Abstract
Brain abscess is a rare but life-threatening condition. Intracardiac or extracardiac right-to-left shunting in patients with unrepaired cyanotic congenital heart disease, pulmonary arteriovenous malformations, or venovenous collaterals allows microbes unfiltered access to the brain. Brain abscess must be considered when cyanotic patients present with headache. (Level of Difficulty: Beginner.)
Key Words: brain abscess, cyanosis, Fontan
Abbreviations and Acronyms: AVM, arteriovenous malformation; CT, computed tomography; MRI, magnetic resonance imaging
Graphical abstract
Brain abscess is a rare but life-threatening condition. Intracardiac or extracardiac right-to-left shunting in patients with unrepaired cyanotic…
History of Presentation
A 15-year-old female patient, status post–nonfenestrated extracardiac Fontan, presented to the emergency department with throbbing frontal headache and malaise. She reported temporary pain relief with acetaminophen but had increasing headache intensity over the preceding 5 days. There was no photophobia, phonophobia, head trauma, fever, nausea, or vomiting. Parents had observed increased somnolence for 1 day prior to presentation. Neurologic status in the emergency room was normal and head imaging was not performed. The patient had an oxygen saturation of 82% and an otherwise reassuring examination. A complete blood count, hepatic panel, ammonia level, and urinalysis were normal. Aside from mild hyponatremia, there was no significant electrolyte disturbance. Admission for observation was considered, but her pain improved with acetaminophen and she was discharged home. After 48 h, she returned with recurrent symptoms. Neurology recommended migraine treatment with intravenous fluids, prochlorperazine, and valproic acid, none of which resulted in improvement. Given the persistent headache, she was admitted to the general pediatrics service, where she received subsequent doses of analgesics and antiemetics. Oxygen saturations remained in the 80s. An echocardiogram was unchanged from her prior studies. Head imaging was not performed, as her neurologic exam remained nonfocal. She was discharged home the following day after reporting improvement in headache but returned 5 days later with fever, tachycardia, and lethargy. Her oxygen saturation was 88%.
Learning Objectives
-
•
To understand that patients with palliated congenital heart disease, pulmonary AVMs, and venovenous collaterals are at increased risk for brain abscess.
-
•
To recognize clinical factors that should heighten the suspicion of brain abscess formation in such patients, including desaturation that is otherwise unexplained.
-
•
To identify situations in which a lower threshold for brain imaging should be considered in cyanotic patients presenting with headache.
Past Medical History
Born with heterotaxy, polysplenia, and an unbalanced, right-dominant atrioventricular canal defect that was deemed unsuitable for biventricular repair, the patient followed a single ventricle pathway, with Fontan palliation at 3 years of age using a 16-mm extracardiac nonfenestrated conduit (Figure 1). Diagnostic catheterization at 12 years of age showed progressive Fontan baffle obstruction and small left-sided pulmonary arteriovenous malformations (AVMs). Thus, she underwent revision with a 20-mm Fontan conduit. Repeat cardiac catheterization was performed at 13 years of age to address pulmonary artery stenosis, and a network of small venovenous collaterals was noted. Device occlusion of a single large collateral (Figure 2) was performed at that time. She had no prior history of migraines, serious bacterial infections, or endocarditis. Two capped teeth were extracted approximately 2 months prior to presentation due to adjacent gum swelling, and a course of antibiotics had been completed.
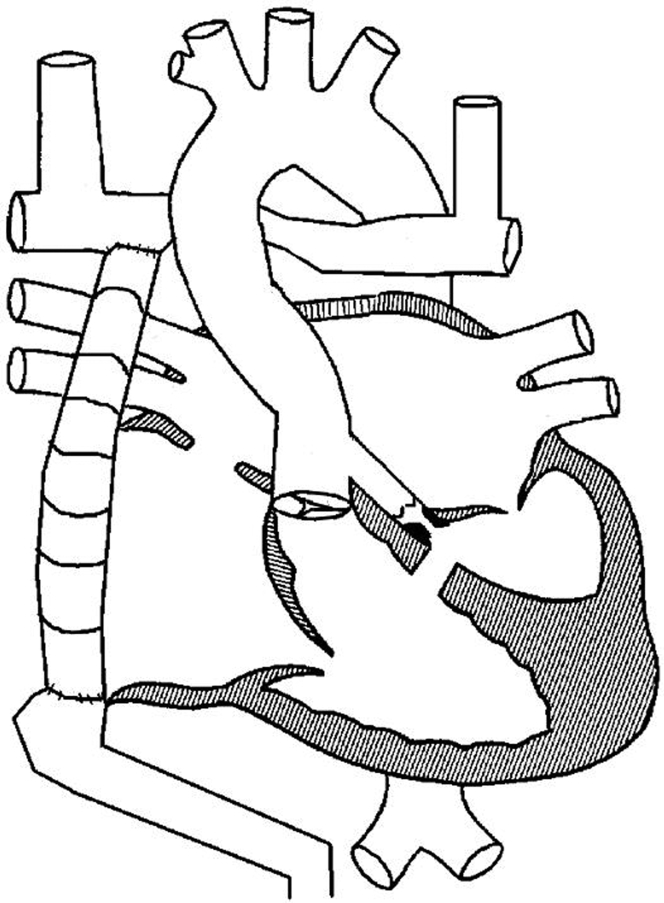
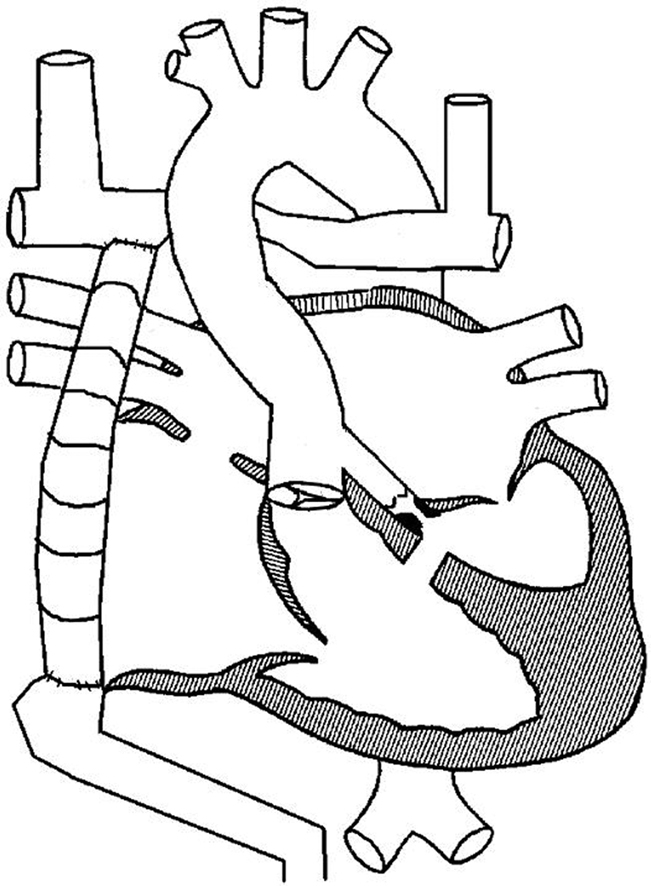
Figure 1.
Line Drawing Representing the Patient’s Complex Cardiac Anatomy
Pulmonary blood flow is passively supplied by bilateral bidirectional Glenn circuits and a nonfenestrated extracardiac Fontan conduit while systemic cardiac output is provided by pulmonary venous blood flow through the reconstructed aortic arch. Not depicted are the patient’s pulmonary arteriovenous malformations and venovenous collateral vessels.
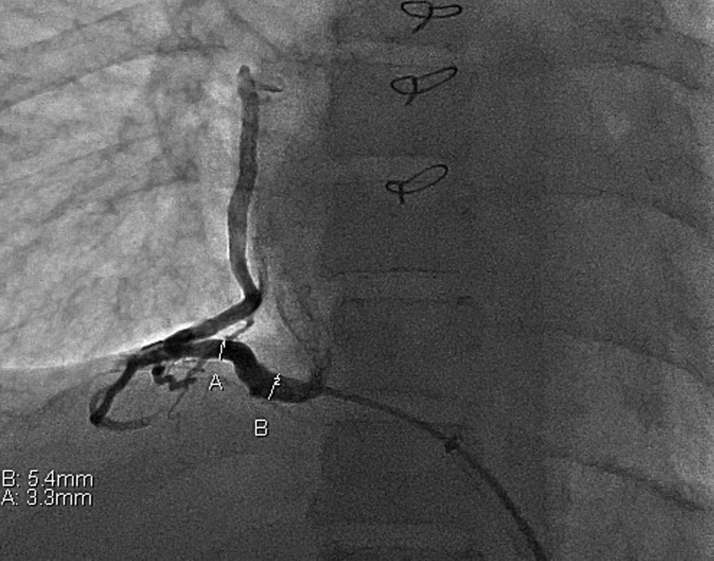
Figure 2.
Still Image From the Patient’s Cardiac Catheterization Approximately 1 Year Prior to Her Case Presentation
In this anteroposterior projection, contrast is seen filling a large, right-sided collateral vessel that arises from the inferior vena cava and drains desaturated blood into the right-sided pulmonary veins.
Differential Diagnosis
The differential diagnosis for headache, fever, and lethargy includes intracranial mass such as abscess or tumor, ischemic or hemorrhagic stroke, medication overdose or accidental ingestion, and overwhelming sepsis, among other possibilities. Migraine or tension headache, while considerations initially, are less likely in the setting of an obtunded patient with fever and tachycardia.
Investigations
After rapid assessment in the emergency department on the third visit, noncontrast head computed tomography (CT) showed a right temporal lobe mass with vasogenic edema and midline shift. Leukocytosis was present, with a white blood cell count of nearly 20,000, and a C-reactive protein level was elevated at 8.3 mg/dl. Blood cultures were drawn and hypertonic saline, corticosteroids, and levetiracetam were given. Rapid-sequence magnetic resonance imaging (MRI) showed a large, peripherally enhancing lesion measuring approximately 6 cm in diameter, consistent with brain abscess (Figure 3). The patient was taken to the operating room, where emergent craniectomy confirmed a purulent abscess. Transthoracic and transesophageal echocardiography showed normal single-ventricle systolic function, patent Fontan and Glenn circuits, and no evidence of thrombus or vegetation. A dental examination performed during hospitalization was not concerning for active dental decay or infection. No primary source of infection was identified by clinical examination or imaging.
Figure 3.
Images From the Patient’s Brain Magnetic Resonance Imaging With Contrast Upon Presentation
Axial, coronal, and sagittal cuts demonstrate a large peripherally enhancing mass centered in the right anterior temporal lobe. The mass measures approximately 5.5 × 3.8 × 5.2 cm and up to 6.3 cm in greatest oblique anteroposterior dimension. There is internal restricted diffusion consistent with abscess. Marked surrounding vasogenic edema is present, with resultant mass effect on surrounding structures and 0.9-cm midline shift.
Management
Abscess cultures grew Streptococcus intermedius, which was treated with intravenous ceftriaxone and metronidazole. Serial brain imaging over the course of hospitalization showed improvement in midline shift and eventual resolution of cerebral edema. The patient returned to her neurologic baseline approximately 2 weeks after abscess drainage and completed an 8-week antibiotic course. Nine months after diagnosis, she continues to do well but remains desaturated to the upper 80s and low 90s due to the fine venovenous collateral network that is not amenable to coil embolization.
Discussion
Because of its rarity in the pediatric population, cardiogenic brain abscess has been not been extensively studied. Current literature suggests that right-to-left shunting resulting from unrepaired cyanotic congenital heart disease and pulmonary AVMs increases the likelihood of brain abscess by allowing pathogens direct access to the systemic vasculature. Focal areas of tissue hypoxia in the brain may also create a suitable environment for abscess formation (1). Adult patients with pulmonary AVMs are at increased risk of brain abscess compared with the general population, and the risk increases with more profound hypoxia (2). Venovenous collaterals create similar routes for bacteria to bypass the filtering effects of the lungs. Both of these vascular malformations are associated with the Fontan circulation.
Patients with brain abscess often present with nonspecific features. In a recent retrospective analysis of 26 patients with complex congenital heart disease, headache, and vomiting were the most common presenting symptoms. Fever was present in about 30% of patients, laboratory markers of infection in 20%, and focal neurologic deficits in a mere 15% (3). When brain abscess is suspected, recommendations include rapid acquisition of blood work, including complete blood count, inflammatory markers, and a blood culture, as well as urgent brain CT. Lumbar puncture may be performed if not contraindicated, and if rapid-sequence MRI is available, this modality may be helpful in delineating the lesion further. A thorough otolaryngology examination, cardiac evaluation with echocardiography, skin inspection, and dental examination are recommended as well to identify any primary source of infection. Chest roentgenogram or chest CT may also be performed if there is suspicion for primary lung disease (4).
This case demonstrates the challenge of diagnosing brain abscess in pediatric patients with complex congenital heart disease. The report of frontal headache responsive to analgesia alone unaccompanied by focal neurologic deficits or fever seemed to result in delayed diagnosis, yet the decision to perform head imaging is sometimes difficult, given the effects of repeated radiation exposure over time. In retrospect, the patient’s increased somnolence could have been interpreted as a change in baseline neurologic status, prompting earlier head imaging in the setting of cyanosis and persistent headache.
Follow-Up
After successful completion of her antibiotic course, the patient experienced no clinical or radiographic evidence of recurrent infection. There were no obvious residual neurologic deficits, although she developed unusual, painful sensations in her lower extremities near the end of her antibiotic treatment that have improved over time. Contrast MRI of her lower spine was negative for meningeal or nerve root enhancement, and the etiology of this neuropathy remains unclear. She continues to follow-up frequently with her cardiologist, given her single-ventricle physiology.
Conclusions
Conventional teaching is that intracardiac right-to-left shunting resulting from partially palliated cyanotic heart disease results in an increased risk for brain abscess formation, but we often neglect to remember that, despite surgical separation of the systemic venous and arterial circulations in the nonfenestrated Fontan circuit, pulmonary AVMs or venovenous collaterals develop spontaneously over time, increasing the risk for brain abscess. Lower-than-normal oxygen saturations in Fontan patients without an alternate etiology should alert the physician to these conditions. Although rare, brain abscess should remain on the differential for any Fontan patient with persistent headache, especially when accompanied by hypoxia and neurologic changes.
Footnotes
All authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
References
- 1.Takeshita M., Kagawa M., Yonetani H. Risk factors for brain abscess in patients with congenital cyanotic heart disease. Neurol Med Chir (Tokyo) 1992;32:667–670. doi: 10.2176/nmc.32.667. [DOI] [PubMed] [Google Scholar]
- 2.Boother E.J., Brownlow S., Tighe H.C., Bamford K.B., Jackson J.E., Shovlin C.L. Cerebral abscess associated with odontogenic bacteremias, hypoxemia, and iron loading in immunocompetent patients with right-to-left shunting through pulmonary arteriovenous malformations. Clin Infect Dis. 2017;65:595–603. doi: 10.1093/cid/cix373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Udayakumaran S., Onyia C.U., Kumar R.K. Forgotten? Not yet. Cardiogenic brain abscess in children: a case series-based review. World Neurosurg. 2017;107:124–129. doi: 10.1016/j.wneu.2017.07.144. [DOI] [PubMed] [Google Scholar]
- 4.Mameli C., Genoni T., Madia C., Doneda C., Penagini F., Zuccotti G. Brain abscess in pediatric age: a review. Childs Nerv Syst. 2019;35:1117–1128. doi: 10.1007/s00381-019-04182-4. [DOI] [PubMed] [Google Scholar]