnormal cleavage. Sci. Rep. 2014;4:6598. doi: 10.1038/srep06598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Hammadeh M.E., Al Hasani S., Rosenbaum P., Schmidt W., Fischer Hammadeh C. Reactive oxygen species, total antioxidant concentration of seminal plasma and their effect on sperm parameters and outcome of IVF/ICSI patients. Arch. Gynecol. Obstet. 2008;277:515–526. doi: 10.1007/s00404-007-0507-1. [DOI] [PubMed] [Google Scholar]
- 194.Das S., Chattopadhyay R., Jana S.K., Narendra B.K., Chakraborty C., Chakravarty B., Chaudhury K. Cut-off value of reactive oxygen species for predicting semen quality and fertilization outcome. Syst. Biol. Reprod. Med. 2008;54:47–54. doi: 10.1080/19396360701883274. [DOI] [PubMed] [Google Scholar]
- 195.Loft S., Kold-Jensen T., Hjollund N.H., Giwercman A., Gyllemborg J., Ernst E., Olsen J., Scheike T., Poulsen H.E., Bonde J.P. Oxidative DNA damage in human sperm influences time to pregnancy. Hum. Reprod. 2003;18:1265–1272. doi: 10.1093/humrep/deg202. [DOI] [PubMed] [Google Scholar]
- 196.Pujol A., Obradors A., Esteo E., Costilla B., García D., Vernaeve V., Vassena R. Oxidative stress level in fresh ejaculate is not related to semen parameters or to pregnancy rates in cycles with donor oocytes. J. Assist. Reprod. Genet. 2016;33:529–534. doi: 10.1007/s10815-016-0660-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Kamkar N., Ramezanali F., Sabbaghian M. The relationship between sperm DNA fragmentation, free radicals and antioxidant capacity with idiopathic repeated pregnancy loss. Reprod. Biol. 2018;18:330–335. doi: 10.1016/j.repbio.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 198.Mohanty G., Swain N., Goswami C., Kar S., Samanta L. Histone retention, protein carbonylation, and lipid peroxidation in spermatozoa: Possible role in recurrent pregnancy loss. Syst. Biol. Reprod. Med. 2016;62:201–212. doi: 10.3109/19396368.2016.1148798. [DOI] [PubMed] [Google Scholar]
- 199.Pavin C.U.M., Leivas F.G., Santos F.W., Missio D., Mesquita F.S., Brum D.D.S. Cushioned centrifugation during sperm selection increases the fertilization and cleavage rates of cattle embryos produced in vitro. Anim. Reprod. Sci. 2020;219:106508. doi: 10.1016/j.anireprosci.2020.106508. [DOI] [PubMed] [Google Scholar]
- 200.Barak Y., Menezo Y., Veiga A., Elder K. A physiological replacement for polyvinylpyrrolidone (PVP) in assisted reproductive technology. Hum. Fert. 2001;4:99–103. doi: 10.1080/1464727012000199371. [DOI] [PubMed] [Google Scholar]
- 201.Balaban B., Lundin K., Morrell J.M., Tjellstrom H., Urman B., Holmes P.V. An alternative to PVP for slowing sperm prior to ICSI. Hum. Reprod. 2003;18:1887–1889. doi: 10.1093/humrep/deg385. [DOI] [PubMed] [Google Scholar]
- 202.Choe S.A., Tae J.C., Shin M.Y., Kim H.J., Kim C.H., Lee J.Y., Hwang D., Kim K.C., Suh C.S., Jee B.C. Application of sperm selection using hyaluronic acid binding in intracytoplasmic sperm injection cycles: A sibling oocyte study. J. Korean Med. Sci. 2012;27:1569–1573. doi: 10.3346/jkms.2012.27.12.1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Roychoudhury S., Maldonado-Rosas I., Agarwal A., Esteves S.C., Henkel R., Sharma R. Human sperm handling in intracytoplasmic sperm injection processes: In vitro studies on mouse oocyte activation, embryo development competence and sperm oxidation-reduction potential. Andrologia. 2018;50:e12943. doi: 10.1111/and.12943. [DOI] [PubMed] [Google Scholar]
- 204.Braga D.P., Setti A.S., Figueira R.C., Iaconelli A., Jr., Borges E., Jr. The negative influence of sperm cryopreservation on the quality and development of the embryo depends on the morphology of the oocyte. Andrology. 2015;3:723–728. doi: 10.1111/andr.12049. [DOI] [PubMed] [Google Scholar]
- 205.Yildiz C., Ottaviani P., Law N., Ayearst R., Liu L., McKerlie C. Effects of cryopreservation on sperm quality, nuclear DNA integrity, in vitro fertilization, and in vitro embryo development in the mouse. Reproduction. 2007;133:585–595. doi: 10.1530/REP-06-0256. [DOI] [PubMed] [Google Scholar]
- 206.Oikawa T., Itahashi T., Yajima R., Numabe T. Glutathione treatment of Japanese Black bull sperm prior to intracytoplasmic sperm injection promotes embryo development. J. Reprod. Dev. 2018;64:303–309. doi: 10.1262/jrd.2018-023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Balao da Silva C.M., Ortega-Ferrusola C., Morrell J.M., Rodriguez Martínez H., Peña F.J. Flow cytometric chromosomal sex sorting of stallion spermatozoa induces oxidative stress on mitochondria and genomic DNA. Reprod. Domest. Anim. 2016;51:18–25. doi: 10.1111/rda.12640. [DOI] [PubMed] [Google Scholar]
- 208.Steele H., Makri D., Maalouf W.E., Reese S., Kölle S. Bovine sperm sexing alters sperm morphokinetics and subsequent early embryonic development. Sci. Rep. 2020;10:6255. doi: 10.1038/s41598-020-63077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Zhang P.P., Wang J.J., Li C.Y., Hao H.S., Wang H.Y., Du W.H., Pang Y.W., Zhao S.J., Zou H.Y., Hao T., et al. Protective effect of vitamin C and lycopene on the in vitro fertilization capacity of sex-sorted bull sperm by inhibiting the oxidative stress. Reprod. Domest. Anim. 2020;55:1103–1114. doi: 10.1111/rda.13748. [DOI] [PubMed] [Google Scholar]