Abstract
Cardiac tamponade is a rare but potentially fatal complication of inferior vena cava filter retrieval. We discuss such a case to facilitate prompt recognition and prevention of this complication by medical providers. (Level of Difficulty: Beginner.)
Key Words: cardiac tamponade, complication, inferior vena cava filter, pericardial effusion, retrieval
Abbreviations and Acronyms: IVC, inferior vena cava; PE, pulmonary embolus
Graphical abstract

Cardiac tamponade is a rare but potentially fatal complication of inferior vena cava filter retrieval. We discuss such a case to facilitate prompt…
History of Presentation
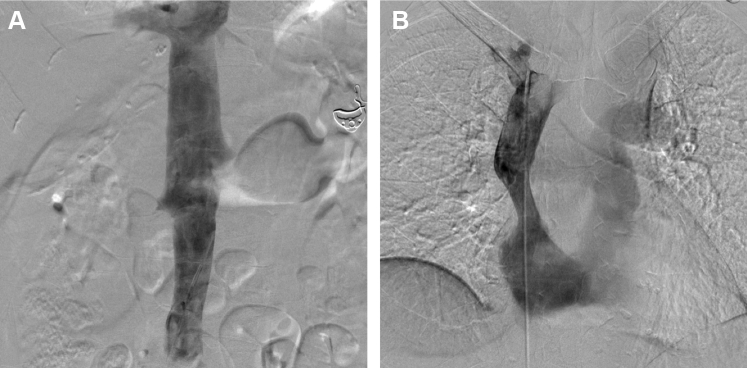
A 74-year-old woman presented for scheduled inferior vena cava (IVC) filter retrieval. Central venous access was gained via the right internal jugular vein. A 16-F Cook retrieval sheath (Cook Medical, Bloomington, Indiana) was advanced to the IVC and snaring of the filter was attempted but was unsuccessful. Next, forceps were advanced through the sheath and used to grasp the superior portion of the filter. After retracting the filter into the sheath, the filter’s hook was seen protruding from the mid-portion of the sheath on fluoroscopy (Figure 1, Video 1). Despite these findings, the sheath and filter were removed. Visual inspection of the sheath demonstrated a linear tear from the distal to mid-portion with the filter hook protruding from the sheath. Post-removal IVC (Figure 2A) and superior vena cava (Figure 2B) venography demonstrated no evidence of contrast extravasation, filling defects, or stasis.
Learning Objectives
-
•
To draw attention to cardiac tamponade as a complication of IVC filter retrieval.
-
•
To increase understanding of the broad scope of clinical manifestations of cardiac tamponade, including atypical presentations.
-
•
To highlight factors that are associated with increased risk of complications in IVC filter retrieval.
-
•
To compare the utility of varying modalities in diagnosis of cardiac tamponade.
Figure 1.
Fluoroscopic Images
Fluoroscopy demonstrating penetration of the inferior vena cava filter (arrow) through the Cook retrieval sheath.
Video 1.
Online video 1
Figure 2.
Post-Retrieval Venography
(A) Inferior vena cava venogram. (B) Superior vena cava venogram. Neither demonstrate evidence of contrast extravasation, filling defects, or stasis.
Ten min following the procedure, the patient became acutely hypotensive (blood pressure 70s/50s mm Hg), tachycardic (heart rate 105 to 110 beats/min), and tachypneic, but continued to saturate well on room air. She was given naloxone, a normal saline bolus, and albumin without significant hemodynamic improvement. The patient was started on norepinephrine. Beside echocardiogram demonstrated a large pericardial effusion. The patient denied chest pain but experienced nausea and nonbloody emesis. Physical examination revealed a lethargic female with intermittent bleeding from her right internal jugular access site. She was tachycardic with a regular rhythm on cardiac examination and her lungs were clear to auscultation bilaterally.
Past Medical History
The patient is a 74-year-old female with a history of hypertension. An Option ELITE (Argon Medical Devices, Frisco, Texas) retrievable IVC filter was placed 6 months prior, following the discovery of a left lower extremity deep vein thrombosis and bilateral pulmonary emboli (PE) in the setting of prolonged immobilization following a motor vehicle accident. Anticoagulation was initially deferred given consideration for operative repair of lumbar fractures sustained during the accident and concern for aortic injury.
Differential Diagnosis
This patient’s acute decompensation in the context of a new large pericardial effusion following IVC filter retrieval raised concern for injury of the vena cava, aorta, or branch vessels; injury of the right atrium or ventricle; and aortic dissection.
Investigations
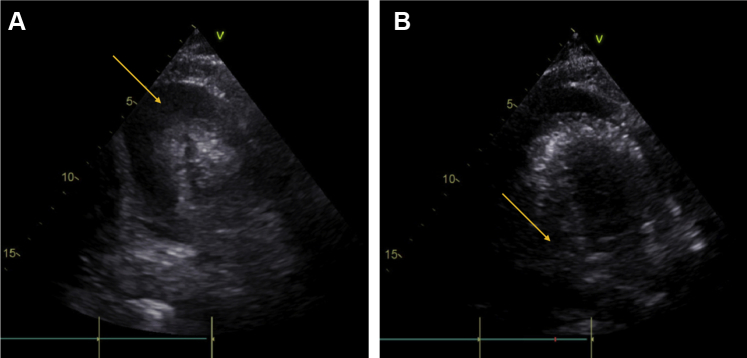
Laboratory studies were significant for a down-trending hemoglobin (10.7, compared with 13.1 pre-procedure). Chest radiograph demonstrated interstitial pulmonary vascular markings suggestive of mild pulmonary edema. Electrocardiography showed diffuse ST-segment elevation and PR-segment depression. A repeat echocardiogram demonstrated evidence of tamponade physiology (Figure 3).
Figure 3.
Transthoracic Echocardiogram Showing Tamponade Physiology
(A) Large pericardial effusion (arrow). (B) Right ventricular diastolic collapse (arrow).
Management
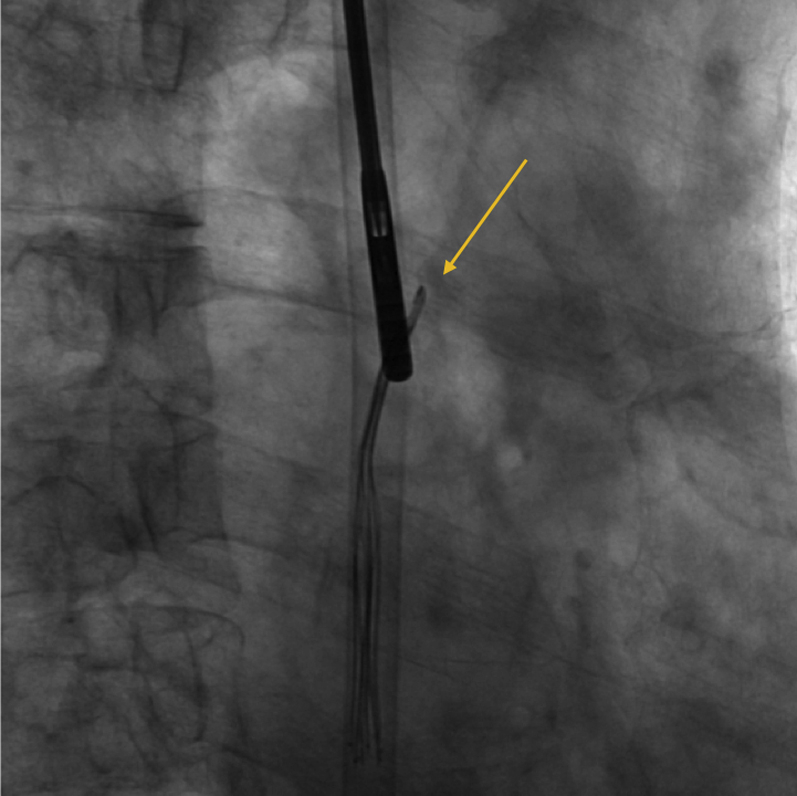
The patient underwent emergent pericardiocentesis with fluoroscopic and echocardiographic guidance (Figure 4, Video 2) with removal of 265 ml of bloody pericardial fluid. A pericardial drain was placed. The patient’s blood pressure and heart rate rapidly normalized after pericardiocentesis. Analysis of the pericardial fluid was consistent with hemopericardium. The pericardial drain was removed after 24 h and the patient was discharged home 2 days later.
Figure 4.

Transthoracic Echocardiogram During Pericardiocentesis
Decreased effusion size and improved filling of the right ventricle.
Video 2.
Online video 2
Discussion
IVC filters are used in the setting of acute proximal venous thrombosis in patients who have either a contraindication to anticoagulation, experienced complications of anticoagulation, and/or as an adjunct in patients that have failed treatment with anticoagulation (1,2). IVC filters decrease the risk of PE but have no effect on overall survival (3).
Long-term complications of indwelling filters include thrombotic occlusion of the IVC and/or filter thrombosis, vascular wall penetration, filter fracture, filter migration, embolization, and penetration of surrounding visceral organs (1,3, 4, 5). Limited case reports have described filter fracture with embolization of fragments to and perforation of the right ventricle, leading to hemopericardium and cardiac tamponade (2,6). Given that device-related complications seem to increase with filter dwell time (4), the U.S. Food and Drug Administration has recommended that retrievable IVC filters be removed as soon as protection from PE is no longer needed (3).
However, IVC filter retrieval carries significant risks, including IVC dissection, intussusception, thrombus formation, and stenosis (1,4). Filter fracture with embedded strut, intramural hemorrhage, PE, and recurrent lower extremity deep vein thrombosis have been additionally reported (1,4,5). Less frequent complications include arteriovenous fistula formation (1) and cardiac tamponade secondary to guidewire coiling within the right ventricle (7). Our patient seems to be the first reported case of cardiac tamponade caused by a tear in the retrieval sheath with protrusion of the filter hook. We suspect that the filter hook or the fractured sheath perforated the wall of the vena cava and entered the pericardial space, resulting in the rapid development of hemopericardium.
Cardiac tamponade is a cardiac emergency in which the intrapericardial pressure from a pericardial effusion impairs cardiac filling during diastole, resulting in hemodynamic compromise (8). Elevated filling pressures, reduced stroke volume, and a compensatory increase in sympathetic tone are responsible for most clinical findings (9). These include the signs described in Beck's triad: hypotension, elevated jugular venous pressure, and diminished heart sounds (8,10). Additional manifestations include narrowed pulse pressure, a thready pulse (8,9), sinus tachycardia, increased systemic vascular resistance, cool skin, and delayed capillary refill (9). This patient presented with hypotension, narrowed pulse pressure, sinus tachycardia, and tachypnea.
Cardiac tamponade can present acutely with pleuritic chest pain or chest fullness and dyspnea on exertion progressing to orthopnea (8,10). Less often, patients present with symptoms related to the compression of adjacent intrathoracic structures by an expanding pericardium, such as hoarseness, dysphagia, nausea, or hiccups (8,10). Although this patient denied chest pain, she experienced significant nausea. Also notable was the acuity of her presentation, with shock developing within minutes of filter retrieval. Patients may also present with nonspecific symptoms, such as weakness, fatigue, anorexia, and cough (10). This patient developed both lethargy and cough.
Chest radiograph is neither sensitive nor specific in the diagnosis of pericardial effusion but, in larger effusions, may reveal cardiomegaly in the absence of pulmonary congestion (8,9). Electrocardiography findings suggestive of pericardial effusion include electrical alternans and/or low voltages (8,9). This patient’s electrocardiogram showed diffuse ST-segment elevation and PR-segment depression, suggestive of pericarditis, possibly secondary to hemopericardium. Echocardiography remains the gold standard for diagnosis, and typically reveals diastolic collapse of the right atrium (late diastole) and right ventricle (early diastole) (8,9). Without chamber collapse, the negative predictive value for cardiac tamponade is >90% (8).
Follow-Up
The patient was seen 1 month following her pericardiocentesis. She was doing well clinically, with stable vital signs, unremarkable physical examination, and no symptomatic complaints.
Conclusions
This case demonstrates the acute decompensation of a patient because of cardiac tamponade following IVC filter retrieval. Although the exact location of the injury that led to the tamponade is uncertain, the vena cava was likely punctured by the filter hook or fractured sheath, creating a communication with the pericardial space and resulting in the rapid development of hemopericardium. The patient’s presentation lacked many classic features of tamponade but was notable for its acuity. Although infrequent, cardiac tamponade should be suspected in patients who develop hemodynamic instability following a retrieval procedure. Post-retrieval venography failed to detect the complication in this case, which was only elucidated by echocardiography. Physicians should continue to report these and other procedural complications to facilitate prompt recognition by other providers.
Footnotes
All authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
Appendix
For supplemental videos, please see the online version of this paper.
References
- 1.DeSai C., Lamus D., Kumar G. Arteriovenous fistula: a rare complication of IVC filter retrieval. Vasc Endovascular Surg. 2019;53:501–506. doi: 10.1177/1538574419849998. [DOI] [PubMed] [Google Scholar]
- 2.Nicholson W., Nicholson W.J., Tolerico P. Prevalence of fracture and fragment embolization of Bard retrievable vena cava filters and clinical implications including cardiac perforation and tamponade. Arch Intern Med. 2010;170:1827–1831. doi: 10.1001/archinternmed.2010.316. [DOI] [PubMed] [Google Scholar]
- 3.Crumley K.D., Hyatt E., Kalva S.P., Shah H. Factors affecting inferior vena cava filter retrieval: a review. Vasc Endovascular Surg. 2019;53:224–229. doi: 10.1177/1538574418814061. [DOI] [PubMed] [Google Scholar]
- 4.Desai K.R., Laws J.L., Salem R. Defining prolonged dwell time: when are advanced inferior vena cava filter retrieval techniques necessary? Circ Cardiovasc Interv. 2017;10:1–5. doi: 10.1161/CIRCINTERVENTIONS.116.003957. [DOI] [PubMed] [Google Scholar]
- 5.Al-Hakim R., Kee S.T., Olinger K., Lee E.W., Moriarty J.M., Mcwilliams J.P. Inferior vena cava filter retrieval: effectiveness and complications of routine and advanced techniques. J Vasc Interv Radiol. 2014;25:933–939. doi: 10.1016/j.jvir.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 6.Mehta J.J., Demarco B., Vavalle J.P., Tahir K.S., Rossi J.S. Hemopericardium and cardiac tamponade secondary to migrated inferior vena cava filter. Case Rep Cardiol. 2018;2018:1–3. doi: 10.1155/2018/5919767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marquess J.S., Burke C.T., Beecham A.H. Factors associated with failed retrieval of the Günther Tulip inferior vena cava filter. J Vasc Interv Radiol. 2008;19:1321–1327. doi: 10.1016/j.jvir.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Hoit B.D. Pericardial effusion and cardiac tamponade in the new millennium. Curr Cardiol Rep. 2017;19:1–11. doi: 10.1007/s11886-017-0867-5. [DOI] [PubMed] [Google Scholar]
- 9.Kearns M.J., Walley K.R. Tamponade: hemodynamic and echocardiographic diagnosis. Chest. 2017;153:1266–1275. doi: 10.1016/j.chest.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Adler Y., Charron P., Imazio M. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: the Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS) Eur Heart J. 2015;36:2921–2964. doi: 10.1093/eurheartj/ehv318. [DOI] [PMC free article] [PubMed] [Google Scholar]