Abstract
Objective:
To determine whether cerebral small vessel disease or disability modify the effect of systolic blood pressure (SBP) treatment on cognitive and vascular outcomes in older patients with recent lacunar stroke.
Methods:
Participants aged ≥65 years of the Secondary Prevention of Small Subcortical Strokes Trial were randomized to a higher (130–149mmHg) or lower (<130mmHg) SBP target. The primary outcome was change in cognitive function (Cognitive Abilities Screening Instrument); secondary outcomes were incident mild cognitive impairment, stroke, major vascular events (all-stroke, myocardial infarction), and all-cause death. Results were stratified by severity of white matter hyperintensities (WMH; none/mild, moderate, severe) on baseline MRI, and by disability (no vs. ≥1 limitations in activities of daily living).
Results:
1,263 participants (mean age 73.8±5.9 years, 40% women) were included. Participants with severe WMH or disability had worse cognitive function at baseline and after a mean follow-up of 3.9 years. No significant interactions existed between treatment group and effect modifiers (WMH, disability) for change in cognitive function (p for interaction 0.42 and 0.66, respectively). A lower SBP target appeared more beneficial among those with worse WMH burden for vascular outcomes (p for interaction = 0.01 for stroke and 0.03 for major vascular events).
Conclusions:
There was no difference in the effect of lowering SBP to <130mmHg on cognitive function by cerebral small vessel disease or disability among older adults with a history of lacunar stroke. Those with evidence of small vessel disease may derive greater benefit from lower SBP on prevention of subsequent vascular events.
Trial registration:
Clinicaltrials.gov Identifier: NCT00059306.
Keywords: Blood pressure, aging, cognitive function, lacunar stroke
Introduction
Lacunar strokes are small subcortical brain infarcts that encompass a third of all ischemic strokes.1 Hypertension is the most prevalent stroke risk factor; and blood pressure (BP) control is a cornerstone of stroke prevention, with current guidelines recommending intensive antihypertensive treatment with a target systolic BP <130 mmHg in patients with lacunar stroke.2–4 In addition to stroke prevention, there is interest from patients and providers in the effects of a lower BP target on cognitive health.
The evidence on the effect of lowering BP on cognitive outcomes is conflicting. The SPRINT randomized controlled trial (RCT) of 9,361 hypertensive adults at increased risk of cardiovascular disease (CVD) found that participants randomized to an intensive BP treatment target had a 19% lower risk for mild cognitive impairment (MCI) (95% confidence interval, CI, 5 to 31%).5 Conversely, results from the Secondary Prevention of Small Subcortical Strokes (SPS3) trial,6,7 an international randomized clinical trial that assessed the effect of higher (systolic BP 130–149 mmHg) vs. lower (systolic BP <130 mmHg) BP targets in patients with recent small subcortical stroke on subsequent recurrent stroke events, demonstrated no overall differences in change in cognitive function by BP treatment group.
One potential explanation for these conflicting findings is heterogeneity in treatment effects of BP lowering by functional status. In the Systolic Hypertension in the Elderly (SHEP) trial, the presence of self-reported ability limitations appeared to modify the effect of the intervention, such that among those reporting limitations, antihypertensive medication use was not associated with a reduced risk of death, cardiovascular death, or myocardial infarction.8 Furthermore, the intervention appeared to be protective for risk of falls in participants without ability limitations but not in those with ability limitations. Observational studies have found that functional ability may modify the effect of BP, such that higher BP is associated with preserved cognitive function among individuals with disabilities.9,10
In addition to functional status, subclinical vessel disease may modify the effect of BP lowering on cognitive function and vascular outcomes. White matter hyperintensities (WMH) are a measure of vascular aging and subclinical cerebral small vessel disease, and increased WMH levels have been associated with cognitive decline.11 Recent hypertension guidelines recommend lower BP targets among high-risk groups. Since persons with WMH are a high-risk group, it is possible that they may gain greater protection from lower BP targets.12 A substudy of the SPRINT trial found that an intensive BP treatment target was associated with a smaller increase in WMH.13 Alternatively, some have suggested that older adults with vascular disease may need a higher BP for adequate cerebral perfusion to maintain cognitive function. However, whether the effect of intensive BP control on cognition varies by WMH severity has not yet been examined.
The primary goal of this study therefore was to assess whether WMH or disability modify the effect of a lower BP target on changes in cognitive function in older adults in the SPS3 trial. We hypothesized that a lower BP target would be associated with worse cognitive outcomes in those with disability and a higher WMH burden. As a secondary aim, we also examined effect modification for major vascular events. Testing for effect modification by WMH and disability could inform who would benefit or be harmed from intensive BP control and inform more tailored recommendations for BP targets.
Methods
Study population
The Secondary Prevention of Small Subcortical Strokes (SPS3) trial (ClinicalTrials.gov Identifier: NCT00059306) is an international randomized clinical trial that assessed the effect of higher vs. lower (130–149 mmHg vs. <130 mmHg) BP targets in patients with recent small subcortical stroke on subsequent recurrent stroke events. The protocol and the main results have been previously published.6,14,15 For the present analysis, we restricted the population to participants aged 65 years and older.
Exposure definition
The primary exposure of interest was the randomization group with allocation to either a higher systolic BP target of 130–149 mmHg, or to a lower systolic BP target of <130 mmHg. The intervention details have been previously described;15 in brief, treatment allocation was open-label, and antihypertensive treatment followed a recommended algorithm with monthly dose and drug titrations until a stable systolic BP in the target range was reached, and with quarterly checks thereafter.
Effect modifiers
We pre-specified two potential effect modifiers based on reviewing the literature. The first effect modifier was presence of white matter hyperintensities identified on baseline brain MRIs. WMH were scored according to the Age-Related White Matter Changes (ARWMC) scale, and categorized into three groups (none or mild vs. moderate vs. severe).16 The second effect modifier was disability as defined by limitations in the 10-item Barthel activities of daily living (ADL) scale. We categorized disability into two groups (zero vs. one or more limitations), with limitations defined as a score of less than the maximum per ADL scale item.17
Outcome definitions
Cognitive outcome
The primary outcome was change in cognitive function as measured by the Cognitive Abilities Screening Instrument (CASI) at each yearly follow-up study visit until year 5.18 This instrument provides quantitative assessment on nine cognitive domains (attention, concentration, orientation, long-term memory, short-term memory, language, visual construction, list-generating fluency, abstraction and judgment) with a total of 25 items and a score range of 0 to 100. We standardized the raw scores into Z-scores, based on published normative data, as previously described.6 We excluded CASI Z-scores from assessments done after recurrent strokes.
A secondary cognitive outcome was incident MCI, defined as a standardized score of ≤1.5 standard deviations in any neuropsychological test of cognitive function performed (except for the CASI assessment), as previously done.7 Participants with prevalent MCI at baseline were excluded from this analysis. Subjects with significant cognitive impairment at baseline were excluded from participation in the SPS3 trial.6
Vascular events and death
Additional secondary outcomes were all stroke, major vascular events, and all-cause death. All stroke consisted of either ischemic stroke (defined as a focal neurological deficit that persisted >24 hours with no hemorrhage present in cerebral imaging) and/or hemorrhagic stroke (defined as intracerebral, sub-/epidural, or subarachnoid hemorrhage).14 Major vascular event was defined as an acute hospital admission for a major vascular event, such as all stroke, or myocardial infarction [compatible clinical presentation and changes in ECG or cardiac enzyme levels]).
Statistical analysis
We summarized baseline characteristics by randomization group, and calculated descriptive statistics to evaluate differences between subgroups.
We used linear mixed models to assess the impact of WMH and disability on the relationship between BP targets and the change in CASI Z-score. We compared fixed-effects models with several covariance structures, as well as random-effects models, and chose the model with the lowest Akaike information criterion (fixed-effects model with an unstructured covariance). The model accounted for within-subject correlations due to repeated measures and for varying numbers of cognitive assessments across participants, and included a three-way interaction term between randomization group (and their two-way combinations), the categories of the effect modifier, time as a continuous measure. We used Cox proportional hazards models to assess the impact of effect modifiers on the relationship of BP targets with incident mild cognitive impairment, vascular events, and death. We assessed the proportional hazards assumption through 1) log-log plots, 2) introduction of time as an interaction term, and 3) Schoenfeld residuals. The models included a two-way interaction term with treatment and effect modifier (WMH, or disability). All models were adjusted for age, sex and race.
We conducted parallel Cox models for the secondary outcomes of all stroke, major vascular events, and all-cause mortality. In a prespecified sensitivity analysis, we restricted the analysis to hypertensive participants at baseline (systolic BP ≥130 mmHg, or on antihypertensive medication). In post-hoc exploratory analyses, we further adjusted for between-treatment group differences at baseline.
We used Stata (version 15.1, Stata Corporation) for data management and analysis, and R (version 3.5.1) for visualizations. Statistical significance was defined for all analyses as two-sided p<0.05.
The SPS3 trial is registered with ClinicalTrials.gov, number NCT00059306.
Results
Population characteristics
This study included 1,263 participants aged 65 years or older. Because randomization was not age-stratified, there were some modest baseline imbalances between randomized allocation groups; participants randomized to lower BP target were more likely to be female and more likely to have diabetes mellitus (Table 1). A higher proportion of participants in the lower BP target group had no or mild WMH, compared to participants in the higher BP target group, but between-group differences of baseline characteristics stratified by effect modifiers were not of clinically relevant magnitudes (eTables 1 and 2). Of the 1,227 participants with a baseline assessment of cognitive function, 567 (46%) had mild cognitive impairment at baseline, and 146 (12%) had no follow-up cognitive assessment.
Table 1:
Baseline characteristics of SPS3 Study participants aged 65 years or older by randomized blood pressure target group
| Lower BP target n = 618 |
Higher BP target n = 645 |
P-value | |
|---|---|---|---|
| Demographics | |||
| Age (years, mean±SD) | 73.9±6.0 | 73.7±5.9 | 0.46 |
| Female (n, %) | 266 (43) | 239 (37) | 0.03 |
| Race/ethnicity (n, %) | |||
| White | 352 (57) | 361 (56) | 0.76 |
| Hispanic | 205 (33) | 210 (33) | |
| Black | 51 (8) | 59 (9) | |
| Other | 10 (2) | 15 (2) | |
| Education (n, %) | |||
| 0–8 years | 398 (27) | 392 (26) | 0.90 |
| 9–12 years | 565 (38) | 581 (38) | |
| >12 years | 538 (36) | 546 (36) | |
| Cardiovascular risk factors | |||
| Blood pressure (mmHg, mean±SD) | |||
| Systolic | 144.4±19.3 | 143.7±18.3 | 0.47 |
| Diastolic | 75.2±9.9 | 76.2±10.1 | 0.08 |
| Body-mass index (kg/m2, mean±SD) | 27.6±5.6 | 27.8±5.0 | 0.41 |
| History of hypertension (n, %) | 475 (77) | 499 (77) | 0.83 |
| Diabetes mellitus (n, %) | 217 (35) | 194 (30) | 0.06 |
| Previous stroke or TIA (n, %) | 91 (15) | 95 (15) | 0.99 |
| History of ischemic heart disease | 59 (10) | 81 (13) | 0.09 |
| Current smoking (n, %) | 73 (12) | 59 (9) | 0.12 |
| CKD (eGFR < 60ml/min; n, %) | 155 (25) | 150 (23) | 0.45 |
| Medication | |||
| ACE inhibitors / AT2 antagonists | 417 (67) | 420 (65) | 0.38 |
| Calcium-channel blockers | 145 (23) | 152 (24) | 0.97 |
| Beta blockers | 145 (23) | 149 (23) | 0.88 |
| Diuretics | 199 (32) | 230 (36) | 0.20 |
| Other antihypertensive medications | 49 (8) | 51 (8) | 0.99 |
| Statin (n, %) | 413 (67) | 440 (68) | 0.60 |
| Modified Rankin stroke disability score (n, %) | |||
| 0 | 106 (17) | 101 (16) | 0.70 |
| 1 | 311 (50) | 346 (54) | |
| 2 | 130 (21) | 129 (20) | |
| 3 | 71 (11) | 69 (11) | |
| White Matter Hyperintensities (ARWMC score, n, %) | |||
| None/mild | 244 (40) | 213 (34) | 0.05 |
| Moderate | 196 (32) | 208 (33) | |
| Severe | 169 (28) | 206 (33) | |
| Barthel ADL limitations (n, %) | |||
| No limitations | 390 (63) | 432 (67) | 0.15 |
| 1+ limitations | 228 (37) | 213 (33) |
Abbreviations: ADL, activities of daily living; ARWMC, age-related white matter changes; BP, blood pressure; CKD, chronic kidney disease; CVD, cardiovascular disease; eGFR, estimated glomerular filtration rate; n, number; SD, standard deviation
Mean study follow-up time was 3.9 years (range 0.04 – 8.5, standard deviation [SD] 2.0). Median time from baseline to last cognitive assessment was 3 years (interquartile range 2 to 5 years). Average systolic BP remained within the specified treatment target throughout the follow-up period (eFigure 1). The mean number (±SD) of antihypertensives was 2.0±1.4 in the lower treatment target group and 1.5±1.3 in the higher treatment target group at one year follow-up (p <0.001), and 2.3±1.2 vs. 1.6±1.4 at the final study visit (p <0.001) (eTable 3). Rates of statin use in the lower and higher BP target groups remained similar throughout follow-up.
Effect modification by WMH and disability on the relationship of BP treatment targets and cognitive decline
Figure 1 and eTable 4 show the predicted mean CASI Z-scores at each assessment from baseline to year 5, stratified by the candidate effect modifiers of WMH and disability status. Cognitive function started lower and declined further in participants with severe WMH, but rates of decline did not differ by BP target (mean difference 0.00, 95%CI −0.07 to 0.07, p=0.80), and the overall test for difference in trajectories across the WMH strata was not statistically significant (p-value for interaction = 0.42). Participants with ADL disability at baseline had worse cognitive function at baseline and throughout follow-up, compared to those with no ADL limitations, but there was little apparent difference in trajectory by BP target in either strata (p-value for interaction = 0.66). Results were similar when we restricted the analysis to those with hypertension at baseline, or adjusted for baseline imbalances (eTable 5).
Figure 1:
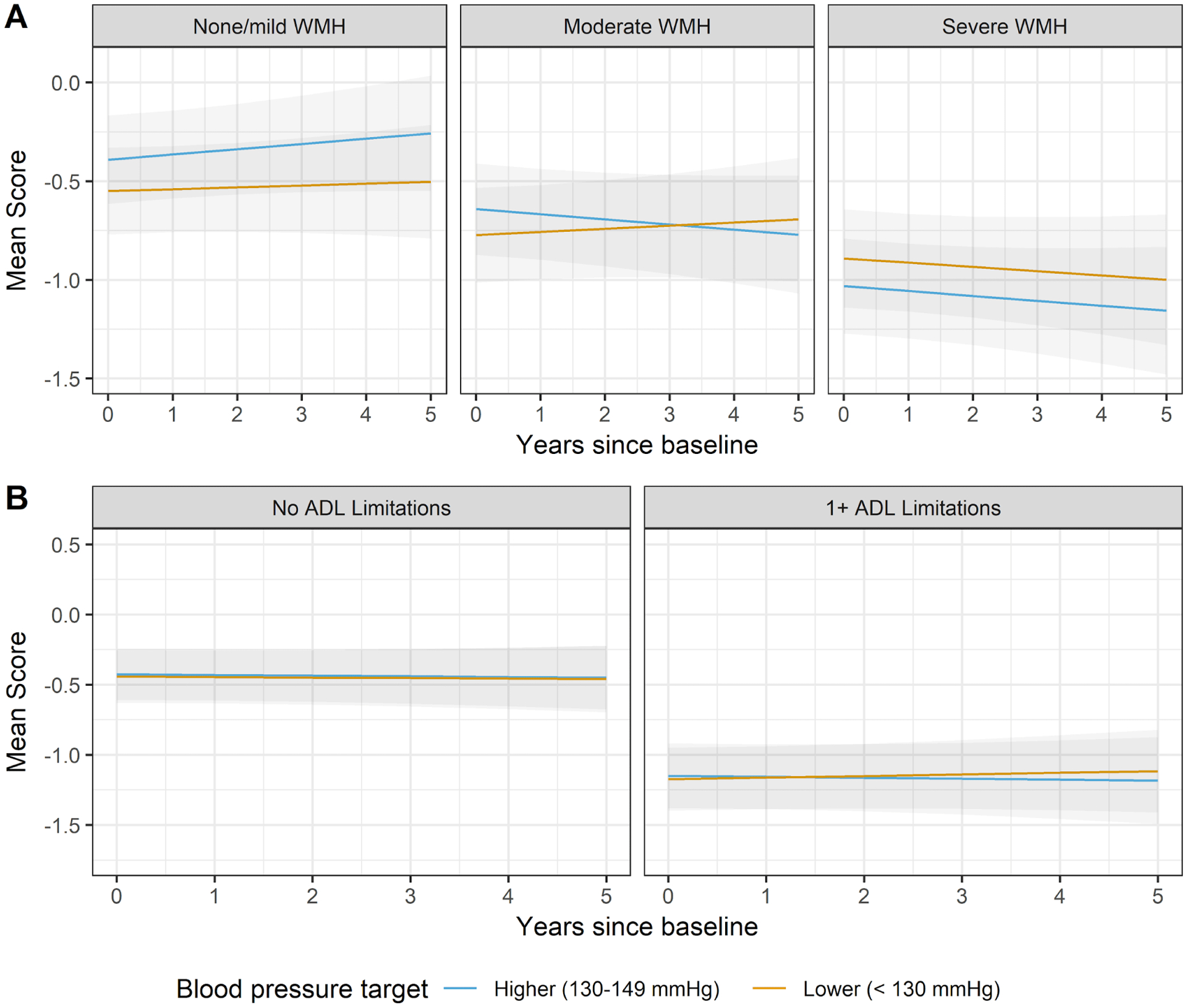
Predicted mean CASI Z-scores by treatment group and effect modifier
Panels: A: Stratified by white matter hyperintensities; B: Stratified by ADL limitations. Grey area represents 95% CI.
Abbreviations: ADL, activities of daily living; BP, blood pressure; CASI, Cognitive Abilities Screening Instrument; CI, confidence interval
Effect modification by WMH and disability on the relationship between BP treatment targets and incident mild cognitive impairment
Of 649 participants with adequate data to determine absence of mild cognitive impairment at baseline, 581 had at least one follow-up cognitive assessment. Of those 581, 190 (33%) met the criteria for mild cognitive impairment at one time during follow-up (Figure 2). Overall, annual rates of MCI were similar in the lower and higher BP target arms (12.0% vs. 12.7%, p=0.65), and there appeared to be little difference between BP targets when stratified by WMH or disability (p-values for interaction 0.85 and 0.47, respectively). Results were similar in sensitivity analyses restricting the analysis to those with hypertension at baseline, and after adjusting for baseline imbalances (eTable 6).
Figure 2:
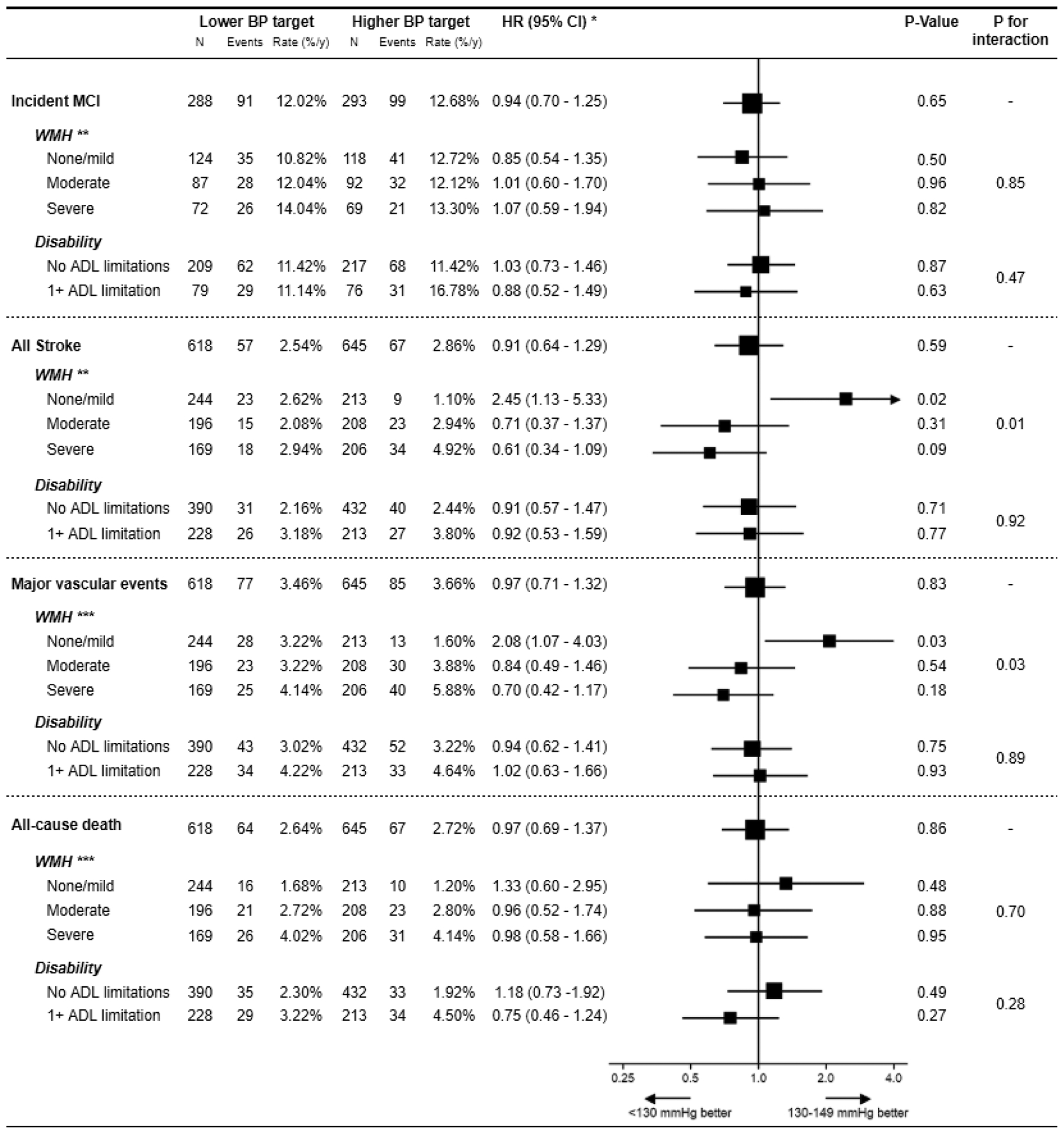
Effect modification of WMH and disability on incident mild cognitive impairment, vascular events, and death
* Lower vs. higher target. Analysis was adjusted for age, sex and race.
** WMH was missing for 19 participants (5 in lower BP target group, 14 in higher BP target group).
*** WMH was missing for 27 participants (9 in lower BP target group, 18 in higher BP target group).
Abbreviations: ADL, activities of daily living; BP, blood pressure; CI, confidence interval; HR, hazard ratio; MCI, mild cognitive impairment; N, number; WMH, white matter hyperintensities; y, year
Effect modification by WMH and disability on the relationship of BP treatment targets and vascular outcomes
Figure 2 shows event rates and hazard ratios for the vascular outcomes by level of WMH and disability. The effect of BP targets on risk of stroke and major vascular events appeared to differ substantially by WMH severity. In particular, the lower BP target was associated with increased risks of stroke and major vascular events among those with lower WMH, and with decreased risk among those with higher WMH (p-value for interaction = 0.01 for stroke, 0.03 for MVE). By contrast, the effect of BP targets on risk of stroke and major vascular events did not appear to differ by level of disability.
Among those with no/mild WMH, our analysis suggested that the lower BP target arm had a 33% increased risk of death, but confidence intervals were too wide to rule out the possibility of no effect. An association ranging from a 40% lower risk to a 3-fold higher risk, is also reasonably compatible with our data, given our assumptions. Results for all stroke were similar when we restricted the analysis to those with hypertension at baseline, or adjusted for baseline imbalances (eTable 7).
Discussion
In this study of older adults randomized to lower (<130 mmHg) vs. higher (130 – 149 mmHg) systolic BP target after a diagnosis of lacunar stroke, we found no evidence of cognitive benefit or harm with lower BP among participants with post-stroke disability or a higher burden of cerebral small vessel disease. Persons with post-stroke disability or severe cerebral small vessel disease had lower levels of cognitive function at baseline and over follow-up. Notably, we found that the effect of a lower BP target on stroke and major vascular events differed by the level of cerebral small vessel disease. Among those with moderate or severe WMH, the point estimate for vascular events was in the protective direction, whereas among those with no WMH, the effect of lower BP target was in the harmful direction. These data suggest that individuals with a history of lacunar stroke and evidence of small vessel disease will get greater benefit from a lower BP on prevention of subsequent vascular events, but no benefit or harm on cognitive function.
There are conflicting findings regarding the role of intensive BP targets on cognitive function and brain health. In the SPRINT trial, participants randomized to an intensive treatment target of <120 mmHg systolic had a reduced risk for mild cognitive impairment.5 However, both the SPS3 and ACCORD-MIND trials showed no effect of intensive BP control on cognitive function, and intensive BP control was associated with lower total brain volume at 40 months follow-up in ACCORD.6,19 In contrast, observational evidence suggests an adverse effect of lower BP on cognitive health, especially among those older adults with functional impairment. For example, data from the Leiden 85-Plus study showed that higher BP level was associated with lower risk for cognitive decline in longitudinal analyses.9 Associations of higher BP with lower risk for cognitive impairment have also been reported in an Italian cohort,20 and a recent study from our group demonstrated that elevated systolic BP (≥140 mmHg) was associated with an increase in cognitive function among older adults with a disability.10 Some have suggested that heterogeneity in vascular disease and functional status could explain these apparently conflicting effects, but our study found no evidence of effect modification with BP lowering on cognitive outcomes in the SPS3 trial. Another potential explanation for the discrepant findings stems from observational data showing that midlife hypertension contributes to late-life cognitive decline, an effect that would be absent in typical shorter trial periods.21,22
Interestingly, we did find evidence that small vessel disease modified the benefit of a lower BP target on major vascular events in older adults. A previous analysis of the entire SPS3 population had found a significant interaction between ARWMC score and BP target for all stroke, but no significant between-group differences within WMH tertiles.23 Our findings suggest that older adults with a history of lacunar stroke and with moderate or severe WMH derive greater benefit from a lower BP target than those with no WMH. The 2014 American Heart Association / American Stroke Association guidelines on the secondary prevention after stroke recommend antihypertensive treatment initiation with systolic BP ≥140 mmHg, with an individualized treatment target, stating reasonable targets as systolic BP <140 mmHg for ischemic stroke or TIA, and <130 mmHg for lacunar stroke.2 Our findings show that treatment response may depend on the burden of cerebral small vessel disease in elderly patients. While caution must be used in the interpretation of results from this secondary trial analysis, and the results should be confirmed in other studies, our findings support reasoning for an individualized BP treatment goal.
There are potential pathophysiological mechanisms for our findings: In patients with more severe vascular disease burden, the reduction of vascular risk might overpower the potential adverse effects of BP lowering. Conversely, patients with no or mild small vessel disease may be at lower vascular risk (e.g. lower stroke recurrence risk) and may thus benefit less from lower BP targets, but still experience potential adverse effects such as inadequate organ perfusion. It is also possible that the lack of cerebral small vessel disease selects a subtype of stroke patients where hypertension is not a primary stroke risk contributor.
A major strength of our study is the use of clinical trial data to test for heterogeneous treatment effects, which lowers the likelihood that any apparent differences in the effect of lower BP are due to confounding factors. However, the results of this study should be interpreted in light of several limitations. First, the participants of the SPS3 trial generally had mild strokes as measured by the Modified Rankin Scale.12 Our results may thus not be generalizable to patients with more severe stroke symptoms or to the general population. Second, data on WMH were available at baseline only, and adjustment for changes in WMH volume or severity was not possible. Third, the SPS3 trial was stopped 10 months early due to an interim analysis showing no between-treatment group difference in stroke recurrence but an increased risk of major bleedings, which limited follow-up data on vascular and cognitive outcomes. Fourth, this study was a post-hoc analysis of trial data, and false positive results cannot be excluded. Fifth, it is unclear why our finding of effect modification for vascular events did not extend to cognitive outcomes. Future research should explore whether other factors can systematically identify subpopulations who may derive greater or lesser cognitive benefit from intensive BP control.
Conclusion
In this secondary analysis of the SPS3 trial, using data from 1,263 patients aged 65 years and older with a recent lacunar stroke, a lower systolic BP treatment goal <130 mmHg was not associated with higher risk for cognitive decline or mild cognitive impairment, and no evidence of harm was found for patients with disability or higher burden of cerebral small vessel disease. Conversely, a lower systolic BP treatment goal was associated with higher risk for subsequent stroke and major vascular events in patients with no or mild evidence of small cerebral vessel disease, as compared to a higher treatment goal of 130–149 mmHg. Future clinical trials on secondary prevention after vascular events should further investigate the influence of functional status and small vessel disease on treatment response, particularly in older adults.
Supplementary Material
Sources of support:
SPS3 was an investigator initiated study funded by a cooperative agreement from the National Institute of Neurological Disorders and Stroke of United States (Grant #2 U01 NS38529-04A1). Dr. Blum’s work was supported by a grant from the Swiss National Science Foundation (P2BEP3_175289). Dr. Peralta’s and Dr. Odden’s work was supported by a grant from the National Institute on Aging (Grant number R01AG046206).
Footnotes
Declaration of interest: Carmen Peralta is the Chief Medical Officer and has ownership in Cricket Health.
References
- 1.Regenhardt RW, Das AS, Lo EH, Caplan LR. Advances in Understanding the Pathophysiology of Lacunar Stroke: A Review. JAMA Neurol. 2018;75(10):1273. doi: 10.1001/jamaneurol.2018.1073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–2236. doi: 10.1161/STR.0000000000000024 [DOI] [PubMed] [Google Scholar]
- 3.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. The Lancet. 2016;388(10046):761–775. doi: 10.1016/S0140-6736(16)30506-2 [DOI] [PubMed] [Google Scholar]
- 5.Williamson JD, Pajewski NM, Auchus AP, et al. Effect of Intensive vs Standard Blood Pressure Control on Probable Dementia: A Randomized Clinical Trial. JAMA. 2019;321(6):553–561. doi: 10.1001/jama.2018.21442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pearce LA, McClure LA, Anderson DC, et al. Effects of long-term blood pressure lowering and dual antiplatelet treatment on cognitive function in patients with recent lacunar stroke: a secondary analysis from the SPS3 randomised trial. Lancet Neurol. 2014;13(12):1177–1185. doi: 10.1016/S1474-4422(14)70224-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacova C, Pearce LA, Costello R, et al. Cognitive impairment in lacunar strokes: The SPS3 trial. Ann Neurol. 2012;72(3):351–362. doi: 10.1002/ana.23733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charlesworth CJ, Peralta CA, Odden MC. Functional Status and Antihypertensive Therapy in Older Adults: A New Perspective on Old Data. Am J Hypertens. 2016;29(6):690–695. doi: 10.1093/ajh/hpv177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sabayan B, Oleksik AM, Maier AB, et al. High Blood Pressure and Resilience to Physical and Cognitive Decline in the Oldest Old: The Leiden 85-Plus Study. J Am Geriatr Soc. 2012;60(11):2014–2019. doi: 10.1111/j.1532-5415.2012.04203.x [DOI] [PubMed] [Google Scholar]
- 10.Miller LM, Peralta CA, Fitzpatrick AL, et al. The role of functional status on the relationship between blood pressure and cognitive decline: the Cardiovascular Health Study. J Hypertens. May 2019. doi: 10.1097/HJH.0000000000002102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prins ND, Scheltens P. White matter hyperintensities, cognitive impairment and dementia: an update. Nat Rev Neurol. 2015;11(3):157–165. doi: 10.1038/nrneurol.2015.10 [DOI] [PubMed] [Google Scholar]
- 12.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. J Am Coll Cardiol. 2018;71(19):e127–e248. doi: 10.1016/j.jacc.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 13.Nasrallah IM, Pajewski NM, Auchus AP, et al. Association of Intensive vs Standard Blood Pressure Control With Cerebral White Matter Lesions. JAMA. 2019;322(6):524–534. doi: 10.1001/jama.2019.10551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.SPS3 Study Group, Benavente OR, Coffey CS, Conwit R, Hart RG, McClure LA, Pearce LA, Pergola PE, Szychowski JM. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. The Lancet. 2013;382(9891):507–515. doi: 10.1016/S0140-6736(13)60852-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Benavente OR, White CL, Pearce L, et al. The Secondary Prevention of Small Subcortical Strokes (SPS3) Study. Int J Stroke. 2011;6(2):164–175. doi: 10.1111/j.1747-4949.2010.00573.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wahlund LO, Barkhof F, Fazekas F, et al. A New Rating Scale for Age-Related White Matter Changes Applicable to MRI and CT. Stroke. 2001;32(6):1318–1322. doi: 10.1161/01.STR.32.6.1318 [DOI] [PubMed] [Google Scholar]
- 17.Mahoney FI, Barthel DW. FUNCTIONAL EVALUATION: THE BARTHEL INDEX. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 18.Teng EL, Hasegawa K, Homma A, et al. The Cognitive Abilities Screening Instrument (CASI): A Practical Test for Cross-Cultural Epidemiological Studies of Dementia. Int Psychogeriatr. 1994;6(1):45–58. doi: 10.1017/S1041610294001602 [DOI] [PubMed] [Google Scholar]
- 19.Launer LJ, Miller ME, Williamson JD, et al. Effects of intensive glucose lowering on brain structure and function in people with type 2 diabetes (ACCORD MIND): a randomised open-label substudy. Lancet Neurol. 2011;10(11):969–977. doi: 10.1016/S1474-4422(11)70188-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mossello E, Pieraccioli M, Nesti N, et al. Effects of low blood pressure in cognitively impaired elderly patients treated with antihypertensive drugs. JAMA Intern Med. 2015;175(4):578–585. doi: 10.1001/jamainternmed.2014.8164 [DOI] [PubMed] [Google Scholar]
- 21.Qiu C, Winblad B, Fratiglioni L. The age-dependent relation of blood pressure to cognitive function and dementia. Lancet Neurol. 2005;4(8):487–499. doi: 10.1016/S1474-4422(05)70141-1 [DOI] [PubMed] [Google Scholar]
- 22.Iadecola Costantino, Yaffe Kristine, Biller José, et al. Impact of Hypertension on Cognitive Function: A Scientific Statement From the American Heart Association. Hypertension. 2016;68(6):e67–e94. doi: 10.1161/HYP.0000000000000053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ikeme JC, Pergola PE, Scherzer R, et al. Cerebral White Matter Hyperintensities, Kidney Function Decline, and Recurrent Stroke After Intensive Blood Pressure Lowering: Results From the Secondary Prevention of Small Subcortical Strokes (SPS3) Trial. J Am Heart Assoc. February 2019. http://www.ahajournals.org/doi/abs/10.1161/JAHA.118.010091. Accessed October 20, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


