Heng-Wen Chou, MD, and Shu-Chien Huang, MD, PhD
Central Message.
Aortic blood flow is an interplay of ECMO cannula position, ECMO, and native left ventricular function during VA ECMO support.
See Article page 85.
Over the past few years, the adult cardiac extracorporeal membrane oxygenation (ECMO) support has risen rapidly.1 Venoarterial (VA) ECMO support can rescue patients with acute cardiogenic shock, including postoperative cardiac failure.2 Cannulation for VA-ECMO is not difficult for cardiac surgeons; however, the consideration is not the same as traditional cardiopulmonary bypass with full heparinization and cardiac arrest.
In this issue of the Journal, Fukunaga and colleagues3 describe a case with descending aortic thrombosis and acute type B dissection during central ECMO. In this case, the EPOA aortic cannula was inserted to descending aorta, and the aortic dissection and thrombus were disclosed by transesophageal echocardiography.
Although the definite cause of aortic dissection is not clear, the combination of intra-aortic balloon pump (IABP) and aortic cannula in the descending aorta carries the high risk of aortic injury. When the balloon inflates, the cannula is pushed against the aortic wall. If the high-pressure blood flow from VA ECMO cannula was directed to the aortic wall, the combination of direct injury and blood flow injury might be the cause of aortic dissection.
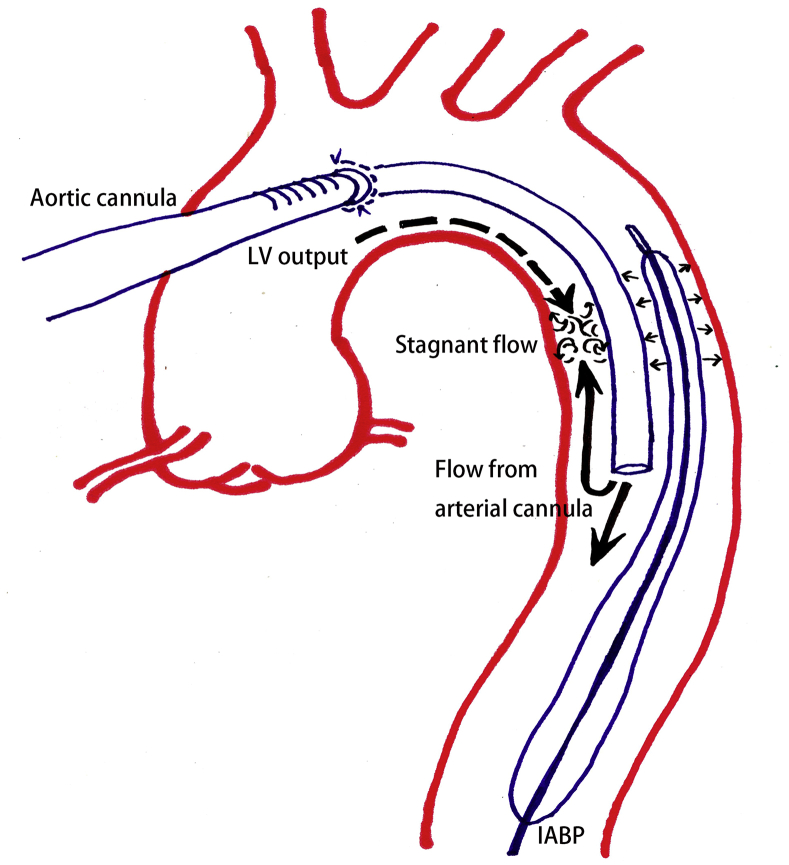
The thrombus formation in the proximal descending aorta is also likely related to the position of aortic cannula (Figure 1). The North/South syndrome, or blue-head syndrome, is characterized as upper-body cyanosis (cerebral hypoxia) while patients are on femoral VA-ECMO.2 The blood flow pattern in the aorta is a combination effect of native left ventricular output and the blood flow from arterial cannula in VA ECMO. The unloading procedure (pulmonary vein venting) could avoid pulmonary edema but could also decrease native left ventricular outflow. The blood flow stagnation could happen at the “perfusion border,” especially if the pulsation is low. Thrombus formation will occur because the patient is not full heparinized. Thus, VA ECMO is easy to implant, but the cannula position, the management of native left ventricular output (preload, afterload, inotropic agents), the presence of IABP, and left ventricular decompression procedures all require careful consideration of their individual and combined effects. Once the patient is placed on mechanical support, careful monitoring and thoughtful consideration of the blood flow pattern are the key to avoiding complications.
Figure 1.
In the case with aortic cannula and IABP in descending aorta, the mechanical trauma and blood flow stagnation resulted in complications. LV, Left ventricular; IABP, intra-aortic balloon pump.
In summary, this is a case demonstrating the serious effect of inappropriate aortic cannula during ECMO + IABP support. The combined effect of mechanical circulatory devices and left ventricular performance is a cardinal consideration in managing patients with cardiogenic shock.
Footnotes
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
References
- 1.Guglin M., Zucker M.J., Bazan V.M., Bozkurt B., El Banayosy A., Estep J.D., et al. Venoarterial ECMO for adults: JACC scientific expert panel. J Am Coll Cardiol. 2019;73:698–716. doi: 10.1016/j.jacc.2018.11.038. [DOI] [PubMed] [Google Scholar]
- 2.Rao P., Khalpey Z., Smith R., Burkhoff D., Kociol R.D. Venoarterial extracorporeal membrane oxygenation for cardiogenic shock and cardiac arrest. Circ Heart Fail. 2018;11:e004905. doi: 10.1161/CIRCHEARTFAILURE.118.004905. [DOI] [PubMed] [Google Scholar]
- 3.Fukunaga N., Badiwala M.V., Yau T.M., Rao V., Cusimano R.J. Descending aortic thrombosis and acute type B dissection during central extracorporeal membrane oxygenation: a word of caution. J Thorac Cardiovasc Surg Tech. 2021;6:85–87. doi: 10.1016/j.xjtc.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]