Transient cortical blindness (TCB) is an uncommon complication following coronary angiography. This report describes a case of TCB after coronary…
Key Words: complication, contrast agent, coronary angiography
Abbreviations and Acronyms: BP, blood pressure; CT, computed tomography; MRI, magnetic resonance imaging; TCB, transient cortical blindness
Abstract
Transient cortical blindness (TCB) is an uncommon complication following coronary angiography. This report describes a case of TCB after coronary angiography in a patient admitted for acute myocardial infarction. The patient’s vision recovered completely within 16 h, and cardiac magnetic resonance imaging performed 2 months later revealed no significant abnormalities. (Level of Difficulty: Beginner.)
Graphical abstract
Transient cortical blindness is an uncommon complication which follows coronary angiography. It was first reported in 1970 (1) with an incidence of 0.05% to 0.08% (2). The mechanism and physiopathology remain unknown and largely speculative (3). It has been attributed to a toxic reaction of the contrast agent as it penetrates into the brain parenchyma, and some patients seem to be more susceptible than others (4). Symptoms of blurring of vision and blindness may begin during the procedure or develop after it is completed. Neurological examination is completely normal. Other symptoms such as headache, disorientation, and amnesia may be present 5, 6, 7. The demonstration of contrast enhancement in the occipital cortex on computed tomography (CT) scan or cardiac magnetic resonance confirms the diagnosis in most cases (8). The outcome is generally favorable, with the return of sight within 24 to 48 h (5).
Learning Objectives
-
•
Transient cortical blindness is a rare but recognized complication following coronary angiography which needs to be taken into consideration.
-
•
This paper reports an infrequent clinical case, alerting the reader to not only the existence of cortical blindness but also its presentation, differential diagnosis, and treatment.
History of Presentation and Medical History
A 45-year-old female with multiple sclerosis, high blood pressure, and obesity presented to the emergency department with recurrent episodes of chest pain. She was admitted to the cardiology department where non-ST-segment elevation myocardial infarction, Killip stage I, with a hypertensive profile (blood pressure: 169/112 mm Hg) was diagnosed. Conventional treatment according to European guidelines was implemented, and an invasive approach was taken 15 h after admission. Following protocol, the patient was pre-treated with acetylsalicylic acid, ticagrelor, nitrates, and unfractionated heparin. Diagnostic coronary angiography was performed from the right radial artery and revealed 3-vessel coronary disease. A staged intervention was chosen, and an angioplasty of the left anterior descending artery with implantation of an Onyx 2.5- × 22-mm medicate stent (Medtronic, Friedly, Minnesota) was immediately performed. Overall, 133 ml of contrast agent, iomeprol, was used during the procedure. The final angiographic result was good, without clinical complications.
One hour after the procedure, the patient started complaining of headache and blurred vision, which quickly progressed to complete bilateral blindness. She also presented with behavioral changes, anxiety, nausea, and decreased auditory acuity.
Neurological examination did not reveal any other changes. Cranial nerve, sensory, and motor examinations were normal. There was no facial asymmetry, aphasia, dysarthria, or dysmetria. Oculomotor movements and pupillary reflexes were preserved. Fundoscopy examination was completely normal.
Differential Diagnosis and Investigations
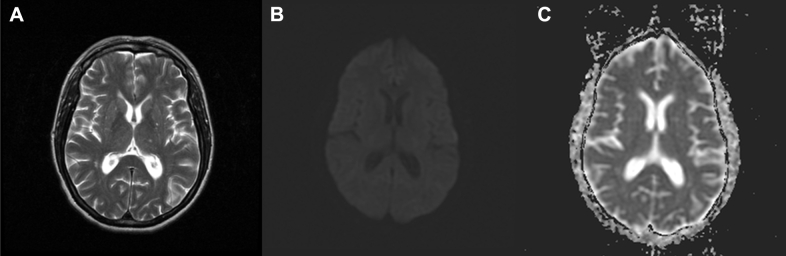
Blood analysis showed preserved renal function and normal ionogram. Immediately, brain CT scan and cranial angiography were performed and did not reveal acute endocranial lesions, especially of a vascular cause, which is the main differential diagnosis (Figure 1). In order to exclude an anaphylactic reaction to the contrast agent, hydrocortisone was administered but without any improvement. Electroencephalography showed no paroxysmal activity and a discretely slow and diffuse base rhythm.
Figure 1.
Brain CT Scan 2 h After Cardiac Catheterization
The axial cut at the level of the ventricular prolongations of the occipital lobes shows normal density of the surrounding parenchyma and sulcus. CT = computed tomography.
Management
After neurological and ophthalmological evaluation, bilateral cortical blindness without focal neurological deficits was diagnosed. Because of acute psychomotor agitation, sedation with midazolam and haloperidol was needed. Except for sedation, only intravenous hydration was carried out.
Follow-Up
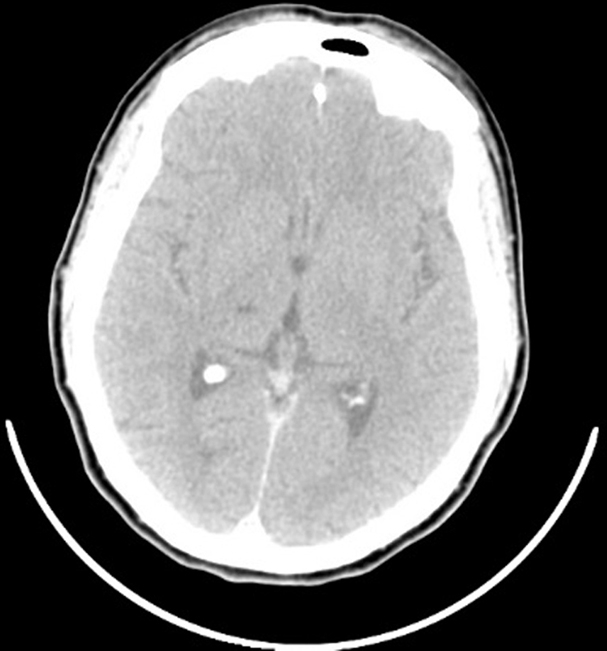
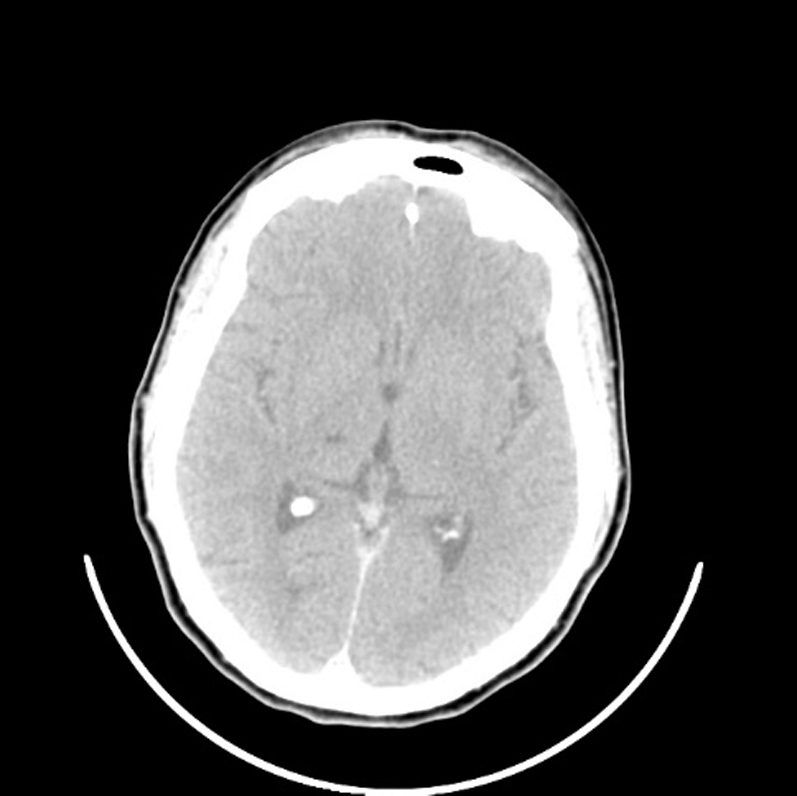
The patient's vision started to improve and recovered completely within 16 h of the coronary angiography procedure. She remained asymptomatic during the subsequent hospital stay, without any recurrence or complications. Cardiac magnetic resonance performed 2 months after the episode showed no significant abnormalities (Figure 2).
Figure 2.
MR Imaging Performed 2 Months After the Episode
Axial sections of the T2 sequences (A), diffusion-weighted imaging (B), and apparent diffusion coefficient map (C) show normal signal emission of the parenchyma and sulcus in the occipital region and absence of diffusion abnormalities; therefore, recent ischemic or hemorrhagic lesions in this region are excluded. MR = magnetic resonance.
Discussion
There are several possible complications after cardiac catheterization, usually divided into coronary vascular injury, other vascular events, and systemic nonvascular events. Major adverse cardiac and cerebrovascular events include death, stroke, and myocardial infarction. Additional complications include bleeding, nephropathy, atheroembolism, allergic reactions, and arrhythmia (9).
Transient cortical blindness is a rare but recognized complication following coronary angiography. It was the first case to be reported in the authors’ catheterization laboratory.
The physiopathology remains unknown and largely speculative. It has been attributed to a toxic reaction of the contrast agent as it penetrates the brain parenchyma, caused by an acute disruption of the blood-brain barrier. An intrinsic vulnerability of the occipital cortex (reduced sympathetic innervation and relative lack of protective sympathetic mediated arteriolar vasoconstriction) may justify an increased frequency of its involvement (3). Direct idiosyncratic neurotoxicity appears to be the most plausible explanation (2), although it does not seem to be volume-dependent (4). Some patients are more prone than others to idiosyncratic reactions, and some risk factors have been proposed: uncontrolled hypertension, hypoventilation, immunological mechanisms, and renal insufficiency (4).
Interestingly, in many documented cases of transient cortical blindness, patients had already been exposed to contrast agents before, without any complications 4, 6, 8. Symptoms may begin during the procedure or develop after it is completed. It usually presents as blurring of vision which rapidly progresses to total blindness (2). Besides that, neurological examination is completely normal, including fundoscopic examination. Associated symptoms include severe headache (5), vomiting, confusion, disorientation (6), and total retrograde amnesia (7).
Differential diagnosis with embolic complications caused by catheter manipulation can be difficult. Although cerebral infarction is rare, microembolization (air, thrombus, or aortic atheroma) has been reported in patients undergoing cardiac catheterization (10). Such events are normally silent or associated with focal neurological defects (3), in contrast to this complication.
The demonstration of contrast enhancement in the occipital cortex on CT scan or cardiac magnetic resonance confirms the diagnosis in most cases. Repeated imaging of the brain shows complete resolution of that (8).
Cortical blindness is usually transient and resolves completely without requiring any treatment. Despite limited evidence, one possibility could be to reduce the amount of contrast agent and treat the patient with steroids before exposure (5). The outcome is generally favorable, with the return of sight within 24 to 48 h. Experience with re-exposure is limited but appears to carry no increased risk (5).
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
References
- 1.Fischer-Williams M., Gottschalk P.G., Browell J.N. Transient cortical blindness: an unusual complication of coronary angiography. Neurology. 1970;20:353–355. doi: 10.1212/wnl.20.4.353. [DOI] [PubMed] [Google Scholar]
- 2.Mouine N., Ndom M.S., Hankari T., Zbir M. Transient cortical blindness after coronary angiography: report of 2 cases. Am J Mens Health. 2010;7:431–433. [Google Scholar]
- 3.Borghi C., Saia F., Marzocchi A., Branzi A. The conundrum of transient cortical blindness following coronary angiography. J Cardiovasc Med. 2008;9:1063–1065. doi: 10.2459/JCM.0b013e3282fe1718. [DOI] [PubMed] [Google Scholar]
- 4.Alp B.N., Bozbuga N., Tuncer M.A., Yakut C. Transient cortical blindness after coronary angiography. J Int Med Res. 2009;37:1246–1251. doi: 10.1177/147323000903700433. [DOI] [PubMed] [Google Scholar]
- 5.Rama B.N., Pagano T.V., DelCore M., Knobel K.R., Lee J. Cortical Blindness after cardiac catheterization: effect of rechallenge with dye. Cathet Cardiovasc Diagn. 1993;28:149–151. doi: 10.1002/ccd.1810280211. [DOI] [PubMed] [Google Scholar]
- 6.Lara J.G., Vázquez-Rodríguez J.M., Salgado-Fernández J. Transient cortical blindness following cardiac catheterization: an alarming but infrequent complication with a good prognosis. Rev Esp Cardiol. 2008;61:88–90. [PubMed] [Google Scholar]
- 7.Sticherling C., Berkefeld J., Auch-Schwelk W., Lanfermann H. Transient bilateral cortical blindness after coronary angiography. Lancet. 1998;351:570. doi: 10.1016/S0140-6736(05)78557-3. [DOI] [PubMed] [Google Scholar]
- 8.Balasingam S., Azman R.R., Nazri M. Contrast media induced transient cortical blindness. QJM. 2016;109:121–122. doi: 10.1093/qjmed/hcv121. [DOI] [PubMed] [Google Scholar]
- 9.Bashore T.M., Balter S., Barac A., Byrne J.G., Cavendish J.J., Chambers C.E. 2012 American College of Cardiology Foundation/Society for Cardiovascular Angiography and Interventions Expert Consensus document on cardiac catheterization laboratory standards update. J Am Coll Cardiol. 2012;59:2221–2305. doi: 10.1016/j.jacc.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 10.Tavakol M., Ashraf S., Brener S.J. Risks and complications of coronary angiography: a comprehensive review. Glob J Health Sci. 2012;4:65–93. doi: 10.5539/gjhs.v4n1p65. [DOI] [PMC free article] [PubMed] [Google Scholar]