Abstract
Mitochondria play key roles in ATP supply, calcium homeostasis, redox balance control and apoptosis, which in neurons are fundamental for neurotransmission and to allow synaptic plasticity. Their functional integrity is maintained by mitostasis, a process that involves mitochondrial transport, anchoring, fusion and fission processes regulated by different signaling pathways but mainly by the peroxisome proliferator-activated receptor-γ coactivator-1α (PGC-1α). PGC-1α also favors Ca2+ homeostasis, reduces oxidative stress, modulates inflammatory processes and mobilizes mitochondria to where they are needed. To achieve their functions, mitochondria are tightly connected to the endoplasmic reticulum (ER) through specialized structures of the ER termed mitochondria-associated membranes (MAMs), which facilitate the communication between these two organelles mainly to aim Ca2+ buffering. Alterations in mitochondrial activity enhance reactive oxygen species (ROS) production, disturbing the physiological metabolism and causing cell damage. Furthermore, cytosolic Ca2+ overload results in an increase in mitochondrial Ca2+, resulting in mitochondrial dysfunction and the induction of mitochondrial permeability transition pore (mPTP) opening, leading to mitochondrial swelling and cell death through apoptosis as demonstrated in several neuropathologies. In summary, mitochondrial homeostasis is critical to maintain neuronal function; in fact, their regulation aims to improve neuronal viability and to protect against aging and neurodegenerative diseases.
Keywords: mitochondria, mitostasis, calcium, oxidative stress, nitric oxide, aging
1. Introduction
The brain is the most energy-demanding organ in the body, consuming up to 20% of the total oxygen supply and up to 20% of total glucose intake [1], especially in the neuropil [2]. This energy is needed for normal cellular functions, but in particular, neurons must restore ionic gradients to allow action potentials, carry out neurotransmission, provide the machinery for synaptic plasticity, and maintain healthy and functional membranes along axons and dendrites.
Adenosine triphosphate (ATP) is mainly produced by glucose metabolism and through the mitochondrial respiratory chain (MRC). Therefore, mitochondria need to be functionally active in soma, axons and dendrites throughout the life of an individual. Axonal transport of mitochondria, and mitochondrial fission and fusion, contribute tomaintaining a functional and healthy pool of mitochondria. These mitochondria are relocated continuously along the neurons depending on the local energy requirements [3]. The complex, dynamic system that maintains and delivers mitochondria is termed mitostasis and it regulates the number, trafficking and protein turnover of mitochondria in each compartment of the neuron [4].
On the other hand, mitochondria participateactively in calcium (Ca2+) homeostasis, a process reviewed in the present work, and this mitochondrial function is fundamental for neuronal activity [5].To achieve this aim, they are physically and functionally linked to the endoplasmic reticulum (ER) by specialized structures, mitochondria-associated membranes (MAMs), which have been proposed to be highly relevant in calcium buffering. They are sites of juxtaposed ER and outer mitochondrial membrane (OMM), which facilitate organelle communication, allowing the regulation of Ca2+ fluxes from ER to mitochondria, among other cellular functions such aslipid synthesis and transport, and glucose metabolism [6]. Ca2+ also regulates mitochondrial functions and itsdyshomeostasisaffects the MRC, triggering free radical production [7]. Reactive oxygen species (ROS) production, Ca2+ uptake and mitochondrial membrane depolarization have been linked to neuronal apoptosis [8]. They disrupt the normal mitochondrial functioningthrough the uncoupling of MRC, compromising energy production [7].
Considering the long life of the neurons, mitostasis is fundamental to maintain healthy and functional neurons even during aging. Here, we present a review of the role of the factors implicated in mitostasis and its relationship with Ca2+ and free radicals in health, aging and neurodegenerative processes.
2. Mitostasis in Neurons
The maintenance and distribution of the mitochondrial reserve is termed mitostasis, which includes mitochondrialtransport, anchoring, fission and fusion. In fact, most of the mitochondria do not exist as small, distinct organelles, but rather form a highly interconnected reticulum with contiguous membranes [9]. This reticulum is highly dynamic with ongoing divisions and reconnections. The balance of fission and fusion determines the length of mitochondria, and it is regulated by stress and nutrient availability [10]. Mitostasis also involves protein reparation or degradation, and the formation of mitochondria-derived vesicles yielding to mitophagy and macroautophagy [4].
In particular, mitochondrial biogenesis requires materials from the cytoplasm and nucleus, since mammalian mitochondria DNA (mtDNA) encodes only 13 proteins [11]. For this reason, mitochondrial biogenesis requires the importation of over 1500 proteins encoded by the nuclear genome [12] and phospholipids for the inner mitochondrial membrane (IMM) and the OMM [13].
2.1. Mitochondrial Trafficking
The location of mitochondria, depending on local energy demands, is critical for polarized cells such as neurons. Interconnected mitochondria are located in neuronal cell soma. However, to enter the axon, a mitochondrion must undergo a fission reaction. This reaction frees it from its mitochondrial reticulum.
Once released, mitochondrial fast anterograde transport is mediated by microtubules [14]. Mitochondrial Rho GTPase 1 and 2 (Miro 1 and 2) serve as Ca2+ sensors that regulate kinesin-mediated mitochondrial motility. Miro 1 and 2 have an outer C-terminal transmembrane domain with GTPase domains, which interact with the trafficking kinesin protein (TRAK)/Milton family of proteins [15,16,17,18,19]. These cargo adaptorsbind to Kinesin-1 anddynein/dynactin, beingcritical in mitochondrial trafficking and its spatial distribution [20]. Kinesin-1 cargoes, often together with dynein, drive mitochondria transport into the axon [18,21], and the dynein/dynactin cargo complextransports mitochondria into dendrites [20,22].
On the other hand, shorter-range mitochondrial transport is actin-dependent anduses the dynein/dynactin complex as actin-mitochondrial anchorage. The cargo Myosin 19 (Myo19) [23] has been suggested as critical for this process [24].
2.2. Mitochondrial Anchoring
Mitochondrial anchoring to inner cell structures is needed to provide the required energy at the right place, as around two-thirds of neuronal mitochondria remain stationary [25]. These pools of mitochondria are mainly located in the soma and in areas with high ATP demand, such as the nodes of Ranvier, axonal presynaptic endings and dendrites [26]. Mitochondria anchoring mechanisms are not fully understood and they seem to involve different proteins depending on the localization of the mitochondria. For instance, in axonal presynaptic endings, activation of adenosine monophosphate-activated protein kinase (AMPK) by synaptic activity leads to myosin VI phosphorylation, ending with mitochondrial recruitment and syntaphilin-mediated anchoring on presynaptic filamentous actin [27]. This process is specific to the stationary mitochondria, not being related to the mitochondria mobility machinery [3,28]. Remarkably, it is an axon exclusive physiological mechanism. On the other hand, axonal mitochondrial anchor mislocalization to dendrites has been associated with multiple sclerosis disease [29].
2.3. Mitochondrial Fission
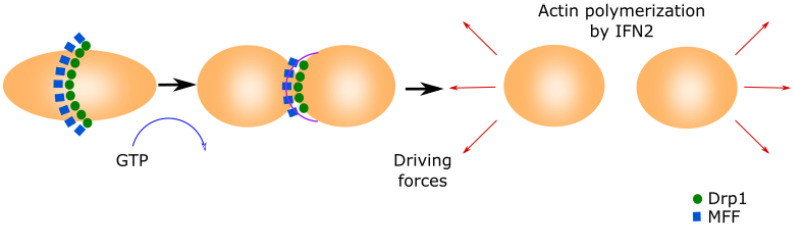
Mitochondrial fission is essential for shaping the mitochondrial network and is required for generating additional mitochondria of the appropriate size for their transport by molecular motors along the cytoskeleton [30] (Figure 1).
Figure 1.
Mitochondrial fission.This process is initiated by MFF forming a ring in the middle of the primary organelle to be divided. Drp1 GTPase translocates to the mitochondria and binds to MFF, inducing a conformational change by the hydrolysis of GTP. This conformational change generates the ring contraction, which starts mitochondrial fission. The reorganization of the cytoskeleton generates the driving forces that separate both new mitochondria.
Mitochondria fission starts when the mitochondrial fission factor (MFF) surrounds the OMM forming a ring [31,32]. Mitochondrial fission 1 (Fis1) and mitochondrial dynamics proteins of 49 and 51 kDa (MID49 and MID51) recruit the cytoplasmic Dynamin-related protein 1 (Drp1) [33,34,35]. Drp1 translocates to the mitochondria and binds to MFF, inducing a conformational change due to its GTPase activity. This conformational change produces the ring contraction that starts mitochondrial fission [33,36]. Cellular cytoskeleton further separates both mitochondria depending on the MAMs. The Inverted Formin 2 protein (INF2) is localized in MAMs and its activation causes actin polymerization, which generates the driven force separating both mitochondria [37].
2.4. Mitochondrial Fusion
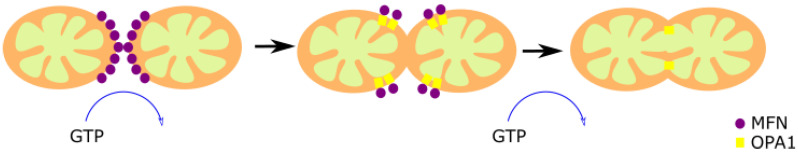
Mitochondrial fusion is a cell protective mechanism [38] based in two different and concomitant processes, the OMM fusion and the IMM fusion (Figure 2).
Figure 2.
Mitochondrial fusion. The fusion of two preexistent mitochondria is a protective mechanism based on the fusion of the OMM and IMM. The OMM fusion is mediated by MFN1 and MFN2, and the fusion of the IMM is mediated by OPA1. First, MFN1 and MFN2 GTPase activity induce the formation of homo- or hetero-oligomeric complexes in the fusion spot. Then, OPA1-mediated GTP hydrolysis promotes the membrane fusion.
The dynamin-associated GTPases Mitofusin proteins 1 and 2 (MFN1 and MFN2) are responsible for the OMM fusion [39,40]. Both GTPases share a high structural and biochemical homology, but they have different roles [41]. MFN1 is found exclusively in the OMM, and allows the contact between the OMM of different mitochondria [42]. MFN2, found in mitochondria and ER, has an anchoring role since it joins the two organelles, forming homotypic and heterotypic complexes with MFN1 [43]. The spiral domains of MFN1 and MFN2 interact, forming homo- or hetero-oligomeric complexes through GTP hydrolysis in the fusion spot [44]. However, there are controversial reports regarding the relevance of this mechanism since it was observed that the loss of MFN-2 increased the ER–mitochondrial juxtaposition [45]. This fact does not contradict that the functionality of mitochondria–ER contacts is affected in MFN2 KO cells, as suggested by the previous observation that Ca2+ transfer from the ER to the mitochondria is altered in these cells [43].
The optic atrophy 1 protein (OPA1) mediates the IMM fusion [46,47]. The long form of the protein (l-OPA1) works as a coordinator of the IMM of both fusing mitochondria. The two membranes fuse through the short isoform (s-OPA1) by its GTPase activity [48]. OPA1 is also associated with the maintenance of the MRC by cristae organization, and the control of apoptosis [49,50,51,52], demonstrating versatility of functions.
2.5. The regulator of Mitochondrial Biogenesis PGC-1α
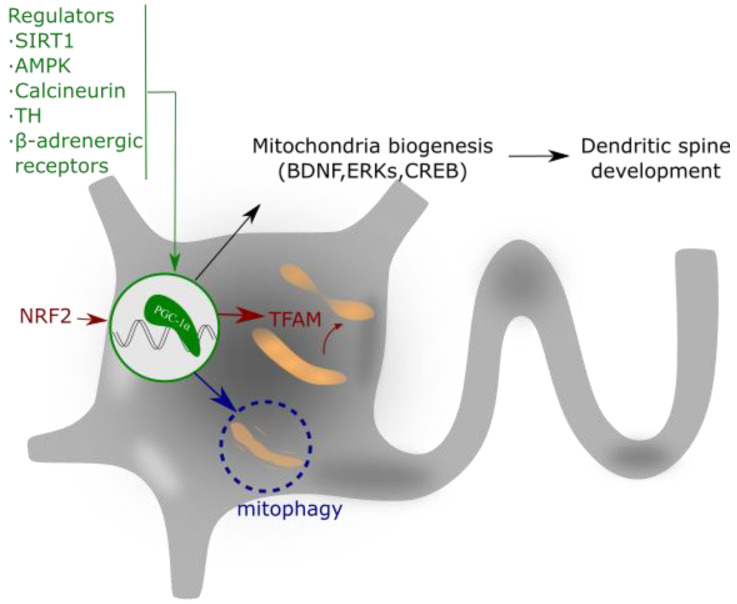
The peroxisome proliferator-activated receptor-γ (PPARγ) coactivator-1 α (PGC-1α) is a member of a transcription coactivator family, composed ofPGC-1α, PGC-1β and PGC-related coactivator (PRC). These proteins play a central role in the regulation of mitochondrial biogenesis and cellular energy metabolism [53] (Figure 3).
Figure 3.
PGC-1α regulates mitochondrial biogenesis and spine growth. Its activity is based on the interaction with NRF that activates to TFAM. This complex regulates mitochondrial gene expression and addresses the requirements of neuronal energy when needed for dendrite activity or growth. PGC-1α expression is regulated by different intracellular signaling pathways, as explained in the text.
The action mechanism of PGC-1α implies its interaction with two nuclear transcription factors, nuclear respiratory factors 1 and 2 (NRF-1 and 2), which activate the mitochondrial transcription factor A (TFAM), a mtDNA-binding protein [54]. TFAM and the cofactor mitochondrial transcription factor B (TFB1M) are essential for mitochondrial gene expression [55]. This molecular pathway promotes the equilibrium in the assembly of some components of the MRC, which ultimately ensures appropriate mitochondrial function, mtDNA replication and apoptosis control [56,57,58].
The expression and/or activity of PGC-1α is regulated by different intracellular signaling pathways such as the PGC-1α regulatory cascade [59], thyroid hormone (TH) [60], sirtuin 1 (SIRT1) [61,62], calcineurin [63], AMPK [64], cyclin-dependent kinases (CDKs) [65], and β-adrenergic signaling [66]. These regulators of PGC-1α aim to coordinate the expression and function of mitochondrial proteins during mitochondrial biogenesis [67]. Additionally, not only transcriptional regulation but also post-translational modifications allow the control of the PGC-1α activity. For example, PGC-1α phosphorylation by p38 mitogen-activated protein kinase alpha (p38α) enhances its activity [68], and PGC-1α acetylation suppresses its activity [61].
PGC-1α and mitochondrial biogenesis play important roles in the formation and maintenance of dendritic spines and synapses in hippocampal neurons [69]. In this context, PGC-1α also controls the synthesis of the Brain-Derived Neurotrophic Factor (BDNF) [70] and the activity of Extracellular Signal-Regulated Kinases (ERKs) [71]. BNDF has been widely reported in the literature as a neuroprotective agent produced by physical exercise [72] and, interestingly, exercise induces the upregulation of PGC-1α expression and increases mitochondrial mass within the brain [73]. In addition to its role in mitochondrial biogenesis, PGC-1α also regulates apoptosis and the ROS detoxification system [74].
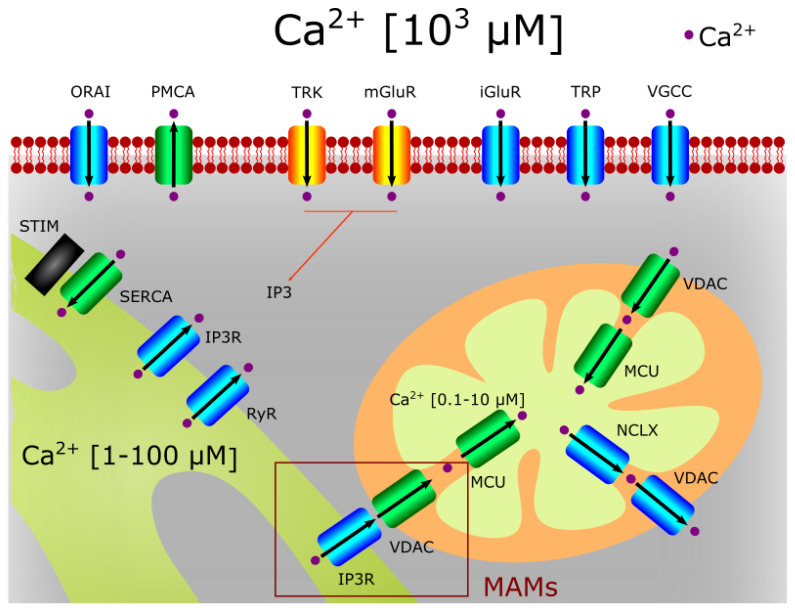
3. The Role of Mitochondria in Calcium Homeostasis
Mitochondria regulate the intracellular Ca2+ in tight association with the ER, but mitochondrial Ca2+ also controls mitostasis and even neuronal fate (Figure 4).
Figure 4.
Ca2+ homeostasis in neurons. The entrance of extracellular Ca2+ into neurons is due to the direct activation of neurotransmitter and neurotrophin receptors (such as NMDAR and TRK) and cationic channels (such as TRPs or voltage activated Ca2+ channels). The VDAC channel can import or export Ca2+ in the mitochondria when associated to MCU or NCLX, respectively. IP3R and VDAC channels found in MAMs can also transport Ca2+ from the ER to the mitochondria. The Ca2+ extrusion to the extracellular medium is mediated by ATPases (i.e., PMCA).
3.1. Calcium Entrance to Mitochondria
Ca2+ entry from the cytosol into the mitochondria requires its flow through both the OMM and the IMM. The first step is carried out by the voltage-dependent anion channel 1 (VDAC1), the most abundant protein at the OMM. VDAC1 is a channel that allows the entry and exit of multiple metabolites and ions. It shows two voltage-dependent conductance states [75]. At the high conductance state (at low potentials of −20 to +20 mV), it is permeable even to large metabolites and cations, such as acetylcholine, dopamine, glutamate and ATP [76,77]. At the low conductance state, at higher positive or negative potentials (>30–60 mV), the selective permeability shifts to small cations, including Ca2+ [78,79,80].
The transport of Ca2+ into the mitochondrial matrix from the intermembrane space is mainly mediated by the membrane Ca2+ uniporter (MCU). This protein constitutes a heteromeric channel complex at the IMM along with mitochondrial calcium uniporter dominant negative subunit beta (MCUb), which is a paralog of MCU acting as dominant negative subunit [81]. Essential MCU regulator (EMRE), mitochondrial calcium uptake 1 and 2 (MICU1,2) and MCU regulator 1 (MCUR1) have multiple functions as scaffold factors for the MCU complex function, promoting mitochondrial bioenergetics and the activation of the solute carrier 25A23 (SLC25A23) [82,83,84,85]. The efficiency of Ca2+ influx through this channel complex in the mitochondria depends on the highly negative mitochondrial membrane potential (ΔΨm), produced by the pumping of protons across the IMM into the intermembrane space by complexes I, III, and IV of the MRC. Such ΔΨm allows ATP synthesis bycomplex V (ATP synthase) and determines the electrochemical driving force for Ca2+ movement. MCU is the pore-forming subunit, whose activity is regulated by MCUb (a paralog of MCU acting as dominant negative subunit) [81], MICU1 and MICU2 (as Ca2+-dependent modulators), and MCUR1 and SLC25A23 (as positive regulators). EMRE has been shown to be essential for MCU-mediated mitochondrial Ca2+ uptake [86]. Thus, EMRE is considered as the scaffolding protein-mediating interaction of MICU1 and MICU2 with MCU [87]. Through their EF-hand Ca2+-binding motifs, MICU1 and MICU2 sense the Ca2+ at the intermembrane space to modulate pore gating [88,89]. At resting low Ca2+ levels, they inhibit MCU channel activity [90,91,92]. Once Ca2+ rises above 1–2 μM, MICU1 and MICU2 drive channel gating, with MICU1 working as a positive regulator, which promotes the MCU open conformation [88,93,94], and MICU2 slowing channel activation. It results in the limitation of the mitochondrial Ca2+ uptake for the proper control of Ca2+ homeostasis [92,94]. Besides, MICU1 and MICU2 have been reported to form heterodimers that respond to sub-micromolar Ca2+ in a steep co-operativity manner, thus defining MCU threshold and functioning as ON/OFF switches for mitochondrial Ca2+ uptake [90]. The enhancement of MCU channel activity induced by MCUR1 seems to be related with its role as a scaffold factor required for the correct assembly of the whole uniporter complex [95].
Steady-state levels of mitochondrial Ca2+ depend on the dynamic balance between this MCU-mediated Ca2+ influx and Ca2+ efflux through the Li+-permeable Na+/Ca2+ exchanger (NCLX), also located at the IMM [96].
In this way, the mitochondrial network regulates the local Ca2+ concentrations at cellular microdomains where Ca2+ signaling is intense, in particular, at the close vicinity of the ER and the plasma membrane. In the plasma membrane they act as intracellular Ca2+ buffers, since they are located in the proximity of Ca2+ channels. In the ER or the sarcoendoplasmic reticulum, mitochondria regulate the diffusion of Ca2+ waves through the cytosol [97].
Due to the essential role of Ca2+ in cellular homeostasis, its flow is tightly regulated. This process is cell specific through the differential expression of multiple Ca2+ channels and pumps both at the plasma membrane and intracellular organelles, such as the ER. The Ca2+-buffering function of mitochondria in cytosolic signaling microdomains strongly controls the regulation of many of these Ca2+ pathways, because their activity is allosterically modulated by cytosolic Ca2+. This is the case of the store-operated Ca2+ channel (SOC) [98], ryanodine receptors (RyR) [99], L-type Ca2+ channels [100] or transient receptor potential (TRP) channels [101].
3.2. Calcium Functions in Mitochondria
Inside the mitochondria, Ca2+ plays a crucial role by allowing the regulation of the metabolic energy supply. It works as an indirect enhancer of three proton pumps in the MRC: complexes I, III, and IV [102,103,104]. Besides, Ca2+ also upregulates the ATP synthase itself [105,106]. Moreover, mitochondrial Ca2+ has been shown to inhibit mitochondrial elimination of reactive oxygen species (ROS) in a dose-dependent manner from 1 to 100 µM. This concentration range makes this mechanism relevant in both physiology and pathology [107].
Furthermore, calcium-dependent activation of CAMKIIβ is linked to mitochondrial biogenesis in neurons. This protein is able to activate AMPK, which is one of the main regulators of PGC1α [108].
Finally, both cytosolic Ca2+ overload or the imbalance between mitochondrial Ca2+ uptake and removal can lead to the toxic accumulation of Ca2+ in mitochondria. This often results in the opening of the mitochondrial permeability transition pore (mPTP), which in turn leads to mitochondrial swelling and dysfunction, and finally to cell death through apoptosis or necrosis in several neuropathologies [109,110,111,112,113,114,115], such asAlzheimer’s disease (AD) and hypoxic-ischemic brain injury.
3.3. The Role of the MAMs
Mitochondria do not function as isolated structures; in fact, up to a 5–20% of the mitochondrial surface is likely in close contact with the ER [116,117]. These sites are physical/functional platformsinvolved in different fundamental cellular processes. The ER–mitochondrial contacts do not occur randomly, but on specific domains termed MAMs, which have a well-defined structure with several proteins present at both the OMM and the ER membrane [118]. MAMs allow a better transport of Ca2+ to mitochondria and regulate spikes of activity through Ca2+ transport from the ER to the mitochondria [119].The alteration of MAMs yields to the lack of Ca2+ homeostasis and mitochondrial biogenesis impairment [97,116,120,121].
The core of the MAMs is a conserved multiprotein complex formed by the IP3Rs (ER), which interacts with the cytosolic fraction of the mitochondrial chaperone glucose-regulated protein 75 (Grp75) and the VDAC1 [122]. It works as an anchor but also allows Ca2+ transfer and favors phospholipid exchange between the two organelles. Other proteins have been proposed to play a key role in MAMs formation and function such as MFN2, an ER–mitochondria anchor [43,123]. The vesicle-associated membrane protein-B (VAPB) and the tyrosine phosphatase-interacting protein-51 (PTPIP51), located at the ER and mitochondria, respectively, have also been described as scaffold-forming dimers [124,125].
In the same way, the phosphofurin acidic cluster sorting protein 2 (PACS-2), which seems to constitute part of the MAMs, also acts as another regulatory signaling protein [126]. Even while the role of PACS-2 as a ER–mitochondria tether scaffold lacks the necessary evidence, the depletion of this protein causes mitochondrial disconnection from the ER [126,127]. It has been proposed that two distinct domains are present in MAMs that differ in their lipid content, function and control of glucose homeostasis [128,129,130,131].
Additionally, it must be notedthat the proteolytic processing of some of the MAMs complexes also act as signaling mechanisms, being able to drive critical processes such as cell death. That is the case of the ER, B-cell receptor-associated protein 31 (BAP31) and Fis1 complex since a sustained/increased efflux of reticular Ca2+ to the mitochondria induces the cleavage of the BAP31 leading to neuronal apoptosis [132].
3.4. The Role of Calcium in mPTP Opening
Ca2+ plays a crucial role in apoptosis either in the extrinsic pathway as a second messenger or in the intrinsic pathway through mitochondrial-mediated death. In the intrinsic pathway, the high mitochondrial Ca2+ load opens the mPTP, located in the IMM. The opening of mPTP causes reduction of the ΔΨm, dysfunction of MRC and the release of the cytochrome C (CytC) [133,134,135,136,137]. CytC leads to the formation of a complex with the apoptosis protease-activating factor-1 (APAF-1), that activates the caspase cascade to finally induce cell death [138]. This process is further enhanced by the production of ROS and yields to a lower production of ATP [139]. Moreover, CytC favors mitophagy and impairs mitostasis [140]. The pathological relevance of this mechanism is shown in several neurodegenerative diseases, since an increase in mPTP activity has been reported in AD [136,137], amyotrophic lateral sclerosis (ALS) [141,142,143], Parkinson’s disease (PD) [144], and Huntington’s disease (HD) [145,146]. On the other hand, the opening of the mPTP and mitochondrial dysfunction in mitochondrial diseases promote the production of ROS that deteriorate their own repair and function dynamics, causing a vicious circle that aggravates this pathological process [139].
4. ROS Production by Mitochondria
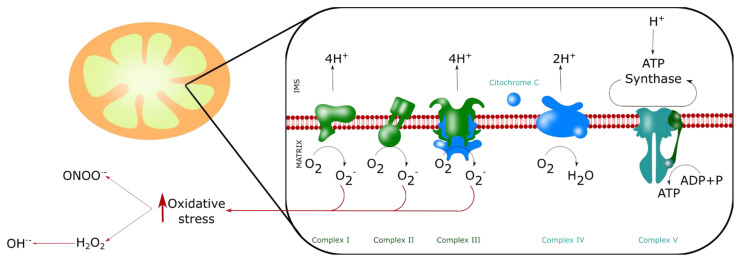
Mitochondria produce ROS, mainly superoxide anion (O2·−) by the MRC, and indirectly hydrogen peroxide (H2O2) and hydroxyl radical (OH·−) [147] (Figure 5). However, the role of ROS cannot be misunderstood. ROS constitute a cellular signaling system, and neuronal function depends on the subtle control of ROS levels. ROS have a direct influence on the intracellular Ca2+ levels since they can modulate the activity of several Ca2+ channels including IP3Rs, sarco/endoplasmic reticulum Ca2+-ATPase (SERCA) and MCU [148,149,150]. Fine-tuning redox reactions and ion signaling pathways are fundamental for proper neuronal function. Therefore, the antioxidant enzymes superoxide dismutase (SOD) and catalase (CAT), and the glutathione system are important for the maintenance of the normal neuronal redox state and, consequently, neurotransmission and cognitive processes [151,152,153]. In fact, in an aging rat animal model, Cu/Zn SOD (SOD1) overexpression induces an altered redox status and a decrease in N-methyl-D-aspartate receptor (NMDAR) synaptic function, glutathione peroxidase (GPx) activity and glutathione (GSH) levels. SOD1 overexpression also impaired long-term potentiation (LTP) followed by impaired learning.
Figure 5.
ROS production by mitochondria. Mitochondria produce ROS, mainly superoxide anion O2·− by the MRC (at the complexes I, II and III), and indirectly hydroxyl radical (OH·), hydrogen peroxide (H2O2) andperoxynitrite (ONOO−). These four molecules are the main reactive agents inducing nitro-oxidative stress.
On the other hand, aging and neurodegenerative diseases are characterized by an increase in ROS generation, with the consequent alteration of the ΔΨm, Ca2+ dyshomeostasis and decreased ATP production. Mitochondrial fission in neurons can be initiated by ROS, where MFN2 plays a protective role, but Drp1-mediated fission increases ROS production [154]. Overall, in vitro experiments demonstrated that cells exposed to ROS have altered morphology of the mitochondrial network, and this morphological alteration depends on the amount of ROS and the duration of the experimental challenge [155]. It has also been demonstrated that the overproduction of ROS can induce further ROS production, generating a permanent pro-oxidative state. This state leads tonucleic acid, protein and lipid oxidation, having a determinant role in cellular fate and neurodegenerative diseases [147].
5. Nitric Oxide and Mitochondria
Nitric oxide (NO) has a regulatory effect on mitochondrial function and mitostasis. Mitochondria produce their own NO by a constitutive mitochondrial NO-synthase (mtNOS; an isoform of the neuronal NOS), whose activation depends on Ca2+ [156,157,158]. The role of mtNOS has a special significance, because this enzyme produces the vast majority of cellular NO, much more than all the other NOS together [159]. Therefore, mtNOS plays key roles in health and also age-related metabolic alterations [160].
NO favors mitochondrial biogenesis inducing mtDNA replication and PGC-1α, NRF-1 and TFAM expression [161], but it also regulates mitochondrial functions. NO decreases the activity of the MRC through the inhibition of CytC. Thus, mtNOS has a function as a physiological modulator of ATP production [162,163]. NO in high concentrations activates the mPTP [164] leading to apoptosis;however, it could even be protective, since it has been demonstrated that mtNOS has an antiapoptotic role through S-nitrozation of caspase 3, which renders it inactive [165].
On the other hand, NO can react with O2·−, generating peroxynitrite (ONOO−) [166,167]. Peroxynitrite is a highly reactive anion that nitrates proteins and lipids, which negatively impacts their physiological functions, especially in neurodegenerative diseases [156,168,169].
6. Mitochondria in Aging and Neurodegeneration
Aging is defined as a progressive time-related accumulation of changes responsible for or at least involved in an increased susceptibility to disease and death. In fact, mitostasis imbalance leads to the development of cognitive decline [170,171] and neurodegeneration [157,172,173].
6.1. Physiological Aging
During aging, neural activity is less localized in certain brain regions, notably in the prefrontal cortex, while performing executive-function related tasks [174,175]. These observations suggest that reductions in higher-order brain functions are accompanied by stereotypical, structural and neurophysiological changes in the brain, with variable degrees of cognitive decline that are significantly induced by aging in the absence of disease [176,177]. This reduction in brain metabolic activity during aging has been proposed to be due to mitochondrial dysfunction, which produces impaired energy supply, imbalanced Ca2+ buffering, increased production of ROS, DNA alteration, opening of the mPTP and apoptosis. All these factors plus the dysregulation of different proteins (Table 1) contribute to the progressive decline of long-lived neurons linked to aging, which is exacerbated in neurodegenerative diseases [178].
Table 1.
Proteins involved in mitochondrial dysfunction in aging.
| Molecule | Function | Ref. |
|---|---|---|
| DNA polymerase γ (Polγ) | Mitochondrial DNA polymerase | [189] |
| Hsp70/Hsp90 molecular chaperones | Protection and interaction with protein import receptor Tom70 | [190] |
| Lon Protease | Involved in drug-induced mitochondrial dysfunction and endoplasmic reticulum stress | [191] |
| Transcription Factor ATF5 | Mitochondrial unfolded protein response (mtUPR) | [192] |
| Estrogen receptor | Involved in mtUPR | [193] |
| α-ketoglutarate dehydrogenase, and pyruvate dehydrogenase | Mitochondrial respiration | [194] |
| DRP1 | Replication machinery | [195] |
In particular, mitochondrial dysfunction is an early and common pathological feature of aging in which the activities of complexes I, III, and IV are decreased [179,180,181]. Impairment in mitochondrial function occurs when the activity of complex IV of the MRC is reduced. Simultaneously, complex V, which metabolizes ADP to form ATP, is functionally altered and damaged by oxidation. Therefore, VDAC in the OMM is also damaged by oxidative stress, and these changes contribute to the formation of the mPTP, significantly enhanced in neurodegenerative processes [182,183,184].
According to the mitochondrial theory of aging, the accumulation of mutations in mtDNA due to continuous exposure to ROS is a key factor in cellular aging [185]. DNA alterations are due to the susceptibility of mtDNA to ROS-induced strand breaks and point or deletion mutations. In some cases, the mtDNA repair system fails and mtDNA mutations can be transmitted to and accumulated in daughter mitochondria [186,187].
Regarding Ca2+ homeostasis during physiological aging, there is an increase in intracellular Ca2+ due to the increased activity of L- and N-type voltage-gated Ca2+ channels (VGCC), and the enhanced age-dependent expression of the N-type [188] in the plasmatic membrane. This increase in Ca2+ load also contributes to mPTP formation, mitochondrial dysfunction and apoptosis.
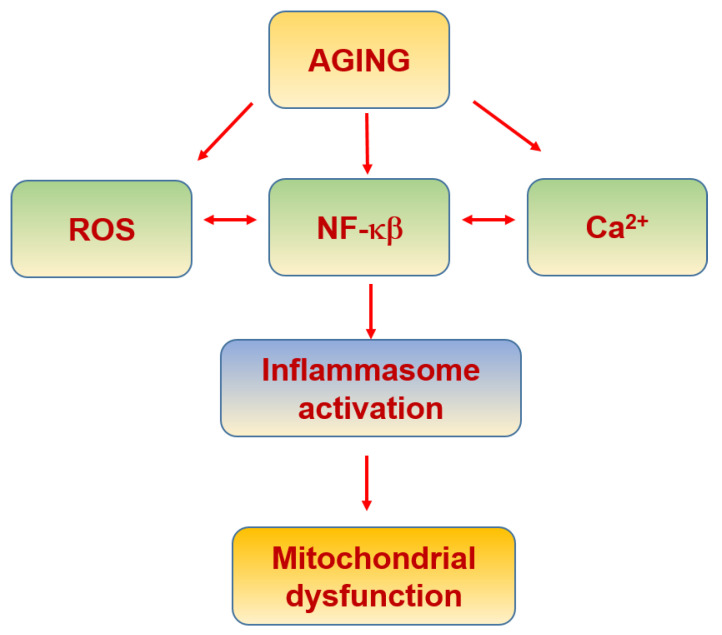
6.2. Inflammaging
A lowgrade of chronic activation of the inflammatory response associated with aging, termed inflammaging, yields to an inflammatory status that worsens or contributes to the onset of age-associated pathologies [196]. In fact, NF-κB, the master regulator of the inflammatory cascade within cells, increases its activity with aging, being linked to a wide spectrum of age-related disorders [197,198] (Figure 6). The activation of NF-κB promotes the expression of interleukin 1β (IL-1ß) and interleukin 18 (IL-18), two major products of the inflammasome [199,200]. Moreover, NF-κB activation also promotes tumor necrosis factor α (TNF-α) and interleukin 6 (IL-6) expression [200], which contribute to mitochondrial dysfunction [199].
Figure 6.
Inflammaging and mitochondria.
Inflammasomes are multiprotein signaling patterns responsible for the maturation of pro-IL-1β and pro-IL-18. Most inflammasomes consist of an upstream sensor, in most cases an adaptor protein (ASC), and inflammatory caspases such as caspase-1. Upon activation, sensor proteins oligomerize with adaptor proteins, forming large complexes called specks (ASC specks) [201]. There is a close relationship between the inflammasome and mitophagy. Firstly, it acts as a protective mechanism. In fact, the inflammasome induces the expression of PGC-1α [202]. However, once dysregulated it becomes a pathological process that aggravates mitochondrial damage [202] (Table 2).
Table 2.
Proteins involved in mitochondrial dysfunction in imflammaging.
| Molecule | Function | Ref. |
|---|---|---|
| Cyclic GMP-AMP (cGAS) and the cyclic GMP-AMP receptor stimulator of interferon genes (STING), (cGAS-STING) | Inflammatory response | [212] |
| Mitochondria-associated viral sensor (MAVS) | Mitochondrial adaptor | [213] |
| Retinoic acid-inducible gene I (RIG-I) | RNA helicase | [214] |
| NOD-like receptor family member X1 (NLRX1) | Regulators of MAVS function | [215] |
| TNF-receptor-associated factor (TRAF) | Type I IFN production | [216] |
| Succinate dehydrogenase | Inflammatory response | [217] |
| mtDNA | Dysfunctionby oxidation | [218] |
| Cardiolipin | Nlrp3 activation | [219] |
| N-formyl peptides | Proinflammatory signalling | [220] |
| TFAM transcription factor | Inflammatory response | [221] |
The inflammasome is modulated by the MAMs [203]. The nucleotide-binding oligomerization domain-like receptor 3 (NOD-like receptor 3 or NLRP3), an inflammasome component, when activated binds to the ER associated with caspase-1 [204,205], promoting its activation, which results in proteolytic activation of IL-1ß and IL-18 [206]. Significantly, NLRP3 is activated by ROS, suggesting inflammasome activation originates in the mitochondria [200,206]. On the other hand, when VDAC1 expression is decreased, the entry of mitochondrial Ca2+ is affected, and inflammasome activity is reduced [204]. Accordingly, MAMs, through the exchange of ER and mitochondrial content, including Ca2+ and ROS, among others, constitute a highly complex regulatory mechanism able to coordinate several cellular processes, including the inflammatory response [207,208,209].
In fact, the study of pathological conditions with high levels of inflammatory components suggests that age-related disorders such as neurodegenerative diseases and aging itself could be controlled by the modulation of the inflammatory mechanisms [198,210,211].
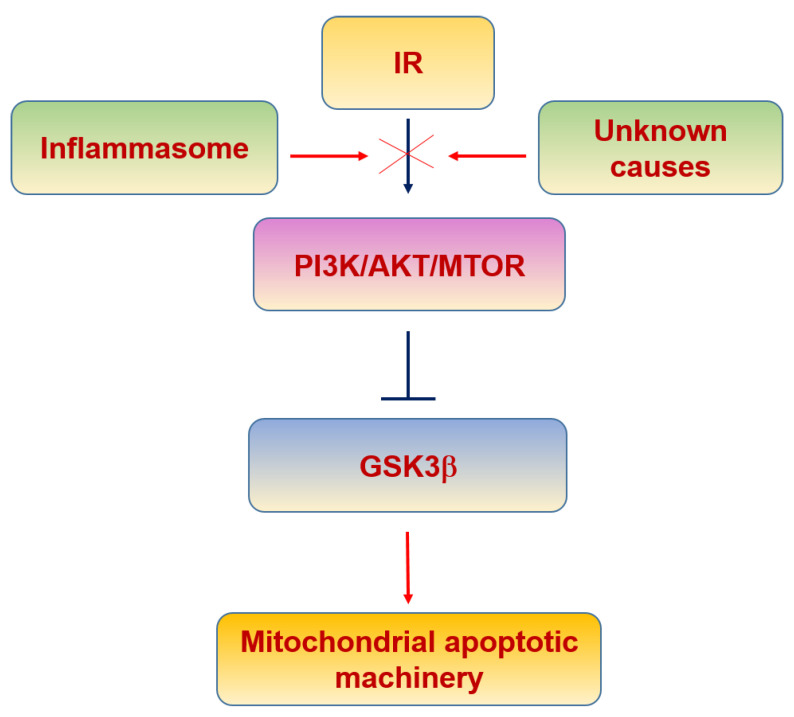
6.3. Insulin Resistance
Insulin receptor (IR) is found in different brain areas, particularly in the hypothalamus, cortex and hippocampus [222]. It has been demonstrated that insulin enhances cognition and memory [223], modulates GABAergic activity in the cerebellum [224], protects against apoptosis [225], and regulates mitochondrial function [226,227].
Type 2 diabetes (T2D) is a pathological condition characterized by hyperglycemia, hyperinsulinemia and insulin resistance, and whose onset occurs in late adulthood and aging affecting millions of people worldwide. The pathophysiological relevance of T2D is also highlighted in brain aging, considering that T2D has been proposed as a risk factor for the development of AD. This relationship has ledto some authors terming AD as Type 3 Diabetes, since epidemiological studies have found insulin resistance to bea prodromal feature in AD patients [228,229]. Interestingly, oligomeric amyloid β-peptide (Aβ) binds to IR, impairing its function [230].
There is evidence linking insulin signaling and mitochondrial function. IR phosphorylation leads to brain mitochondrial biogenesis since it is able to activate the PI3K/AKT/mTOR pathway [231,232,233] (Figure 7). Moreover, the inhibition of the IR intracellular signaling has been shown to decrease mTOR signaling and PGC-1α levels [234,235], impairing mitochondrial biogenesis.
Figure 7.
Insulin resistance and mitochondria.
Classically, glycogen synthase kinase 3β (GSK3β) is inhibited by insulin signaling [236]. It is a neuronal protective mechanism induced by insulin, since GSK3β plays key roles in activating apoptosis by the induction of the mPTP, mitochondrial swelling, ΔΨm loss and CytC release [237,238]. Moreover, oxidative stress increases GSK3β activity and induces its translocation into mitochondria in a kinase activity-dependent manner, where the N-terminal domain of GSK3β may function as a mitochondrial targeting sequence [239]. These data suggest that GSK3β in mitochondria is a regulator of the mPTP opening, yielding to apoptosis. In fact, the inactivation of mitochondrial GSK3β is associated with suppression of mPTP opening [240,241]. Given that insulin signaling inhibits GSK3β, the lack of the proper intracellular activity mediated by PI3K/AKT suggests that GSK3β would play a deleterious role in neurons after the onset of insulin resistance.
The role of inflammaging [196] in insulin resistance can be relevant since pro-inflammatory cytokines activate IkB kinase (IKK) and c-Jun N-terminal kinase (JNK), which inhibit insulin signaling by phosphorylating the IR at serine-302 (pS302) and serine-307 (pS307), instead of its normal phosphorylating sites at tyrosine residues [242,243]. In addition, these cytokines also activate the suppressor cytokine signaling (SOCS) protein that binds and blocks the phosphorylated IR [244,245], contributing to mitochondrial dysfunction and triggering ROS production [244] (Table 3).
Table 3.
Proteins involved in mitochondrial dysfunction in insulin resistance.
| Molecule | Function | Ref. |
|---|---|---|
| NADH:O2 oxidoreductase | Oxidoreductase activity | [246] |
| NADH dehydrogenase NDUFB8, succinate dehydrogenase SDHB and COX4I1 | Encoding a complex I accessory subunit to reducemitochondrial activity | [247] |
| Nitric oxide (NO) | Mitochondrial biogenesis at the transcriptional level through activation of cGMP and PGC1α | [161] |
| Hydrogen sulfide (H2S) | Preserves mitochondrial function via increased AKT phosphorylation, increased nuclear localization of NRF1/2, and increased mitochondrial biogenesis | [248] |
| Estrogen 17beta-estradiol | Transcription of nuclear respiratory factor-1 and increases mitocondrial biogenesis. | [249] |
| FOXO 1 | Mitochondrial function | [250] |
| PPARγ | Glucose metabolism and regulation of inflammatory response | [251] |
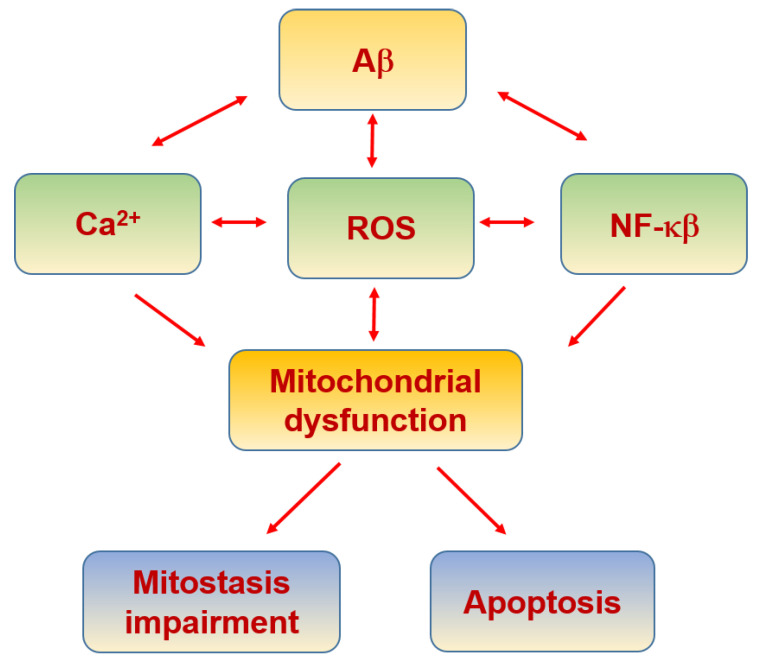
6.4. Alzheimer’s Disease
AD is characterized by the extracellular accumulation of Aβ misfolded into β-sheet in the brain [252,253,254]. Remarkably, nitro-oxidative stress is linked to AD as an etiogenic factor [137,255,256,257,258,259] (Table 4), which is tightly associated with mitochondrial dysfunction (Figure 8). In fact, there is increasing evidence that mitochondrial dysfunction is a key process in the onset and progression of AD [137,260,261]. Mitochondrial dysfunction and axonal degeneration are some of the first pathological characteristics of mild cognitive impairment (MCI), a clinical state that frequently precedes AD [262,263].
Table 4.
Proteins involved in mitochondrial dysfunction in Alzheimer’s disease.
| Molecule | Function | Ref. |
|---|---|---|
| Cytochrome c oxidase and mitochondrial F1F0-ATPase (ATP synthase) | MRC | [297] |
| ERK | Oxidative stress-mediated ERK signal | [298] |
| Amyloid beta (Aβ) binding alcohol dehydrogenase (ABAD) | Promotes Aβ-mediated mitochondrial a dysfunction | [299] |
| mtNADH dehydrogenase 1 (mt-Nd1) |
MRC | [300] |
| OPA1, Mfn1, Mfn2, DRP1 and Fis1 |
Mitochondrial fusion | [269] |
| MT-ND2 and MT-ND5 | MRC | [301] |
Figure 8.
Alzheimer’s disease and mitochondria.
It has been demonstrated in samples from AD patients (at the early and late stages of AD) that complex I mitochondrial genes are downregulated. Increased expression of mtRNAs encoding complex III and IV proteins suggests a response to the increased energy demand [264,265,266]. Similar results have been found in an AD transgenic mouse model [267]. Interestingly, cytoplasmic hybrids (cybrid) derived from MCI and AD patients have higher ADP/ATP and lower nicotinamide adenine dinucleotide (NAD+/NADH) ratios [268].
With respect to mitochondrial biogenesis, postmortem studies with samples from AD patients showed an increase in the expression of Drp1, Fis1 and the mitochondrial matrix protein cyclophilin D (CypD). In contrast, expression of MFN1,2, OPA1 and Translocase of the OMM 40 (TOMM 40) were diminished. Aβ oligomers interact with Drp1, and this interaction increases as the disease progresses, leading to mitochondrial fragmentation, abnormal mitostasis and synaptic damage [269]. Moreover, presenilin 2 (PS2), part of the γ-secretase complex that produces Aβ by the cleavage at the C-terminus, has been shown to increase ER–mitochondria tethering by binding and sequestering MFN2 [123,270,271], therefore, affecting mitochondrial biogenesis.
Sirtuins (SIRT), in particular SIRT1, form a complex with PGC-1α transcriptional complex related with AD pathophysiology. It has been demonstrated that modest fasting reduces BACE1, the enzyme that cleavages the N-term of the amyloid precursor protein to produce Aβ, but increases PGC-1α expression and activity [272]. It is a unique, non-canonical mechanism by which SIRT1-PGC-1α activity induces transcriptional modulation in neurons in response to metabolic challenges reducing the Aβ load. Regarding mitochondria, SIRT1 overexpression protects against Aβ damages at the level of synaptic contacts, dendritic branching and mitochondrial morphology [273]. Furthermore, clusters of SIRT3 protein substrates have been identified in mitochondria, thereby implicating SIRT3 as a major mitochondrial SIRT involved in protecting mitochondrial integrity and energy metabolism under stress conditions. In fact, theloss of this protein has been found to accelerate brain neurodegeneration challenged in excitotoxicity [274,275].
Regarding the neuroprotective Wnt signaling, the activation of the β-catenin-independent pathway by Wnt5a ligand results in the modulation of mitostasis, preventing the changes induced by Aβ in mitochondrial fission–fusion dynamics and modulating the Aβ-induced increase in antiapoptotic Bcl-2 mitochondrial exposure [276]. The activation of the β-catenin-dependent pathway by the Wnt3a ligand has been demonstrated to inhibit the mPTP opening induced by Aβ [277]. On the other hand, the Wnt-induced signaling protein 3 (WISP3/CCN6) has also been related with the appropriate functioning of the mitochondria [278]. Indeed, there are increased mitochondrial ROS and Ca2+ levels in WISP3-depleted cells [279]. These findings suggest that the activation of Wnt pathways prevents mPTP opening and the mechanisms implied in this activity involve the inhibition of mitochondrial GSK3β and/or the modulation of mitochondrial hexokinase II (HKII) levels and activity [280].
Aβ also induces an increase in intracellular Ca2+ by the interaction with L/P/Q-types VGCC [281], NMDAR [282], RyR [283,284] and indirectly by other mechanisms [285,286]. Interestingly, some of the familial forms of AD are due to PS1 mutations which do notaffect Aβ production but rather increase the Ca2+ leak from the ER to the cytoplasm, highlighting the role of Ca2+ in neuronal apoptosis [287]. Moreover, it has been demonstrated that Aβ increases ER–mitochondria coupling and the Ca2+ transfer from the ER to mitochondria [127,288]. This increase in intracellular Ca2+ leads to mitochondrial dysfunction and initiation of apoptosis. Likely, the loss of Ca2+ regulation by the action of Aβ is one of the main causes of the increased production of free radicals and peroxynitrite formation that induces the nitrotyrosination of proteins in AD [168,169,289,290,291].
On the other hand, mitochondrial analysis from AD patient samples showed a significant decrease in mitochondria number in vulnerable neurons that also showed oxidative damage and nitrotyrosination [292,293]. These neurons contained increased levels of mitochondrial degradation products, suggesting either an increased turnover of mitochondria via autophagy or reduced proteolytic turnover leading to accumulation of mtDNA and mitochondrial proteins [292,293]. Interestingly, base excision repair (BER) is one of the most active DNA repair pathways in cells, correcting chromosomal and mtDNA damage from oxidation. It is a process that occurs under conditions of oxidative stress, which may lead to double-strand breaks and induce apoptosis [294]. BER deficiency and polymorphisms have been associated with the development of neurodegenerative diseases, such as AD and ALS, due to the reduction in DNA repairment [295,296].
6.5. Parkinson’s Disease
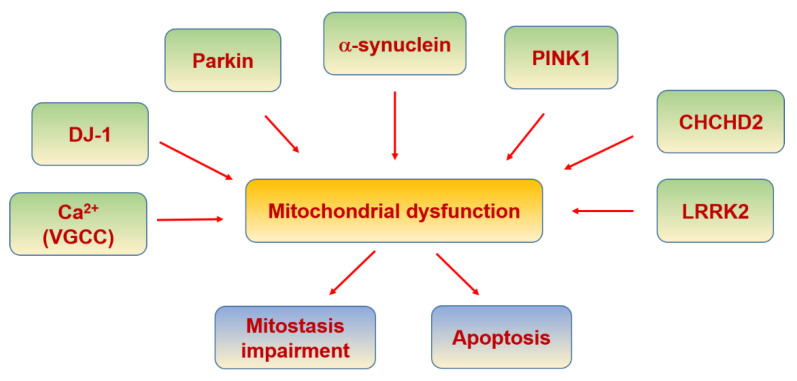
PD is a progressive neurodegenerative disease characterized by the pathological loss of dopaminergic neurons in the substantia nigra pars compacta (SNPC) [302]. Mitochondrial dysfunction has been associated with the pathogenesis of PD since drug abusers were accidentally exposed to 1-methyl4-phenyl-1,2,3,4-tetrahydropyridine (MPTP), which induced acute parkinsonian syndrome due to a metabolite of MPTP inhibiting complex I in the MRC resulting in neuronal death [303]. Since this discovery, further support for the link between mitochondrial defects and PD has been revealed due to genetic factors inducing familial PD such as Parkin, PTEN-induced kinase 1 (PINK1), DJ-1, alpha-synuclein, leucine-rich repeat kinase 2 (LRRK2) and coiled-coil-helix-coiled-coil-helix domain-containing 2 (CHCHD2) (Table 5), which are involved in the function and turnover of mitochondria, impaired mitochondrial dynamics and function in the pathogenesis of PD [304,305] (Figure 9).
Table 5.
Proteins involved in mitochondrial dysfunction in Parkinson disease.
| Molecule | Function | Ref. |
|---|---|---|
| MITOL/MARCH5 | Recruitment to dysfunctional mitochondria | [319] |
| p97 (AAA + ATPase) | Degradation of ubiquitinated Mfn1 | [320] |
| Tim23 complex | Translocation of the positively charged MTS across the IMM | [321] |
| HTRA2/Omi protease | Regulated by PINK 1 | [322] |
| TRAP1 | Regulated by PINK 1 in IMS | [323] |
| complex I subunit NDUFA10 | Regulated by PINK 1 in IMM | [324] |
| PINK1/Parkin | Mutated PINK1 activates Parkin causing mitophagy | [325] |
| PGC-1α | Blocked by mutated Parkin | [308] |
| L- and N-type VGCC | Increase of cytosolic calcium | [310] |
| α-synuclein | MAMs disruption and complex I from MRC inhibition when it is mutated | [312,314] |
| DJ-1 | Oxidative stress sensor and neuroprotective | [326] |
| LRRK2 | Its mutation reduces mitophagy through its disrupted interaction with Miro and a blockade of PINK1/Parkin-dependent mitophagy. | [317,327] |
| CHCHD2 | Regulation of complex IV activity | [318] |
Figure 9.
Parkinson’s disease and mitochondria.
The ubiquitin ligase, Parkin and the mitochondrial kinase PINK1 control the autophagic clearance of defective mitochondria. DJ-1 maintains mitochondrial function in response to oxidative stress [306,307]. Furthermore, PGC-1α, the master regulator of mitochondrial biogenesis and oxidative stress resistance, has been shown to be blocked in familial PD with Parkin mutation [308]. Consistently, the activation of PGC-1α has showed a protective role in dopaminergic neurons when α-synuclein is mutated [306,309].
In PD there is an increase in intracellular Ca2+ caused by L- and N-type VGCC, which can cause saturation of mitochondrial buffering capacity and eventually apoptosis [310]. Ca2+ overload may force the opening of mPTP, leading to retrograde electron flux through the MRC, resulting in increased ROS production, release of Cyt C, and activation of apoptosis [311]. As commented before, MAM allows Ca2+ to be funneled from the ER to the mitochondria via the complex formed by IP3R, VDAC and GRP75, and the activity of this complex is disrupted by α-synuclein [312]. Mutations in α-synuclein also reduce the binding to MAM and increase mitochondrial fragmentation, demonstrating its regulatory role in mitochondrial morphology [313]. Moreover, α-synuclein has been found to influence mitochondrial structure and function, inhibiting complex I from the MRC [314].
Parkin is recruited to damaged or dysfunctional mitochondria in the earlystages, activated by PINK1, resulting in the ubiquitination of OMM proteins and subsequent proteasome degradation. Parkin-mediated mitophagy was found in the distal axons of rodent neurons and in age-related dopaminergic neurodegeneration in Parkin knockout mice with defective mitochondrial DNA replication [315,316].
LRRK2 contributes to mitophagy via its interference with mitochondrial trafficking, as its mutant form in a model of induced pluripotent stem cell-derived neurons impairs proteasome degradation of Miro, the OMM protein. This tethers mitochondria to microtubule motor proteins, resulting in mitophagy due to the disrupted interaction between LRRK2 and Miro [317].
Finally, it has been reported that CHCHD2 or Mitochondria Nuclear Retrograde Regulator 1 (MNRR1) is bound to the mitochondrial complex IV, and its reduced expression resulted in a decrease in mitochondrial complex IV activity, increasing ROS production and mitochondrial fragmentation. This MNRR1-mediated stress response may provide an important survival mechanism for cells under conditions of oxidative or hypoxic stress, both in the acute phase by altering mitochondrial oxygen utilization [318].
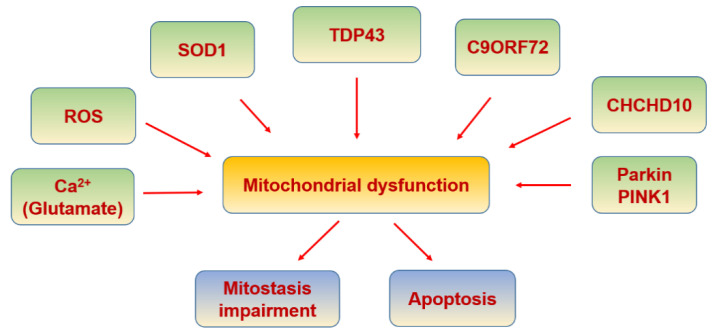
6.6. Amyotrophic Lateral Sclerosis
ALS is a neurodegenerative disease that compromises lower and upper motor neurons. The causes are unknown but 5% of the cases are due to genetic background. These genetic causes include hexanucleotide repeated insertions in C9ORF72 [328,329], or mutations mostly in SOD1 [330], fused in sarcoma (FUS) [331,332] and transactive response DNA binding protein (TARDBP) [333,334] genes (Figure 10). TARDBP gene encodes for TDP-43, an RNA-binding protein, whose aggregates inside the motor neurons are the most significant pathological finding in ALS [335] (Table 6). TDP-43 accumulation also compromises mitostasis, affecting fission and fusion kinetics, mitochondrial transport, bioenergetics, and mitochondrial quality control [336].
Figure 10.
Amyotrophic lateral sclerosis and mitochondria.
Table 6.
Proteins involved in mitochondrial dysfunction in ALS.
| Molecule | Function | Ref. |
|---|---|---|
| SOD-1 | Its aggregation impairs proper mitophagy by optineurin sequestration, and axonal transport of mitochondria | [345] |
| TDP-43 | Involved in interaction with mitochondrial proteins | [349] |
| TIM22 | TDP-43 gains access to the mitochondrial matrix via the mitochondrial import inner membrane | [350] |
| CHCHD10 | Involved in mitochondrial defects | [337] |
| Dbr1 | suppresses TDP-43 toxicity | [351] |
| Ataxin 2 | Increased risk for ALS | [352] |
| GSK-3β | disrupt the VAPB PTPIP51 interaction and ER–mitochondria associations | [353] |
| Alsin | Increased susceptibility to oxidative stress due to a defect in Rab5 relocation to mitochondria | [354] |
A mutation in the mitochondrial protein coiled-coil-helix-coiled-coil-helix domain-containing 10 (CHCHD10), CHCHD10S59L, has also been associated with frontotemporal dementia and ALS [337]. It drove progressive motor deficits, myopathy, cardiomyopathy and accelerated mortality in a mutated mice model [338] and disrupted OPA1-mitofilin complexes in transfected cells and in vivo mice [339]. Evidence from SOD1G93A rat models (substitution of glycine to alanine at position 93) has demonstrated that misfolded SOD1 is able to increase toxicity due to a toxic gain-of-function role, and exists in different conformers dependent on the type of misfolding [340], which deposit on mitochondrial subpopulations on the OMM, IMM, intermembrane space and matrix [341,342]. Consistently, a model of human SOD1G93A transgenic pigs, which displayed ALS-like symptoms, showed impaired mitostasis [343]. Interestingly, it has been suggested that a defect in mitophagy may contribute to the development of ALS, as fewer phagosomes are found than in controls using mice models [344]. This defect could be explained by a mutant SOD1-mediated optineurin sequestration [345]. The mitophagy-associated proteins Parkin and PINK1 have also been found to be downregulated in ALS mice models [346].
Impairment of mitochondrial function can result in excess production of ROS, and due to the proximity to the ROS production site, mtDNA is highly prone to damage. Furthermore, mtDNA is not associated with histones and chromatin-associated proteins for protection and is highly vulnerable to damage [347]. On the other hand, in both sporadic and familial cases of ALS it has been proposed that the excitotoxicity by glutamate could play a key role [348]. This might be due to an increased Ca2+ influx that would affect mitochondrial function and would initiate apoptosis.
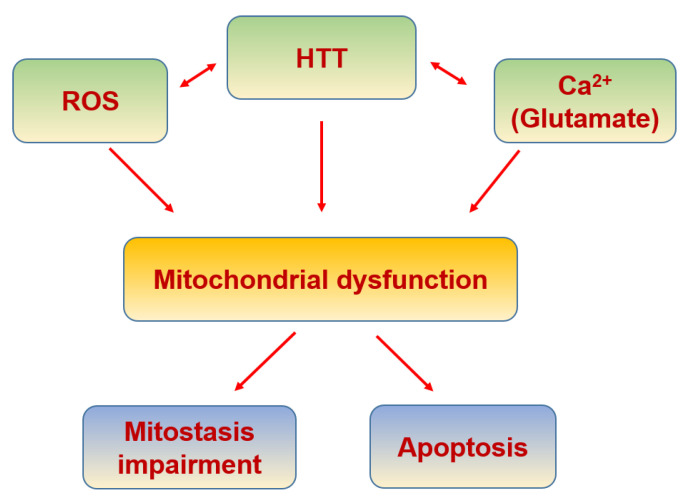
6.7. Huntington’s Disease
HD is a neurodegenerative disease caused by the repetition of CAG in the huntingtin gene, which leads to huntingtin protein (HTT) aggregation (Table 7), inducing neuronal death, mainly in the corpus striatum but also in systemic cells [355]. In HD there is an increase in the expression of the functional subunits of NMDAR due to HTT [356], where NO could be playing a translational role [357,358]. This increase produces a higher and maintained intracellular Ca2+ concentration, affecting mitochondrial function [359] and triggering apoptosis [360] (Figure 11).
Table 7.
Proteins involved in mitochondrial dysfunction in Huntington disease.
| Molecule | Function | Ref. |
|---|---|---|
| Huntingtin | Its aggregation increases mitochondrial calcium concentration and ROS production | [356] |
| Ubiquitin-like protein 1 (NUB1) | Suppressor of mutant Huntington toxicity via enhanced protein clearance | [367] |
| Bcl-2/adenovirus E1B 19-kDa interacting protein 3 (BNip3) | Evidence of an abnormal activation in cells expressing mutant Huntingtin. | [368] |
| p53 | Regulates the levels of huntingtin gene expression | [369] |
| BDNF | Enhancing BDNF vesicular transport along microtubules | [370] |
| Alpha-tubulin deacetylase (HDAC) | Pharmacological inhibition of the HDAC6 deacetylase activity increased acetylated alpha-tubulin levels, and induced mitochondrial motility and fusion in striatal neurons | [371] |
| PGC1a | Transcriptional repression of PGC-1alpha by mutant huntingtin | [372] |
| Drp1 | Its interaction with mutant HTT impairs mitochondrial biogenesis, causing defective mitochondria axonal transport and synaptic degeneration | [366] |
Figure 11.
Huntington’s disease and mitochondria.
HTT is also associated with increased oxidative stress, since the aggregation of the N-terminus fragments of the mutant HTT contributes to an increased generation of ROS [361]. On the other hand, HTT inclusion bodies generate iron-dependent oxidative stress [362]. One of the pathological effects of the increased ROS production is the oxidation of the mtDNA [363], which impairs mitochondrial biogenesis as it has been reported in HD [364,365]. Another factor that contributes to impair mitochondrial biogenesis in HD is the direct interaction of mutated HTT with Drp1 [366].
7. Conclusions
Aging and neurodegenerative processes are not the consequences of a unique signaling pathway alteration but of multifactorial events, including dysfunction of mitochondria that yield to failures in ATP production, increased ROS production and alterations in Ca2+ homeostasis. Considering mitochondria as a therapeutictarget would produce an improvement in the maintenance of the optimum neuronal function. These therapeutic approaches would include the regulation of PGC-1α and calcium buffering systems as well as free radicals’generation, addressing the source of free radicals more than the use of antioxidants that have not demonstrated effective results to date.
Acknowledgments
We thanks to the Library Service of Universitat Pompeu Fabra for their support.
Abbreviations
| AD | Alzheimer’s disease |
| ALS | amyotrophic lateral sclerosis |
| AMPA | α-amino-3 hydroxy-5-methyl-4-isoxazolepropionic acid receptor |
| AMPK | adenosine monophosphate-activated protein kinase |
| ANT | adenine nucleotide translocase |
| APAF-1 | apoptosis protease-activating factor-1 |
| ASC | adaptor protein |
| ATP | adenosine triphosphate |
| Aβ | amyloid beta-peptide |
| BAP31 | B-cell receptor-associated protein 31 |
| BDNF | brain-derived neurotrophic factor |
| BER | Base excision repair |
| β/cAMP | β-adrenergic signalling |
| Ca2+ | Calcium |
| CAMKII | Ca2+/calmodulin-dependent protein kinase |
| CAT | Catalase |
| CDKs | cyclin-dependent kinases |
| CICR | Ca2+-induced Ca2+ release |
| CHCHD2 | coiled-coil-helix-coiled-coil-helix domain containing 2 |
| CHCHD10 | coiled-coil-helix-coiled-coil-helix domain-containing 10 |
| CREB | cAMP response element-binding protein |
| Cybrid | cytoplasmatic hybrids |
| CypD | cyclophilin D |
| CytC | cytochrome C |
| Drp1 | dynamin-related protein 1 |
| EMRE | essential MCU regulator |
| eNOS | endothelial NOS |
| ER | endoplasmic reticulum |
| ERKs | extracellular signal-regulated kinases |
| Fis1 | mitochondrial fission 1 |
| FUS | fused in sarcoma |
| FZ | frizzled receptor |
| GABA | γ-aminobutyric acid |
| GPx | glutathione peroxidase |
| GSH | Glutathione |
| Grp75 | mitochondrial chaperone glucose-regulated protein 75 |
| GSK3β | glycogen synthase kinase-3β |
| H2O2 | hydrogen peroxide |
| HD | Huntington’s disease |
| HKII | hexokinase II |
| HTT | Huntingtin |
| IKK | IkB kinase |
| IL-18 | interleukin 18 |
| IL-1β | interleukin 1β |
| IL-6 | interleukin 6 |
| IMM | inner mitochondrial membrane |
| INF2 | inverted formin 2 |
| IP3R | inositol triphosphate receptor |
| IR | insulin receptor |
| IRS | insulin receptor substrate |
| JNK | c-Jun N-terminal kinase |
| LRP5/6 | low-density lipoprotein receptor-related protein 5/6 |
| LRRK | Leucine Rich Repeat Kinase 2 |
| LTP | long-term potentiation |
| MAM | mitochondria associated membranes |
| MAPK | mitogen activated protein kinases |
| MCI | mild cognitive impairment |
| MCU | mitochondrial Ca2+ uniporter |
| MCUb | Mitochondrial Calcium Uniporter Dominant Negative Subunit Beta |
| MCUR1 | MCU regulator 1 |
| MFF | mitochondrial fission factor |
| MFN | Mitofusin |
| MFN1 | mitofusin protein 1 |
| MFN2 | mitofusin protein 2 |
| MICU1 | mitochondrial calcium uptake 1 |
| MICU2 | mitochondrial calcium uptake 2 |
| MiD49 | mitochondrial dynamic protein 49 |
| MiD50 | mitochondrial dynamic protein 50 |
| Miro | Mitochondrial Rho GTPase |
| MNRR1 | Mitochondria Nuclear Retrograde Regulator 1 |
| mPTP | mitochondrial permeability transition pore |
| MPTP | 1-methyl4-phenyl-1,2,3,4-tetrahydropyridine |
| MRC | mitochondrial respiratory chain |
| mtDNA | mitochondrial DNA |
| mtNOS | mitochondrial NOS |
| mTOR | mechanistic target of rapamycin kinase |
| Myo19 | myosin19 |
| NAD+/NADH | nicotinamide adenine dinucleotide |
| NCLX | Li+-permeable Na+/Ca2+ exchanger |
| NFAT | nuclear factor of activated T-cells |
| NF-κB | nuclear factor kappa-light-chain-enhancer of activated B cells |
| NLRP3 | Nod-like receptor 3 |
| NMDAR | N-methyl-D-aspartate receptor |
| nNOS | neuronal NOS |
| NO | Nitric oxide |
| NOS | constitutive NO-synthase |
| NRF1 | nuclear respiratory factor 1 |
| NRF2 | nuclear respiratory factor 2 |
| O2·− | superoxide anion |
| OH.− | hydroxyl radical |
| OMM | outer mitochondrial membrane |
| ONOO− | Peroxynitrite |
| OPA1 | protein optic atrophy 1 |
| p38α | p38 mitogen-activated protein kinase alpha |
| PACS-2 | phosphofurin acidic cluster sorting protein 2 |
| PD | Parkinson’s disease |
| PGC-1α | peroxisome proliferator-activated receptor-γ (PPARγ) coactivator-1α |
| PGC1β | peroxisome proliferator-activated receptor gamma coactivator 1-beta |
| PI3K | phospho-inositol-3 kinase |
| PINK1 | PTEN-induced kinase 1 |
| PIP | phosphatidylinositol phosphate |
| PKC | protein kinase C |
| PRC | PGC-related coactivator |
| PS2 | presenilin 2 |
| pS302 | phosphorylation of insulin receptor at serine-302 |
| pS307 | phosphorylation of insulin receptor at serine-307 |
| PTPIP51 | tyrosine phosphatase-interacting protein-51 |
| ROS | reactive oxygen species |
| RyR | ryanodine receptor |
| SERCA | sarco/endoplasmic reticulum Ca2+-ATPase |
| SIRT | silent mating type information regulation 2 homolog |
| SOC | store-operated Ca2+ channel |
| SOCE | store operated Ca2+ entry |
| SOCS | suppressor cytokine signalling |
| SOD | antioxidant enzymes superoxide dismutase |
| SOD1 | Cu/Zn superoxide dismutase 1 |
| SLC25A23 | solute carrier 25A23 |
| STIM | stromal interaction molecule |
| T2D | type 2 diabetes |
| SNPC | substantia nigra pars compacta |
| SNPH | Syntaphilin |
| TCA | tricarboxylic acid cycle |
| TARDBP/TDP-43 | transactive response DNA binding protein 43 |
| TFAM | mitochondrial transcription factor A |
| TFB1M | cofactor mitochondrial transcription factor B |
| TH | thyroid hormone |
| TNF-α | tumor necrosis factor α |
| TOMM 40 | Translocase of the OMM 40 |
| TRAK | trafficking kinesin protein |
| TRP | transient receptor potential |
| VAPB | vesicle-associated membrane protein-B |
| VDAC | voltage dependent anion channel 1 |
| VGCC | voltage-gated Ca2+ channels |
| WISP3/CCN6 | Wnt-induced signaling protein 3 |
| Wnt | Wnt signaling pathway |
| ΔΨm | mitochondrial membrane potential. |
Author Contributions
All authors have made equal intellectual contributions to the writing of this manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the Spanish Ministry of Science and Innovation and FEDER Funds through grants SAF2017-83372-R (FJM); RTI2018-094809-B-I00 (JMFF); PID2019-106755RB-I00 (RV); and through the “María de Maeztu” Programme for Units of Excellence in R&D (award CEX2018-000792-M).
Institutional Review Board Statement
Ethical review and approval were waived for this study since it is a review of published works. We have not carried out experiments in this review.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare that they have no competing interests that might be perceived to influence the results and discussion reported in this paper.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Erbslöh F., Bernsmeier A., Hillesheim H.R. Der Glucoseverbrauch des Gehirns und seine Abhängigkeit von der Leber. Arch. für Psychiatr. und Nervenkrankheiten Ver. mit Zeitschrift für die Gesamte Neurol. und Psychiatr. 1958;196:611–626. doi: 10.1007/BF00344388. [DOI] [PubMed] [Google Scholar]
- 2.Sokoloff L. Energetics of functional activation in neural tissues. Neurochem. Res. 1999;24:321–329. doi: 10.1023/A:1022534709672. [DOI] [PubMed] [Google Scholar]
- 3.Lin M.Y., Sheng Z.H. Regulation of mitochondrial transport in neurons. Exp. Cell Res. 2015;334:35–44. doi: 10.1016/j.yexcr.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Misgeld T., Schwarz T.L. Mitostasis in neurons: Maintaining mitochondria in an extended cellular architecture. Neuron. 2017;96:651–666. doi: 10.1016/j.neuron.2017.09.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brini M., Calì T., Ottolini D., Carafoli E. Neuronal calcium signaling: Function and dysfunction. Cell. Mol. Life Sci. 2014;71:2787–2814. doi: 10.1007/s00018-013-1550-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calvo-Rodriguez M., Bacskai B.J. Mitochondria and calcium in Alzheimer’s disease: From cell signaling to neuronal cell death. Trends Neurosci. 2021;44:136–151. doi: 10.1016/j.tins.2020.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Cadenas E., Davies K.J.A. Mitochondrial free radical generation, oxidative stress, and aging. Free Radic. Biol. Med. 2000;29:222–230. doi: 10.1016/S0891-5849(00)00317-8. [DOI] [PubMed] [Google Scholar]
- 8.Kruman I.I., Mattson M.P. Pivotal role of mitochondrial calcium uptake in neural cell apoptosis and necrosis. J. Neurochem. 1999;72:529–540. doi: 10.1046/j.1471-4159.1999.0720529.x. [DOI] [PubMed] [Google Scholar]
- 9.Braschi E., McBride H.M. Mitochondria and the culture of the Borg. BioEssays. 2010;32:958–966. doi: 10.1002/bies.201000073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wai T., Langer T. Mitochondrial dynamics and metabolic regulation. Trends Endocrinol. Metab. 2016;27:105–117. doi: 10.1016/j.tem.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Calvo S.E., Mootha V.K. The mitochondrial proteome and human disease. Annu. Rev. Genomics Hum. Genet. 2010;11:25–44. doi: 10.1146/annurev-genom-082509-141720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nicolas E., Tricarico R., Savage M., Golemis E.A., Hall M.J. Disease-associated genetic variation in human mitochondrial protein import. Am. J. Hum. Genet. 2019;104:784–801. doi: 10.1016/j.ajhg.2019.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Connerth M., Tatsuta T., Haag M., Klecker T., Westermann B., Langer T. Intramitochondrial transport of phosphatidic acid in yeast by a lipid transfer protein. Science (80-. ). 2012;338:815–818. doi: 10.1126/science.1225625. [DOI] [PubMed] [Google Scholar]
- 14.Vicario-Orri E., Opazo C.M., Muñoz F.J. The pathophysiology of axonal transport in Alzheimer’s disease. J. Alzheimer’s Dis. 2014;43:1097–1113. doi: 10.3233/JAD-141080. [DOI] [PubMed] [Google Scholar]
- 15.Guo X., Macleod G.T., Wellington A., Hu F., Panchumarthi S., Schoenfield M., Marin L., Charlton M.P., Atwood H.L., Zinsmaier K.E. The GTPase dMiro is required for axonal transport of mitochondria to drosophila synapses. Neuron. 2005;47:379–393. doi: 10.1016/j.neuron.2005.06.027. [DOI] [PubMed] [Google Scholar]
- 16.Brickley K., Stephenson F.A. Trafficking kinesin protein (TRAK)-mediated transport of mitochondria in axons of hippocampal neurons. J. Biol. Chem. 2011;286:18079–18092. doi: 10.1074/jbc.M111.236018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stowers R.S., Megeath L.J., Górska-Andrzejak J., Meinertzhagen I.A., Schwarz T.L. Axonal transport of mitochondria to synapses depends on Milton, a novel Drosophila protein. Neuron. 2002;36:1063–1077. doi: 10.1016/S0896-6273(02)01094-2. [DOI] [PubMed] [Google Scholar]
- 18.Nangaku M., Sato-Yoshitake R., Okada Y., Noda Y., Takemura R., Yamazaki H., Hirokawa N. KIF1B, a novel microtubule plus end-directed monomeric motor protein for transport of mitochondria. Cell. 1994;79:1209–1220. doi: 10.1016/0092-8674(94)90012-4. [DOI] [PubMed] [Google Scholar]
- 19.Fransson Å., Ruusala A., Aspenström P. The atypical Rho GTPases Miro-1 and Miro-2 have essential roles in mitochondrial trafficking. Biochem. Biophys. Res. Commun. 2006;344:500–510. doi: 10.1016/j.bbrc.2006.03.163. [DOI] [PubMed] [Google Scholar]
- 20.Van Spronsen M., Mikhaylova M., Lipka J., Schlager M.A., van den Heuvel D.J., Kuijpers M., Wulf P.S., Keijzer N., Demmers J., Kapitein L.C., et al. TRAK/Milton motor-adaptor proteins steer mitochondrial trafficking to axons and dendrites. Neuron. 2013;77:485–502. doi: 10.1016/j.neuron.2012.11.027. [DOI] [PubMed] [Google Scholar]
- 21.Pilling A.D., Horiuchi D., Lively C.M., Saxton W.M. Kinesin-1 and dynein are the primary motors for fast transport of mitochondria in Drosophila motor axons. Mol. Biol. Cell. 2006;17:2057–2068. doi: 10.1091/mbc.e05-06-0526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kapitein L.C., Schlager M.A., Kuijpers M., Wulf P.S., van Spronsen M., MacKintosh F.C., Hoogenraad C.C. Mixed microtubules steer dynein-driven cargo transport into dendrites. Curr. Biol. 2010;20:290–299. doi: 10.1016/j.cub.2009.12.052. [DOI] [PubMed] [Google Scholar]
- 23.Quintero O.A., DiVito M.M., Adikes R.C., Kortan M.B., Case L.B., Lier A.J., Panaretos N.S., Slater S.Q., Rengarajan M., Feliu M., et al. Human Myo19 is a novel myosin that associates with mitochondria. Curr. Biol. 2009;19:2008–2013. doi: 10.1016/j.cub.2009.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.López-Doménech G., Covill-Cooke C., Ivankovic D., Halff E.F., Sheehan D.F., Norkett R., Birsa N., Kittler J.T. Miro proteins coordinate microtubule- and actin-dependent mitochondrial transport and distribution. EMBO J. 2018;37:321–336. doi: 10.15252/embj.201696380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morris R.L., Hollenbeck P.J. The regulation of bidirectional mitochondrial transport is coordinated with axonal outgrowth. J. Cell Sci. 1993;104:917–927. doi: 10.1242/jcs.104.3.917. [DOI] [PubMed] [Google Scholar]
- 26.Kraft L.M., Lackner L.L. Mitochondrial anchors: Positioning mitochondria and more. Biochem. Biophys. Res. Commun. 2018;500:2–8. doi: 10.1016/j.bbrc.2017.06.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li S., Xiong G.J., Huang N., Sheng Z.H. The cross-talk of energy sensing and mitochondrial anchoring sustains synaptic efficacy by maintaining presynaptic metabolism. Nat. Metab. 2020;2:1077–1095. doi: 10.1038/s42255-020-00289-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwarz T.L. Mitochondrial trafficking in neurons. Cold Spring Harb. Perspect. Biol. 2013;5 doi: 10.1101/cshperspect.a011304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Joshi D.C., Zhang C.L., Babujee L., Vevea J.D., August B.K., Sheng Z.H., Chapman E.R., Gomez T.M., Chiu S.Y. Inappropriate intrusion of an axonal mitochondrial anchor into dendrites causes neurodegeneration. Cell Rep. 2019;29:685–696.e5. doi: 10.1016/j.celrep.2019.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fukumitsu K., Hatsukano T., Yoshimura A., Heuser J., Fujishima K., Kengaku M. Mitochondrial fission protein Drp1 regulates mitochondrial transport and dendritic arborization in cerebellar Purkinje cells. Mol. Cell. Neurosci. 2016;71:56–65. doi: 10.1016/j.mcn.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 31.Gandre-Babbe S., Van Der Bliek A.M. The novel tail-anchored membrane protein Mff controls mitochondrial and peroxisomal fission in mammalian cells. Mol. Biol. Cell. 2008;19:2402–2412. doi: 10.1091/mbc.e07-12-1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Otera H., Wang C., Cleland M.M., Setoguchi K., Yokota S., Youle R.J., Mihara K. Mff is an essential factor for mitochondrial recruitment of Drp1 during mitochondrial fission in mammalian cells. J. Cell Biol. 2010;191:1141–1158. doi: 10.1083/jcb.201007152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smirnova E., Griparic L., Shurland D.L., Van der Bliek A.M. Dynamin-related protein Drp1 is required for mitochondrial division in mammalian cells. Mol. Biol. Cell. 2001;12:2245–2256. doi: 10.1091/mbc.12.8.2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoon Y., Krueger E.W., Oswald B.J., McNiven M.A. The mitochondrial protein hFis1 regulates mitochondrial fission in mammalian cells through an interaction with the dynamin-like protein DLP1. Mol. Cell. Biol. 2003;23:5409–5420. doi: 10.1128/MCB.23.15.5409-5420.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Palmer C.S., Osellame L.D., Laine D., Koutsopoulos O.S., Frazier A.E., Ryan M.T. MiD49 and MiD51, new components of the mitochondrial fission machinery. EMBO Rep. 2011;12:565–573. doi: 10.1038/embor.2011.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Friedman J.R., Lackner L.L., West M., DiBenedetto J.R., Nunnari J., Voeltz G.K. ER tubules mark sites of mitochondrial division. Science. 2011;334:358–362. doi: 10.1126/science.1207385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Korobova F., Ramabhadran V., Higgs H.N. An actin-dependent step in mitochondrial fission mediated by the ER-associated formin INF2. Science. 2013;339:464–467. doi: 10.1126/science.1228360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen H., McCaffery J.M., Chan D.C. Mitochondrial fusion protects against neurodegeneration in the cerebellum. Cell. 2007;130:548–562. doi: 10.1016/j.cell.2007.06.026. [DOI] [PubMed] [Google Scholar]
- 39.Santel A., Fuller M.T. Control of mitochondrial morphology by a human mitofusin. J. Cell Sci. 2001;114:867–874. doi: 10.1242/jcs.114.5.867. [DOI] [PubMed] [Google Scholar]
- 40.Hales K.G., Fuller M.T. Developmentally regulated mitochondrial fusion mediated by a conserved, novel, predicted GTPase. Cell. 1997;90:121–129. doi: 10.1016/S0092-8674(00)80319-0. [DOI] [PubMed] [Google Scholar]
- 41.Zorzano A., Pich S. What is the biological significance of the two mitofusin proteins present in the outer mitochondrial membrane of mammalian cells? IUBMB Life. 2006;58:441–443. doi: 10.1080/15216540600644838. [DOI] [PubMed] [Google Scholar]
- 42.Ishihara N., Eura Y., Mihara K. Mitofusin 1 and 2 play distinct roles in mitochondrial fusion reactions via GTPase activity. J. Cell Sci. 2004;117:6535–6546. doi: 10.1242/jcs.01565. [DOI] [PubMed] [Google Scholar]
- 43.De Brito O.M., Scorrano L. Mitofusin 2 tethers endoplasmic reticulum to mitochondria. Nature. 2008;456:605–610. doi: 10.1038/nature07534. [DOI] [PubMed] [Google Scholar]
- 44.Koshiba T., Detmer S.A., Kaiser J.T., Chen H., McCaffery J.M., Chan D.C. Structural basis of mitochondrial tethering by mitofusin complexes. Science. 2004;305:858–862. doi: 10.1126/science.1099793. [DOI] [PubMed] [Google Scholar]
- 45.Cosson P., Marchetti A., Ravazzola M., Orci L. Mitofusin-2 independent juxtaposition of endoplasmic reticulum and mitochondria: An ultrastructural study. PLoS One. 2012;7 doi: 10.1371/journal.pone.0046293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Olichon A., Emorine L.J., Descoins E., Pelloquin L., Brichese L., Gas N., Guillou E., Delettre C., Valette A., Hamel C.P., et al. The human dynamin-related protein OPA1 is anchored to the mitochondrial inner membrane facing the inter-membrane space. FEBS Lett. 2002;523:171–176. doi: 10.1016/S0014-5793(02)02985-X. [DOI] [PubMed] [Google Scholar]
- 47.Meeusen S., DeVay R., Block J., Cassidy-Stone A., Wayson S., McCaffery J.M., Nunnari J. Mitochondrial inner-membrane fusion and crista maintenance requires the dynamin-related GTPase Mgm1. Cell. 2006;127:383–395. doi: 10.1016/j.cell.2006.09.021. [DOI] [PubMed] [Google Scholar]
- 48.DeVay R.M., Dominguez-Ramirez L., Lackner L.L., Hoppins S., Stahlberg H., Nunnari J. Coassembly of Mgm1 isoforms requires cardiolipin and mediates mitochondrial inner membrane fusion. J. Cell Biol. 2009;186:793–803. doi: 10.1083/jcb.200906098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen H., Vermulst M., Wang Y.E., Chomyn A., Prolla T.A., McCaffery J.M., Chan D.C. Mitochondrial fusion is required for mtdna stability in skeletal muscle and tolerance of mtDNA mutations. Cell. 2010;141:280–289. doi: 10.1016/j.cell.2010.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patten D.A., Wong J., Khacho M., Soubannier V., Mailloux R.J., Pilon-Larose K., MacLaurin J.G., Park D.S., McBride H.M., Trinkle-Mulcahy L., et al. OPA1-dependent cristae modulation is essential for cellular adaptation to metabolic demand. EMBO J. 2014;33:2676–2691. doi: 10.15252/embj.201488349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cogliati S., Frezza C., Soriano M.E., Varanita T., Quintana-Cabrera R., Corrado M., Cipolat S., Costa V., Casarin A., Gomes L.C., et al. Mitochondrial cristae shape determines respiratory chain supercomplexes assembly and respiratory efficiency. Cell. 2013;155:160–171. doi: 10.1016/j.cell.2013.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Olichon A., Baricault L., Gas N., Guillou E., Valette A., Belenguer P., Lenaers G. Loss of OPA1 perturbates the mitochondrial inner membrane structure and integrity, leading to cytochrome c release and apoptosis. J. Biol. Chem. 2003;278:7743–7746. doi: 10.1074/jbc.C200677200. [DOI] [PubMed] [Google Scholar]
- 53.Wu Z., Puigserver P., Andersson U., Zhang C., Adelmant G., Mootha V., Troy A., Cinti S., Lowell B., Scarpulla R.C., et al. Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC-1. Cell. 1999;98:115–124. doi: 10.1016/S0092-8674(00)80611-X. [DOI] [PubMed] [Google Scholar]
- 54.Virbasius J.V., Scarpulla R.C. Activation of the human mitochondrial transcription factor A gene by nuclear respiratory factors: A potential regulatory link between nuclear and mitochondrial gene expression in organelle biogenesis. Proc. Natl. Acad. Sci. USA. 1994;91:1309–1313. doi: 10.1073/pnas.91.4.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McCulloch V., Shadel G.S. Human mitochondrial transcription factor B1 interacts with the C-terminal activation region of h-mtTFA and stimulates transcription independently of Its RNA methyltransferase activity. Mol. Cell. Biol. 2003;23:5816–5824. doi: 10.1128/MCB.23.16.5816-5824.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guo J., Zheng L., Liu W., Wang X., Wang Z., Wang Z., French A.J., Kang D., Chen L., Thibodeau S.N., et al. Frequent truncating mutation of TFAM induces mitochondrial DNA depletion and apoptotic resistance in microsatellite-unstable colorectal cancer. Cancer Res. 2011;71:2978–2987. doi: 10.1158/0008-5472.CAN-10-3482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kanki T., Ohgaki K., Gaspari M., Gustafsson C.M., Fukuoh A., Sasaki N., Hamasaki N., Kang D. Architectural role of mitochondrial transcription factor A in maintenance of human mitochondrial DNA. Mol. Cell. Biol. 2004;24:9823–9834. doi: 10.1128/MCB.24.22.9823-9834.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kaufman B.A., Durisic N., Mativetsky J.M., Costantino S., Hancock M.A., Grutter P., Shoubridge E.A. The mitochondrial transcription factor TFAM coordinates the assembly of multiple DNA molecules into nucleoid-like structures. Mol. Biol. Cell. 2007;18:3225–3236. doi: 10.1091/mbc.e07-05-0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schilling J., Kelly D.P. The PGC-1 cascade as a therapeutic target for heart failure. J. Mol. Cell. Cardiol. 2011;51:578–583. doi: 10.1016/j.yjmcc.2010.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McClure T.D., Young M.E., Taegtmeyer H., Ning X.-H., Buroker N.E., López-Guisa J., Portman M.A. Thyroid hormone interacts with PPARα and PGC-1 during mitochondrial maturation in sheep heart. Am. J. Physiol. Circ. Physiol. 2005;289:H2258–H2264. doi: 10.1152/ajpheart.00473.2005. [DOI] [PubMed] [Google Scholar]
- 61.Rodgers J.T., Lerin C., Haas W., Gygi S.P., Spiegelman B.M., Puigserver P. Nutrient control of glucose homeostasis through a complex of PGC-1α and SIRT1. Nature. 2005;434:113–118. doi: 10.1038/nature03354. [DOI] [PubMed] [Google Scholar]
- 62.Gurd B.J., Yoshida Y., McFarlan J.T., Holloway G.P., Moyes C.D., Heigenhauser G.J.F., Spriet L., Bonen A. Nuclear SIRT1 activity, but not protein content, regulates mitochondrial biogenesis in rat and human skeletal muscle. Am. J. Physiol. - Regul. Integr. Comp. Physiol. 2011;301 doi: 10.1152/ajpregu.00417.2010. [DOI] [PubMed] [Google Scholar]
- 63.Schaeffer P.J., Wende A.R., Magee C.J., Neilson J.R., Leone T.C., Chen F., Kelly D.P. Calcineurin and calcium/calmodulin-dependent protein kinase activate distinct metabolic gene regulatory programs in cardiac muscle. J. Biol. Chem. 2004;279:39593–39603. doi: 10.1074/jbc.M403649200. [DOI] [PubMed] [Google Scholar]
- 64.Zong H., Ren J.M., Young L.H., Pypaert M., Mu J., Birnbaum M.J., Shulman G.I. AMP kinase is required for mitochondrial biogenesis in skeletal muscle in response to chronic energy deprivation. Proc. Natl. Acad. Sci. USA. 2002;99:15983–15987. doi: 10.1073/pnas.252625599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sano M., Wang S.C., Shirai M., Scaglia F., Xie M., Sakai S., Tanaka T., Kulkarni P.A., Barger P.M., Youker K.A., et al. Activation of cardiac Cdk9 represses PGC-1 and confers a predisposition to heart failure. EMBO J. 2004;23:3559–3569. doi: 10.1038/sj.emboj.7600351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Brandt N., Nielsen L., Thiellesen Buch B., Gudiksen A., Ringholm S., Hellsten Y., Bangsbo J., Pilegaard H. Impact of β-adrenergic signaling in PGC-1α-mediated adaptations in mouse skeletal muscle. Am. J. Physiol. Metab. 2018;314:E1–E20. doi: 10.1152/ajpendo.00082.2017. [DOI] [PubMed] [Google Scholar]
- 67.Puigserver P., Rhee J., Lin J., Wu Z., Yoon J.C., Zhang C.Y., Krauss S., Mootha V.K., Lowell B.B., Spiegelman B.M. Cytokine stimulation of energy expenditure through p38 MAP kinase activation of PPARγ coactivator-1. Mol. Cell. 2001;8:971–982. doi: 10.1016/S1097-2765(01)00390-2. [DOI] [PubMed] [Google Scholar]
- 68.Fan M., Rhee J., St-Pierre J., Handschin C., Puigserver P., Lin J., Jäeger S., Erdjument-Bromage H., Tempst P., Spiegelman B.M. Suppression of mitochondrial respiration through recruitment of p160 myb binding protein to PGC-1α: Modulation by p38 MAPK. Genes Dev. 2004;18:278–289. doi: 10.1101/gad.1152204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cheng A., Wan R., Yang J.L., Kamimura N., Son T.G., Ouyang X., Luo Y., Okun E., Mattson M.P. Involvement of PGC-1α in the formation and maintenance of neuronal dendritic spines. Nat. Commun. 2012;3 doi: 10.1038/ncomms2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wrann C.D., White J.P., Salogiannnis J., Laznik-Bogoslavski D., Wu J., Ma D., Lin J.D., Greenberg M.E., Spiegelman B.M. Exercise induces hippocampal BDNF through a PGC-1α/FNDC5 pathway. Cell Metab. 2013;18:649–659. doi: 10.1016/j.cmet.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang Y., Li R., Meng Y., Li S., Donelan W., Zhao Y., Qi L., Zhang M., Wang X., Cui T., et al. Irisin stimulates browning of white adipocytes through mitogen-activated protein kinase p38 MAP kinase and ERK MAP kinase signaling. Diabetes. 2014;63:514–525. doi: 10.2337/db13-1106. [DOI] [PubMed] [Google Scholar]
- 72.Pedersen B.K. Physical activity and muscle–brain crosstalk. Nat. Rev. Endocrinol. 2019;15:383–392. doi: 10.1038/s41574-019-0174-x. [DOI] [PubMed] [Google Scholar]
- 73.Steiner J.L., Murphy E.A., McClellan J.L., Carmichael M.D., Davis J.M. Exercise training increases mitochondrial biogenesis in the brain. J. Appl. Physiol. 2011;111:1066–1071. doi: 10.1152/japplphysiol.00343.2011. [DOI] [PubMed] [Google Scholar]
- 74.St-Pierre J., Drori S., Uldry M., Silvaggi J.M., Rhee J., Jäger S., Handschin C., Zheng K., Lin J., Yang W., et al. Suppression of reactive oxygen species and neurodegeneration by the PGC-1 transcriptional coactivators. Cell. 2006;127:397–408. doi: 10.1016/j.cell.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 75.Colombini M. VDAC structure, selectivity, and dynamics. Biochim. Biophys. Acta - Biomembr. 2012;1818:1457–1465. doi: 10.1016/j.bbamem.2011.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gincel D., Silberberg S.D., Shoshan-Barmatz V. Modulation of the voltage-dependent anion channel (VDAC) by glutamate. J. Bioenerg. Biomembr. 2000;32:571–583. doi: 10.1023/A:1005670527340. [DOI] [PubMed] [Google Scholar]
- 77.Rostovtseva T., Colombini M. VDAC channels mediate and gate the flow of ATP: Implications for the regulation of mitochondrial function. Biophys. J. 1997;72:1954–1962. doi: 10.1016/S0006-3495(97)78841-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gincel D., Zaid H., Shoshan-Barmatz V. Calcium binding and translocation by the voltage-dependent anion channel: A possible regulatory mechanism in mitochondrial function. Biochem. J. 2001;358:147–155. doi: 10.1042/bj3580147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rapizzi E., Pinton P., Szabadkai G., Wieckowski M.R., Vandecasteele G., Baird G., Tuft R.A., Fogarty K.E., Rizzuto R. Recombinant expression of the voltage-dependent anion channel enhances the transfer of Ca2+ microdomains to mitochondria. J. Cell Biol. 2002;159:613–624. doi: 10.1083/jcb.200205091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tan W., Colombini M. VDAC closure increases calcium ion flux. Biochim. Biophys. Acta - Biomembr. 2007;1768:2510–2515. doi: 10.1016/j.bbamem.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Raffaello A., De Stefani D., Sabbadin D., Teardo E., Merli G., Picard A., Checchetto V., Moro S., Szabò I., Rizzuto R. The mitochondrial calcium uniporter is a multimer that can include a dominant-negative pore-forming subunit. EMBO J. 2013;32:2362–2376. doi: 10.1038/emboj.2013.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mallilankaraman K., Cárdenas C., Doonan P.J., Chandramoorthy H.C., Irrinki K.M., Golenár T., Csordás G., Madireddi P., Yang J., Müller M., et al. MCUR1 is an essential component of mitochondrial Ca2+ uptake that regulates cellular metabolism. Nat. Cell Biol. 2012;14:1336–1343. doi: 10.1038/ncb2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Perocchi F., Gohil V.M., Girgis H.S., Bao X.R., McCombs J.E., Palmer A.E., Mootha V.K. MICU1 encodes a mitochondrial EF hand protein required for Ca2+ uptake. Nature. 2010;467:291–296. doi: 10.1038/nature09358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Plovanich M., Bogorad R.L., Sancak Y., Kamer K.J., Strittmatter L., Li A.A., Girgis H.S., Kuchimanchi S., De Groot J., Speciner L., et al. MICU2, a paralog of MICU1, resides within the mitochondrial uniporter complex to regulate calcium handling. PLoS ONE. 2013;8 doi: 10.1371/journal.pone.0055785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hoffman N.E., Chandramoorthy H.C., Shanmughapriya S., Zhang X.Q., Vallem S., Doonan P.J., Malliankaraman K., Guo S., Rajan S., Elrod J.W., et al. SLC25A23 augments mitochondrial Ca2+ uptake, interacts with MCU, and induces oxidative stress-mediated cell death. Mol. Biol. Cell. 2014;25:936–947. doi: 10.1091/mbc.e13-08-0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sancak Y., Markhard A.L., Kitami T., Kovács-Bogdán E., Kamer K.J., Udeshi N.D., Carr S.A., Chaudhuri D., Clapham D.E., Li A.A., et al. EMRE is an essential component of the mitochondrial calcium uniporter complex. Science (80-. ). 2013;342:1379–1382. doi: 10.1126/science.1242993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tsai M.F., Phillips C.B., Ranaghan M., Tsai C.W., Wu Y., Williams C., Miller C. Dual functions of a small regulatory subunit in the mitochondrial calcium uniporter complex. Elife. 2016;5 doi: 10.7554/eLife.15545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mallilankaraman K., Doonan P., Cárdenas C., Chandramoorthy H.C., Müller M., Miller R., Hoffman N.E., Gandhirajan R.K., Molgó J., Birnbaum M.J., et al. MICU1 is an essential gatekeeper for mcu-mediated mitochondrial Ca2+ uptake that regulates cell survival. Cell. 2012;151:630–644. doi: 10.1016/j.cell.2012.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kamer K.J., Mootha V.K. MICU1 and MICU2 play nonredundant roles in the regulation of the mitochondrial calcium uniporter. EMBO Rep. 2014;15:299–307. doi: 10.1002/embr.201337946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kamer K.J., Grabarek Z., Mootha V.K. High-affinity cooperative Ca2+ binding by MICU 1– MICU 2 serves as an on–off switch for the uniporter. EMBO Rep. 2017;18:1397–1411. doi: 10.15252/embr.201643748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liu J.C., Liu J., Holmström K.M., Menazza S., Parks R.J., Fergusson M.M., Yu Z.X., Springer D.A., Halsey C., Liu C., et al. MICU1 serves as a molecular gatekeeper to prevent In vivo mitochondrial calcium overload. Cell Rep. 2016;16:1561–1573. doi: 10.1016/j.celrep.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Payne R., Hoff H., Roskowski A., Foskett J.K. MICU2 restricts spatial crosstalk between InsP3R and MCU channels by regulating threshold and gain of MICU1-mediated inhibition and activation of MCU. Cell Rep. 2017;21:3141–3154. doi: 10.1016/j.celrep.2017.11.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Csordás G., Golenár T., Seifert E.L., Kamer K.J., Sancak Y., Perocchi F., Moffat C., Weaver D., De la Fuente S., Bogorad R., et al. MICU1 controls both the threshold and cooperative activation of the mitochondrial Ca2+ uniporter. Cell Metab. 2013;17:976–987. doi: 10.1016/j.cmet.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Patron M., Checchetto V., Raffaello A., Teardo E., VecellioReane D., Mantoan M., Granatiero V., Szabò I., DeStefani D., Rizzuto R. MICU1 and MICU2 finely tune the mitochondrial Ca2+ uniporter by exerting opposite effects on MCU activity. Mol. Cell. 2014;53:726–737. doi: 10.1016/j.molcel.2014.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tomar D., Dong Z., Shanmughapriya S., Koch D.A., Thomas T., Hoffman N.E., Timbalia S.A., Goldman S.J., Breves S.L., Corbally D.P., et al. MCUR1 is a scaffold factor for the MCU complex function and promotes mitochondrial bioenergetics. Cell Rep. 2016;15:1673–1685. doi: 10.1016/j.celrep.2016.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Palty R., Silverman W.F., Hershfinkel M., Caporale T., Sensi S.L., Parnis J., Nolte C., Fishman D., Shoshan-Barmatz V., Herrmann S., et al. NCLX is an essential component of mitochondrial Na+/Ca2+ exchange. Proc. Natl. Acad. Sci. USA. 2010;107:436–441. doi: 10.1073/pnas.0908099107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Rizzuto R., De Stefani D., Raffaello A., Mammucari C. Mitochondria as sensors and regulators of calcium signalling. Nat. Rev. Mol. Cell Biol. 2012;13:566–578. doi: 10.1038/nrm3412. [DOI] [PubMed] [Google Scholar]
- 98.Gilabert J., Parekh A. Respiring mitochondria determine the pattern of activation and inactivation of the store-operated Ca(2+) current I(CRAC) EMBO J. 2000;19:6401–6407. doi: 10.1093/emboj/19.23.6401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Pacher P., Thomas A.P., Hajnóczky G. Ca2+ marks: Miniature calcium signals in single mitochondria driven by ryanodine receptors. Proc. Natl. Acad. Sci. USA. 2002;99:2380–2385. doi: 10.1073/pnas.032423699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nita I.I., Hershfinkel M., Fishman D., Ozeri E., Rutter G.A., Sensi S.L., Khananshvili D., Lewis E.C., Sekler I. The mitochondrial Na +/Ca2+ exchanger upregulates glucose dependent Ca2+ signalling linked to insulin secretion. PLoS One. 2012;7 doi: 10.1371/journal.pone.0046649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nita I.I., Caspi Y., Gudes S., Fishman D., Lev S., Hersfinkel M., Sekler I., Binshtok A.M. Privileged crosstalk between TRPV1 channels and mitochondrial calcium shuttling machinery controls nociception. Biochim. Biophys. Acta - Mol. Cell Res. 2016;1863:2868–2880. doi: 10.1016/j.bbamcr.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 102.Glancy B., Willis W.T., Chess D.J., Balaban R.S. Effect of calcium on the oxidative phosphorylation cascade in skeletal muscle mitochondria. Biochemistry. 2013;52:2793–2809. doi: 10.1021/bi3015983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Arnold S., Kadenbach B. Cell respiration is controlled by ATP, an allosteric inhibitor of cytochrome-C oxidase. Eur. J. Biochem. 1997;249:350–354. doi: 10.1111/j.1432-1033.1997.t01-1-00350.x. [DOI] [PubMed] [Google Scholar]
- 104.Panov A.V., Scaduto R.C. Influence of calcium on NADH and succinate oxidation by rat heart submitochondrial particles. Arch. Biochem. Biophys. 1995;316:815–820. doi: 10.1006/abbi.1995.1109. [DOI] [PubMed] [Google Scholar]
- 105.McCormack J.G., Denton R.M. Intracellular calcium ions and intramitochondrial Ca2+ in the regulation of energy metabolism in mammalian tissues. Proc. Nutr. Soc. 1990;49:57–75. doi: 10.1079/PNS19900009. [DOI] [PubMed] [Google Scholar]
- 106.Territo P.R., Mootha V.K., French S.A., Balaban R.S. Ca2+ activation of heart mitochondrial oxidative phosphorylation: Role of the F0/F1-ATPase. Am. J. Physiol. Cell Physiol. 2000;278 doi: 10.1152/ajpcell.2000.278.2.C423. [DOI] [PubMed] [Google Scholar]
- 107.Tretter L., Takacs K., Kövér K., Adam-Vizi V. Stimulation of H2O2 generation by calcium in brain mitochondria respiring on α-glycerophosphate. J. Neurosci. Res. 2007;85:3471–3479. doi: 10.1002/jnr.21405. [DOI] [PubMed] [Google Scholar]
- 108.Vaarmann A., Mandel M., Zeb A., Wareski P., Liiv J., Kuum M., Antsov E., Liiv M., Cagalinec M., Choubey V., et al. Mitochondrial biogenesis is required for axonal growth. Dev. 2016;143:1981–1992. doi: 10.1242/dev.128926. [DOI] [PubMed] [Google Scholar]
- 109.Haworth R.A., Hunter D.R. The Ca2+-induced membrane transition in mitochondria. II. Nature of the Ca2+ trigger site. Arch. Biochem. Biophys. 1979;195:460–467. doi: 10.1016/0003-9861(79)90372-2. [DOI] [PubMed] [Google Scholar]
- 110.Baines C.P., Kaiser R.A., Purcell N.H., Blair N.S., Osinska H., Hambleton M.A., Brunskill E.W., Sayen M.R., Gottlieb R.A., Dorn G.W., et al. Loss of cyclophilin D reveals a critical role for mitochondrial permeability transition in cell death. Nature. 2005;434:658–662. doi: 10.1038/nature03434. [DOI] [PubMed] [Google Scholar]
- 111.Berman S.B., Hastings T.G. Dopamine oxidation alters mitochondrial respiration and induces permeability transition in brain mitochondria: Implications for Parkinson’s disease. J. Neurochem. 1999;73:1127–1137. doi: 10.1046/j.1471-4159.1999.0731127.x. [DOI] [PubMed] [Google Scholar]
- 112.Du H., Guo L., Fang F., Chen D., A Sosunov A., M McKhann G., Yan Y., Wang C., Zhang H., Molkentin J.D., et al. Cyclophilin D deficiency attenuates mitochondrial and neuronal perturbation and ameliorates learning and memory in Alzheimer’s disease. Nat. Med. 2008;14:1097–1105. doi: 10.1038/nm.1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Schinzel A.C., Takeuchi O., Huang Z., Fisher J.K., Zhou Z., Rubens J., Hetz C., Danial N.N., Moskowitz M.A., Korsmeyer S.J. Cyclophilin D is a component of mitochondrial permeability transition and mediates neuronal cell death after focal cerebral ischemia. Proc. Natl. Acad. Sci. USA. 2005;102:12005–12010. doi: 10.1073/pnas.0505294102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wang X., Carlsson Y., Basso E., Zhu C., Rousset C.I., Rasola A., Johansson B.R., Blomgren K., Mallard C., Bernardi P., et al. Developmental shift of cyclophilin D contribution to hypoxic-ischemic brain injury. J. Neurosci. 2009;29:2588–2596. doi: 10.1523/JNEUROSCI.5832-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Crompton M. The mitochondrial permeabitity transition pore and its role in cell death. Biochem. J. 1999;341:233–249. doi: 10.1042/bj3410233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rizzuto R., Pinton P., Carrington W., Fay F.S., Fogarty K.E., Lifshitz L.M., Tuft R.A., Pozzan T. Close contacts with the endoplasmic reticulum as determinants of mitochondrial Ca2+ responses. Science. 1998;280:1763–1766. doi: 10.1126/science.280.5370.1763. [DOI] [PubMed] [Google Scholar]
- 117.Achleitner G., Gaigg B., Krasser A., Kainersdorfer E., Kohlwein S.D., Perktold A., Zellnig G., Daum G. Association between the endoplasmic reticulum and mitochondria of yeast facilitates interorganelle transport of phospholipids through membrane contact. Eur. J. Biochem. 1999;264:545–553. doi: 10.1046/j.1432-1327.1999.00658.x. [DOI] [PubMed] [Google Scholar]
- 118.Hayashi T., Rizzuto R., Hajnoczky G., Su T.P. MAM: More than just a housekeeper. Trends Cell Biol. 2009;19:81–88. doi: 10.1016/j.tcb.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Eisner V., Csordás G., Hajnóczky G. Interactions between sarco-endoplasmic reticulum and mitochondria in cardiac and skeletal muscle-pivotal roles in Ca2+ and reactive oxygen species signaling. J. Cell Sci. 2013;126:2965–2978. doi: 10.1242/jcs.093609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Csordás G., Várnai P., Golenár T., Roy S., Purkins G., Schneider T.G., Balla T., Hajnóczky G. Imaging interorganelle contacts and local calcium dynamics at the ER-mitochondrial interface. Mol. Cell. 2010;39:121–132. doi: 10.1016/j.molcel.2010.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Witherspoon M., Sandu D., Lu C., Wang K., Edwards R., Yeung A., Gelincik O., Manfredi G., Gross S., Kopelovich L., et al. ETHE1 overexpression promotes SIRT1 and PGC1α mediated aerobic glycolysis, oxidative phosphorylation, mitochondrial biogenesis and colorectal cancer. Oncotarget. 2019;10:4004–4017. doi: 10.18632/oncotarget.26958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Szabadkai G., Bianchi K., Várnai P., De Stefani D., Wieckowski M.R., Cavagna D., Nagy A.I., Balla T., Rizzuto R. Chaperone-mediated coupling of endoplasmic reticulum and mitochondrial Ca2+ channels. J. Cell Biol. 2006;175:901–911. doi: 10.1083/jcb.200608073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Filadi R., Greotti E., Turacchio G., Luini A., Pozzan T., Pizzo P. Mitofusin 2 ablation increases endoplasmic reticulum-mitochondria coupling. Proc. Natl. Acad. Sci. USA. 2015;112:E2174–E2181. doi: 10.1073/pnas.1504880112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.De vos K.J., Mórotz G.M., Stoica R., Tudor E.L., Lau K.F., Ackerley S., Warley A., Shaw C.E., Miller C.C. VAPB interacts with the mitochondrial protein PTPIP51 to regulate calcium homeostasis. Hum. Mol. Genet. 2012;21:1299–1311. doi: 10.1093/hmg/ddr559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Stoica R., De Vos K.J., Paillusson S., Mueller S., Sancho R.M., Lau K.F., Vizcay-Barrena G., Lin W.L., Xu Y.F., Lewis J., et al. ER-mitochondria associations are regulated by the VAPB-PTPIP51 interaction and are disrupted by ALS/FTD-associated TDP-43. Nat. Commun. 2014;5 doi: 10.1038/ncomms4996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Simmen T., Aslan J.E., Blagoveshchenskaya A.D., Thomas L., Wan L., Xiang Y., Feliciangeli S.F., Hung C.H., Crump C.M., Thomas G. PACS-2 controls endoplasmic reticulum-mitochondria communication and Bid-mediated apoptosis. EMBO J. 2005;24:717–729. doi: 10.1038/sj.emboj.7600559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hedskog L., Pinho C.M., Filadi R., Rönnbäck A., Hertwig L., Wiehager B., Larssen P., Gellhaar S., Sandebring A., Westerlund M., et al. Modulation of the endoplasmic reticulum-mitochondria interface in Alzheimer’s disease and related models. Proc. Natl. Acad. Sci. USA. 2013;110:7916–7921. doi: 10.1073/pnas.1300677110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hayashi T., Fujimoto M. Detergent-resistant microdomains determine the localization of σ-1 receptors to the endoplasmic reticulum-mitochondria junction. Mol. Pharmacol. 2010;77:517–528. doi: 10.1124/mol.109.062539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Arasaki K., Shimizu H., Mogari H., Nishida N., Hirota N., Furuno A., Kudo Y., Baba M., Baba N., Cheng J., et al. A Role for the ancient SNARE syntaxin 17 in regulating mitochondrial division. Dev. Cell. 2015;32:304–317. doi: 10.1016/j.devcel.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 130.Rieusset J. The role of endoplasmic reticulum-mitochondria contact sites in the control of glucose homeostasis: An update. Cell Death Dis. 2018;9 doi: 10.1038/s41419-018-0416-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lee H.J., Jung Y.H., Choi G.E., Kim J.S., Chae C.W., Lim J.R., Kim S.Y., Yoon J.H., Cho J.H., Lee S.J., et al. Urolithin A suppresses high glucose-induced neuronal amyloidogenesis by modulating TGM2-dependent ER-mitochondria contacts and calcium homeostasis. Cell Death Differ. 2021;28:184–202. doi: 10.1038/s41418-020-0593-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Iwasawa R., Mahul-Mellier A.L., Datler C., Pazarentzos E., Grimm S. Fis1 and Bap31 bridge the mitochondria-ER interface to establish a platform for apoptosis induction. EMBO J. 2011;30:556–568. doi: 10.1038/emboj.2010.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Qian T., Herman B., Lemasters J.J. The mitochondrial permeability transition mediates both necrotic and apoptotic death of hepatocytes exposed to Br-A23187. Toxicol. Appl. Pharmacol. 1999;154:117–125. doi: 10.1006/taap.1998.8580. [DOI] [PubMed] [Google Scholar]
- 134.Vander Heiden M.G., Chandel N.S., Li X.X., Schumacker P.T., Colombini M., Thompson C.B. Outer mitochondrial membrane permeability can regulate coupled respiration and cell survival. Proc. Natl. Acad. Sci. USA. 2000;97:4666–4671. doi: 10.1073/pnas.090082297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cerella C., Diederich M., Ghibelli L. The dual role of calcium as messenger and stressor in cell damage, death, and survival. Int. J. Cell Biol. 2010;2010:14. doi: 10.1155/2010/546163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Tajes M., Eraso-Pichot A., Rubio-Moscardó F., Guivernau B., Ramos-Fernández E., Bosch-Morató M., Guix F.X., Clarimón J., Miscione G.P., Boada M., et al. Methylglyoxal produced by amyloid-β peptide-induced nitrotyrosination of triosephosphate isomerase triggers neuronal death in alzheimer’s disease. J. Alzheimer’s Dis. 2014;41:273–288. doi: 10.3233/JAD-131685. [DOI] [PubMed] [Google Scholar]
- 137.Tajes M., Eraso-Pichot A., Rubio-Moscardó F., Guivernau B., Bosch-Morató M., Valls-Comamala V., Muñoz F.J. Methylglyoxal reduces mitochondrial potential and activates Bax and caspase-3 in neurons: Implications for Alzheimer’s disease. Neurosci. Lett. 2014;580:78–82. doi: 10.1016/j.neulet.2014.07.047. [DOI] [PubMed] [Google Scholar]
- 138.Henshall D.C., Bonislawski D.P., Skradski S.L., Araki T., Lan J.Q., Schindler C.K., Meller R., Simon R.P. Formation of the Apaf-1/cytochrome c complex precedes activation of caspase-9 during seizure-induced neuronal death. Cell Death Differ. 2001;8:1169–1181. doi: 10.1038/sj.cdd.4400921. [DOI] [PubMed] [Google Scholar]
- 139.Suárez-Rivero J., Villanueva-Paz M., de la Cruz-Ojeda P., de la Mata M., Cotán D., Oropesa-Ávila M., de Lavera I., Álvarez-Córdoba M., Luzón-Hidalgo R., Sánchez-Alcázar J. Mitochondrial dynamics in mitochondrial diseases. Diseases. 2016;5:1. doi: 10.3390/diseases5010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Twig G., Elorza A., Molina A.J.A., Mohamed H., Wikstrom J.D., Walzer G., Stiles L., Haigh S.E., Katz S., Las G., et al. Fission and selective fusion govern mitochondrial segregation and elimination by autophagy. EMBO J. 2008;27:433–446. doi: 10.1038/sj.emboj.7601963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Martin L.J. The mitochondrial permeability transition pore: A molecular target for amyotrophic lateral sclerosis therapy. Biochim. Biophys. Acta Mol. Basis Dis. 2010;1802:186–197. doi: 10.1016/j.bbadis.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Keep M., Elmér E., Fong K.S.K., Csiszar K. Intrathecal cyclosporin prolongs survival of late-stage ALS mice. Brain Res. 2001;894:327–331. doi: 10.1016/S0006-8993(01)02012-1. [DOI] [PubMed] [Google Scholar]
- 143.Sasaki S., Iwata M. Ultrastructural change of synapses of Betz cells in patients with amyotrophic lateral sclerosis. Neurosci. Lett. 1999;268:29–32. doi: 10.1016/S0304-3940(99)00374-2. [DOI] [PubMed] [Google Scholar]
- 144.Thomas B., Banerjee R., Starkova N.N., Zhang S.F., Calingasan N.Y., Yang L., Wille E., Lorenzo B.J., Ho D.J., Beal M.F., et al. Mitochondrial permeability transition pore component cyclophilin D distinguishes nigrostriatal dopaminergic death paradigms in the MPTP mouse model of Parkinson’s disease. Antioxidants Redox Signal. 2012;16:855–868. doi: 10.1089/ars.2010.3849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Quintanilla R.A., Johnson G.V.W. Role of mitochondrial dysfunction in the pathogenesis of Huntington’s disease. Brain Res. Bull. 2009;80:242–247. doi: 10.1016/j.brainresbull.2009.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Choo Y.S., Johnson G.V.W., MacDonald M., Detloff P.J., Lesort M. Mutant huntingtin directly increases susceptibility of mitochondria to the calcium-induced permeability transition and cytochrome c release. Hum. Mol. Genet. 2004;13:1407–1420. doi: 10.1093/hmg/ddh162. [DOI] [PubMed] [Google Scholar]
- 147.Miranda S., Opazo C., Larrondo L.F., Muñoz F.J., Ruiz F., Leighton F., Inestrosa N.C. The role of oxidative stress in the toxicity induced by amyloid β-peptide in Alzheimer’s disease. Prog. Neurobiol. 2000;62:633–648. doi: 10.1016/S0301-0082(00)00015-0. [DOI] [PubMed] [Google Scholar]
- 148.Szalai G., Krishnamurthy R., Hajnóczky G. Apoptosis driven by IP3-linked mitochondrial calcium signals. EMBO J. 1999;18:6349–6361. doi: 10.1093/emboj/18.22.6349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Sharov V.S., Dremina E.S., Galeva N.A., Williams T.D., Schöneich C. Quantitative mapping of oxidation-sensitive cysteine residues in SERCA in vivo and in vitro by HPLC-electrospray-tandem MS: Selective protein oxidation during biological aging. Biochem. J. 2006;394:605–615. doi: 10.1042/BJ20051214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hou T., Zhang X., Xu J., Jian C., Huang Z., Ye T., Hu K., Zheng M., Gao F., Wang X., et al. Synergistic triggering of superoxide flashes by mitochondrial Ca2+ uniport and basal reactive oxygen species elevation. J. Biol. Chem. 2013;288:4602–4612. doi: 10.1074/jbc.M112.398297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Balaban R.S., Nemoto S., Finkel T. Mitochondria, oxidants, and aging. Cell. 2005;120:483–495. doi: 10.1016/j.cell.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 152.Wojsiat J., Zoltowska K.M., Laskowska-Kaszub K., Wojda U. Oxidant/antioxidant imbalance in Alzheimer’s disease: Therapeutic and diagnostic prospects. Oxid. Med. Cell. Longev. 2018:2018. doi: 10.1155/2018/6435861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kumar A., Yegla B., Foster T.C. Redox signaling in neurotransmission and cognition during aging. Antioxidants Redox Signal. 2018;28:1724–1745. doi: 10.1089/ars.2017.7111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Tian L., Potus F., Wu D., Dasgupta A., Chen K.-H., Mewburn J., Lima P., Archer S.L. Increased Drp1-mediated mitochondrial fission promotes proliferation and collagen production by right ventricular fibroblasts in experimental pulmonary arterial hypertension. Front. Physiol. 2018;9:828. doi: 10.3389/fphys.2018.00828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Jendrach M., Mai S., Pohl S., Vöth M., Bereiter-Hahn J. Short- and long-term alterations of mitochondrial morphology, dynamics and mtDNA after transient oxidative stress. Mitochondrion. 2008;8:293–304. doi: 10.1016/j.mito.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 156.Guix F.X., Uribesalgo I., Coma M., Muñoz F.J. The physiology and pathophysiology of nitric oxide in the brain. Prog. Neurobiol. 2005;76:126–152. doi: 10.1016/j.pneurobio.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 157.Picón-Pagès P., Garcia-Buendia J., Muñoz F.J. Functions and dysfunctions of nitric oxide in brain. Biochim. Biophys. Acta - Mol. Basis Dis. 2019;1865:1949–1967. doi: 10.1016/j.bbadis.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 158.Ghafourifar P., Cadenas E. Mitochondrial nitric oxide synthase. Trends Pharmacol. Sci. 2005;26:190–195. doi: 10.1016/j.tips.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 159.Brodsky S.V., Gao S., Li H., Goligorsky M.S. Hyperglycemic switch from mitochondrial nitric oxide to superoxide production in endothelial cells. Am. J. Physiol. - Hear. Circ. Physiol. 2002;283 doi: 10.1152/ajpheart.00196.2002. [DOI] [PubMed] [Google Scholar]
- 160.Dzurik R., Krivosikova Z., Stefikova K., Spustova V. Mitochondria and mitochondrial nitric oxide synthase alterations participate in energetical dysbalance, aging and age-related diseases—PubMed. Bratisl. Lek. Listy. 2006;107:405–411. [PubMed] [Google Scholar]
- 161.Nisoli E., Clementi E., Paolucci C., Cozzi V., Tonello C., Sciorati C., Bracale R., Valerio A., Francolini M., Moncada S., et al. Mitochondrial biogenesis in mammals: The role of endogenous nitric oxide. Science. 2003;299:896–899. doi: 10.1126/science.1079368. [DOI] [PubMed] [Google Scholar]
- 162.Alvarez S., Valdez L.B., Zaobornyj T., Boveris A. Oxygen dependence of mitochondrial nitric oxide synthase activity. Biochem. Biophys. Res. Commun. 2003;305:771–775. doi: 10.1016/S0006-291X(03)00818-0. [DOI] [PubMed] [Google Scholar]
- 163.Sarti P., Giuffré A., Forte E., Mastronicola D., Barone M.C., Brunori M. Nitric oxide and cytochrome C oxidase: Mechanisms of inhibition and NO degradation. Biochem. Biophys. Res. Commun. 2000;274:183–187. doi: 10.1006/bbrc.2000.3117. [DOI] [PubMed] [Google Scholar]
- 164.Brookes P.S., Padilla Salinas E., Darley-Usmar K., Eiserich J.P., Freeman B.A., Darley-Usmar V.M., Anderson P.G. Concentration-dependent effects of nitric oxide on mitochondrial permeability transition and cytochrome c release. J. Biol. Chem. 2000;275:20474–20479. doi: 10.1074/jbc.M001077200. [DOI] [PubMed] [Google Scholar]
- 165.Mannick J.B., Schonhoff C., Papeta N., Ghafourifar P., Szibor M., Fang K., Gaston B. S-nitrosylation of mitochondrial caspases. J. Cell Biol. 2001;154:1111–1116. doi: 10.1083/jcb.200104008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.ILL-Raga G., Palomer E., Ramos-Fernández E., Guix F.X., Bosch-Morató M., Guivernau B., Tajes M., Valls-Comamala V., Jiménez-Conde J., Ois A., et al. Fibrinogen nitrotyrosination after ischemic stroke impairs thrombolysis and promotes neuronal death. Biochim. Biophys. Acta - Mol. Basis Dis. 2015;1852:421–428. doi: 10.1016/j.bbadis.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 167.Tajes M., Ill-Raga G., Palomer E., Ramos-Fernández E., Guix F.X., Bosch-Morató M., Guivernau B., Jiménez-Conde J., Ois A., Pérez-Asensio F., et al. Nitro-oxidative stress after neuronal ischemia induces protein nitrotyrosination and cell death. Oxid. Med. Cell. Longev. 2013;2013 doi: 10.1155/2013/826143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Muñoz F.J., Opazo C., Gil-Gómez G., Tapia G., Fernández V., Valverde M.A., Inestrosa N.C. Vitamin E but not 17β-estradiol protects against vascular toxicity induced by β-amyloid wild type and the dutch amyloid variant. J. Neurosci. 2002;22:3081–3089. doi: 10.1523/JNEUROSCI.22-08-03081.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Coma M., Guix F.X., Uribesalgo I., Espuña G., Solé M., Andreu D., Muñoz F.J., Muñoz F.J. Lack of oestrogen protection in amyloid-mediated endothelial damage due to protein nitrotyrosination. Brain. 2005;128:1613–1621. doi: 10.1093/brain/awh492. [DOI] [PubMed] [Google Scholar]
- 170.Fernandez A., Meechan D.W., Karpinski B.A., Paronett E.M., Bryan C.A., Rutz H.L., Radin E.A., Lubin N., Bonner E.R., Popratiloff A., et al. Mitochondrial dysfunction leads to cortical under-connectivity and cognitive impairment. Neuron. 2019;102:1127–1142.e3. doi: 10.1016/j.neuron.2019.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Netto M.B., de Oliveira Junior A.N., Goldim M., Mathias K., Fileti M.E., da Rosa N., Laurentino A.O., de Farias B.X., Costa A.B., Rezin G.T., et al. Oxidative stress and mitochondrial dysfunction contributes to postoperative cognitive dysfunction in elderly rats. Brain. Behav. Immun. 2018;73:661–669. doi: 10.1016/j.bbi.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 172.Lin M.T., Beal M.F. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature. 2006;443:787–795. doi: 10.1038/nature05292. [DOI] [PubMed] [Google Scholar]
- 173.Elfawy H.A., Das B. Crosstalk between mitochondrial dysfunction, oxidative stress, and age related neurodegenerative disease: Etiologies and therapeutic strategies. Life Sci. 2019;218:165–184. doi: 10.1016/j.lfs.2018.12.029. [DOI] [PubMed] [Google Scholar]
- 174.Cabeza R. Hemispheric asymmetry reduction in older adults: The HAROLD model. Psychol. Aging. 2002;17:85–100. doi: 10.1037/0882-7974.17.1.85. [DOI] [PubMed] [Google Scholar]
- 175.Park D.C., Reuter-Lorenz P. The adaptive brain: Aging and neurocognitive scaffolding. Annu. Rev. Psychol. 2009;60:173–196. doi: 10.1146/annurev.psych.59.103006.093656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Bishop N.A., Lu T., Yankner B.A. Neural mechanisms of ageing and cognitive decline. Nature. 2010;464:529–535. doi: 10.1038/nature08983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Andrews-Hanna J.R., Snyder A.Z., Vincent J.L., Lustig C., Head D., Raichle M.E.E., Buckner R.L. Disruption of large-scale brain systems in advanced aging. Neuron. 2007;56:924–935. doi: 10.1016/j.neuron.2007.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Onyango I.G., Lu J., Rodova M., Lezi E., Crafter A.B., Swerdlow R.H. Regulation of neuron mitochondrial biogenesis and relevance to brain health. Biochim. Biophys. Acta Mol. Basis Dis. 2010;1802:228–234. doi: 10.1016/j.bbadis.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 179.Ojaimi J., Masters C.L., Opeskin K., McKelvie P., Byrne E. Mitochondrial respiratory chain activity in the human brain as a function of age. Mech. Ageing Dev. 1999;111:39–47. doi: 10.1016/S0047-6374(99)00071-8. [DOI] [PubMed] [Google Scholar]
- 180.Petrosillo G., Matera M., Casanova G., Ruggiero F.M., Paradies G. Mitochondrial dysfunction in rat brain with aging. Involvement of complex I, reactive oxygen species and cardiolipin. Neurochem. Int. 2008;53:126–131. doi: 10.1016/j.neuint.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 181.Kaur Sandhu S., Kaur G. Mitochondrial electron transport chain complexes in aging rat brain and lymphocytes. Biogerontology. 2003;4:19–29. doi: 10.1023/A:1022473219044. [DOI] [PubMed] [Google Scholar]
- 182.Mattson M.P., Magnus T. Ageing and neuronal vulnerability. Nat. Rev. Neurosci. 2006;7:278–294. doi: 10.1038/nrn1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Shoshan-Barmatz V., Maldonado E., Krelin Y. VDAC1 at the crossroads of cell metabolism, apoptosis and cell stress. Cell Stress. 2017;1:11–36. doi: 10.15698/cst2017.10.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Rottenberg H., Hoek J.B. The path from mitochondrial ROS to aging runs through the mitochondrial permeability transition pore. Aging Cell. 2017;16:943–955. doi: 10.1111/acel.12650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Harman D. Aging: A theory based on free radical and radiation chemistry. J. Gerontol. 1956;11:298–300. doi: 10.1093/geronj/11.3.298. [DOI] [PubMed] [Google Scholar]
- 186.Kennedy S.R., Salk J.J., Schmitt M.W., Loeb L.A. Ultra-sensitive sequencing reveals an age-related increase in somatic mitochondrial mutations that are inconsistent with oxidative damage. PLoS Genet. 2013;9 doi: 10.1371/journal.pgen.1003794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Vermulst M., Wanagat J., Kujoth G.C., Bielas J.H., Rabinovitch P.S., Prolla T.A., Loeb L.A. DNA deletions and clonal mutations drive premature aging in mitochondrial mutator mice. Nat. Genet. 2008;40:392–394. doi: 10.1038/ng.95. [DOI] [PubMed] [Google Scholar]
- 188.Schampel A., Kuerten S. Danger: High voltage—the role of Voltage-Gated Calcium Channels in central nervous system pathology. Cells. 2017;6:43. doi: 10.3390/cells6040043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Kaguni L. DNA polymerase gamma, the mitochondrial replicase. Annu. Rev. Biochem. 2004;73:293–320. doi: 10.1146/annurev.biochem.72.121801.161455. [DOI] [PubMed] [Google Scholar]
- 190.Pavlov P., Hutter-Paier B., Havas D., Windisch M., Winblad B. Development of GMP-1 a molecular chaperone network modulator protecting mitochondrial function and its assessment in fly and mice models of Alzheimer’s disease. J. Cell. Mol. Med. 2018;22:3464–3474. doi: 10.1111/jcmm.13624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Polo M., Alegre F., Moragrega A., Gibellini L., Marti-Rodrigo A., Blas-Garcia A., Esplugues J., Apostolova N. Lon protease: A novel mitochondrial matrix protein in the interconnection between drug-induced mitochondrial dysfunction and endoplasmic reticulum stress. Br. J. Pharmacol. 2017;174:4409–4429. doi: 10.1111/bph.14045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Fiorese C., Schulz A., Lin Y., Rosin N., Pellegrino M., Haynes C. The Transcription Factor ATF5 Mediates a Mammalian Mitochondrial UPR. Curr. Biol. 2016;26:2037–2043. doi: 10.1016/j.cub.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Papa L., Germain D. Estrogen receptor mediates a distinct mitochondrial unfolded protein response. J. Cell Sci. 2011;124:1396–1402. doi: 10.1242/jcs.078220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Casley C.S., Canevari L., Land J.M., Clark J.B., Sharpe M.A. β-Amyloid inhibits integrated mitochondrial respiration and key enzyme activities. J. Neurochem. 2002;80:91–100. doi: 10.1046/j.0022-3042.2001.00681.x. [DOI] [PubMed] [Google Scholar]
- 195.Michikawa Y., Mazzucchelli F., Bresolin N., Scarlato G., Attardi G. Aging-dependent large accumulation of point mutations in the human mtDNA control region for replication. Science. 1999;286:774–779. doi: 10.1126/science.286.5440.774. [DOI] [PubMed] [Google Scholar]
- 196.Franceschi C., Garagnani P., Parini P., Giuliani C., Santoro A. Inflammaging: A new immune–metabolic viewpoint for age-related diseases. Nat. Rev. Endocrinol. 2018;14:576–590. doi: 10.1038/s41574-018-0059-4. [DOI] [PubMed] [Google Scholar]
- 197.Adler A.S., Sinha S., Kawahara T.L.A., Zhang J.Y., Segal E., Chang H.Y. Motif module map reveals enforcement of aging by continual NF-κB activity. Genes Dev. 2007;21:3244–3257. doi: 10.1101/gad.1588507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Zhang R., Liu Y., Yan K., Chen L., Chen X.R., Li P., Chen F.F., Jiang X.D. Anti-inflammatory and immunomodulatory mechanisms of mesenchymal stem cell transplantation in experimental traumatic brain injury. J. Neuroinflamm. 2013;10:871. doi: 10.1186/1742-2094-10-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Tilstra J.S., Clauson C.L., Niedernhofer L.J., Robbins P.D. NF-κB in aging and disease. Aging Dis. 2011;2(6):449–465. [PMC free article] [PubMed] [Google Scholar]
- 200.Naik E., Dixit V.M. Mitochondrial reactive oxygen species drive proinflammatory cytokine production. J. Exp. Med. 2011;208:417–420. doi: 10.1084/jem.20110367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Swacha P., Gekara N.O., Erttmann S.F. Methods in Enzymology. Volume 625. Academic Press Inc.; Cambridge, MA, USA: 2019. Biochemical and microscopic analysis of inflammasome complex formation; pp. 287–298. [DOI] [PubMed] [Google Scholar]
- 202.Yuk J.M., Silwal P., Jo E.K. Inflammasome and mitophagy connection in health and disease. Int. J. Mol. Sci. 2020;21:4714. doi: 10.3390/ijms21134714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Horner S.M., Liu H.M., Park H.S., Briley J., Gale M. Mitochondrial-associated endoplasmic reticulum membranes (MAM) form innate immune synapses and are targeted by hepatitis C virus. Proc. Natl. Acad. Sci. USA. 2011;108:14590–14595. doi: 10.1073/pnas.1110133108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Zhou R., Yazdi A.S., Menu P., Tschopp J. A role for mitochondria in NLRP3 inflammasome activation. Nature. 2011;469:221–226. doi: 10.1038/nature09663. [DOI] [PubMed] [Google Scholar]
- 205.Lu M., Yin N., Liu W., Cui X., Chen S., Wang E. Curcumin ameliorates diabetic nephropathy by suppressing NLRP3 inflammasome signaling. Biomed Res. Int. 2017;2017:1–10. doi: 10.1155/2017/1516985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Baroja-Mazo A., Martín-Sánchez F., Gomez A.I., Martínez C.M., Amores-Iniesta J., Compan V., Barberà-Cremades M., Yagüe J., Ruiz-Ortiz E., Antón J., et al. The NLRP3 inflammasome is released as a particulate danger signal that amplifies the inflammatory response. Nat. Immunol. 2014;15:738–748. doi: 10.1038/ni.2919. [DOI] [PubMed] [Google Scholar]
- 207.Booth D.M., Enyedi B., Geiszt M., Várnai P., Hajnóczky G. Redox nanodomains are induced by and control calcium signaling at the ER-mitochondrial interface. Mol. Cell. 2016;63:240–248. doi: 10.1016/j.molcel.2016.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Marchi S., Patergnani S., Pinton P. The endoplasmic reticulum-mitochondria connection: One touch, multiple functions. Biochim. Biophys. Acta - Bioenerg. 2014;1837:461–469. doi: 10.1016/j.bbabio.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 209.Schrader M., Costello J.L., Godinho L.F., Azadi A.S., Islinger M. Proliferation and fission of peroxisomes - An update. Biochim. Biophys. Acta - Mol. Cell Res. 2016;1863:971–983. doi: 10.1016/j.bbamcr.2015.09.024. [DOI] [PubMed] [Google Scholar]
- 210.De Mario A., Quintana-Cabrera R., Martinvalet D., Giacomello M. (Neuro)degenerated mitochondria-ER contacts. Biochem. Biophys. Res. Commun. 2017;483:1096–1109. doi: 10.1016/j.bbrc.2016.07.056. [DOI] [PubMed] [Google Scholar]
- 211.Rea I.M., Gibson D.S., McGilligan V., McNerlan S.E., Denis Alexander H., Ross O.A. Age and age-related diseases: Role of inflammation triggers and cytokines. Front. Immunol. 2018;9 doi: 10.3389/fimmu.2018.00586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Chung K., Dhillon P., Huang S., Sheng X., Shrestha R., Qiu C., Kaufman B., Park J., Pei L., Baur J., et al. Mitochondrial Damage and Activation of the STING Pathway Lead to Renal Inflammation and Fibrosis. Cell Metab. 2019;30:784–799.e5. doi: 10.1016/j.cmet.2019.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Seth R., Sun L., Ea C., Chen Z. Identification and characterization of MAVS, a mitochondrial antiviral signaling protein that activates NF-kappaB and IRF 3. Cell. 2005;122:669–682. doi: 10.1016/j.cell.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 214.Yoneyama M., Kikuchi M., Natsukawa T., Shinobu N., Imaizumi T., Miyagishi M., Taira K., Akira S., Fujita T. The RNA helicase RIG-I has an essential function in double-stranded RNA-induced innate antiviral responses. Nat. Immunol. 2004;5:730–737. doi: 10.1038/ni1087. [DOI] [PubMed] [Google Scholar]
- 215.Moore C., Bergstralh D., Duncan J., Lei Y., Morrison T., Zimmermann A., Accavitti-Loper M., Madden V., Sun L., Ye Z., et al. NLRX1 is a regulator of mitochondrial antiviral immunity. Nature. 2008;451:573–577. doi: 10.1038/nature06501. [DOI] [PubMed] [Google Scholar]
- 216.Oganesyan G., Saha S., Guo B., He J., Shahangian A., Zarnegar B., Perry A., Cheng G. Critical role of TRAF3 in the Toll-like receptor-dependent and -independent antiviral response. Nature. 2006;439:208–211. doi: 10.1038/nature04374. [DOI] [PubMed] [Google Scholar]
- 217.Mills E., Kelly B., Logan A., Costa A., Varma M., Bryant C., Tourlomousis P., Däbritz J., Gottlieb E., Latorre I., et al. Succinate dehydrogenase supports metabolic repurposing of mitochondria to drive inflammatory macrophages. Cell. 2016;167:457–470.e13. doi: 10.1016/j.cell.2016.08.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Collins L., Hajizadeh S., Holme E., Jonsson I., Tarkowski A. Endogenously oxidized mitochondrial DNA induces in vivo and in vitro inflammatory responses. J. Leukoc. Biol. 2004;75:995–1000. doi: 10.1189/jlb.0703328. [DOI] [PubMed] [Google Scholar]
- 219.Iyer S., He Q., Janczy J., Elliott E., Zhong Z., Olivier A., Sadler J., Knepper-Adrian V., Han R., Qiao L., et al. Mitochondrial cardiolipin is required for Nlrp3 inflammasome activation. Immunity. 2013;39:311–323. doi: 10.1016/j.immuni.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Wenceslau C., McCarthy C., Goulopoulou S., Szasz T., NeSmith E., Webb R. Mitochondrial-derived N-formyl peptides: Novel links between trauma, vascular collapse and sepsis. Med. Hypotheses. 2013;81:532–535. doi: 10.1016/j.mehy.2013.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Julian M., Shao G., Vangundy Z., Papenfuss T., Crouser E. Mitochondrial transcription factor A, an endogenous danger signal, promotes TNFα release via RAGE- and TLR9-responsive plasmacytoid dendritic cells. PLoS ONE. 2013;8 doi: 10.1371/journal.pone.0072354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Havrankova J., Roth J., Brownstein M.J. Concentrations of insulin and of insulin receptors in the brain are independent of peripheral insulin levels. Studies of obese and streptozotocin-treated rodents. J. Clin. Invest. 1979;64:636–642. doi: 10.1172/JCI109504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Park C.R., Seeley R.J., Craft S., Woods S.C. Intracerebroventricular insulin enhances memory in a passive-avoidance task. Physiol. Behav. 2000;68:509–514. doi: 10.1016/S0031-9384(99)00220-6. [DOI] [PubMed] [Google Scholar]
- 224.Van Der Heide L.P., Kamal A., Artola A., Gispen W.H., Ramakers G.M.J. Insulin modulates hippocampal activity-dependent synaptic plasticity in a N-methyl-D-aspartate receptor and phosphatidyl-inositol-3-kinase-dependent manner. J. Neurochem. 2005;94:1158–1166. doi: 10.1111/j.1471-4159.2005.03269.x. [DOI] [PubMed] [Google Scholar]
- 225.Ryu B.R., Ko H.W., Jou I., Noh J.S., Gwag B.J. Phosphatidylinositol 3-kinase-mediated regulation of neuronal apoptosis and necrosis by insulin and IGF-I. J. Neurobiol. 1999;39:536–546. doi: 10.1002/(SICI)1097-4695(19990615)39:4<536::AID-NEU7>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 226.Montgomery M.K., Turner N. Mitochondrial dysfunction and insulin resistance: An update. Endocr. Connect. 2015;4 doi: 10.1530/EC-14-0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Turner N., Bruce C.R., Beale S.M., Hoehn K.L., So T., Rolph M.S., Cooney G.J. Excess lipid availability increases mitochondrial fatty acid oxidative capacity in muscle: Evidence against a role for reduced fatty acid oxidation in lipid-induced insulin resistance in rodents. Diabetes. 2007;56:2085–2092. doi: 10.2337/db07-0093. [DOI] [PubMed] [Google Scholar]
- 228.Rivera E.J., Goldin A., Fulmer N., Tavares R., Wands J.R., De La Monte S.M. Insulin and insulin-like growth factor expression and function deteriorate with progression of Alzheimer’s disease: Link to brain reductions in acetylcholine. J. Alzheimer’s Dis. 2005;8:247–268. doi: 10.3233/JAD-2005-8304. [DOI] [PubMed] [Google Scholar]
- 229.Steen E., Terry B.M., Rivera E.J., Cannon J.L., Neely T.R., Tavares R., Xu X.J., Wands J.R., De La Monte S.M. Impaired insulin and insulin-like growth factor expression and signaling mechanisms in Alzheimer’s disease - Is this type 3 diabetes? J. Alzheimer’s Dis. 2005;7:63–80. doi: 10.3233/JAD-2005-7107. [DOI] [PubMed] [Google Scholar]
- 230.Smith L.M., Strittmatter S.M. Binding sites for amyloid-β oligomers and synaptic toxicity. Cold Spring Harb. Perspect. Med. 2017;7 doi: 10.1101/cshperspect.a024075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Wardelmann K., Blümel S., Rath M., Alfine E., Chudoba C., Schell M., Cai W., Hauffe R., Warnke K., Flore T., et al. Insulin action in the brain regulates mitochondrial stress responses and reduces diet-induced weight gain. Mol. Metab. 2019;21:68–81. doi: 10.1016/j.molmet.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Okouchi M., Okayama N., Steven Alexander J., Yee Aw T. NRF2-dependent glutamate-L-cysteine ligase catalytic subunit expression mediates insulin protection against hyperglycemia-induced brain endothelial cell apoptosis. Curr. Neurovasc. Res. 2006;3:249–261. doi: 10.2174/156720206778792876. [DOI] [PubMed] [Google Scholar]
- 233.Melser S., Lavie J., Bénard G. Mitochondrial degradation and energy metabolism. Biochim. Biophys. Acta Mol. Cell Res. 2015;1853:2812–2821. doi: 10.1016/j.bbamcr.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 234.Koo S.H., Satoh H., Herzig S., Lee C.H., Hedrick S., Kulkarni R., Evans R.M., Olefsky J., Montminy M. PGC-1 promotes insulin resistance in liver through PPAR-α-dependent induction of TRB-3. Nat. Med. 2004;10:530–534. doi: 10.1038/nm1044. [DOI] [PubMed] [Google Scholar]
- 235.Pagel-Langenickel I., Bao J., Joseph J.J., Schwartz D.R., Mantell B.S., Xu X., Raghavachari N., Sack M.N. PGC-1α integrates insulin signaling, mitochondrial regulation, and bioenergetic function in skeletal muscle. J. Biol. Chem. 2008;283:22464–22472. doi: 10.1074/jbc.M800842200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.McManus E.J., Sakamoto K., Armit L.J., Ronaldson L., Shpiro N., Marquez R., Alessi D.R. Role that phosphorylation of GSK3 plays in insulin and Wnt signalling defined by knockin analysis. EMBO J. 2005;24:1571–1583. doi: 10.1038/sj.emboj.7600633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Das S., Wong R., Rajapakse N., Murphy E., Steenbergen C. Glycogen synthase kinase 3 inhibition slows mitochondrial adenine nucleotide transport and regulates voltage-dependent anion channel phosphorylation. Circ. Res. 2008;103:983–991. doi: 10.1161/CIRCRESAHA.108.178970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Yang K., Chen Z., Gao J., Shi W., Li L., Jiang S., Hu H., Liu Z., Xu D., Wu L. The key roles of GSK-3β in regulating mitochondrial activity. Cell. Physiol. Biochem. 2017;44:1445–1459. doi: 10.1159/000485580. [DOI] [PubMed] [Google Scholar]
- 239.Tanno M., Kuno A., Ishikawa S., Miki T., Kouzu H., Yano T., Murase H., Tobisawa T., Ogasawara M., Horio Y., et al. Translocation of glycogen synthase kinase-3β (GSK-3β), a trigger of permeability transition, is kinase activity-dependent and mediated by interaction with voltage-dependent anion channel 2 (VDAC2) J. Biol. Chem. 2014;289:29285–29296. doi: 10.1074/jbc.M114.563924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Juhaszova M., Zorov D.B., Kim S.H., Pepe S., Fu Q., Fishbein K.W., Ziman B.D., Wang S., Ytrehus K., Antos C.L., et al. Glycogen synthase kinase-3β mediates convergence of protection signalling to inhibit the mitochondrial permeability transition pore. J. Clin. Invest. 2004;113:1535–1549. doi: 10.1172/JCI19906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Nishihara M., Miura T., Miki T., Tanno M., Yano T., Naitoh K., Ohori K., Hotta H., Terashima Y., Shimamoto K. Modulation of the mitochondrial permeability transition pore complex in GSK-3β-mediated myocardial protection. J. Mol. Cell. Cardiol. 2007;43:564–570. doi: 10.1016/j.yjmcc.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 242.Gao Z., Zhang X., Zuberi A., Hwang D., Quon M.J., Lefevre M., Ye J. Inhibition of insulin sensitivity by free fatty acids requires activation of multiple serine kinases in 3T3-L1 adipocytes. Mol. Endocrinol. 2004;18:2024–2034. doi: 10.1210/me.2003-0383. [DOI] [PubMed] [Google Scholar]
- 243.Aguirre V., Werner E.D., Giraud J., Lee Y.H., Shoelson S.E., White M.F. Phosphorylation of Ser307 in insulin receptor substrate-1 blocks interactions with the insulin receptor and inhibits insulin action. J. Biol. Chem. 2002;277:1531–1537. doi: 10.1074/jbc.M101521200. [DOI] [PubMed] [Google Scholar]
- 244.Tu D., Gao Y., Yang R., Guan T., Hong J.S., Gao H.M. The pentose phosphate pathway regulates chronic neuroinflammation and dopaminergic neurodegeneration. J. Neuroinflammation. 2019;16 doi: 10.1186/s12974-019-1659-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Ronn S.G., Billestrup N., Mandrup-Poulsen T. Diabetes and Suppressors of Cytokine Signaling Proteins. Diabetes. 2007;56:541–548. doi: 10.2337/db06-1068. [DOI] [PubMed] [Google Scholar]
- 246.Kelley D., He J., Menshikova E., Ritov V. Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes. 2002;51:2944–2950. doi: 10.2337/diabetes.51.10.2944. [DOI] [PubMed] [Google Scholar]
- 247.Cummins T., Holden C., Sansbury B., Gibb A., Shah J., Zafar N., Tang Y., Hellmann J., Rai S., Spite M., et al. Metabolic remodeling of white adipose tissue in obesity. Am. J. Physiol. Endocrinol. Metab. 2014;307 doi: 10.1152/ajpendo.00271.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Elrod J.W., Calvert J.W., Morrison J., Doeller J.E., Kraus D.W., Tao L., Jiao X., Scalia R., Kiss L., Szabo C., et al. Hydrogen sulfide attenuates myocardial ischemia-reperfusion injury by preservation of mitochondrial function. Proc. Natl. Acad. Sci. USA. 2007;104:15560–15565. doi: 10.1073/pnas.0705891104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Mattingly K., Ivanova M., Riggs K., Wickramasinghe N., Barch M., Klinge C. Estradiol stimulates transcription of nuclear respiratory factor-1 and increases mitochondrial biogenesis. Mol. Endocrinol. 2008;22:609–622. doi: 10.1210/me.2007-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Cheng Z., Guo S., Copps K., Dong X., Kollipara R., Rodgers J., Depinho R., Puigserver P., White M. Foxo1 integrates insulin signaling with mitochondrial function in the liver. Nat. Med. 2009;15:1307–1311. doi: 10.1038/nm.2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Villapol S. Roles of Peroxisome Proliferator-Activated Receptor-gamma on brain and peripheral inflammation. Cell. Mol. Neurobiol. 2018;38:121. doi: 10.1007/s10571-017-0554-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Masters C.L., Simms G., Weinman N.A., Multhaup G., McDonald B.L., Beyreuther K. Amyloid plaque core protein in Alzheimer disease and Down syndrome. Proc. Natl. Acad. Sci. USA. 1985;82:4245–4249. doi: 10.1073/pnas.82.12.4245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Picón-Pagès P., Bonet J., García-García J., Garcia-Buendia J., Gutierrez D., Valle J., Gómez-Casuso C.E.S., Sidelkivska V., Alvarez A., Perálvarez-Marín A., et al. Human albumin impairs amyloid β-peptide fibrillation through its C-terminus: From docking modeling to protection against neurotoxicity in Alzheimer’s disease. Comput. Struct. Biotechnol. J. 2019;17:963–971. doi: 10.1016/j.csbj.2019.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Valls-Comamala V., Guivernau B., Bonet J., Puig M., Perálvarez-Marín A., Palomer E., Fernàndez-Busquets X., Altafaj X., Tajes M., Puig-Pijoan A., et al. The antigen-binding fragment of human gamma immunoglobulin prevents amyloid β-peptide folding into β-sheet to form oligomers. Oncotarget. 2017;8:41154–41165. doi: 10.18632/oncotarget.17074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Picón-Pagès P., Gutiérrez D.A., Barranco-Almohalla A., Crepin G., Tajes M., Ill-Raga G., Guix F.X., Menéndez S., Arumí-Uría M., Vicente R., et al. Amyloid beta-peptide increases BACE1 translation through the phosphorylation of the eukaryotic initiation factor-2 α. Oxid. Med. Cell. Longev. 2020;2020 doi: 10.1155/2020/2739459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Guix F.X., Wahle T., Vennekens K., Snellinx A., Chávez-Gutiérrez L., Ill-Raga G., Ramos-Fernandez E., Guardia-Laguarta C., Lleó A., Arimon M., et al. Modification of γ-secretase by nitrosative stress links neuronal ageing to sporadic Alzheimer’s disease. EMBO Mol. Med. 2012;4:660–673. doi: 10.1002/emmm.201200243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Ill-Raga G., Tajes M., Busquets-García A., Ramos-Fernández E., Vargas L.M., Bosch-Morató M., Guivernau B., Valls-Comamala V., Eraso-Pichot A., Guix F.X., et al. Physiological control of nitric oxide in neuronal BACE1 translation by heme-regulated eIF2α kinase HRI induces synaptogenesis. Antioxidants Redox Signal. 2015;22:1295–1307. doi: 10.1089/ars.2014.6080. [DOI] [PubMed] [Google Scholar]
- 258.Ramos-Fernández E., Tajes M., Palomer E., Ill-Raga G., Bosch-Morató M., Guivernau B., Román-Dégano I., Eraso-Pichot A., Alcolea D., Fortea J., et al. Posttranslational nitro-glycative modifications of albumin in alzheimer’s disease: Implications in cytotoxicity and amyloid-β peptide aggregation. J. Alzheimer’s Dis. 2014;40:643–657. doi: 10.3233/JAD-130914. [DOI] [PubMed] [Google Scholar]
- 259.Tajes M., Guivernau B., Ramos-Fernández E., Bosch-Morató M., Palomer E., Guix F.X., Muñoz F.J. The pathophysiology of triose phosphate isomerase dysfunction in alzheimer’s disease. Histol. Histopathol. 2013;28:43–51. doi: 10.14670/HH-28.43. [DOI] [PubMed] [Google Scholar]
- 260.Baloyannis S.J. Mitochondrial alterations in Alzheimer’s disease. J. Alzheimer’s Dis. 2006;9:119–126. doi: 10.3233/JAD-2006-9204. [DOI] [PubMed] [Google Scholar]
- 261.Swerdlow R.H. Mitochondria and mitochondrial cascades in Alzheimer’s Disease. J. Alzheimer’s Dis. 2018;62:1403–1416. doi: 10.3233/JAD-170585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Serrano-Pozo A., Frosch M.P., Masliah E., Hyman B.T. Neuropathological alterations in Alzheimer disease. Cold Spring Harb. Perspect. Med. 2011;1 doi: 10.1101/cshperspect.a006189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Fiala J.C., Feinberg M., Peters A., Barbas H. Mitochondrial degeneration in dystrophic neurites of senile plaques may lead to extracellular deposition of fine filaments. Brain Struct. Funct. 2007;212:195–207. doi: 10.1007/s00429-007-0153-1. [DOI] [PubMed] [Google Scholar]
- 264.Swerdlow R.H., Khan S.M. A “mitochondrial cascade hypothesis” for sporadic Alzheimer’s disease. Med. Hypotheses. 2004;63:8–20. doi: 10.1016/j.mehy.2003.12.045. [DOI] [PubMed] [Google Scholar]
- 265.Manczak M., Park B.S., Jung Y., Reddy P.H. Differential expression of oxidative phosphorylation genes in patients with Alzheimer’s disease: Implications for early mitochondrial dysfunction and oxidative damage. NeuroMolecular Med. 2004;5:147–162. doi: 10.1385/NMM:5:2:147. [DOI] [PubMed] [Google Scholar]
- 266.Manczak M., Anekonda T.S., Henson E., Park B.S., Quinn J., Reddy P.H. Mitochondria are a direct site of Aβ accumulation in Alzheimer’s disease neurons: Implications for free radical generation and oxidative damage in disease progression. Hum. Mol. Genet. 2006;15:1437–1449. doi: 10.1093/hmg/ddl066. [DOI] [PubMed] [Google Scholar]
- 267.Rhein V., Song X., Wiesner A., Ittner L.M., Baysang G., Meier F., Ozmen L., Bluethmann H., Dröse S., Brandt U., et al. Amyloid-β and tau synergistically impair the oxidative phosphorylation system in triple transgenic Alzheimer’s disease mice. Proc. Natl. Acad. Sci. USA. 2009;106:20057–20062. doi: 10.1073/pnas.0905529106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Silva D.F., Selfridge J.E., Lu J., Lezi E., Roy N., Hutfles L., Burns J.M., Michaelis E.K., Yan S.D., Cardoso S.M., et al. Bioenergetic flux, mitochondrial mass and mitochondrial morphology dynamics in AD and MCI cybrid cell lines. Hum. Mol. Genet. 2013;22:3931–3946. doi: 10.1093/hmg/ddt247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Manczak M., Calkins M.J., Reddy P.H. Impaired mitochondrial dynamics and abnormal interaction of amyloid beta with mitochondrial protein Drp1 in neurons from patients with Alzheimer’s disease: Implications for neuronal damage. Hum. Mol. Genet. 2011;20:2495–2509. doi: 10.1093/hmg/ddr139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Filadi R., Greotti E., Turacchio G., Luini A., Pozzan T., Pizzo P. On the role of Mitofusin 2 in endoplasmic reticulum-mitochondria tethering. Proc. Natl. Acad. Sci. USA. 2017;114:E2266–E2267. doi: 10.1073/pnas.1616040114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Leal N.S., Schreiner B., Pinho C.M., Filadi R., Wiehager B., Karlström H., Pizzo P., Ankarcrona M. Mitofusin-2 knockdown increases ER–mitochondria contact and decreases amyloid β-peptide production. J. Cell. Mol. Med. 2016;20:1686–1695. doi: 10.1111/jcmm.12863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Wang R., Li J.J., Diao S., Kwak Y.D., Liu L., Zhi L., Büeler H., Bhat N.R., Williams R.W., Park E.A., et al. Metabolic stress modulates Alzheimer’s β-secretase gene transcription via SIRT1-PPARγ-PGC-1 in neurons. Cell Metab. 2013;17:685–694. doi: 10.1016/j.cmet.2013.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Godoy P., Hewitt N.J., Albrecht U., Andersen M.E., Ansari N., Bhattacharya S., Bode J.G., Bolleyn J., Borner C., Böttger J., et al. Recent advances in 2D and 3D in vitro systems using primary hepatocytes, alternative hepatocyte sources and non-parenchymal liver cells and their use in investigating mechanisms of hepatotoxicity, cell signaling and ADME. Arch. Toxicol. 2013;87:1315–1530. doi: 10.1007/s00204-013-1078-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Han P., Tang Z., Yin J., Maalouf M., Beach T.G., Reiman E.M., Shi J. Pituitary adenylate cyclase-activating polypeptide protects against β-amyloid toxicity. Neurobiol. Aging. 2014;35:2064–2071. doi: 10.1016/j.neurobiolaging.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 275.Khanna A., Acharjee P., Acharjee A., Trigun S.K. Mitochondrial SIRT3 and neurodegenerative brain disorders. J. Chem. Neuroanat. 2019;95:43–53. doi: 10.1016/j.jchemneu.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 276.Silva-Alvarez C., Arrázola M.S., Godoy J.A., Ordenes D., Inestrosa N.C. Canonical Wnt signaling protects hippocampal neurons from Aβ oligomers: Role of non-canonical Wnt-5a/Ca2+ in mitochondrial dynamics. Front. Cell. Neurosci. 2013;7:97. doi: 10.3389/fncel.2013.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Arrázola M.S., Silva-Alvarez C., Inestrosa N.C. How the Wnt signaling pathway protects from neurodegeneration: The mitochondrial scenario. Front. Cell. Neurosci. 2015;9:166. doi: 10.3389/fncel.2015.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Pennica D., Swanson T.A., Welsh J.W., Roy M.A., Lawrence D.A., Lee J., Brush J., Taneyhill L.A., Deuel B., Lew M., et al. WISP genes are members of the connective tissue growth factor family that are up-regulated in Wnt-1-transformed cells and aberrantly expressed in human colon tumors. Proc. Natl. Acad. Sci. USA. 1998;95:14717–14722. doi: 10.1073/pnas.95.25.14717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Patra M., Mahata S.K., Padhan D.K., Sen M. CCN6 regulates mitochondrial function. J. Cell Sci. 2016;129:2841–2851. doi: 10.1242/jcs.186247. [DOI] [PubMed] [Google Scholar]
- 280.Arrázola M.S., Ramos-Fernández E., Cisternas P., Ordenes D., Inestrosa N.C. Wnt signaling prevents the aβ oligomer-induced mitochondrial permeability transition pore opening preserving mitochondrial structure in hippocampal neurons. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0168840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Gavello D., Calorio C., Franchino C., Cesano F., Carabelli V., Carbone E., Marcantoni A. Early alterations of hippocampal neuronal firing induced by Abeta42. Cereb. Cortex. 2018;28:433–446. doi: 10.1093/cercor/bhw377. [DOI] [PubMed] [Google Scholar]
- 282.Guivernau B., Bonet J., Valls-Comamala V., Bosch-Morató M., Godoy J.A., Inestrosa N.C., Perálvarez-Marín A., Fernández-Busquets X., Andreu D., Oliva B., et al. Amyloid-β peptide nitrotyrosination stabilizes oligomers and enhances NMDAR-mediated toxicity. J. Neurosci. 2016;36:11693–11703. doi: 10.1523/JNEUROSCI.1081-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Oulès B., Del Prete D., Greco B., Zhang X., Lauritzen I., Sevalle J., Moreno S., Paterlini-Bréchot P., Trebak M., Checler F., et al. Ryanodine receptor blockade reduces amyloid-β load and memory impairments in Tg2576 mouse model of alzheimer disease. J. Neurosci. 2012;32:11820–11834. doi: 10.1523/JNEUROSCI.0875-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Del Prete D., Checler F., Chami M. Ryanodine receptors: Physiological function and deregulation in Alzheimer disease. Mol. Neurodegener. 2014;9:21. doi: 10.1186/1750-1326-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Bosch-Morató M., Iriondo C., Guivernau B., Valls-Comamala V., Vidal N., Olivé M., Querfurth H., Muñoz F.J. Increased amyloid β-peptide uptake in skeletal muscle is induced by hyposialylation and may account for apoptosis in GNE myopathy. Oncotarget. 2016;7:13354–13371. doi: 10.18632/oncotarget.7997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Rubio-Moscardo F., Setó-Salvia N., Pera M., Bosch-Morató M., Plata C., Belbin O., Gené G., Dols-Icardo O., Ingelsson M., Helisalmi S., et al. Rare Variants in Calcium Homeostasis Modulator 1 (CALHM1) Found in Early Onset Alzheimer’s Disease Patients Alter Calcium Homeostasis. PLoS ONE. 2013;8 doi: 10.1371/journal.pone.0074203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Supnet C., Bezprozvanny I. Presenilins function in ER calcium leak and Alzheimer’s disease pathogenesis. Cell Calcium. 2011;50:303–309. doi: 10.1016/j.ceca.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Kipanyula M.J., Contreras L., Zampese E., Lazzari C., Wong A.K.C., Pizzo P., Fasolato C., Pozzan T. Ca2+ dysregulation in neurons from transgenic mice expressing mutant presenilin 2. Aging Cell. 2012;11:885–893. doi: 10.1111/j.1474-9726.2012.00858.x. [DOI] [PubMed] [Google Scholar]
- 289.Ill-Raga G., Ramos-Fernández E., Guix F.X., Tajes M., Bosch-Morató M., Palomer E., Godoy J., Belmar S., Cerpa W., Simpkins J.W., et al. Amyloid-β peptide fibrils induce nitro-oxidative stress in neuronal cells. J. Alzheimer’s Dis. 2010;22:641–652. doi: 10.3233/JAD-2010-100474. [DOI] [PubMed] [Google Scholar]
- 290.Guix F.X., Ill-Raga G., Bravo R., Nakaya T., De Fabritiis G., Coma M., Miscione G.P., Vill-Freixa J., Suzuki T., Fernandez-Busquets X., et al. Amyloid-dependent triosephosphate isomerase nitrotyrosination induces glycation and tau fibrillation. Brain. 2009;132:1335–1345. doi: 10.1093/brain/awp023. [DOI] [PubMed] [Google Scholar]
- 291.Coma M., Guix F.X., Ill-Raga G., Uribesalgo I., Alameda F., Valverde M.A., Muñoz F.J. Oxidative stress triggers the amyloidogenic pathway in human vascular smooth muscle cells. Neurobiol. Aging. 2008;29:969–980. doi: 10.1016/j.neurobiolaging.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 292.Kang D., Hamasaki N. Mitochondrial transcription factor A in the maintenance of mitochondrial DNA: Overview of its multiple roles. Ann. N. Y. Acad. Sci. 2005;1042:101–108. doi: 10.1196/annals.1338.010. [DOI] [PubMed] [Google Scholar]
- 293.Hirai K., Aliev G., Nunomura A., Fujioka H., Russell R.L., Atwood C.S., Johnson A.B., Kress Y., Vinters H.V., Tabaton M., et al. Mitochondrial abnormalities in Alzheimer’s disease. J. Neurosci. 2001;21:3017–3023. doi: 10.1523/JNEUROSCI.21-09-03017.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Maynard S., Schurman S.H., Harboe C., De Souza-Pinto N.C., Bohr V.A. Base excision repair of oxidative DNA damage and association with cancer and aging. Carcinogenesis. 2009;30:2–10. doi: 10.1093/carcin/bgn250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Sliwinska M.W., Violante I.R., Wise R.J.S., Leech R., Devlin J.T., Geranmayeh F., Hampshire A. Stimulating multiple-demand cortex enhances vocabulary learning. J. Neurosci. 2017;37:7606–7618. doi: 10.1523/JNEUROSCI.3857-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Lillenes M.S., Rabano A., Støen M., Riaz T., Misaghian D., Møllersen L., Esbensen Y., Günther C.C., Selnes P., Stenset V.T.V., et al. Altered DNA base excision repair profile in brain tissue and blood in Alzheimer’s disease. Mol. Brain. 2016;9 doi: 10.1186/s13041-016-0237-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Bosetti F., Brizzi F., Barogi S., Mancuso M., Siciliano G., Tendi E., Murri L., Rapoport S., Solaini G. Cytochrome c oxidase and mitochondrial F1F0-ATPase (ATP synthase) activities in platelets and brain from patients with Alzheimer’s disease. Neurobiol. Aging. 2002;23:371–376. doi: 10.1016/S0197-4580(01)00314-1. [DOI] [PubMed] [Google Scholar]
- 298.Gan X., Huang S., Wu L., Wang Y., Hu G., Li G., Zhang H., Yu H., Swerdlow R., Chen J., et al. Inhibition of ERK-DLP1 signaling and mitochondrial division alleviates mitochondrial dysfunction in Alzheimer’s disease cybrid cell. Biochim. Biophys. Acta. 2014;1842:220–231. doi: 10.1016/j.bbadis.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Valaasani K., Sun Q., Hu G., Li J., Du F., Guo Y., Carlson E., Gan X., Yan S. Identification of human ABAD inhibitors for rescuing Aβ-mediated mitochondrial dysfunction. Curr. Alzheimer Res. 2014;11:128–136. doi: 10.2174/1567205011666140130150108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Cieślik M., Czapski G., Wójtowicz S., Wieczorek I., Wencel P., Strosznajder R., Jaber V., Lukiw W., Strosznajder J. Alterations of Transcription of Genes Coding Anti-oxidative and Mitochondria-Related Proteins in Amyloid β Toxicity: Relevance to Alzheimer’s Disease. Mol. Neurobiol. 2020;57:1374–1388. doi: 10.1007/s12035-019-01819-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Dzitoyeva S., Chen H., Manev H. Effect of aging on 5-hydroxymethylcytosine in brain mitochondria. Neurobiol. Aging. 2012;33:2881–2891. doi: 10.1016/j.neurobiolaging.2012.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Surmeier D.J. Determinants of dopaminergic neuron loss in Parkinson’s disease. FEBS J. 2018;285:3657–3668. doi: 10.1111/febs.14607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Langston J., Ballard P., Tetrud J., Irwin I. Chronic Parkinsonism in humans due to a product of meperidine-analog synthesis. Science. 1983;219:979–980. doi: 10.1126/science.6823561. [DOI] [PubMed] [Google Scholar]
- 304.Akundi R.S., Zhi L., Sullivan P.G., Büeler H. Shared and cell type-specific mitochondrial defects and metabolic adaptations in primary cells from PINK1-deficient mice. Neurodegener. Dis. 2013;12:136–149. doi: 10.1159/000345689. [DOI] [PubMed] [Google Scholar]
- 305.Büeler H. Mitochondrial dynamics, cell death and the pathogenesis of Parkinson’s disease. Apoptosis. 2010;15:1336–1353. doi: 10.1007/s10495-010-0465-0. [DOI] [PubMed] [Google Scholar]
- 306.Ciron C., Zheng L., Bobela W., Knott G.W., Leone T.C., Kelly D.P., Schneider B.L. PGC-1α activity in nigral dopamine neurons determines vulnerability to α-synuclein. Acta Neuropathol. Commun. 2015;3:16. doi: 10.1186/s40478-015-0200-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.McCoy M.K., Cookson M.R. Mitochondrial quality control and dynamics in Parkinson’s disease. Antioxidants Redox Signal. 2012;16:869–882. doi: 10.1089/ars.2011.4019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Pacelli C., De Rasmo D., Signorile A., Grattagliano I., di Tullio G., D’Orazio A., Nico B., Comi G.P., Ronchi D., Ferranini E., et al. Mitochondrial defect and PGC-1α dysfunction in parkin-associated familial Parkinson’s disease. Biochim. Biophys. Acta - Mol. Basis Dis. 2011;1812:1041–1053. doi: 10.1016/j.bbadis.2010.12.022. [DOI] [PubMed] [Google Scholar]
- 309.Zheng B., Liao Z., Locascio J.J., Lesniak K.A., Roderick S.S., Watt M.L., Eklund A.C., Zhang-James Y., Kim P.D., Hauser M.A., et al. PGC-1α, a potential therapeutic target for early intervention in Parkinson’s disease. Sci. Transl. Med. 2010;2:52ra73. doi: 10.1126/scitranslmed.3001059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Cataldi M. The changing landscape of Voltage-Gated Calcium Channels in neurovascular disorders and in neurodegenerative diseases. Curr. Neuropharmacol. 2013;11:276–297. doi: 10.2174/1570159X11311030004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Ruiz-Meana M., Garcia-Dorado D., Miró-Casas E., Abellán A., Soler-Soler J. Mitochondrial Ca2+ uptake during simulated ischemia does not affect permeability transition pore opening upon simulated reperfusion. Cardiovasc. Res. 2006;71:715–724. doi: 10.1016/j.cardiores.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 312.Thoudam T., Jeon J.-H., Ha C.-M., Lee I.-K. Role of mitochondria-associated endoplasmic reticulum membrane in inflammation-mediated metabolic diseases. Mediators Inflamm. 2016;2016 doi: 10.1155/2016/1851420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Paillusson S., Gomez-Suaga P., Stoica R., Little D., Gissen P., Devine M.J., Noble W., Hanger D.P., Miller C.C.J. α-Synuclein binds to the ER–mitochondria tethering protein VAPB to disrupt Ca2+ homeostasis and mitochondrial ATP production. Acta Neuropathol. 2017;134:129–149. doi: 10.1007/s00401-017-1704-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Devi L., Raghavendran V., Prabhu B.M., Avadhani N.G., Anandatheerthavarada H.K. Mitochondrial import and accumulation of α-synuclein impair complex I in human dopaminergic neuronal cultures and Parkinson disease brain. J. Biol. Chem. 2008;283:9089–9100. doi: 10.1074/jbc.M710012200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Ashrafi G., Schlehe J.S., LaVoie M.J., Schwarz T.L. Mitophagy of damaged mitochondria occurs locally in distal neuronal axons and requires PINK1 and Parkin. J. Cell Biol. 2014;206:655–670. doi: 10.1083/jcb.201401070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Pickrell A.M., Huang C.H., Kennedy S.R., Ordureau A., Sideris D.P., Hoekstra J.G., Harper J.W., Youle R.J. Endogenous Parkin preserves dopaminergic substantia nigral neurons following mitochondrial DNA mutagenic stress. Neuron. 2015;87:371–381. doi: 10.1016/j.neuron.2015.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Hsieh C.H., Shaltouki A., Gonzalez A.E., da Cruz A.B., Burbulla L.F., St. Lawrence E., Schüle B., Krainc D., Palmer T.D., Wang X. Functional impairment in Miro degradation and mitophagy Is a shared feature in familial and sporadic Parkinson’s disease. Cell Stem Cell. 2016;19:709–724. doi: 10.1016/j.stem.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Aras S., Bai M., Lee I., Springett R., Hüttemann M., Grossman L.I. MNRR1 (formerly CHCHD2) is a bi-organellar regulator of mitochondrial metabolism. Mitochondrion. 2015;20:43–51. doi: 10.1016/j.mito.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 319.Koyano F., Yamano K., Kosako H., Tanaka K., Matsuda N. Parkin recruitment to impaired mitochondria for nonselective ubiquitylation is facilitated by MITOL. J. Biol. Chem. 2019;294:10300. doi: 10.1074/jbc.RA118.006302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Rabinovich E., Kerem A., Fröhlich K., Diamant N., Bar-Nun S. AAA-ATPase p97/Cdc48p, a cytosolic chaperone required for endoplasmic reticulum-associated protein degradation. Mol. Cell. Biol. 2002;22:626–634. doi: 10.1128/MCB.22.2.626-634.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Sekine S., Youle R. PINK1 import regulation; a fine system to convey mitochondrial stress to the cytosol. BMC Biol. 2018;16 doi: 10.1186/s12915-017-0470-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Plun-Favreau H., Klupsch K., Moisoi N., Gandhi S., Kjaer S., Frith D., Harvey K., Deas E., Harvey R.J., McDonald N., et al. The mitochondrial protease HtrA2 is regulated by Parkinson’s disease-associated kinase PINK1. Nat. Cell Biol. 2007 911. 2007;9:1243–1252. doi: 10.1038/ncb1644. [DOI] [PubMed] [Google Scholar]
- 323.Pridgeon J., Olzmann J., Chin L., Li L. PINK1 protects against oxidative stress by phosphorylating mitochondrial chaperone TRAP1. PLoS Biol. 2007;5:1494–1503. doi: 10.1371/journal.pbio.0050172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Morais V., Verstreken P., Roethig A., Smet J., Snellinx A., Vanbrabant M., Haddad D., Frezza C., Mandemakers W., Vogt-Weisenhorn D., et al. Parkinson’s disease mutations in PINK1 result in decreased Complex I activity and deficient synaptic function. EMBO Mol. Med. 2009;1:99–111. doi: 10.1002/emmm.200900006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Barazzuol L., Giamogante F., Brini M., Calì T. PINK1/Parkin Mediated Mitophagy, Ca2+ Signalling, and ER-Mitochondria Contacts in Parkinson’s Disease. Int. J. Mol. Sci. 2020;21:1772. doi: 10.3390/ijms21051772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Dolgacheva L., Berezhnov A., Fedotova E., Zinchenko V., Abramov A. Role of DJ-1 in the mechanism of pathogenesis of Parkinson’s disease. J. Bioenerg. Biomembr. 2019;51:175–188. doi: 10.1007/s10863-019-09798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Bonello F., Hassoun S., Mouton-Liger F., Shin Y., Muscat A., Tesson C., Lesage S., Beart P., Brice A., Krupp J., et al. LRRK2 impairs PINK1/Parkin-dependent mitophagy via its kinase activity: Pathologic insights into Parkinson’s disease. Hum. Mol. Genet. 2019;28:1645–1660. doi: 10.1093/hmg/ddz004. [DOI] [PubMed] [Google Scholar]
- 328.DeJesus-Hernandez M., Mackenzie I.R., Boeve B.F., Boxer A.L., Baker M., Rutherford N.J., Nicholson A.M., Finch N.C.A., Flynn H., Adamson J., et al. Expanded GGGGCC Hexanucleotide Repeat in Noncoding Region of C9ORF72 Causes Chromosome 9p-Linked FTD and ALS. Neuron. 2011;72:245–256. doi: 10.1016/j.neuron.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Renton A.E., Majounie E., Waite A., Simón-Sánchez J., Rollinson S., Gibbs J.R., Schymick J.C., Laaksovirta H., van Swieten J.C., Myllykangas L., et al. A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. Neuron. 2011;72:257–268. doi: 10.1016/j.neuron.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Rosen D.R., Siddique T., Patterson D., Figlewicz D.A., Sapp P., Hentati A., Donaldson D., Goto J., O’Regan J.P., Deng H.X., et al. Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature. 1993;362:59–62. doi: 10.1038/362059a0. [DOI] [PubMed] [Google Scholar]
- 331.Vance C., Rogelj B., Hortobágyi T., De Vos K.J., Nishimura A.L., Sreedharan J., Hu X., Smith B., Ruddy D., Wright P., et al. Mutations in FUS, an RNA processing protein, cause familial amyotrophic lateral sclerosis type 6. Science. 2009;323:1208–1211. doi: 10.1126/science.1165942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Neumann M., Rademakers R., Roeber S., Baker M., Kretzschmar H.A., MacKenzie I.R.A. A new subtype of frontotemporal lobar degeneration with FUS pathology. Brain. 2009;132:2922–2931. doi: 10.1093/brain/awp214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Sreedharan J., Blair I.P., Tripathi V.B., Hu X., Vance C., Rogelj B., Ackerley S., Durnall J.C., Williams K.L., Buratti E., et al. TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science. 2008;319:1668–1672. doi: 10.1126/science.1154584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Kabashi E., Valdmanis P.N., Dion P., Spiegelman D., McConkey B.J., Velde C.V., Bouchard J.P., Lacomblez L., Pochigaeva K., Salachas F., et al. TARDBP mutations in individuals with sporadic and familial amyotrophic lateral sclerosis. Nat. Genet. 2008;40:572–574. doi: 10.1038/ng.132. [DOI] [PubMed] [Google Scholar]
- 335.Zufiría M., Gil-Bea F.J., Fernández-Torrón R., Poza J.J., Muñoz-Blanco J.L., Rojas-García R., Riancho J., de Munain A.L. ALS: A bucket of genes, environment, metabolism and unknown ingredients. Prog. Neurobiol. 2016;142:104–129. doi: 10.1016/j.pneurobio.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 336.Gao J., Wang L., Yan T., Perry G., Wang X. TDP-43 proteinopathy and mitochondrial abnormalities in neurodegeneration. Mol. Cell. Neurosci. 2019;100 doi: 10.1016/j.mcn.2019.103396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Bannwarth S., Ait-El-Mkadem S., Chaussenot A., Genin E.C., Lacas-Gervais S., Fragaki K., Berg-Alonso L., Kageyama Y., Serre V., Moore D.G., et al. A mitochondrial origin for frontotemporal dementia and amyotrophic lateral sclerosis through CHCHD10 involvement. Brain. 2014;137:2329–2345. doi: 10.1093/brain/awu138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Anderson C.J., Bredvik K., Burstein S.R., Davis C., Meadows S.M., Dash J., Case L., Milner T.A., Kawamata H., Zuberi A., et al. ALS/FTD mutant CHCHD10 mice reveal a tissue-specific toxic gain-of-function and mitochondrial stress response. Acta Neuropathol. 2019;138 doi: 10.1007/s00401-019-01989-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Liu T., Woo J.A.A., Bukhari M.Z., LePochat P., Chacko A., Selenica M.L.B., Yan Y., Kotsiviras P., Buosi S.C., Zhao X., et al. CHCHD10-regulated OPA1-mitofilin complex mediates TDP-43-induced mitochondrial phenotypes associated with frontotemporal dementia. FASEB J. 2020;34:8493–8509. doi: 10.1096/fj.201903133RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Pickles S., Semmler S., Broom H.R., Destroismaisons L., Legroux L., Arbour N., Meiering E., Cashman N.R., Vande Velde C. ALS-linked misfolded SOD1 species have divergent impacts on mitochondria. Acta Neuropathol. Commun. 2016;4:43. doi: 10.1186/s40478-016-0313-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Tafuri F., Ronchi D., Magri F., Comi G.P., Corti S. SOD1 misplacing and mitochondrial dysfunction in amyotrophic lateral sclerosis pathogenesis. Front. Cell. Neurosci. 2015:9. doi: 10.3389/fncel.2015.00336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Kawamata H., Manfredi G. Different regulation of wild-type and mutant Cu,Zn superoxide dismutase localization in mammalian mitochondria. Hum. Mol. Genet. 2008;17:3303–3317. doi: 10.1093/hmg/ddn226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Crociara P., Chieppa M.N., Vallino Costassa E., Berrone E., Gallo M., Lo Faro M., Pintore M.D., Iulini B., D’Angelo A., Perona G., et al. Motor neuron degeneration, severe myopathy and TDP-43 increase in a transgenic pig model of SOD1-linked familiar ALS. Neurobiol. Dis. 2019;124:263–275. doi: 10.1016/j.nbd.2018.11.021. [DOI] [PubMed] [Google Scholar]
- 344.Rogers R.S., Tungtur S., Tanaka T., Nadeau L.L., Badawi Y., Wang H., Ni H.M., Ding W.X., Nishimune H. Impaired mitophagy plays a role in denervation of neuromuscular junctions in ALS mice. Front. Neurosci. 2017;11 doi: 10.3389/fnins.2017.00473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Tak Y.J., Park J.H., Rhim H., Kang S. ALS-related mutant SOD1 aggregates interfere with mitophagy by sequestering the autophagy receptor optineurin. Int. J. Mol. Sci. 2020;21:7525. doi: 10.3390/ijms21207525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Moller A., Bauer C.S., Cohen R.N., Webster C.P., De Vos K.J. Amyotrophic lateral sclerosis-associated mutant SOD1 inhibits anterograde axonal transport of mitochondria by reducing Miro1 levels. Hum. Mol. Genet. 2017;26:4668–4679. doi: 10.1093/hmg/ddx348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Nita M., Grzybowski A. The role of the reactive oxygen species and oxidative stress in the pathomechanism of the age-related ocular diseases and other pathologies of the anterior and posterior eye segments in adults. Oxid. Med. Cell. Longev. 2016;2016 doi: 10.1155/2016/3164734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Van Den Bosch L., Van Damme P., Bogaert E., Robberecht W. The role of excitotoxicity in the pathogenesis of amyotrophic lateral sclerosis. Biochim. Biophys. Acta - Mol. Basis Dis. 2006;1762:1068–1082. doi: 10.1016/j.bbadis.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 349.Davis S.A., Itaman S., Khalid-Janney C.M., Sherard J.A., Dowell J.A., Cairns N.J., Gitcho M.A. TDP-43 interacts with mitochondrial proteins critical for mitophagy and mitochondrial dynamics. Neurosci. Lett. 2018;678:8–15. doi: 10.1016/j.neulet.2018.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Wang W., Wang L., Lu J., Siedlak S., Fujioka H., Liang J., Jiang S., X M., Jiang Z., da Rocha E., et al. The inhibition of TDP-43 mitochondrial localization blocks its neuronal toxicity. Nat. Med. 2016;22:869–878. doi: 10.1038/nm.4130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Armakola M., Higgins M., Figley M., Barmada S., Scarborough E., Diaz Z., Fang X., Shorter J., Krogan N., Finkbeiner S., et al. Inhibition of RNA lariat debranching enzyme suppresses TDP-43 toxicity in ALS disease models. Nat. Genet. 2012;44:1302–1309. doi: 10.1038/ng.2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Elden A.C., Kim H.-J., Hart M.P., Chen-Plotkin A.S., Johnson B.S., Fang X., Armakola M., Geser F., Greene R., Lu M.M., et al. Ataxin-2 intermediate-length polyglutamine expansions are associated with increased risk for ALS. Nat. 2010 4667310. 2010;466:1069–1075. doi: 10.1038/nature09320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Stoica R., Paillusson S., Gomez-Suaga P., Mitchell J., Lau D., Gray E., Sancho R., Vizcay-Barrena G., De Vos K., Shaw C., et al. ALS/FTD-associated FUS activates GSK-3β to disrupt the VAPB-PTPIP51 interaction and ER-mitochondria associations. EMBO Rep. 2016;17:1326–1342. doi: 10.15252/embr.201541726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Hsu F., Spannl S., Ferguson C., Hyman A., Parton R., Zerial M. Rab5 and Alsin regulate stress-activated cytoprotective signaling on mitochondria. Elife. 2018;7 doi: 10.7554/eLife.32282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Strong T.V., Tagle D.A., Valdes J.M., Elmer L.W., Boehm K., Swaroop M., Kaatz K.W., Collins F.S., Albin R.L. Widespread expression of the human and rat Huntington’s disease gene in brain and nonneural tissues. Nat. Genet. 1993;5:259–265. doi: 10.1038/ng1193-259. [DOI] [PubMed] [Google Scholar]
- 356.Chen N., Luo T., Wellington C., Metzler M., McCutcheon K., Hayden M.R., Raymond L.A. Subtype-specific enhancement of NMDA receptor currents by mutant huntingtin. J. Neurochem. 1999;72:1890–1898. doi: 10.1046/j.1471-4159.1999.0721890.x. [DOI] [PubMed] [Google Scholar]
- 357.Ramos-Fernández E., Tajes M., ILL-Raga G., Vargas L., Busquets-García A., Bosch-Morató M., Guivernau B., Valls-Comamala V., Gomis M., Grau C., et al. Glutamatergic stimulation induces GluN2B translation by the nitric oxide-Heme-Regulated eIF2alpha kinase in cortical neurons. Oncotarget. 2016;7:58876–58892. doi: 10.18632/oncotarget.11417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Muñoz F.J., Godoy J.A., Cerpa W., Poblete I.M., Huidobro-Toro J.P., Inestrosa N.C. Wnt-5a increases NO and modulates NMDA receptor in rat hippocampal neurons. Biochem. Biophys. Res. Commun. 2014;444:189–194. doi: 10.1016/j.bbrc.2014.01.031. [DOI] [PubMed] [Google Scholar]
- 359.Seong I.S., Ivanova E., Lee J.M., Choo Y.S., Fossale E., Anderson M.A., Gusella J.F., Laramie J.M., Myers R.H., Lesort M., et al. HD CAG repeat implicates a dominant property of huntingtin in mitochondrial energy metabolism. Hum. Mol. Genet. 2005;14:2871–2880. doi: 10.1093/hmg/ddi319. [DOI] [PubMed] [Google Scholar]
- 360.Hodgson J.G., Agopyan N., Gutekunst C.A., Leavitt B.R., Lepiane F., Singaraja R., Smith D.J., Bissada N., McCutcheon K., Nasir J., et al. A YAC mouse model for Huntington’s disease with full-length mutant huntingtin, cytoplasmic toxicity, and selective striatal neurodegeneration. Neuron. 1999;23:181–192. doi: 10.1016/S0896-6273(00)80764-3. [DOI] [PubMed] [Google Scholar]
- 361.Hands S., Sajjad M.U., Newton M.J., Wyttenbach A. In vitro and in vivo aggregation of a fragment of huntingtin protein directly causes free radical production. J. Biol. Chem. 2011;286:44512–44520. doi: 10.1074/jbc.M111.307587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Firdaus W.J.J., Wyttenbach A., Giuliano P., Kretz-Remy C., Currie R.W., Arrigo A.P. Huntingtin inclusion bodies are iron-dependent centers of oxidative events. FEBS J. 2006;273:5428–5441. doi: 10.1111/j.1742-4658.2006.05537.x. [DOI] [PubMed] [Google Scholar]
- 363.Ayala-Peña S. Role of oxidative DNA damage in mitochondrial dysfunction and Huntington’s disease pathogenesis. Free Radic. Biol. Med. 2013;62:102–110. doi: 10.1016/j.freeradbiomed.2013.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Jodeiri Farshbaf M., Ghaedi K. Huntington’s disease and mitochondria. Neurotox. Res. 2017;32:518–529. doi: 10.1007/s12640-017-9766-1. [DOI] [PubMed] [Google Scholar]
- 365.Gemba H., Kyuhou S., Matsuzaki R., Amino Y. Oxidative damage to mitochondrial DNA in Huntington’s disease parietal cortex. Neurosci. Lett. 1999;272:53–56. doi: 10.1016/S0304-3940(99)00578-9. [DOI] [PubMed] [Google Scholar]
- 366.Shirendeb U.P., Calkins M.J., Manczak M., Anekonda V., Dufour B., McBride J.L., Mao P., Reddy P.H. Mutant Huntingtin’s interaction with mitochondrial protein Drp1 impairs mitochondrial biogenesis and causes defective axonal transport and synaptic degeneration in Huntington’s Disease. Hum. Mol. Genet. 2012;21:406–420. doi: 10.1093/hmg/ddr475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Lu B., Al-Ramahi I., Valencia A., Wang Q., Berenshteyn F., Yang H., Gallego-Flores T., Ichcho S., Lacoste A., Hild M., et al. Identification of NUB1 as a suppressor of mutant Huntington toxicity via enhanced protein clearance. Nat. Neurosci. 2013;16:562–570. doi: 10.1038/nn.3367. [DOI] [PubMed] [Google Scholar]
- 368.Sassone J., Colciago C., Marchi P., Ascardi C., Alberti L., Pardo A.D., Zippel R., Sipione S., Silani V., Ciammola A. Mutant Huntingtin induces activation of the Bcl-2/adenovirus E1B 19-kDa interacting protein (BNip3) Cell Death Dis. 2010;1:e7. doi: 10.1038/cddis.2009.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Feng Z., Jin S., Zupnick A., Hoh J., de Stanchina E., Lowe S., Prives C., Levine A. p53 tumor suppressor protein regulates the levels of huntingtin gene expression. Oncogene. 2006;25:1–7. doi: 10.1038/sj.onc.1209021. [DOI] [PubMed] [Google Scholar]
- 370.Gauthier L., Charrin B., Borrell-Pagès M., Dompierre J., Rangone H., Cordelières F., De Mey J., MacDonald M., Lessmann V., Lessmann S., et al. Huntingtin controls neurotrophic support and survival of neurons by enhancing BDNF vesicular transport along microtubules. Cell. 2004;118:127–138. doi: 10.1016/j.cell.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 371.Guedes-Dias P., de Proença J., Soares T., Leitão-Rocha A., Pinho B., Duchen M., Oliveira J. HDAC6 inhibition induces mitochondrial fusion, autophagic flux and reduces diffuse mutant huntingtin in striatal neurons. Biochim. Biophys. Acta. 2015;1852:2484–2493. doi: 10.1016/j.bbadis.2015.08.012. [DOI] [PubMed] [Google Scholar]
- 372.Jesse S., Bayer H., Alupei M.C., Zügel M., Mulaw M., Tuorto F., Malmsheimer S., Singh K., Steinacker J., Schumann U., et al. Ribosomal transcription is regulated by PGC-1alpha and disturbed in Huntington’s disease. Sci. Rep. 2017;7:1–10. doi: 10.1038/s41598-017-09148-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.