Abstract
A patient with alveolar capillary dysplasia has survived more than 56 months with medical therapy. Intrauterine exposure to metformin potentially modified the severity of disease. In combination with other agents, endothelin receptor antagonists and amlodipine have been key medications in lowering pulmonary arterial pressure and managing right heart failure. (Level of Difficulty: Beginner.)
Key Words: echocardiography, pulmonary hypertension, right-sided heart catheterization
Abbreviations and Acronyms: ACD, alveolar capillary dysplasia; iNO, inhaled nitric oxide; PH, pulmonary hypertension
Graphical abstract
A patient with alveolar capillary dysplasia has survived more than 56 months with medical therapy. Intrauterine exposure to metformin potentially…
The majority of patients with alveolar capillary dysplasia (ACD) die in early infancy from respiratory failure with hypoxemia and pulmonary hypertension (1). However, a recent report has reviewed several patients with an atypical phenotype and relatively long survival (2). The role of medical therapy in ACD is unknown because atypical patients may be overlooked if genetic testing or a histological evaluation is not performed. Here, we report a patient who has survived for more than 56 months with medical therapy including key agents that potentially modified the severity of pulmonary vascular disease or lowered pulmonary artery pressure.
Learning Objectives
-
•
To demonstrate that rare patients with alveolar capillary dysplasia can be treated long term with medical therapy.
-
•
To highlight key elements of medical care that potentially modified the severity of pulmonary vascular disease or improved cardiovascular function.
History of Presentation
A 43-year-old woman developed gestational diabetes and started treatment with metformin 1,000 mg/day at 14 weeks’ gestation. The dose was increased to 2,000 mg/day at 17 weeks’ gestation. A fetal right pleural effusion, noted during the third trimester, resolved before birth. A male neonate was born at a gestational age of 37 weeks. He developed acute respiratory failure and pulmonary hypertension (PH) during the first day of life. Hypoxemia and PH persisted despite treatment with high-frequency oscillatory ventilation, surfactant, and inhaled nitric oxide (iNO). He was transported and supported with venous/venous extracorporeal membrane oxygenation from 17 h of age to 6 days of age. In addition to iNO, inpatient therapy included epoprostenol, sildenafil, and bosentan. His end-systolic eccentricity index, a measure of ventricular septal flattening or increased systolic pulmonary arterial pressure, normalized after the onset of treatment with bosentan, allowing iNO and epoprostenol to be stopped.
Management
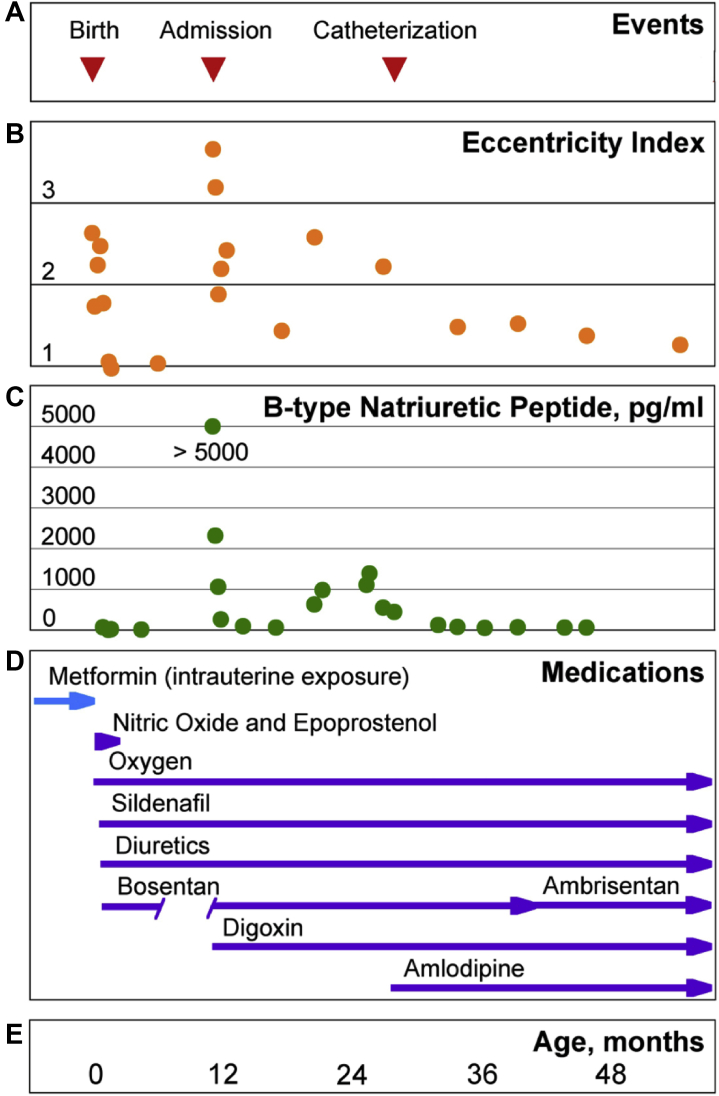
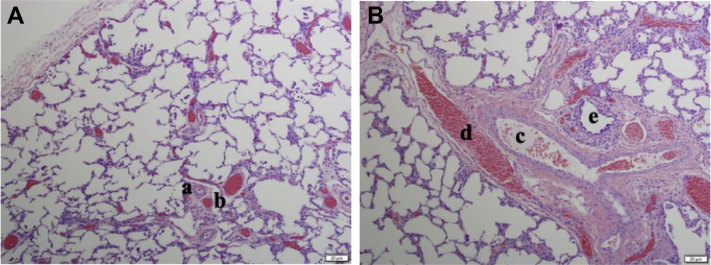
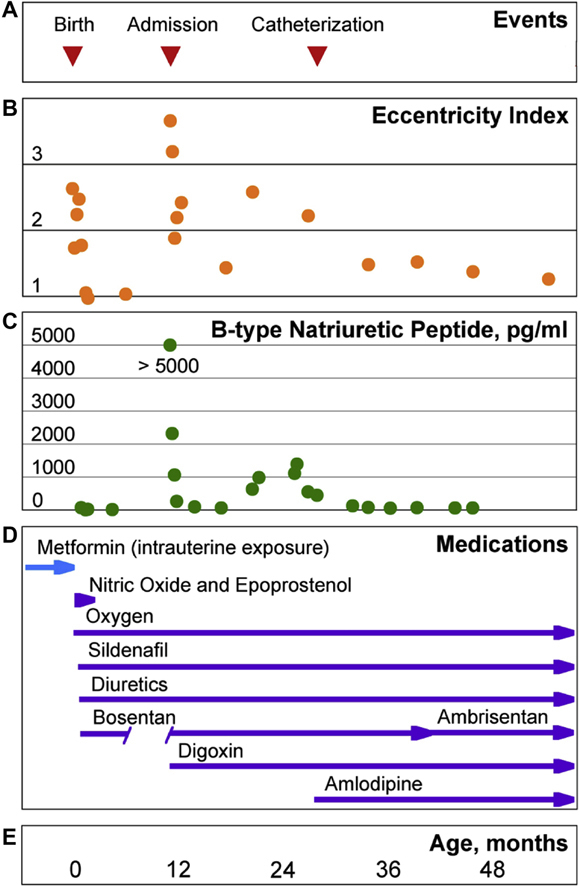
Figure 1 shows his clinical course over time with noteworthy events, end-systolic eccentricity indices, B-type natriuretic peptide levels, and medications. He was initially treated as an outpatient with sildenafil, bosentan, furosemide, and full-time supplemental oxygen. His clinical course was consistent with resolving pulmonary hypertension. Bosentan was discontinued, and he was transitioned from full-time oxygen to nighttime oxygen. He was admitted to the hospital at 10 months of life with evidence of severe PH and right heart failure. Airway secretions tested positive for rhinovirus and beta-lactamase–negative Hemophilus influenza. A high-resolution computed tomography scan of the chest showed bilateral ground glass opacities and septal thickening. A lung biopsy showed evidence of “a mild form of alveolar capillary dysplasia with misalignment of the pulmonary veins,” as shown in Figure 2. Genetic testing revealed a c.246C>G (p.F82L) heterozygous, novel, and de novo variant in the FOXF1 gene. He was again treated as an outpatient with sildenafil, full-time oxygen, and furosemide, with the addition of bosentan, digoxin, chlorothiazide, spironolactone, beclomethasone, albuterol, and aspirin.
Figure 1.
Chronological Summary of Medical Care
(A) Key events (upper section); (B) Serial measurements of the end-systolic eccentricity index, an echocardiographic estimate of the ratio of systolic pulmonary to systolic systemic arterial pressure (normal: 1.00). Waveforms of tricuspid valve regurgitation were rarely adequate to estimate the right ventricular systolic pressure by echocardiography. (C) Serial measurements of B-type natriuretic peptide, a gauge of right heart function (normal: <100 pg/ml). (D) Medications. (E) Age.
Figure 2.
Histology Samples Demonstrating a Mild Variant of Alveolar Capillary Dysplasia
(A) There is medial muscularization of the intralobular arterioles (a) with adjacent dilated venules (b). (B) A thickened pulmonary arteriole (c) is surrounded by an adjacent bronchial venule (d, misaligned pulmonary vein) and bronchiole (e). In both images, the capillary bed is diminished, and there is heterogeneous alveolar septal thickening. The lack of homogenous septal thickening demonstrates a milder pattern in this disease process.
During the subsequent year, he again developed findings consistent with a mild increase in the severity of PH and right heart failure. A hemodynamic evaluation was performed at 25 months of life to explore options for treatment with additional medications. The results of heart catheterization and acute vasodilator testing are shown in Table 1. His response to supplemental oxygen with iNO suggested that he may benefit from treatment with a calcium-channel blocker. His acute response to intravenous nicardipine confirmed that this may be an appropriate option for precision care. Over time, his end-systolic eccentricity indices and B-type natriuretic peptide levels have improved while he is being treated with amlodipine. He is able to perform at the same level of physical activity as his healthy siblings. He has not developed evidence of right heart failure despite occasional respiratory infections. He is currently being treated with sildenafil, ambrisentan, amlodipine, digoxin, furosemide, aspirin, fluticasone, and blow-by oxygen at night.
Table 1.
Arterial Blood Gases, Pressure Measurements, and Hemodynamic Calculations
| 35% Oxygen | 100% Oxygen | 100% Oxygen Nitric Oxide 20 ppm |
100% Oxygen | 100% Oxygen Nicardipine 3 μg/kg/min |
|
|---|---|---|---|---|---|
| pH | 7.39 | 7.41 | 7.40 | 7.41 | 7.39 |
| Pao2, mm Hg | 101 | 308 | 349 | 356 | 309 |
| mPAP, mm Hg | 51 | 49 | 39 | 47 | 43 |
| mLAP, mm Hg | 7 | — | — | — | — |
| mSAP, mm Hg | 47 | 49 | 44 | 52 | 47 |
| mRAP, mm Hg | 7 | — | — | — | — |
| CI, l/min/m2 | 3.09 | 2.72 | 2.81 | 2.65 | 2.72 |
| Rp, U·m2 | 14.2 | 15.4 | 11.4 | 15.1 | 13.2 |
| Rs, U·m2 | 12.9 | 15.4 | 14.4 | 17.0 | 14.7 |
CI = cardiac index; mLAP = mean left atrial pressure; mPAP = mean pulmonary arterial pressure; mRAP = mean right atrial pressure; mSAP = mean systemic arterial pressure; Pao2 = systemic arterial oxygen tension; Rp = pulmonary vascular resistance index; Rs = systemic vascular resistance index.
Discussion
This case describes a patient with a variant in the FOXF1 gene and histological findings consistent with a mild form of ACD who has survived for more than 56 months. It is possible that intrauterine exposure to metformin modified the severity of disease. We do not know whether medical therapy modified the severity of disease following birth. However, a combination of medications has provided enough cardiovascular support for him to participate in age-appropriate activities. Only 2 other reported children with ACD have lived longer than 2 years without lung transplantation (2). A favorable outcome potentially depends on the extent of arteriolar obstruction and intrapulmonary shunting through bronchial veins and venules (3,4). Furthermore, some patients may respond favorably to specific medications.
Variants in FOXF1 may inhibit STAT3, a critical transcriptional regulator of angiogenesis, and cause ACD in the mouse (5). Metformin may also inhibit STAT3 signaling, raising concern that intrauterine exposure might further exacerbate the disease process. However, metformin might modify the severity of disease when STAT3 signaling is suppressed with a genetic variant by facilitating angiogenesis through other pathways during vascular development, including an increase in adenosine monophosphate–activated protein kinase signaling (6). If so, additional studies are needed to determine whether there is a critical period before or after birth when metformin could favorably modify the severity of ACD. None of the previous reports of atypical ACD included a maternal medication history (2).
Additional potential key elements of care are medications that decrease pulmonary vascular resistance. We do not know whether iNO, epoprostenol and sildenafil independently influenced early survival. However, eccentricity indices improved with these agents and normalized after treatment with bosentan. Clinical worsening occurred after stopping bosentan, suggesting that endothelin receptor antagonists have been key medications for long-term care. However, we acknowledge that clinical worsening could have occurred with a respiratory infection even if bosentan was continued. iNO decreased pulmonary arterial pressure during heart catheterization at 2 years of age. If available in the future, iNO may be a key option for the long-term precision care of our patient. Intravenous nicardipine acutely improved pulmonary arterial pressure to a lesser extent than iNO. Accordingly, amlodipine has provided long-term precision care.
Conclusions
A small subset of patients with ACD may survive with medical therapy. Additional studies are needed to determine whether metformin or other agents may modify the severity of disease during pulmonary vascular development. For this patient, key agents were identified when clinical worsening occurred following withdrawal of a medication and when pulmonary arterial pressure decreased during acute vasodilator testing. Precision care may prevent right heart failure and improve functional capacity by maintaining the lowest attainable pulmonary vascular resistance.
Acknowledgments
The institutional review board of the University of Utah approved this study (IRB_00033414) and waived the need for informed consent.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
References
- 1.Bishop N.B., Stankiewicz P., Steinhorn R.H. Alveolar capillary dysplasia. Am J Respir Crit Care Med. 2011;184:172–179. doi: 10.1164/rccm.201010-1697CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edwards J.J., Murali C., Pogoriler J. Histopathological and genetic features of alveolar capillary dysplasia with atypical late presentation and prolonged survival. J Pediatr. 2019;210:214–219. doi: 10.1016/j.jpeds.2019.01.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galambos C., Sims-Lucas S., Ali N., Gien J., Dishop M.K., Abman S.H. Intrapulmonary vascular shunt pathways in alveolar capillary dysplasia with misalignment of pulmonary veins. Thorax. 2015;70:84–85. doi: 10.1136/thoraxjnl-2014-205851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norvik C.C., Westöö C.K., Peruzzi N. Synchrotron-based phase contrast micro-CT as a tool for understanding pulmonary vascular pathobiology and the 3-D micro-anatomy of alveolar capillary dysplasia. Am J Physiol Lung Cell Mol Physiol. 2020;318:L65–L75. doi: 10.1152/ajplung.00103.2019. [DOI] [PubMed] [Google Scholar]
- 5.Pradhan A., Dunn A., Ustiyan V. The S52F FOXF1 mutation inhibits STAT3 signaling and causes alveolar capillary dysplasia. Am J Respir Crit Care Med. 2019;200:1045–1056. doi: 10.1164/rccm.201810-1897OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teng R.J., Du J., Afolayan A.J., Eis A., Shi Y., Konduri G.G. AMP kinase activation improves angiogenesis in pulmonary artery endothelial cells with in utero pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol. 2013;304:L29–L42. doi: 10.1152/ajplung.00200.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]