Background:
An augmented reality (AR)-based navigation system allows visualization of the center of the femoral head and femoral mechanical axis superimposed on the surgical field during total knee arthroplasty (TKA) and may help surgeons to improve the accuracy of distal femoral resection.
Methods:
First, we resected 10 femoral Sawbones specimens using the AR-based navigation system and performed computed tomography (CT) to measure the resection angle of the distal part of the femur. We calculated the absolute values of the differences between angles measured using CT images and angles displayed on the smartphone screen of the navigation system. Second, we measured coronal alignment using standing long-leg radiographs for 72 patients undergoing TKA and compared the error in the resection angle between TKA using the AR-based navigation system and that using a conventional intramedullary guide.
Results:
In the experimental study, the absolute values of the differences between angles measured on CT images and angles displayed using the AR-based navigation system were 0.8° ± 0.5° (range, 0.3° to 1.9°) in the coronal plane and 0.6° ± 0.5° (range, 0.0° to 1.4°) in the sagittal plane. In the clinical study, the mean absolute value of the error in coronal alignment was significantly smaller in the AR-based navigation group than the intramedullary-guide group (1.1° ± 1.0° [range, 0.0° to 3.2°] compared with 2.2° ± 1.6° [range, 0.0° to 5.5°], respectively; 95% confidence interval, 0.5° to 1.8°; p < 0.001).
Conclusions:
The AR-based navigation system may enable surgeons to perform distal femoral resection more accurately than with the conventional intramedullary guide during TKA.
Clinical Relevance:
This study validates the use of AR technology to enhance the precision of bone resection in TKA.
Lower-limb alignment in total knee arthroplasty (TKA) can affect the longevity of the prosthesis, the functional outcome of the knee, and patient satisfaction1,2. Modern technologies, such as computer navigation and robotic systems, allow surgeons to obtain more precise alignment than achieved with conventional surgical techniques3. However, the main drawback of these systems has been a lack of cost-effectiveness4. Radiation exposure is another important concern because some of these systems require preoperative computed tomography (CT) of the lower limb5.
Recently, we developed the AR-KNEE system, a novel augmented reality (AR)-based navigation system using AR technology applied to TKA. In the AR milieu, 3-dimensional (3-D) virtual objects are integrated into a 3-D real environment in real time6-8. The AR-KNEE system allows surgeons to see the center of the femoral head and femoral mechanical axis integrated in the surgical field. The running cost is low because surgeons can use the AR-KNEE system with a free application installed on their own smartphone. In addition, the AR-KNEE system does not require any preoperative imaging studies. Although the AR-KNEE system was shown to be accurate to within <1° in both coronal and sagittal planes in resection of the proximal part of the tibia9, there have been no studies to date assessing the accuracy of this system in distal femoral resection.
We performed the present study to evaluate the accuracy of the AR-KNEE system in distal femoral resection during TKA. This investigation consisted of 2 parts: a pilot study using femoral Sawbones specimens (Pacific Research Laboratories) to verify the accuracy of the AR-KNEE system and a clinical study to compare the accuracy of resection using the AR-KNEE system with that using the conventional intramedullary guide. We tested the following 2 hypotheses: (1) the mean error in both coronal and sagittal alignment would be <1.0° when resecting Sawbones specimens using the AR-KNEE system, and (2) coronal alignment would be more accurate in patients when using the AR-KNEE system compared with the conventional intramedullary guide.
Materials and Methods
The study protocols for both the pilot study using Sawbones specimens and the clinical study to compare the AR-KNEE system and conventional intramedullary guide were approved by the institutional review board.
AR-KNEE System
AR technology can project computer-generated images onto real-world images and show the results on the display of a smartphone10. The AR-KNEE system allows the surgeon to view the center of the femoral head and femoral mechanical axis superimposed onto the surgical field on the display of the surgeon’s own smartphone. The AR-KNEE system also shows the varus/valgus angle in the coronal plane and the flexion/extension angle in the sagittal plane. The AR-KNEE system provides real-time information similar to conventional computer navigation.
The AR-KNEE system does not require any additional incisions, as its dedicated jig is placed on the articular surface of the distal part of the femur. Surgeons can use the AR-KNEE system regardless of the brand of prosthesis used. The operation of the AR-KNEE system is completed by the surgeon in the sterile zone alone; neither assistants nor additional equipment are required in the nonsterile zone.
A resin marker with a square 2-dimensional bar code is laid on a stable location in the surgical field. This marker is not fixed to the patient but is only placed on a stable site, such as a Mayo table. The surgeon inserts the spike of the dedicated jig of the AR-KNEE system at the midpoint of the mediolateral width of the distal part of the femur and attaches a smartphone to the jig. The spike has anterior and posterior fins. The surgeon aligns these fins to the Whiteside line, defined as the line connecting the anterior patellar groove and the center of the intercondylar notch. Viewing the marker through the camera of the smartphone, the surgeon moves the leg of the patient from flexion to extension and rotates the leg externally and internally (Fig. 1). This allows the application to determine the center of the femoral head using the least squares method11. After completing registration, the AR-KNEE system enables the surgeon to view the center of the femoral head and the mechanical axis of the femur superimposed on the image of the femur on their smartphone display (Fig. 2). The axis of rotation of the femur is determined according to the Whiteside line when the spike of the dedicated jig is inserted. The center of the femoral head, the midpoint of the mediolateral width of the distal part of the femur, and the axis of rotation of the femur constitute the femoral coordinate system of the AR-KNEE system (Fig. 3). As an option, the surgeon can manually register the Whiteside line or surgical epicondylar axis as the rotational axis by touching the anatomic landmarks (Fig. 4).
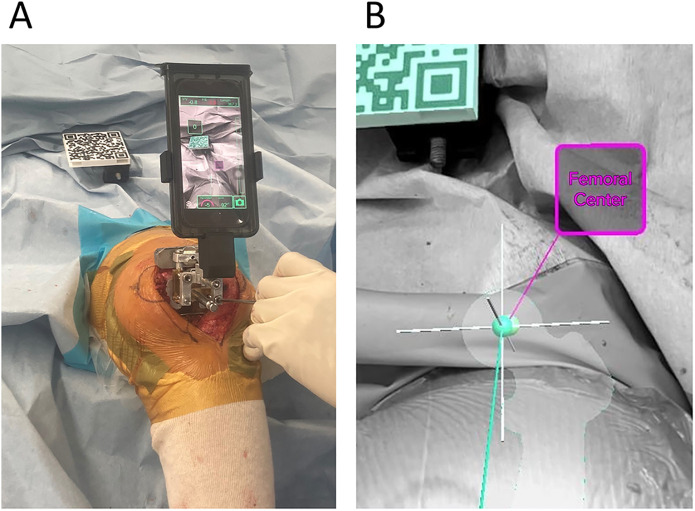
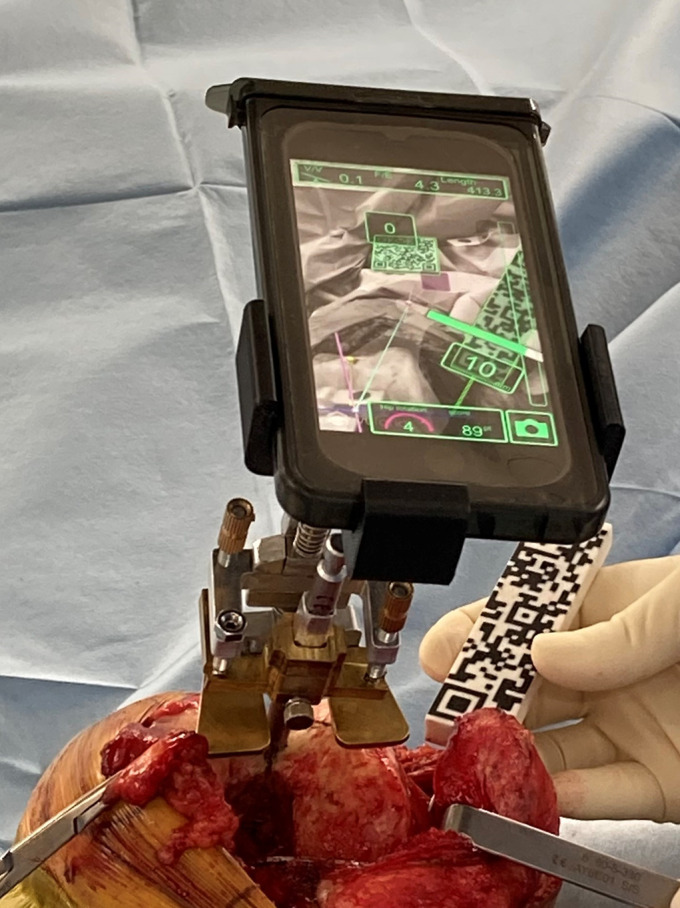
Fig. 1.
Registration of the femoral head center in the AR-KNEE system (left knee). The surgeon moves the leg from flexion to extension and rotates the leg externally and internally while viewing the resin marker with a square 2-dimensional bar code through the camera of a smartphone. After registration, the AR-KNEE system enables the surgeon to view the center of the femoral head and the mechanical axis of the femur on the smartphone display in real time. Note that the marker is not fixed to the patient but is only placed in a stable location.
Fig. 2.
Figs. 2-A and 2-B Aligning the dedicated cutting jig of the AR-KNEE system (left knee). Fig. 2-A The smartphone shows the angle between the cutting jig and the mechanical axis of the femur in real time. The surgeon aligns the jig using a screwdriver, viewing the angle on the smartphone. When the smartphone camera recognizes the 2-dimensional bar code, the color of the marker turns light green on the screen. Fig. 2-B Screenshot of the smartphone image. The light green sphere is the center of the femoral head, and the light green line is the mechanical axis of the femur.
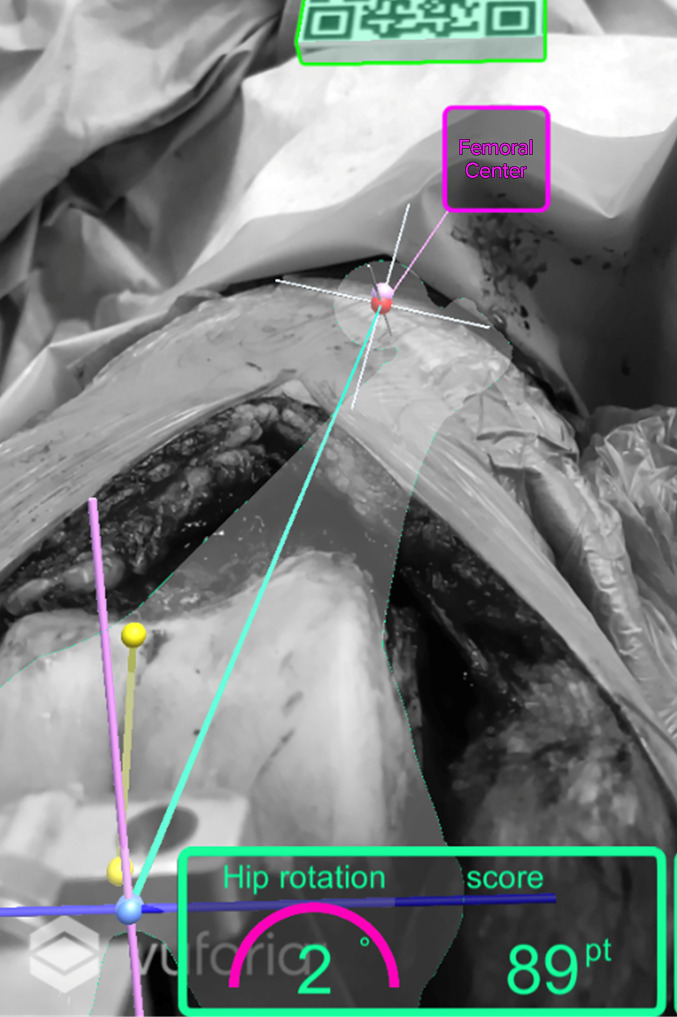
Fig. 3.
A femoral coordinate system superimposed on the surgical field (screenshot of the smartphone image, left knee). The light green line connecting the center of the femoral head (red sphere) and the insertion point of the spike of the dedicated jig (light blue sphere) is the mechanical axis of the femur. The rotational axis of the femur (light purple line) is set by aligning the anterior and posterior fins of the spike to the Whiteside line when the dedicated jig is fixed at the distal part of the femur. The sagittal plane is formed from the light green and light purple lines. The surgeon can also register the Whiteside line by touching the anterior patellar groove and the center of the intercondylar notch using a pointer (yellow line connecting 2 yellow spheres).
Fig. 4.
Registration of the surgical epicondylar axis using a pointer with a rectangular 2-dimensional bar code (left knee). Although the AR-KNEE system is designed to utilize the Whiteside line as the reference axis of rotation of the femur, the surgical epicondylar axis can also be utilized with manual registration of the sulcus of the medial epicondyle and the most prominent point of the lateral epicondyle according to the surgeon’s preference. Note that the color of the whole pointer turns light green on the screen after the smartphone camera recognizes the pointer.
Verification of the Accuracy of the AR-KNEE System Using Sawbones Specimens
A total of 10 femoral Sawbones specimens were resected by a single surgeon (S.T.) using the AR-KNEE system. We aimed perpendicular to the femoral mechanical axis in the coronal plane and at 5° of flexion in the sagittal plane. The rotational alignment was determined according to the surgical epicondylar axis.
We performed CT of the resected Sawbones and measured the varus/valgus angle in the coronal plane and flexion/extension angle in the sagittal plane using computer software (ZedKnee; LEXI)9. To measure these angles, we established a 3-D coordinate system according to the following definition: (1) the x axis refers to the line connecting the sulcus of the medial epicondyle and the most prominent point of the lateral epicondyle, (2) the y axis refers to a line perpendicular to the plane formed by the center of the femoral head and the midpoint of the mediolateral width of the resected distal part of the femur, and (3) the z axis refers to a line perpendicular to both the x and y axes. The coronal plane consisted of the x and y axes, and the sagittal plane consisted of the y and z axes.
Accuracy of the Femoral Resection Angle: AR-KNEE System Versus Conventional Intramedullary Guide
This study included 74 consecutive TKAs performed by a single surgeon (S.T.) between March 2020 and August 2020. All patients received a posterior cruciate-stabilized knee prosthesis (Triathlon [Stryker] or Persona [Zimmer Biomet]). Exclusion criteria determined prior to data collection were preoperative ankylosis of the knee and the inability to attain the appropriate extension knee angle despite postoperative rehabilitation.
The AR-KNEE system was used for distal femoral resection in 31 knees (AR-KNEE group), and the intramedullary guide was used in the remaining 43 knees (intramedullary-guide group). The target of femoral coronal alignment was perpendicular to the mechanical axis in both groups. A postoperative standing long-leg radiograph with the patella facing forward was made when the knee extension angle of each patient was more than −5° (i.e., flexion contracture was <5°). Three investigators blinded to the groups independently measured the lateral distal femoral angle (LDFA) to the first decimal place (Fig. 5). Although CT-based measurement would assess postoperative lower-limb alignment more accurately than the use of standing radiographs, our clinical study omitted routine postoperative CT scans to avoid patient radiation exposure. The primary outcomes of this comparative study were the absolute values of the differences between the LDFA measured using a standing long-leg radiograph and the targeted LDFA of 90°.
Fig. 5.
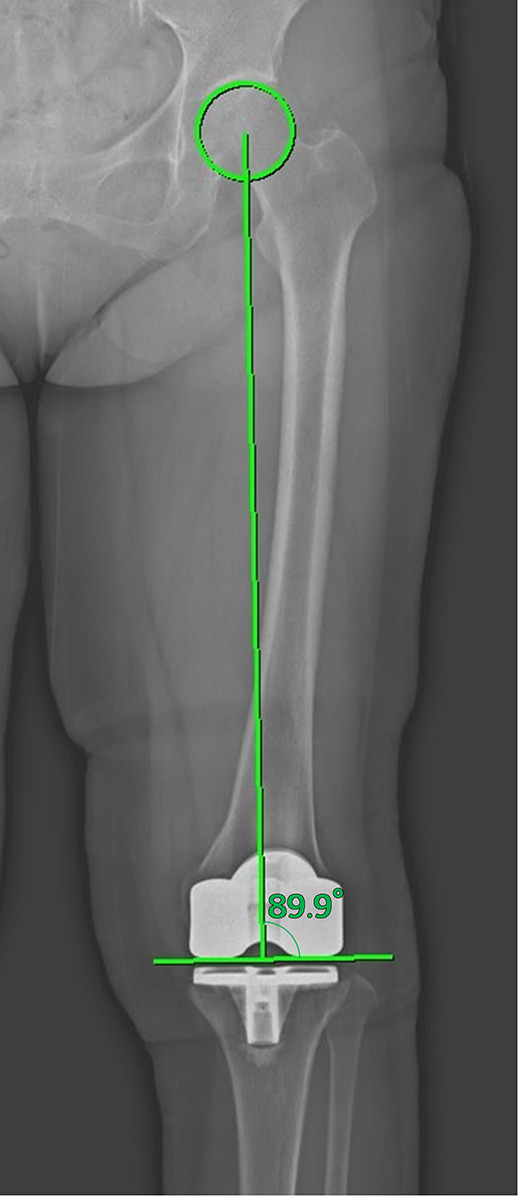
Measurement of the lateral distal femoral angle (LDFA) using a standing long-leg radiograph. The LDFA was measured between the mechanical axis and a line parallel to the femoral component (89.9° in this patient). The mechanical axis is defined as the line connecting the center of the femoral head and the center of the femoral component.
In the AR-KNEE group, we resected the distal part of the femur using the above-mentioned technique. To stabilize the marker, which carried a square 2-dimensional bar code, we attached a mounting bracket for home use to the operating table (see Appendix). A sterile smartphone cover (CleanCase; SteriDev) was used to manage sterility in the operative field (Fig. 6).
Fig. 6.

Sterile smartphone cover to manage sterility in the operative field. The nonsterile mobile device is inserted into the sterile smartphone cover (CleanCase; SteriDev). The surgeon can operate the smartphone with gloved hands.
In the intramedullary-guide group, we preoperatively measured (1) the angle between the femoral mechanical axis and the predicted line through which the femoral intramedullary rod would pass and (2) the depth of the resected bone at both medial and lateral condyles (Fig. 7). First, we set the valgus angle of distal femoral resection to the measured angle. After inserting the intramedullary rod into the femur, the valgus angulation was adjusted using the depth of the resected medial and distal condyles.
Fig. 7.
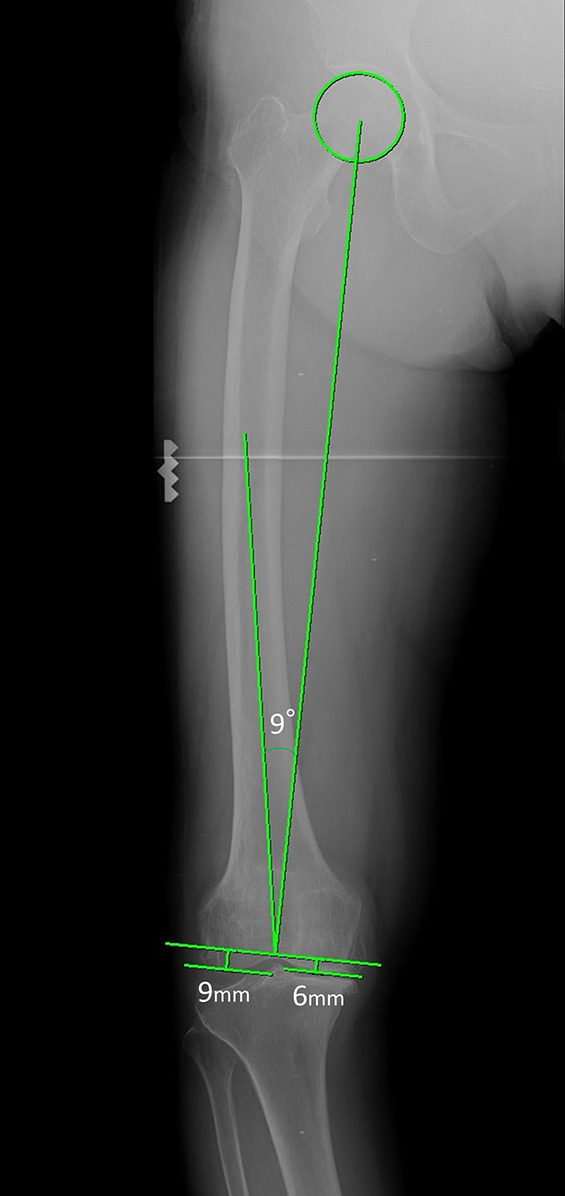
Preoperative planning for distal femoral resection in the intramedullary-guide group. The depth of the resected distal part of the femur (6 mm of the medial condyle and 9 mm of the lateral condyle in this patient) was measured preoperatively and assumed that the distal part of the femur would be accurately resected at the planned valgus angle, which was determined to be the angle between the femoral mechanical axis and the line through which the intramedullary rod was predicted to pass (9° in this patient). After inserting the intramedullary rod into the femur, the valgus angulation was adjusted using the preoperatively measured depth of the resected medial and lateral condyles. Note that we did not employ the anatomical axis of the femur because the line through which the intramedullary guide passed differed from the anatomical axis of the femur. In this patient, the intramedullary guide did not pass through the proximal part of the femur because of lateral femoral bowing.
Statistical Analysis
Verification of the accuracy of the AR-KNEE system using femoral Sawbones specimens was performed in the manner of a descriptive study. We calculated the absolute values of the differences between angles measured using CT and angles displayed on the smartphone screen in terms of varus/valgus and flexion/extension angles. The mean, standard deviation (SD), and range were calculated for each parameter.
In the clinical comparison between the AR-KNEE system and conventional intramedullary guide, we considered an improvement of 1.0° in the LDFA to be clinically meaningful. We needed at least 31 patients per group to detect a mean difference (and SD) of 1.0° ± 1.4° in the LDFA with a 2-sided significance level of 5% and power of 80%. The primary outcome was compared using a Student t test and reported with 95% confidence intervals (CIs) for the between-group differences. To test interobserver reliability, the intraclass correlation coefficients of postoperative measurements of the LDFA using standing long-leg radiographs were calculated for 3 assessors. Other comparisons between the study groups were performed using a Fisher exact test for categorical variables and a Student t test for continuous variables. All tests were 2-sided, and a p value of <0.05 was considered significant.
Source of Funding
There was no external funding for this investigation.
Results
Verification of the Accuracy of the AR-KNEE System Using Sawbones Specimens
The absolute values of the differences between angles measured using CT and angles displayed on the smartphone screen were 0.8° ± 0.5° (range, 0.3° to 1.9°) in the coronal plane and 0.6° ± 0.5° (range, 0.0° to 1.4°) in the sagittal plane.
Accuracy of Femoral Resection Angle: AR-KNEE System Versus Conventional Intramedullary Guide
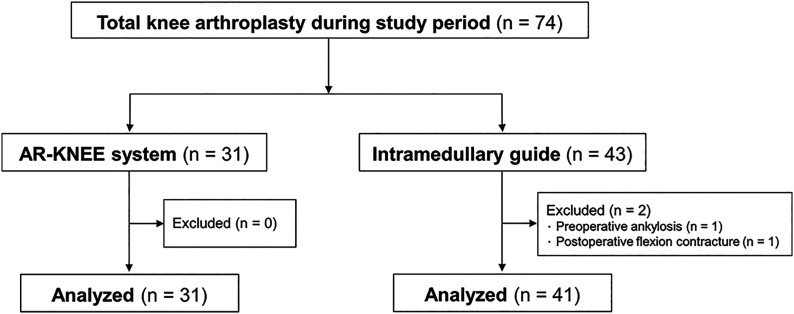
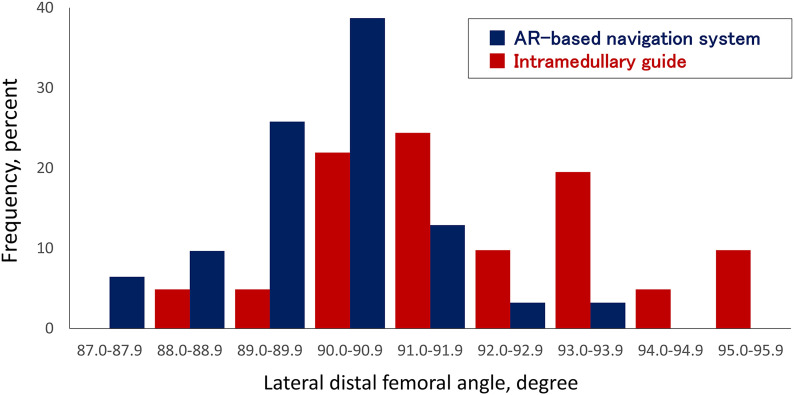
We excluded 2 patients in the conventional intramedullary-guide group (Fig. 8). Table I summarizes the demographic characteristics of the remaining patients. The absolute values of the differences between the LDFA measured using a standing long-leg radiograph and the targeted LDFA of 90° were smaller in the AR-KNEE group than in the intramedullary guide group (1.1° ± 1.0° [range, 0.0° to 3.2°] compared with 2.2° ± 1.6° [range, 0.0° to 5.5°], respectively; 95% CI of the difference between the methods, 0.5° to 1.8°; p < 0.001). Figure 9 shows the distribution of LDFA values for all patients. The intraclass correlation coefficient between the 3 assessors for the LDFA was 0.86 (95% CI, 0.80 to 0.91).
Fig. 8.
Patient flow diagram.
Fig. 9.
Distribution of postoperative lateral distal femoral angle (LDFA) measurements on analysis of standing long-leg radiographs. An LDFA of >90° and of <90° indicate varus and valgus alignment of the femoral component in the coronal plane, respectively.
TABLE I.
Patient Demographic and Baseline Clinical Characteristics
| AR-Based Navigation System (N = 31) | Intramedullary Guide (N = 41) | P Value | |
|---|---|---|---|
| Age* (yr) | 73 ± 9 | 74 ± 7 | 0.57† |
| Female/male sex (no.) | 28/3 | 36/5 | >0.99‡ |
| Height* (cm) | 151 ± 10 | 152 ± 8 | 0.54† |
| Weight* (kg) | 61.7 ± 10.0 | 64.5 ± 13.1 | 0.32† |
| Body mass index* (kg/m2) | 27.1 ± 3.8 | 27.7 ± 4.3 | 0.56† |
| Preop. diagnosis (osteoarthritis/rheumatoid arthritis) (no.) | 29/2 | 40/1 | 0.57‡ |
| Preop. hip-knee-ankle angle*§ (deg) | −10.2 ± 8.8 | −10.4 ± 10.1 | 0.94† |
| Preop. knee flexion angle* (deg) | 122 ± 12 | 119 ± 17 | 0.35† |
| Preop. knee extension angle* (deg) | −10 ± 5 | −11 ± 8 | 0.69† |
| Duration of surgery* (min) | 90 ± 12 | 81 ± 9 | <0.001† |
| Prosthesis (Persona/Triathlon) (no.) | 19/12 | 23/18 | 0.81‡ |
The values are given as the mean and standard deviation.
Student t test.
Fisher exact test.
Negative values indicated varus lower-limb alignment.
No complications were observed in the patients. In particular, no intraoperative loosening of the dedicated jig or intraoperative fracture occurred in the AR-KNEE system group.
Discussion
Although TKA is one of the most successful orthopaedic procedures, obtaining appropriate postoperative lower-limb alignment with high reproducibility is still crucial for boosting longevity of the prosthesis and pain relief1,2. The mean error in distal femoral resection of Sawbones specimens was <1.0° in both coronal and sagittal planes when using the AR-KNEE system in the experimental study. Moreover, the AR-KNEE system, which did not require any expensive equipment or radiation exposure to the patient or surgeon, provided more accurate distal femoral resection than the conventional surgical technique using the intramedullary guide in a clinical setting.
Although AR technology has been used in many orthopaedic procedures12,13, to our knowledge, there have been no clinical studies investigating the usefulness of AR technology in TKA. This is the first clinical study to investigate the accuracy of an AR-based navigation system for TKA. The basic mechanism of the AR-KNEE system is similar to that of conventional infrared optical navigation systems, which use infrared irradiation to recognize reflective balls or infrared light with infrared cameras8. However, the AR-based navigation system uses visible light to recognize markers with an ordinary camera. Our results support the accuracy of AR-based navigation using the markers and camera. In total hip arthroplasty (THA), Ogawa et al. showed that an AR-based navigation system provided a significantly more accurate inclination angle in the acetabular shell placement than the conventional technique8. The results of that study also supported the accuracy of the AR-KNEE system.
The mean operative time in the AR-KNEE group was 9 minutes longer than that in the intramedullary-guide group. We believe that the benefit of more reproducible femoral-component alignment supersedes the 9-minute increase in the operative time. However, it remains a contentious issue whether the prolongation would be justified as there has been conflicting evidence regarding improvement of lower-limb alignment with use of navigation systems. The Australian Orthopaedic Association National Joint Replacement Registry demonstrated reduction of the revision rate after TKA through the use of navigation14, whereas the New Zealand Joint Registry showed no improvement in survival or functional outcome scores15.
Our study had several limitations. First, although we assessed coronal alignment using a standing long-leg radiograph in the clinical study, the sagittal alignment was not measured. The sagittal alignment was measured only in the experimental study using Sawbones utilizing CT because the institutional review board determined that additional radiation exposure was unethical in a clinical setting. The highly reproducible sagittal alignment of the femoral component is crucial as sagittal malalignment can reduce survival of the TKA prosthesis16. We believe that the AR-KNEE system would provide similar reproducibility in sagittal alignment to that in coronal alignment because the mechanism of determining sagittal alignment using the AR-KNEE system is the same as that for coronal alignment. Second, the allocation to the 2 techniques was not randomized in this study. Although there were no significant differences in the demographic data between the AR-KNEE and conventional intramedullary-guide groups, randomly assigning the intervention could eliminate the influence of confounding variables. Finally, as all TKAs were performed by a single surgeon, our findings lack generalizability to the overall population. Randomized controlled studies including multiple surgeons are needed to confirm the clinical effectiveness of the AR-KNEE system.
In conclusion, the mean error in distal femoral resection was <1.0° in both coronal and sagittal planes when using the AR-KNEE system in an experimental setting. The nonrandomized comparative study showed that the AR-KNEE system provided significantly greater accuracy during distal femoral resection in TKA compared with the conventional intramedullary guide in a clinical setting.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A299).
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Hokusuikai Kinen Hospital, Mito, Japan
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A298).
References
- 1.Matsuda S, Kawahara S, Okazaki K, Tashiro Y, Iwamoto Y. Postoperative alignment and ROM affect patient satisfaction after TKA. Clin Orthop Relat Res. 2013. January;471(1):127-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee BS, Cho HI, Bin SI, Kim JM, Jo BK. Femoral component varus malposition is associated with tibial aseptic loosening after TKA. Clin Orthop Relat Res. 2018. February;476(2):400-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsumoto T, Nakano N, Lawrence JE, Khanduja V. Current concepts and future perspectives in computer-assisted navigated total knee replacement. Int Orthop. 2019. June;43(6):1337-43. Epub 2018 May 12. [DOI] [PubMed] [Google Scholar]
- 4.Novak EJ, Silverstein MD, Bozic KJ. The cost-effectiveness of computer-assisted navigation in total knee arthroplasty. J Bone Joint Surg Am. 2007. November;89(11):2389-97. [DOI] [PubMed] [Google Scholar]
- 5.Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M. Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am. 2016. April 20;98(8):627-35. [DOI] [PubMed] [Google Scholar]
- 6.Azuma RT. A survey of augmented reality. Presence: Teleoperators Virtual Environ. 1997. August;6(4):355-85. [Google Scholar]
- 7.Blackwell M, Morgan F, DiGioia AM, 3rd. Augmented reality and its future in orthopaedics. Clin Orthop Relat Res. 1998. September;354:111-22. [DOI] [PubMed] [Google Scholar]
- 8.Ogawa H, Kurosaka K, Sato A, Hirasawa N, Matsubara M, Tsukada S. Does an augmented reality-based portable navigation system improve the accuracy of acetabular component orientation during THA? A randomized controlled trial. Clin Orthop Relat Res. 2020. May;478(5):935-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsukada S, Ogawa H, Nishino M, Kurosaka K, Hirasawa N. Augmented reality-based navigation system applied to tibial bone resection in total knee arthroplasty. J Exp Orthop. 2019. November 11;6(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ogawa H, Hasegawa S, Tsukada S, Matsubara M. A pilot study of augmented reality technology applied to the acetabular cup placement during total hip arthroplasty. J Arthroplasty. 2018. June;33(6):1833-7. Epub 2018 Feb 5. [DOI] [PubMed] [Google Scholar]
- 11.Arun KS, Huang TS, Blostein SD. Least-squares fitting of two 3-d point sets. IEEE Trans Pattern Anal Mach Intell. 1987. May;9(5):698-700. [DOI] [PubMed] [Google Scholar]
- 12.Laverdière C, Corban J, Khoury J, Ge SM, Schupbach J, Harvey EJ, Reindl R, Martineau PA. Augmented reality in orthopaedics: a systematic review and a window on future possibilities. Bone Joint J. 2019. December;101-B(12):1479-88. [DOI] [PubMed] [Google Scholar]
- 13.Casari FA, Navab N, Hruby LA, Kriechling P, Nakamura R, Tori R, de Lourdes Dos Santos Nunes F, Queiroz MC, Fürnstahl P, Farshad M. Augmented reality in orthopedic surgery is emerging from proof of concept towards clinical studies: a literature review explaining the technology and current state of the art. Curr Rev Musculoskelet Med. 2021. April;14(2):192-203. Epub 2021 Feb 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Steiger RN, Liu YL, Graves SE. Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty-five years of age. J Bone Joint Surg Am. 2015. April 15;97(8):635-42. [DOI] [PubMed] [Google Scholar]
- 15.Roberts TD, Frampton CM, Young SW. Outcomes of computer-assisted surgery compared with conventional instrumentation in 19,221 total knee arthroplasties: results after a mean of 4.5 years of follow-up. J Bone Joint Surg Am. 2020. April 1;102(7):550-6. [DOI] [PubMed] [Google Scholar]
- 16.Kim YH, Park JW, Kim JS, Park SD. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop. 2014. February;38(2):379-85. Epub 2013 Sep 10. [DOI] [PMC free article] [PubMed] [Google Scholar]