Abstract
Recently, research has reported that the rates of suicide among Black children between the ages of 5 to 12-years-old are increasing as they are now more likely to commit suicide than White children. Yet, there are very few, if any, frameworks being used by researchers to explain the risks of suicide among Black children. Suicide research has overwhelmingly been focused on White youth thus leaving a critical gap in suicide research. This conceptual paper provides an integrated framework using the Interpersonal-Psychological Theory of Suicide and Intersectionality theory, as a guide for researchers, clinicians, and practitioners to incorporate culturally appropriate techniques in their work as a way to prevent suicide among Black children. This framework highlights racial discrimination, mental health, socioeconomic status, and sexual/gender minority status to be the most preeminent, yet understudied factors leading to suicide risk among Black children in the United States.
Keywords: suicide, Black children, mental health, racial discrimination
Introduction
Death by suicide is a serious public health issue for children in the United States. Among Black children under 12 years of age, there has been a statistically significant increase in death by suicide and suicidal ideation in recent years (Bridge et al., 2018; Lindsey et al., 2019). As a result, in the last decade, suicide has increased from the third to the second leading cause of death in adolescents 11 to 18-years-old (Curtin & Heron, 2019). Although suicide researchers have historically examined suicidal ideation among White children, researchers and clinicians may be unaware of the potential risk factors of suicide for Black children. Due to these disparities in research and practice, Black children continue to be at heightened risk of dying by suicide without interventions being developed and tested with the proper cultural considerations for this group.
The current article provides a review on risk factors that may lead to death by suicide among Black children. Using a well-established framework for suicidal thoughts and behaviors, we incorporate a broader intersectional context to attempt to explain suicidal behavior among Black children in the United States. This article aims to provide one of the first integrated conceptual theoretical frameworks for researchers and clinicians studying suicide among Black children using the Interpersonal-Psychological Theory of Suicide and Internationality Theory. Due to the complex nature of this phenomena, this manuscript provides innovative and race-specific implications for researchers, clinicians, and policy makers to reducing suicidal thoughts, behaviors, and overall death by suicide among Black children.
Risk Factors
Understanding the sudden rising rates of suicide among Black children has been difficult to conceptualize for suicide and mental health researchers. However, the few studies that have acknowledged the recent trend, have consistently provided support for acknowledging mental health outcomes as being the top risk factor for suicide ideation, suicidal behavior, and death by suicide among Black children (Bridge et al., 2018; Lindsey et al., 2019; Switzer, 2019). As Black children have a unique social location in U.S. society, it is important to examine this phenomenon by centering specific risk factors through a racial context. The complexity of childhood and adolescence including identity formation and vulnerability to risk-taking can exacerbate the likelihood of experiencing poor mental health outcomes to an already marginalized group. Therefore, we highlight in this article four important factors that may explain the recent rise of suicidal behaviors among Black children: (1) Mental Health; (2) Socioeconomic Status; (3) Racism and discrimination; and (4) Sexual and Gender Minority Status. It is important to note that we acknowledge that the risk factors mentioned are not exhaustive of other potential stressors that can increase suicide ideation and behaviors among Black children. However, we posit that these risk factors should be further explored.
Mental health.
Difficulties managing mental health has been consistently shown to contribute to suicidal thoughts and behaviors (Brailovskaia et al., 2018; Phillips, 2010). Black children who are living with a mental health disorder, are often less likely to have a mental health condition officially diagnosed, perhaps due to access issues (Lê Cook et al., 2013). Despite the need for effective mental health treatment for Black children, access to mental health services are limited as these services are often inaccessible or unavailable in neighborhoods where Black children are most likely to reside in (Barksdale et al., 2010; Murry et al., 2011).
Mental health stigma and medical mistrust within the Black community may further contribute to disparities in mental health among Black children. The patient/provider relationship can be negatively impacted by perceived racism and discrimination, which in turn can affect the decisions that Black children and their families make regarding their health. Information about unethical medical experiments such as the Tuskegee syphilis study has been passed down through multiple generations of African American families in the United States and contribute to beliefs and mistrust of the healthcare system (Amutah-Onukagha et al., 2018). Due to this mistrust, Black children may be encouraged to seek help from family members or taught to pray for solutions to their mental health issues rather than going to a trained mental health professional (Lindsey et al., 2013). As children have limited mobility to their age and are less autonomous than adults, the decision to seek mental health services often resides in parents/guardians and educators within the child’s life (Opara et al., 2019).
In addition to researchers and practitioners exploring ways to reduce disparities in mental health through increasing access on the organizational level (e.g., offering bus passes to caregivers with transportation barriers and childcare to parents of multiple children) and reducing stigma and mistrust on the individual level (e.g., through discussing issues of confidentiality and privacy with parents) to ensure treatment attendance and engagement. Particularly for youth whom live in under-resourced neighborhoods where mental health clinics are scarce. Schools with high-minority populations, are less likely to have mental health clinicians available for students due to budget cuts, high student populations, and being overworked (Farahmand et al., 2011). Therefore, an important and significant gap in mental health services within schools and under-resource neighborhoods where Black children reside may have a devastating impact on suicidal behavior among Black children.
Neighborhood context and socioeconomic status.
In the United States, race has been found to be a predictor of socioeconomic status (Respress et al., 2018). Among socioeconomic status, there is significant variation in economic levels between Blacks and Whites. Relative to Whites, Blacks are disproportionately overrepresented in the lowest socioeconomic status categories (Miller & Taylor, 2012). U.S. Census data reveals that Blacks are less likely than Whites to graduate from high school or college, have lower average annual incomes, and lower median net worth than Whites (U.S. Census, 2018). As a result, these differences in socioeconomic status likely predispose Black children whose families belong to lower socioeconomic levels, to experience excessive hardships that leave them at greater risk for poorer mental health symptoms such as depression and anxiety than Whites.
In addition to poverty, research suggests that Black children residing in urban, under-resourced low-income environments often experience a greater risk of mental illness due to increased exposure to community violence, gang activity, and drug use (Cullins et al., 2019; Hastings & Snowden, 2019). Specifically, for Black children, early and late adolescents, exposure to violence has been linked to greater post-traumatic stress disorder (PTSD) and depressive symptoms (Davis & Stevenson, 2006). Racially segregated and under-resourced neighborhoods are often outcomes of systemic and structural racism resulting in poor educational outcomes for students, high unemployment rates, crime, violence, and inadequate housing whom reside in such neighborhoods (Miller & Taylor, 2012). Due to this inequity, feelings of hopelessness, despair, and internalized anger among children can become normalized in such communities and lead to feelings of anger and depression (Pinderhughes et al., 2015). Research has shown that depression among Black children is often “masked” as anger resulting in aggressive behaviors that can lead to suspension and expulsion in schools and out-of-school settings (Assari et al., 2018; Mallet, 2016). Masked anger reveals a deeper layer of identifying depression in Black children because symptoms that are typically associated with depression in children from other racial backgrounds are not as easily identifiable in Black children (McLaughlin et al., 2007). Black children’s behaviors and symptoms may be perceived as irritability and aggression as opposed to sadness and decreased energy when dealing with depressive symptoms, paranoia, or anxiety (Clarke & Mosleh, 2015). Such findings indicate that clinicians may not be aware of how to accurately assess for and identify symptoms of depression and anxiety in Black children whose symptoms may manifest differently. Thus, missing a crucial opportunity to intervene.
Perceived racism and discrimination.
In addition to being misdiagnosed, there are culturally specific factors that contribute to depressive symptomology and other mental illnesses for Black children in the United States. One significant factor contributing to the onset of depressive symptoms and suicide is the experience of racial discrimination (Lanier et al., 2017; Seaton et al., 2010). Racial discrimination is the process of excluding, or discriminating against a group or individual based on their race in an unfair manner. English et al. (2014) found that racial discrimination was associated with participation in delinquency and suicide ideation among Black children. Lambert et al. (2009) examined mental health symptoms its association with racism and discrimination and found that Black children who are exposed to racism and discrimination both at the individual level and community level have higher rates of depressive symptoms compared to other racial and ethnic groups. Socioeconomic status and gender differences may be present in the relationship between racial discrimination, mental health symptoms, and suicide ideation. Chambers and Erausquin (2018) found that Black youth from lower socioeconomic statuses were more likely to report higher levels of racial discrimination and exhibit low levels of academic self-concept. Another study, found similar results, indicating that Black male middle school students experienced racial discrimination and higher suicidal ideation than Black female students although Black female middle childhood students had higher rates of depressive symptoms in the study (Lambert et al., 2009).
There is emerging evidence that shows the association between racial discrimination, stress and trauma which results in poor mental health outcomes among Black youth (Hope et al., 2015; Keels et al., 2017; Metzger et al., 2017, 2018). Even more alarming are the effects of racial discrimination on the arousal system which can negatively impact stress regulation systems (Berger & Sarnyai, 2015). This finding reveals that traumatic stress through racial discrimination may be a pathway for increased risk for psychopathology, including suicidal behavior (Polanco-Roman et al., 2019). Race-related trauma stress has been conceptualized in the literature to be one of the leading causes for mental health symptoms among Black youth (Henderson et al., 2019). Black children experience higher levels of discrimination and violence from their teachers and peers when compared to other racial groups (Respress et al., 2018). Within the school context, school officials such as resource officers and security guards have been found to exert more force against Black children and arrest them at higher rates—contributing significantly to the school to prison pipeline theory (Mallett, 2017; Merkwae, 2015). Even among interactions that are not overt such as micro-aggression, Black children tend to encounter numerous subtle racial microaggressions in school settings leaving them to have elevated levels of psychological distress and poor mental health outcomes (Baker, 2017). These occurrences can have a profound effect on Black youth across the lifespan as well. Keels et al. (2017) found in their longitudinal study that among Black youth whom experienced microaggressions in high school, continue to experience greater depressive symptoms at the start of college. More recently, Henderson et al. (2020) found in their phenomenological examination of racial discrimination among Black youth, that participants experienced multiple occurrences of subtle assaults, microaggressions, and racial slights while in school. Participants in the study also admitted to exhibiting feelings of anger, sadness, and depressive symptoms due to the racial discrimination.
Very limited research has focused on racism and discrimination and its association with suicide ideation solely among Black children. One of the few studies to examine the relationship between racial/ethnic discrimination and suicidal behavior among Black youth found a significant association across both boys and girls (Assari et al., 2018). Further, Gunn et al. (in preparation) explored the role of self-worth, social support, and racial discrimination in the development of suicidal thoughts across two waves of data from the Maryland Adolescent Development in Context Study (MADICS). Findings indicated an interactive effect between self-worth and perceptions of racial discrimination wherein suicidal thoughts were elevated among Black youth (specifically boys) who perceived racial discrimination as high while also having high self-worth, indicating, perhaps, that they were aware of their worth but understood that they would be discriminated against regardless. Due to the extant literature on racial discrimination and mental health among Black children, it is essential that researchers begin to further explore prevention strategies that can buffer the effects of racial discrimination among children.
Sexual and gender minority status.
Another risk factor that has been underexplored in research sexual orientation and gender identity among Black youth. Lesbian, gay, bisexual, transgender, and queer youth (LGBTQ) are twice as likely to report suicidal ideation and to attempt suicide than their heterosexual counterparts (Gomez et al., 2011; Grossman & D’Augelli, 2007; King et al., 2008; Stone et al., 2014). Many of these studies of LGBTQ youth can say little about why these rates are higher. However, other smaller studies have demonstrated that multiple factors including increased internalized homophobia and increased religious context of upbringing (Gibbs & Goldbach, 2015), increased rates of victimization (bullying and sexual abuse), and increased rates of depression (Lardier et al., 2017; Mereish et al., 2013), higher levels of perceived discrimination (Huebner et al., 2014) and gender nonconformity—all contribute to increased rates of suicide among LGBTQ youth (Mustanski & Liu, 2013). In addition to lack of interpersonal and social supports that LGBTQ youth may lack, those living in under-resourced environments and of lower socioeconomic background may experience more hardships, exposure to violence, added level of racial discrimination, and poverty related conditions. Furthermore, patterns of suicide and suicidal thoughts are even higher among LGBTQ youth of color living in an urban setting (Lardier et al., 2017). Few studies that have solely examined differences between Black LGBTQ youth and White LGBTQ youth found that Black LGBTQ youth were at elevated risk for death by suicide and suicidal thoughts compared to their counterparts and White LGBTQ youth (Cochran et al., 2007; Meyer et al., 2008). The intersection of multiple marginalized identities (e.g., sexual/gender minority and ethnic/racial minority) can increase an individual’s likelihood of experiencing discrimination and the resulting psychological consequences (Sutter & Perrin, 2016). In addition to experiencing racism and microaggressions outside of the LGBTQ community, LGBTQ racial minorities may experience racism in relationships and social networks within the LGBTQ community.
Within the Black community, Black children whom identify as LGBTQ may not feel supported or comfortable is discussing their identities which may lead to even further marginalization, rejection, and discrimination within their community (Chu, Khoury, et al., 2017). The relationship of Black people within the Black community may provide meaningful evidence of pathways to and predictors of suicide ideation and behaviors among Black children. Dawson (1994) hypothesizes that the fate of a Black individual is intuitively linked with the fate of the Black community as a whole. That is, Black individuals who believe their personal fate depends on the sociopolitical destiny of the Black community in the United States may be more inclined to act in ways that politically support the Black community. Given the unique experiences of having multiple marginalized identities (both Black and LGBTQ), questions remain regarding how Black LGBTQ youth connect their own identity both through racial, sexual, and gender identity. Heteronormative actions and behaviors have been believed to be the gold standard within the Black community (McGuire et al., 2017). Given that the early to late adolescent period emphasizes on identity formation and understanding who one is relation to society. This period of exploration can have a profound effect on LGTBQ Black youth leading to isolation within society and Black community together.
Conceptual Framework
Interpersonal-Psychological Theory of Suicide through an Intersectional Framework
We posit that in order for researchers and clinicians, to understand the increasing number of suicides among Black children, we must understand the intersecting factors that may contribute to their risk. As we understand the risks of suicidal thoughts and behaviors, we can then begin to develop effective prevention strategies to protect Black children (e.g., teaching emotional regulation and cognitive restructuring in response to discrimination based on intersecting identities, such as race, gender, class, sexual orientation). Such strategies, we presume, are going to be different from other children based on the multiple domains of marginalized identities that Black children belong to. To accurately discuss the experiences of Black children, it would be a disservice to fail to incorporate a theory that specifically acknowledges the social locations that have placed Black children in America at risk. Within this framework, we have integrated two theories: One that describes how multiple forms of oppression can affect individuals and families, and lead to barriers to forming healthy relationships and producing negative outcomes (Intersectionality theory; Crenshaw, 1991) and another theory that explores the motivating factors that can lead to death by suicide (the Interpersonal-Psychological Theory of Suicide, IPTS).
Researchers often view salient contextual variables such as race, ethnicity, gender, sexual orientation, socioeconomic status/class, education level, and ability as separate sociocultural demographic variables that rarely influence one another. Yet, intersectionality theorists contend that contextual variables intersect and influence one another, resulting in specific and unique outcomes (Crenshaw, 1991). Although intersectionality has been conceptualized in various ways, researchers suggest that an individual’s multiple identities interact and intersect to shape personal experiences (Crenshaw, 1991), and at times form “intersecting oppressions … that work together to produce injustice” (Collins, 2000, p. 18).
One challenge that remains is reconciling current theoretical frameworks of suicidal thoughts and behaviors with our growing understanding of inter-sectionality, particularly as it pertains to LGBTQ youth. Of these frameworks, the IPTS holds a commanding presence within the field of suicidology and has led to a large body of literature (Chu, Buchman-Schmitt, et al., 2017). The IPTS was first proposed by Joiner (2005) and later expanded on by Van Orden and colleagues (2010). According to the IPTS, the motivation for suicide is the result of the co-occurrence of two interpersonal-psychological factors: (1) thwarted belongingness and (2) perceived burdensomeness. Thwarted belongingness is a general sense of disconnect from others and a sense that one does not belong (“No one cares about me,” “I am alone”). It is the deprivation of the need to belong, a vital psychological need of all humans (Van Orden et al., 2010). Perceived burdensomeness refers to perceptions that you are a detriment to those around you or you are a liability (“Others would be better off without me” “I am a burden”). When both are present, according to the IPTS, the motivation to die by suicide is present.
To understand the transition from suicidal thoughts/desire to actual behavior the IPTS introduces a third concept: the acquired capability for suicide. The acquired capability for suicide refers to the difficulty inherent in suicidal behavior. Suicide often involves violent, painful methods that require a person to face the fear of pain and death. According to the IPTS, only those who have acquired the capability for suicide have the knowhow to engage in behavior likely to lead to death. As an example of this, males are posited to have higher acquired capability due to their engagement in more violent behavior and therefore they are more likely to die by suicide (in the US, males die at a ratio of 3.5:1, Drapeau & McIntosh, 2018). Van Orden and colleagues (2010) expanded on the original framework of Joiner (2005) by incorporating into the model a longstanding risk factor for suicide: hopelessness. Hopelessness has a long history in suicidology, first proposed by Beck and colleagues as part of their cognitive model for suicidal behavior (Beck, Brown, & Steer, 1989). Hopelessness involves a pessimistic and often bleak outlook on current and future circumstances (“Things will not get better”).
Generally, research has found support for the IPTS (Chu, Buchman-Schmitt et al., 2017) though the strength of this support has been challenged as well (Ma et al., 2016). What is clear, however, is that the majority of the research exploring the IPTS focuses on White, non-Hispanic participants. Of the 143 samples utilized in the meta-analysis by Chu, Khoury et al. (2017), over 63% of the participants were White, non-Hispanic. This is partly driven by the use of cross-sectional convenience samples but may also be a byproduct of the central focus of much of suicidology. Recent work has criticized modern theories of suicide for their focus on individual psychology and the dismissal of many factors that influence suicide externally as opposed to internally (Standley, 2020; Hjelmeland & Knizek, 2020; Abrutyn & Mueller, 2019). Abrutyn and Mueller (2019) called for a shift in focus to include sociological and cultural factors into the study of suicidal behavior while Standley (2020) argued for more focus on intersectionality and socioecological approaches to understanding suicide. Hjelmeland and Knizek (2020) more directly criticized the focus of the IPTS on “three internal/psychological factors only” thereby reducing suicide to simplistic rather than more accurately complex explanations (Hjelmeland & Knizek, 2020, p. 168). The goal of this paper is to build on these recent criticisms by situating the IPTS’s internal risk factors within a broader intersectional and non-psychological focus. This may very well enable just the type of shift needed as well as shed much needed light on the development of suicidal thoughts and behaviors among Black children. In order to do this, we conceptualize the role of the various risk factors discussed thus far using a bioecological model (Bronfenbrenner & Morris, 2006) that takes into account characteristics of the individual (such as those proposed by the IPTS) as well as factors from a number of interacting systems.
Figure 1 attempts to highlight how this might be done. While the majority of work in mainstream suicidology focuses on the individual level (e.g., feelings/cognitions relevant to suicidal thoughts and behaviors such as thwarted belongingness or perceived burdensomeness)—this model places the individual characteristics associated with suicide within a broader context. Black children experiencing suicidal thoughts and behaviors may very well be experiencing the psychological characteristics outlined by the IPTS model—but they are doing so within a broader system. Black children who experience suicidal thoughts have possibly not only experienced perceptions of burdensomeness or lack of belonging but may have experienced racial discrimination within their immediate environment and within the broader culture. Each of these systems in turn interact with one another. Black children’s feelings of hopelessness, thwarted belongingness, or perceived burdensomeness do not exist within a vacuum. Such feelings can be amplified by factors in their immediate environments such as living in poverty, being abused, sexism or racism, or community level risk factors such as exposure to community violence, excessive punishment within school settings and drug abuse at the broadest scale. Black children whom lack a sense of belonging or social support may find it more difficult to feel empowered or resilient especially when societal shifts (such as the amplification of anti-Black voices by those in power) occur that negatively impact both the individual child and their communities and environments. In addition, lack of adult allies within this context may contribute to Black children’s low sense of worth and inability to nurture resilience among youth (Opara et al., 2020). A final example of how this can be amplified by belonging to intersecting identities is the increased risk of suicide among LGBTQ Black youth (Bostwick et al., 2014; Kann et al., 2018; Settler & Katz, 2017). While LGBTQ Black youth report similar levels of depressed mood and suicidality compared to LGBTQ youth overall, they are significantly less likely to receive professional care—which may be influenced by a number of factors unique to Black youth discussed above (such as stigma, mistrust, and lack of resources within a community; The Trevor Project, 2020).
Figure 1.
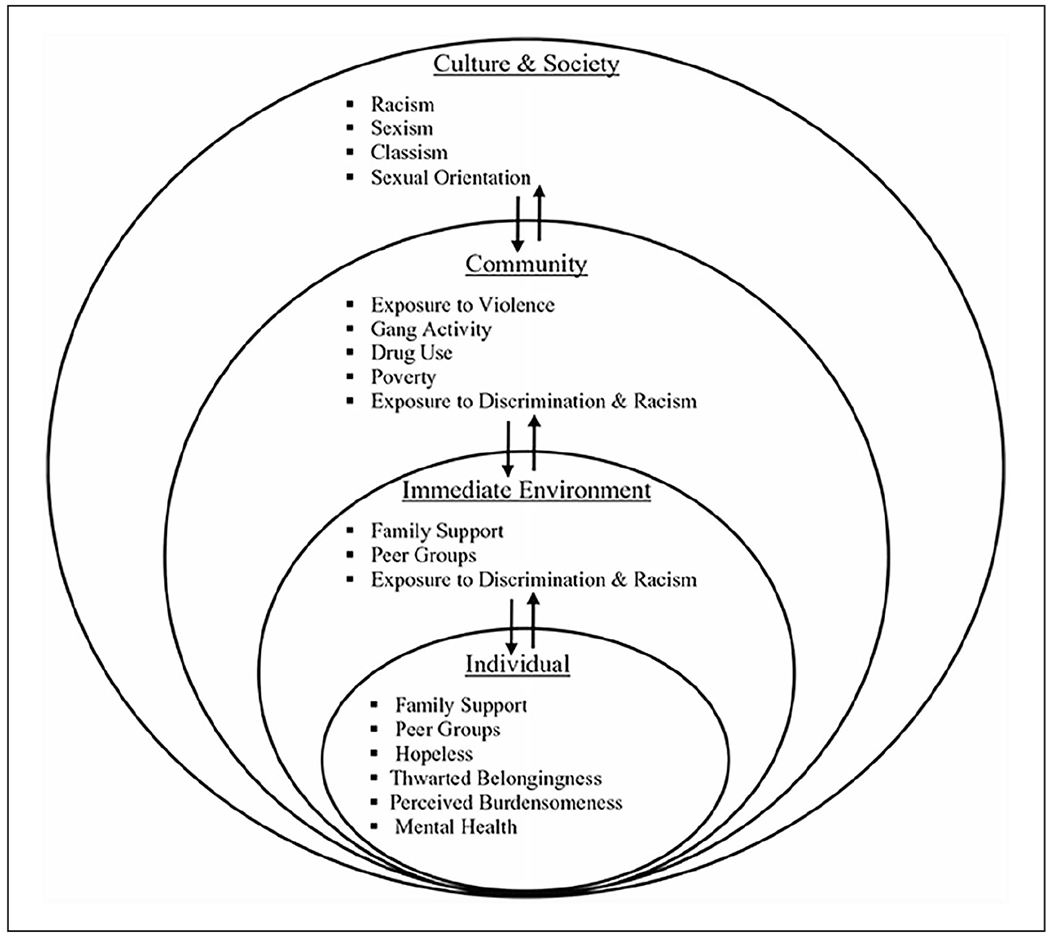
Interpersonal-Psychological Theory of Suicide through an Intersectional Framework.
Implications for Research, Policy, and Practice
Due to the recent attention being placed on the rise of Black children dying by suicide, researchers should seek to center the experiences of Black children using an intersectional lens. Bowleg (2012) posited that the difficulties researchers have in using intersectionality theory is its inability to “test” the theory on a specific population. By nature, the concept of intersectionality subverts its ability to test or measure, as that would assume that categories of identities can be divided and measured. Intersectionality theory allows researchers to understand the importance of viewing populations as having multiplicative identities (socioeconomic status, sexual orientation, gender identity) that contribute to their view of society and their current conditions (Collins, 2000; Opara et al., 2019).
The IPTS calls on clinicians working with suicidal youth to be aware of components that may be seen as significant risk factors for suicidal thoughts and behaviors such as thwarted belongingness, perceived burdensomeness, and hopelessness. The present paper attempts to illustrate how the IPTS can be made more applicable to working with Black children who may be at risk of dying by suicide by focusing on the various levels of influence and intersecting identities. The importance of considering the intersecting effects of multiple risk factors within the context of Black children is consistent with intersectionality theory and recent pushes in the field of suicidology (e.g., Abrutyn & Mueller, 2019) and can be relevant during the assessment and intervention process with Black children in clinical settings. Examples of utilizing IPTS in clinical settings with Black children would include assessing feelings or thoughts around burdensomeness, a lack of belonging and/or social ties, and hopelessness. However, while these should be assessed to aid in identifying those at risk for suicidal thoughts—characteristics of the acquired capability must also be assessed to determine who is at greatest risk for attempting suicide. This can be done by assessing access to means (e.g., firearms in the home or access to firearms within neighborhoods), fearlessness surrounding death, and increased pain tolerance. Within the context of Black children, clinicians should be aware of trauma and abuse, exposure to violence, societal/cultural factors, and resilience as important factors to consider in assessing suicide risk.
Prevention interventions for Black children should target areas where risk factors are more likely to be present and invest in key protective factors that help reduce stigma related to mental health disorders. Researchers and clinicians should understand the inherent mistrust that Black children and families may have with treatment providers. In addition, lack of access to culturally sensitive mental health care clinics in urban communities is an important risk factor that has to be addressed in order to alleviate this issue. Therefore, community-based prevention interventions should be implored for Black children. Specifically, community-based prevention interventions that encourage social support, challenge burdensome feelings through improving sense of worth, and increase racial and gender pride as a strategy to foster sense of belonging to a group and increase their self-worth. In addition, more research should explore gender and LGBTQ specific characteristics of Black children with suicide ideation in order to provide evidence that can be used to develop gender and racial specific interventions for Black children. Research is also needed to explore how risk factors across the various systems (e.g., individual vs immediate environment vs community) interact to influence suicidal thoughts and behaviors among Black children. Some ways this may occur have been discussed early in this manuscript (such as burdensomeness being felt by those experiencing poverty) but must be explored more fully in future research.
Clinicians should understand the impact such risk factors can have on suicide among Black children. There are cultural and gender differences that may seek to increase suicide risk in Black children. Incorporating programs that highlight factors already present within Black families allows individuals from a marginalized background to appreciate the tools they currently possess, thereby empowering youth and families to make effective decisions that impact their view of self in a positive way. Strategies and interventions need to be implemented to help eliminate barriers to seeking mental health services as well as culturally competent mental health providers who can adequately tailor treatment services to the Black experience. More studies addressing cultural competency in the mental health system are needed to combat disparities in mental health treatment among Black children in order to reduce suicide risk.
Lastly, adopting a comprehensive public health framework could aid in the mitigation of risks associated with death by suicide among Black children. The Centers for Disease Control and Prevention (CDC, n.d.) outlined three components that comprise the public health framework: assessment, policy development, and assurance. Assessment refers to the investigation of environmental issues in a community through comprehensive needs assessments and data collection. Policy development refers to developing policies to protect the public’s health and safety. Assurance refers to how polices are enforced, regulated, and evaluated. Researchers and clinicians can play a vital role in ensuring that all components of the framework are adopted and followed in the context of culturally sensitivity. In addition, researchers and clinicians should work collaboratively with federal, state and local policy makers and legislators within a public health framework guided by an IPTS and intersectional model. A multidisciplinary and collaborative approach can inform policies and influence the direction of governmental funds to support the creation of programs and research priorities to address suicide among Black children. More specifically, we advocate for funding mechanisms to be used to provide culturally competent, strengths-based programming to support Black children to be resilient, empowered, and have access to an abundance of resources to address their mental health needs.
Conclusion
Strengths-based and culturally competent frameworks are beginning to emerge as key instruments in social science fields such social work, counseling, and psychology. Practitioners must acknowledge that historically marginalized families should feel valued and applauded for their work in challenging negative narratives and stereotypical beliefs about their groups. As Black families must live in communities that are often segregated and under-resourced, the ability of parents, educators, and adult allies to continue to empower and promote positive sense of self in Black children is crucial in prevention. The incorporation of an intersectional lens in prevention research and clinical practice would allow for more targeted suicide prevention programs. We encourage clinicians to further identify risk factors that may be present in the lives of Black children and begin to target mental health care services to Black children through their environments. Such an approach can be profound in saving the lives of Black children who otherwise may go through the world alone and ignored.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Biographies
Ijeoma Opara is an assistant professor in the School of Welfare at Stony Brook University and Visiting Faculty in the Center for Interdisciplinary Research on AIDS at the Yale School of Public Health. Dr. Opara’s research interests focuses on Black girls, youth empowerment, minority youth substance use and HIV/STI prevention, and Black families.
Maame Araba Assan currently works at the Public Health Management Corporation, a public health non-profit in Philadelphia, focusing on research and evaluation projects related to tobacco control and prevention, asthma, and health equity and healthy living. Her current research interests include HIV/AIDS, infant mortality, and mental illness in communities of color.
Kimberly Pierre received her Master of Public Health degree from Rutgers University with a concentration in Urban Public Health. Kimberly is a sexual risk avoidance specialist. Her areas of research interests include: minority health disparities, women’s health, sexual and reproductive health, and maternal and child health.
John F. Gunn III is a postdoctoral associate at Rutgers University (Newark, NJ) at the NJ Center on Gun Violence Research. Dr. Gunn’s research interests mainly focus on risk and protective factors for suicide across developmental periods, testing theoretical frameworks for suicide, and the impact of media on suicide.
Isha Metzger is an assistant professor of Clinical Psychology at the University of Georgia and Visiting Research Fellow at Yale University. Dr. Metzger is also a Licensed Clinical Psychologist and currently directs The EMPOWER (Engaging Minorities in Prevention, Outreach, Workshops, Evaluation, & Research) Lab, which focuses on disseminating research on preventing risk behaviors and detrimental outcomes among ethnic minority youth.
Jahi Hamilton is pursuing a bachelor’s degree in Psychology at the University of Georgia. Jahi studies the impact sexual orientation and identity has on mental health outcomes such as depression and suicidality.
Eileen Arugu is a social worker with over 5 years of experience working for agencies focused on improving the educational outcomes for urban youth. Eileen earned her MSW from Columbia University School of Social Work with a concentration in mental health. She is passionate about providing quality educational resources for her clients in an effort to close the achievement gap. Presently, Eileen works directly with transitional youth who are involved in the criminal justice system.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abrutyn S, & Mueller AS (2019). Toward a robust science of suicide: Epistemological, theoretical, and methodological considerations in advancing suicidology. Death Studies. 10.1080/07481187.2019.1660081 [DOI] [PubMed] [Google Scholar]
- Amutah-Onukagha N, Mahadevan M, Opara I, Rodriguez M, Trusdell M, & Kelly J (2018). Project THANKS: Examining HIV/AIDS-related barriers and facilitators to care in African American women: A community perspective. AIDS Patient Care and STDs, 32(4), 119–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assari S, Gibbons F, & Simons R (2018). Depression among Black Youth; Interaction of Class and Place. Brain Sciences, 8(6), 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker J (2017). The manifestations of prejudice in everyday life: An examination of racial microaggressions, ethnophaulisms, and integrated threats as observed by white post secondary youth in St. John’s, Newfoundland and Labrador. Memorial University of Newfoundland, St. John’s Newfoundland, and Labrador. [Google Scholar]
- Barksdale CL, Azur M, & Leaf PJ (2010). Differences in mental health service sector utilization among African American and Caucasian youth entering systems of care programs. The Journal of Behavioral Health Services & Research, 37(3), 363–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Brown G, & Steer RA (1989). Prediction of eventual suicide in psychiatric inpatients by clinical ratings of hopelessness. Journal of Consulting and Clinical Psychology, 57(2), 309. [DOI] [PubMed] [Google Scholar]
- Berger M, & Sarnyai Z (2015). “More than skin deep”: stress neurobiology and mental health consequences of racial discrimination. Stress, 18(1), 1–10. [DOI] [PubMed] [Google Scholar]
- Bostwick WB, Meyer I, Aranda F, Russell S, Hughes T, Birkett M, & Mustanski B (2014). Mental health and suicidality among racially/ethnically diverse sexual minority youths. American Journal of Public Health, 104(6), 1129–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L (2012). The problem with the phrase women and minorities: Intersectionality—an important theoretical framework for public health. American Journal of Public Health, 102(7), 1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brailovskaia J, Teismann T, & Margraf J (2018). Cyberbullying, positive mental health and suicide ideation/behavior. Psychiatry Research, 267, 240–242. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Horowitz LM, Fontanella CA, Sheftall AH, Greenhouse J, Kelleher KJ, & Campo JV (2018). Age-related racial disparity in suicide rates among US youths from 2001 through 2015. JAMA Pediatrics, 172(7), 697–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U, & Morris PA (2006). The bioecological model of human development. In Lerner RM (Ed.), Handbook of child development: Vol. 1. Theoretical models of human development (6th ed., pp. 793–828). Wiley. [Google Scholar]
- Chambers BD, & Erausquin JT (2018). Race, sex, and discrimination in school settings: A multilevel analysis of associations with delinquency. Journal of School Health, 88(2), 159–166. [DOI] [PubMed] [Google Scholar]
- Clarke JN, & Mosleh D (2015). Risk and the Black American child: Representations of children’s mental health issues in three popular African American magazines. Health, Risk & Society, 17(1), 1–14. [Google Scholar]
- Cochran SD, Mays VM, Alegria M, Ortega AN, & Takeuchi D (2007). Mental health and substance use disorders among Latino and Asian American lesbian, gay, and bisexual adults. Journal of Consulting and Clinical Psychology, 75(5), 785–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C, Buchman-Schmitt JM, Stanley IH, Hom MA, Tucker RP, Hagan CR, Rogers ML, Podlogar MC, Chiurliza B, Ringer FB, Michaels MS, Patros CHG, & Joiner TE Jr. (2017). The interpersonal theory of suicide: A systematic review and meta-analysis of a decade of cross-national research. Psychological Bulletin, 143(12), 1313–1345. 10.1037/bul0000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu J, Khoury O, Ma J, Bahn F, Bongar B, & Goldblum P (2017). An empirical model and ethnic differences in cultural meanings via motives for suicide. Journal of Clinical Psychology, 73(10), 1343–1359. 10.1002/jclp.22425 [DOI] [PubMed] [Google Scholar]
- Collins PH (2000). Black feminist thought: Knowledge, consciousness, and the politics of empowerment. Routledge. [Google Scholar]
- Crenshaw K (1991). Mapping the margins: Identity politics, intersectionality, and violence against women. Stanford Law Review, 43(6), 1241–1299. [Google Scholar]
- Cullins LM, Solages MM, & McKnight S (2019). Depression in African American and Black Caribbean youth and the intersection of spirituality and religion: Clinical opportunities and considerations. Child and Adolescent Psychiatric Clinics of North America, 28(3), 473–482. [DOI] [PubMed] [Google Scholar]
- Curtin SC, & Heron M (2019) Death rates due to suicide and homicide among persons aged 10–24: United States, 2000–2017. NCHS Data Brief, no 352. National Center for Health Statistics. [PubMed] [Google Scholar]
- Davis GY, & Stevenson HC (2006). Racial socialization experiences and symptoms of depression among Black youth. Journal of Child and Family Studies, 15(3), 293–307. [Google Scholar]
- Dawson MC (1994). A black counterpublic? Economic earthquakes, racial agenda (s), and black politics. Public Culture, 7(1), 195–223. [Google Scholar]
- Drapeau CW, & McIntosh JL (2018). U.S.A. suicide 2017: Official final data. American Association of Suicidology. Retrieved December 10, 2018, from https://www.suicidology.org
- English D, Lambert SF, & Ialongo NS (2014). Longitudinal associations between experienced racial discrimination and depressive symptoms in African American adolescents. Developmental Psychology, 50(4), 1190–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farahmand FK, Grant KE, Polo AJ, & Duffy SN (2011). School-based mental health and behavioral programs for low-income, urban youth: A systematic and meta-analytic review. Clinical Psychology: Science and Practice, 18(4), 372–390. [Google Scholar]
- Gibbs JJ, & Goldbach J (2015). Religious conflict, sexual identity, and suicidal behaviors among LGBT young adults. Archives of Suicide Research, 19(4), 472–488. 10.1080/13811118.2015.1004476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman AH, & D’Augelli AR (2007). Transgender youth and life-threatening behaviors. Suicide & Life-Threatening Behavior, 37(5), 527–537. 10.1521/suli.2007.37.5.527 [DOI] [PubMed] [Google Scholar]
- Gomez J, Miranda R, & Polanco L (2011). Acculturative stress, perceived discrimination, and vulnerability to suicide attempts among emerging adults. Journal of Youth and Adolescence, 40(11), 1465–1476. 10.1007/s10964-011-9688-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn JF III, Goldstein SE, & Eccles JS (in preparation). A longitudinal investigation of suicidal thoughts in African American and European American young adults. [Google Scholar]
- Hastings JF, & Snowden LR (2019). African Americans and Caribbean Blacks: Perceived neighborhood disadvantage and depression. Journal of Community Psychology, 47(2), 227–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson DX, Jones J, McLeod K, Jackson K, Lunsford A, & Metzger I (2020). A phenomenological study of racial harassment in school and emotional effects among the retrospective accounts of older black adolescents. The Urban Review, 1–24. 10.1007/s11256-020-00551-5 [DOI] [Google Scholar]
- Henderson DX, Walker L, Barnes RR, Lunsford A, Edwards C, & Clark C (2019). A framework for race-related trauma in the public education system and implications on health for black youth. Journal of School Health, 89(11), 926–933. 10.1111/josh.12832 [DOI] [PubMed] [Google Scholar]
- Hjelmeland H, & Knizek BL (2020). The emperor’s new clothes? A critical look at the interpersonal theory of suicide. Death Studies, 44(3), 168–178. 10.1080/07481187.2018.1527796 [DOI] [PubMed] [Google Scholar]
- Hope EC, Hoggard LS, & Thomas A (2015). Emerging into adulthood in the face of racial discrimination: Physiological, psychological, and sociopolitical consequences for African American youth. Translational Issues in Psychological Science, 1(4), 342–351. [Google Scholar]
- Huebner DM, Kegeles SM, Rebchook GM, Peterson JL, Neilands TB, Johnson WD, & Eke AN (2014). Social oppression, psychological vulnerability, and unprotected intercourse among young Black men who have sex with men. Health Psychology, 33(12), 1568. [DOI] [PubMed] [Google Scholar]
- Joiner TE Jr. (2005). Why people die by suicide. Harvard University Press. [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, Lowry R, Chyen D, Whittle L, Thornton J, Lim C, Bradford D, Yamakawa Y, Leon M, Brener N, & Ethier KA (2018). Youth risk behavior surveillance-United States, 2017. Morbidity and Mortality Weekly Report Surveillance Summaries, 67(8), 1–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keels M, Durkee M, & Hope E (2017). The psychological and academic costs of school-based racial and ethnic microaggressions. American Educational Research Journal, 54(6), 1316–1344. [Google Scholar]
- King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, & Nazareth I (2008). A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry, 8(1), 70. 10.1186/1471-244X-8-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lardier DT Jr., Bermea AM, Pinto SA, Garcia-Reid P, & Reid RJ (2017). The relationship between sexual minority status and suicidal ideations among urban Hispanic adolescents. Journal of LGBT Issues in Counseling, 11(3), 174–189. [Google Scholar]
- Lambert SF, Herman KC, Bynum MS, & Ialongo NS (2009). Perceptions of racism and depressive symptoms in African American adolescents: The role of perceived academic and social control. Journal of Youth and Adolescence, 38(4), 519–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanier Y, Sommers MS, Fletcher J, Sutton MY, & Roberts DD (2017). Examining racial discrimination frequency, racial discrimination stress, and psychological well-being among Black early adolescents. Journal of Black Psychology, 43(3), 219–229. [Google Scholar]
- Lê Cook B, Barry CL, & Busch SH (2013). Racial/ethnic disparity trends in children’s mental health care access and expenditures from 2002 to 2007. Health Services Research, 48(1), 129–149. 10.1111/j.1475-6773.2012.01439.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsey MA, Chambers K, Pohle C, Beall P, & Lucksted A (2013). Understanding the behavioral determinants of mental health service use by urban, under-resourced black youth: Adolescent and caregiver perspectives. Journal of Child and Family Studies, 22(1), 107–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsey MA, Sheftall AH, Xiao Y, & Joe S (2019). Trends of suicidal behaveiors among high school students in the United States: 1991-2017. Pediatrics, 144(5), e20191187. 10.1542/peds.2019-1187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J, Batterham PJ, Calear AL, & Han J (2016). A systematic review of the predictions of the Interpersonal-Psychological Theory of Suicidal Behavior. Clinical Psychology Review, 46, 34–45. 10.1016/j.cpr.2016.04.008 [DOI] [PubMed] [Google Scholar]
- Mallett CA (2017). The school-to-prison pipeline: Disproportionate impact on vulnerable children and adolescents. Education and Urban Society, 49(6), 563–592. [Google Scholar]
- McGuire KM, Cisneros J, & McGuire TD (2017). Intersections at a (heteronormative) crossroad: Gender and sexuality among Black students’ spiritual-and-religious narratives. Journal of College Student Development, 58(2), 175–197. [Google Scholar]
- McLaughlin KA, Hilt LM, & Nolen-Hoeksema S (2007). Racial/ethnic differences in internalizing and externalizing symptoms in adolescents. Journal of Abnormal Child Psychology, 35(5), 801–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzger IW, Cooper SM, Ritchwood TD, Onyeuku C, & Griffin CB (2017). Profiles of African American college students’ alcohol use and sexual behaviors: Associations with stress, racial discrimination, and social support. The Journal of Sex Research, 54(3), 374–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzger IW, Salami T, Carter S, Halliday-Boykins C, Anderson RE, Jernigan MM, & Ritchwood T (2018). African American emerging adults’ experiences with racial discrimination and drinking habits: The moderating roles of perceived stress. Cultural Diversity and Ethnic Minority Psychology, 24(4), 489–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merkwae A (2015). Schooling the police: Race, disability, and the conduct of school resource officers. Michigan Journal of Race & Law, 21, 147–152. [Google Scholar]
- Mereish EH, O’Cleirigh C, & Bradford JB (2013). Interrelationships between LGBT-based victimization, suicide, and substance use problems in a diverse sample of sexual and gender minorities. Psychology, Health & Medicine 19(1), 1–13. 10.1080/13548506.2013.780129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Dietrich J, & Schwartz S (2008). Lifetime prevalence of mental disorders and suicide attempts in diverse lesbian, gay, and bisexual populations. American Journal of Public Health, 98(6), 1004–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller B, & Taylor J (2012). Racial and socioeconomic status differences in depresssive symptoms among black and white youth: An examination of the mediating effects of family structure, stress and support. Journal of Youth and Adolescence, 41(4), 426–437. [DOI] [PubMed] [Google Scholar]
- Murry VM, Heflinger CA, Suiter SV, & Brody GH (2011). Examining perceptions about mental health care and help-seeking among rural African American families of adolescents. Journal of Youth Adolescence, 40(9), 1118–1131. [DOI] [PubMed] [Google Scholar]
- Mustanski B, & Liu RT (2013). A longitudinal study of predictors of suicide attempts among lesbian, gay, bisexual, and transgender youth. Archives of Sexual Behavior, 42(3), 437–448. [DOI] [PubMed] [Google Scholar]
- Opara I, Lardier DT Jr., Reid RJ, & Garcia-Reid P (2019). “It all starts with the parents”: A qualitative study on protective factors for drug-use prevention among Black and Hispanic girls. Affilia, 34(2), 199–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opara I, Rodas EIR, Lardier DT, Garcia-Reid P, & Reid RJ (2020). Validation of the Abbreviated Socio-Political Control Scale for Youth (SPCS-Y) among urban girls of color. Child and Adolescent Social Work Journal, 37(1), 83–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips MR (2010). Rethinking the role of mental illness in suicide. American Journal of Psychiatry, 167(7), 731–733. 10.1176/appi.ajp.2010.10040589 [DOI] [PubMed] [Google Scholar]
- Pinderhughes H, Davis R, & Williams M (2015). Adverse community experiences and resilience: A framework for addressing and preventing community trauma. Prevention Institute. [Google Scholar]
- Polanco-Roman L, Anglin DM, Miranda R, & Jeglic EL (2019). Racial/ethnic discrimination and suicidal ideation in emerging adults: The role of traumatic stress and depressive symptoms varies by gender not race/ethnicity. Journal of Youth and Adolescence, 48(10), 2023–2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Respress BN, Amutah-Onukagha NN, & Opara I (2018). The effects of school-based discrimination on adolescents of color sexual health outcomes: A social determinants approach. Social Work in Public Health, 33(1), 1–16. [DOI] [PubMed] [Google Scholar]
- Seaton EK, Caldwell CH, & Sellers RM (2010). An Intersectional Approach for Understanding Perceived Discrimination and Psychological Well-Being Among African American and Caribbean Black Youth. Developmental Psychology, 46(5), 1372–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Settler NM, & Katz LF (2017). Minority stress, emotion regulation, and the parenting of sexual minority youth. Journal of GLBT Family Studies, 13(4), 380–400. [Google Scholar]
- Standley CJ (2020). Expanding our paradigms: Intersectional and socioecological approaches to suicide prevention. Death Studies, 1–9. Advance online publication. 10.1080/07481187.2020.1725934 [DOI] [PubMed] [Google Scholar]
- Stone DM, Luo F, Ouyang L, Lippy C, Hertz MF, & Crosby AE (2014). Sexual orientation and suicide ideation, plans, attempts, and medically serious attempts: Evidence from local youth risk behavior surveys, 2001–2009. American Journal of Public Health, 104(2), 262–271. 10.2105/AJPH.2013.301383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutter M, & Perrin PB (2016). Discrimination, mental health, and suicidal ideation among LGBTQ people of color. Journal of Counseling Psychology, 63(1), 98–105. 10.1037/cou0000126 [DOI] [PubMed] [Google Scholar]
- The Trevor Project. (2020, February 13). The Trevor Project research brief: Black LGBTQ youth mental health. The Trevor Project. https://www.thetrevorproject.org/2020/02/13/research-brief-black-lgbtq-youth-mental-health/
- Switzer R (2019). Suicide prevention and intervention. Life-Threatening Behavior, 48, 6. [Google Scholar]
- U.S. Census. (2018). Income and poverty report 2017. https://www.census.gov/content/dam/Census/library/publications/2018/demo/p60-263.pdf
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite S, Selby EA, & Joiner TE Jr. (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. 10.1037/a0018697 [DOI] [PMC free article] [PubMed] [Google Scholar]


