Highlights
-
•
Racial or ethnic health care disparities in cardio-oncology are present, although data remain sparse.
-
•
These disparities stem from structural racism, higher prevalence of CVD risk factors, and reduced access to specialty care.
-
•
A multidisciplinary approach is required to dismantle these disparities and should include key stakeholders, including health care policy makers, patients, scientists, and clinicians.
Key Words: cardio-oncology, cardiotoxicity, disparities, ethnicity, race, structural racism
Abbreviations and Acronyms: HER2, human epidermal growth factor receptor 2; NHW, non-Hispanic White
The field of oncology has seen dramatic advances over the past 25 years, although frequently at the cost of short- and long-term cardiovascular complications of therapy. The populations at risk for these adverse outcomes fall at the intersection of the long-standing disparities stemming from structural racism affecting outcomes in the fields of cardiology and oncology. The current coronavirus disease-2019 pandemic has further amplified the impact of disparities on historically marginalized populations, thus reinforcing the need to identify and address this inequity. This primer aims to shed insight on how racial or ethnic disparities may be magnified in the field of cardio-oncology and propose potential approaches to address these issues.
Disparities in Cardiology and Oncology
Racial or ethnic disparities in CVD morbidity and mortality have persisted in the United States, despite recent advances in early diagnosis, risk factor management, and drug development. Structural racism, defined as legitimization of systems and dynamics that routinely disadvantage historically marginalized groups, is a fundamental driver of these existing disparities (1). The downstream effects of structural racism are a higher prevalence of CVD risk factors and decreased access to high-quality health care that in turn lead to disparities. Notably, Black individuals have worse cardiovascular health and significantly higher rates of fatal CAD compared with their non-Hispanic White (NHW) counterparts (2). The prevalence of CVD risk factors such as hypertension, diabetes, and obesity is higher in Black individuals compared with NHW individuals (2), and these risk factors increase cardiotoxicity risk. When studied in aggregate, although Hispanic individuals have lower rates of CVD mortality, similar disparities and care gaps are noted, including a high prevalence of cardiometabolic risk factors. For example, Puerto Ricans and Mexican individuals have more than twice the prevalence of diabetes mellitus compared with NHWs (3). According to recent estimates, up to 81% of Mexican American men and 78% of Mexican American women are either obese or overweight (3). The disparities seen in CVD risk factors are at least in part the result of factors that are sequalae of oppressive systems that exist in society, such as lower household income and food insecurity, lack of medical literacy, lack of insurance, inability to gain access to health care providers, among others. These racial and ethnic disparities in CVD and CVD risk factors likely contribute to inequities seen in cardiotoxicity from cancer therapies.
In oncology, cancer incidence and mortality are generally highest among Black individuals compared with other races (4). Additionally, although CVD is the leading cause of death in non-Hispanic groups, cancer was the leading cause of death for Hispanic individuals, accounting for 21% of deaths in adult Hispanic individuals in 2016 (4). Hispanic individuals receive diagnoses at more advanced stages of breast and colorectal cancer compared with NHWs (4). These differences stem from structural factors such as lower educational attainment, decreased financial security, lack of health insurance, and less access to high-quality health care, thus leading to lower rates of preventive health services such as cancer screening and a greater prevalence of cancer risk factors such as obesity and smoking. Another contributing factor to disparities in oncology is the differential use of therapies. For example, Black patients are less likely to receive surgical resection and appropriate adjuvant therapy compared with NHWs (5). Supporting the role of treatment inequities in cancer-specific survival disparities, studies in which Black and NHW patients receive identical cancer treatment have not found differences in outcomes (5). This finding highlights the critical role of structural racism and social determinants of health as key factors to address in closing care gaps and improving outcomes across diverse populations in cardiology and oncology.
Disparities in Cardio-Oncology
Limited studies show that patients from historically marginalized racial or ethnic backgrounds experience a higher incidence of cardiotoxicity from oncologic therapies. Anthracyclines are the most studied chemotherapeutic agents associated with myocardial injury. In 2004, a retrospective study of 100 Black patients treated with doxorubicin found that these patients had a 3-fold higher risk of cardiotoxicity compared with non-Black patients in previously described cohorts (6). Trastuzumab, a monoclonal antibody against human epidermal growth factor receptor 2 (HER2), and other HER2-targeted therapies, are associated with cardiotoxicity in up to 17% of patients. A study of 216 patients with breast cancer showed that even after controlling for baseline cardiovascular risk factors, Black women were more than 2-fold more likely to develop cardiotoxicity from trastuzumab use and had a much higher likelihood of not completing therapy compared with NHW women (7). Whether treatment interruption is related to worse overall survival for Black patients with breast cancer is unclear.
Limited data also suggest increased rates of adverse cardiovascular outcomes among Black vs NHW patients with cancer. According to a U.S. national registry database of patients with cancer, Black women with breast cancer were at a 25% greater risk of cardiovascular death compared with NHW women (8). Although cardiotoxicity risk factors such as pre-existing heart failure, hypertension, and diabetes are more prevalent in Black individuals and therefore undoubtedly contribute to risk, how these factors, as well as other potential contributors (eg, social determinants of health), lead to these disparate outcomes remains largely unknown.
Contributors to Disparities
Beyond a differential prevalence of underlying CVD and CVD risk factors and more advanced cancer at presentation, historically marginalized racial or ethnic individuals also face unique challenges that contribute to disparities in the emerging field of cardio-oncology.
Socioeconomic factors and structural racism
Underscoring many of the disparities in health care is the pervasive structural racism in our society. Structural racism, commonly interchanged with systemic or societal racism, promotes inequitable systems that affect adverse health outcomes. Racial and socioeconomic disparities in health care have been shown to contribute to adverse health outcomes. Because of long-standing structural barriers resulting in lower rates of health care access, insurance, and health literacy, Black and Hispanic patients are less likely to engage in routine preventive care (9). Higher rates of unemployment and lower median household incomes in Black and Hispanic individuals compared with NHW individuals that result from structural racism likely affect access to timely and high-quality health care.
Lack of diversity in clinical trials
Without diverse participants, it is difficult to generalize the results of practice-informing clinical trials to different populations. For instance, a recent study examined the representation of Black Americans in 75 leading cancer drug trials from 2014 to 2018 that led to approval by the U.S. Food and Drug Administration. This report noted that the participation-to-prevalence ratio for Black Americans in these trials was 0.31, whereas a participation-to-prevalence ratio of 1 would indicate perfect representation between the drug participants and the disease population (10). Cultural and language incompatibility issues can also influence patient participation. Lack of appropriate communication can compromise informed consent and may affect clinical trial participation. In addition to the lack of racially or ethnically diverse representation, most cardiotoxicity studies do not report data on race or ethnicity, thereby making the true prevalence of cardiotoxicity in different populations unknown.
Patients who are at the highest risk of being affected by these disparities usually live in areas with limited access to large quaternary centers where most cardio-oncology programs currently exist. This lack of specialty care may be a significant contributor to the disparities seen in cardiotoxicity outcomes. Thus, efforts to increase and optimize access to cardio-oncology care (eg, virtual care) are warranted. Additionally, there is a lack of centralized resources, such as guidelines or practice updates for cardio-oncology focused on monitoring and treatments. Given that the field of cardio-oncology is rapidly changing with new cancer therapies, there is a critical need to centralize resources, expand dedicated training, and standardize care to bridge existing practice gaps.
Call to Action
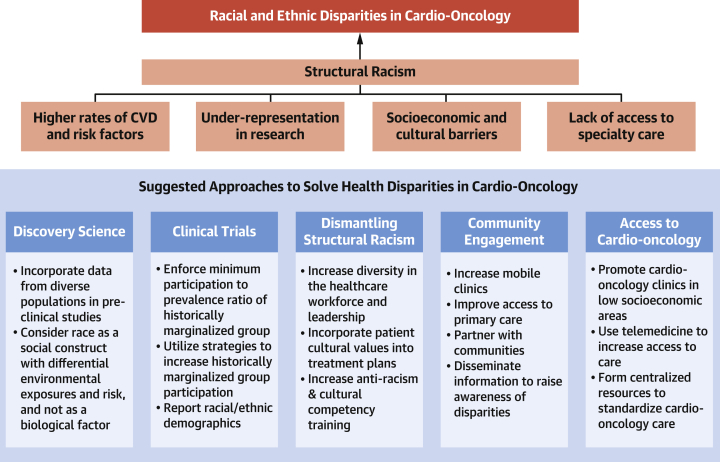
Addressing racial or ethnic disparities in the field of cardio-oncology will require a multifaceted approach with all stakeholders (Figure 1). First, dismantling structural racism should be a priority for all efforts to mitigate disparities. Second, more research is needed to understand more clearly how cardiotoxicity differs by race or ethnicity and by social factors. Currently, most trials do not publish comprehensive racial or ethnic demographic data that could be used to quantify and monitor treatment gaps more accurately. Mandated inclusion of historically marginalized populations in clinical trials by regulatory bodies and funding agencies would make a substantive difference. Understanding and designing interventions that address unique challenges to participation in both research and clinical care, such as language barriers or limited geographic representation of cardio-oncology practices, are critical. Burgeoning racial or ethnic disparities in cardio-oncology stem from long-standing disparities in health care more broadly. Interventions designed to mitigate these disparities must consider social and structural determinants of health and use innovative approaches to increase access to both preventive and specialty care.
Figure 1.
Contributors to Racial and Ethnic Disparities in Cardio-Oncology and Proposed Solutions
Major contributors to racial and ethnic disparities in the field of cardio-oncology and proposed solutions focusing on discovery science, clinical trials, community engagement, dismantling structural racism, and increasing access to specialty care. CVD = cardiovascular disease.
In conclusion, although cardio-oncology is a relatively new field, racial or ethnic disparities are pervasive. An intentional and multidisciplinary approach is required to address both the underlying clinical and social determinants that contribute to the disparity.
Funding Support and Author Disclosures
This work is supported by National Institutes of Health and the American Heart Association Robert Wood Johnson Harold Amos Medical Faculty Development Program and Career Development Award. Dr Rhee has reported receiving funding for this work from National Institutes of Health grant K08 HL148540 and the American Heart Association Career Development Award. Dr Witteles has received consulting fees from Pfizer, Alnylam, Eidos, and Ionis/Akcea unrelated to this work. Dr Rodriguez has reported receiving funding for this work from National Institutes of Health grant K01 HL 144607 and the American Heart Association Robert Wood Johnson Harold Amos Medical Faculty Development Program; and has received consulting fees from Novartis, Janssen, NovoNordisk, and HealthPals unrelated to this work. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
Clyde W. Yancy, MD, served as Guest Editor for this paper. Anju Nohria, MD, served as Guest Editor-in-Chief for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Churchwell K., Elkind M.S.V., Benjamin R.M. American Heart Association. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020;142:e454–e468. doi: 10.1161/CIR.0000000000000936. [DOI] [PubMed] [Google Scholar]
- 2.Carnethon M.R., Pu J., Howard G. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136:e393–e423. doi: 10.1161/CIR.0000000000000534. [DOI] [PubMed] [Google Scholar]
- 3.Swenson C.J., Trepka M.J., Rewers M.J. Cardiovascular disease mortality in Hispanics and non-Hispanic whites. Am J Epidemiol. 2002;156:919–928. doi: 10.1093/aje/kwf140. [DOI] [PubMed] [Google Scholar]
- 4.Cancer facts & figures for Hispanics/Latinos 2018–2020. American Cancer Society. https://www.cancer.org/research/cancer-facts-statistics/hispanics-latinos-facts-figures.html Available at:
- 5.Morris A., Rhoads K.F., Stain S.C. Understanding racial disparities in cancer treatment and outcomes. J Am Coll Surg. 2010;211:105–113. doi: 10.1016/j.jamcollsurg.2010.02.051. [DOI] [PubMed] [Google Scholar]
- 6.Hasan S., Dinh K., Lombardo F. Doxorubicin cardiotoxicity in African Americans. J Natl Med Assoc. 2004;96:196–199. [PMC free article] [PubMed] [Google Scholar]
- 7.Litvak A., Batukbhai B., Russell S.D. Racial disparities in the rate of cardiotoxicity of HER2-targeted therapies among women with early breast cancer. Cancer. 2018;124:1904–1911. doi: 10.1002/cncr.31260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sengupta R., Honey K. AACR cancer disparities progress report 2020: achieving the bold vision of health equity for racial and ethnic minorities and other underserved populations. Cancer Epidemiol Biomarkers Prev. 2020;29:1843. doi: 10.1158/1055-9965.EPI-20-0269. [DOI] [PubMed] [Google Scholar]
- 9.Mochari-Greenberger H., Mills T., Simpson S.L., Mosca L. Knowledge, preventive action, and barriers to cardiovascular disease prevention by race and ethnicity in women: an American Heart Association national survey. J Womens Health (Larchmt) 2010;19:1243–1249. doi: 10.1089/jwh.2009.1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al Hadidi S., Mims M., Miller-Chism C.N., Kamble R. Participation of African American persons in clinical trials supporting U.S. Food and Drug Administration approval of cancer drugs. Ann Intern Med. 2020;173:320–322. doi: 10.7326/M20-0410. [DOI] [PMC free article] [PubMed] [Google Scholar]