Abstract
Objective
To estimate the incidence of hospitalization for reversible cerebral vasoconstriction syndrome (RCVS), we identified RCVS-related hospital admissions across 11 US states in 2016.
Methods
We tested the validity of ICD-10 code I67.841 in 79 patients with hospital admissions for RCVS or other cerebrovascular diseases at 1 academic and 1 community hospital. After determining that this code had a sensitivity of 100% (95% confidence interval [CI], 82%–100%) and a specificity of 90% (95% CI, 79%–96%), we applied it to administrative data from the Healthcare Cost and Utilization Project on all hospital admissions across 11 states. Age- and sex-standardized RCVS incidence was calculated using census data. Descriptive statistics were used to analyze associated diagnoses.
Results
Across 5,067,250 hospital admissions in our administrative data, we identified 222 patients with a discharge diagnosis of RCVS in 2016. The estimated annual age- and sex-standardized incidence of RCVS hospitalization was 2.7 (95% CI, 2.4–3.1) cases per million adults. Many patients had concomitant neurologic diagnoses, including subarachnoid hemorrhage (37%), ischemic stroke (16%), and intracerebral hemorrhage (10%). In the 90 days before the index admission, 97 patients had an emergency department (ED) visit and 34 patients a hospital admission, most commonly for neurologic, psychiatric, and pregnancy-related diagnoses. Following discharge from the RCVS hospital admission, 58 patients had an ED visit and 31 had a hospital admission, most commonly for neurologic diagnoses.
Conclusions
Using population-wide data, we estimated the age- and sex-standardized incidence of hospitalization for RCVS in US adults as approximately 3 per million per year.
The term reversible cerebral vasoconstriction syndrome (RCVS) has been proposed to serve as the unifying diagnosis for several previously disparate but related conditions including Call-Fleming syndrome,1 migrainous vasospasm, benign angiopathy of the CNS, postpartum angiopathy, and drug-induced arteritis.2 The diagnostic criteria for RCVS include angiographically confirmed, multifocal, segmental cerebral artery vasoconstriction, no evidence of cerebral aneurysm, a normal or near-normal CSF profile, severe acute headaches with or without additional neurologic signs, and reversibility of angiographic findings within 12 weeks.2,3
To date, more than 500 cases of RCVS have been reported in the form of case studies and case series. These have elucidated important information including precipitating factors, presenting signs and symptoms, imaging characteristics, and outcomes of RCVS.4-15 Reported risk factors for the development of RCVS include the postpartum period, female sex, migraine, and exposure to vasoactive substances including cannabis, selective serotonin reuptake inhibitors, and nasal decongestants.4,5,8 Prior reports are largely from tertiary care referral centers, and there are no population-based data on the incidence, characteristics, and outcomes of RCVS. We therefore used administrative claims data from 11 geographically dispersed US states to estimate the age- and sex-standardized incidence rates of hospitalization for RCVS and examine its associated manifestations and health care utilization.
Methods
Design and Patient Population
We performed a retrospective cohort study using administrative claims data on all emergency department (ED) visits and hospital admissions involving adults age 18 years and over at nonfederal acute care hospitals in Arkansas, Florida, Georgia, Iowa, Massachusetts, Maryland, Nebraska, New York, Utah, Vermont, and Wisconsin from January through December 2016. Trained analysts used standardized methods to collect data regarding discharges and reported these to state health agencies for regulatory purposes. After quality checking, these data were provided in a deidentified format to the Agency for Healthcare Research and Quality for its Healthcare Cost and Utilization Project.16 A deidentified personal linkage number assigned to all patients allows them to be longitudinally followed across ED encounters and hospital admissions over multiple years.17 These 11 states were chosen because they are the only states that provide longitudinal data to HCUP allowing tracking of patients across multiple ED visits and hospital admissions. In performing this study, we adhered to the Report of Studies Conducted Using Observational Routinely Collected Health Data guidelines for claims-based analytical studies.18 H.K. was responsible for dataset acquisition and data stewardship. The data used in this study are subject to a data agreement and thus cannot be shared directly by the authors, but the source data are publicly available via application to the Healthcare Cost and Utilization Project.
Standard Protocol Approvals, Registrations, and Patient Consents
The institutional review board at Weill Cornell Medicine approved this study and waived the requirement for informed consent given the de-identified nature of the study.
Measurements
Our disease of interest was RCVS, defined using ICD-10 discharge diagnosis code I67.841. To assess the validity of this code for identifying cases of RCVS, before we performed our analysis of deidentified administrative data, we performed a separate, additional analysis involving medical record review at 2 medical centers. We identified 12 hospital admissions at New York–Presbyterian/Weill Cornell Medical Center with a discharge diagnosis code I67.841, as well as a sample of 28 hospital admissions with other cerebrovascular diagnoses that were randomly drawn from among all patients with ischemic or hemorrhagic stroke registered in the Cornell Acute Stroke Academic Registry during calendar years 2011–2017. The medical records from these 40 hospital admissions were reviewed by a single investigator, board certified in vascular neurology, who adjudicated the presence/absence of RCVS while blinded to the hospital discharge diagnosis code. For patients adjudicated to have RCVS, the RCVS2 score was calculated. The RCVS2 score ranges from −2 to 10 and takes into account presence of thunderclap headache, carotid artery involvement, vasoconstrictive triggers, sex, and subarachnoid hemorrhage.19 An identical validation study was performed at Memorial Hospital Central, a nonacademic hospital affiliated with the University of Colorado Health system, involving blinded review of 39 hospital admissions, 13 of which had a discharge diagnosis code I67.841, and a random sample of 26 hospital admissions that had other cerebrovascular diagnoses. Memorial Hospital Central is a community-based hospital with stroke volumes typical of a relatively large community hospital stroke program.
After performing the above validity assessments on diagnosis code I67.841, we used it to identify cases of RCVS among adults in the administrative data from 11 states. The first hospital admission with a discharge diagnosis of I67.841 was considered the index hospital admission (figure). We used concomitant ICD-10 diagnoses to examine presenting manifestations at the time of the index RCVS hospital admission. To understand health care utilization patterns of patients with RCVS, we examined ICD-10 diagnoses during ED visits and hospital admissions before and after the index RCVS hospital admission. We included all ED visits and hospital admissions from January 1, 2016, through December 31, 2016 (figure).
Figure. Schematic Illustration of Ascertainment of Index Reversible Cerebral Vasoconstriction Syndrome (RCVS) Hospital Admission and Preceding, Concomitant, and Subsequent Diagnoses.
ED = emergency department; ICD-10 = International Classification of Diseases–10.
Statistical Analysis
We used descriptive statistics with means and SDs, medians and interquartile ranges (IQRs), or proportions and exact confidence intervals (CIs). We used direct standardization and census data from the 11 states in this analysis to estimate RCVS incidence age- and sex-standardized to the adult population (18 years and over). To estimate the effect of missed RCVS cases, we performed a sensitivity analysis in which we divided our primary incidence estimate by the lower bound of the 95% CI of our calculated sensitivity of the RCVS diagnosis code. All analyses were performed by J.M.-B. and H.K. using Stata/MP, version 14 (StataCorp).
Data Availability
The data used in this study are government data by a data use agreement and cannot be shared directly by the authors. The data are available by request to the Agency for Healthcare Research and Quality. The analysis code will be shared with investigators upon reasonable request to the corresponding author.
Results
In the validation assessments described above, the sensitivity of diagnosis code I67.841 was 100% (95% CI, 66%–100%) and the specificity was 90% (95% CI, 74%–98%) at Weill Cornell Medical Center, and the sensitivity was 100% (95% CI, 69%–100%) and the specificity was 90% (95% CI, 73%–98%) at Memorial Hospital Central. After pooling the data from both centers, the combined sensitivity was 100% (95% CI, 82%–100%) and the combined specificity was 90% (95% CI, 79%–96%). Among patients adjudicated to have RCVS, the median RCVS2 score19 was 6 at Weill Cornell Medical Center and 7.5 at Memorial Hospital Central, suggesting that diagnosis code I67.841 generally identifies true cases of RCVS, given that an RCVS2 score of ≥5 has been reported to be 90% sensitive and 99% specific for gold standard ascertained cases of RCVS.
Across the 11 states included in this analysis, there were 222 patients with a hospital discharge diagnosis of RCVS during 2016. The mean age at the time of diagnosis was 47 (SD 14) years and 172 (78%) patients were women (table 1). The estimated overall age- and sex-standardized incidence of RCVS cases leading to hospitalization in the adult population was calculated as 2.7 (95% CI, 2.4–3.1) cases per million per year. The annual age-standardized incidence in women was calculated as 4.1 (95% CI, 3.5–4.8) cases per million vs 1.2 (95% CI, 0.9–1.6) cases per million in men. Assuming that the RCVS diagnosis code is only 82% sensitive, based on the lower bound of the 95% CI in our validation assessment above, the estimated incidence of RCVS would be 3.3 cases per million per year. In a post hoc sensitivity analysis, after excluding data from Massachusetts, which appeared to have a higher incidence of RCVS, the incidence of RCVS in the other 10 states was 2.1 (95% CI, 1.9–2.6) cases per million per year.
Table 1.
Baseline Characteristics and Demographics of Patients Diagnosed With Reversible Cerebral Vasoconstriction Syndrome (n = 222)

During the index hospital admission for RCVS, many patients had concomitant neurologic diagnoses. Eighty-two patients (36.9%) had a diagnosis of subarachnoid hemorrhage (SAH), 36 patients (16.2%) had a diagnosis of ischemic stroke, 23 patients (10.4%) had a diagnosis of ICH, 17 patients (7.7%) had a diagnosis of posterior reversible encephalopathy syndrome (PRES), and 22 patients (9.9%) had a diagnosis of seizures (table 2). The median hospital length of stay was 4 (IQR, 3–10) days, and 17 (7.7%) patients required mechanical ventilation. Most patients (147 [66.2%]) returned home upon discharge, with 23 requiring home health care. The majority of the other patients were transferred to a rehabilitation facility or nursing home (42 [18.9%]).
Table 2.
Diagnoses Associated With Reversible Cerebral Vasoconstriction Syndrome (RCVS), Listed by Number of Patients With at Least 1 Such Diagnosis

In the 90 days prior to the index RCVS diagnosis, 86 patients (38.7%) presented to the ED at least once (table 2). Fifty-five (24.7%) patients had at least 1 ED visit for a neurologic diagnosis, 42 of whom (19%) presented for headache (table 2). These 86 patients had 149 total ED visits preceding their index RCVS diagnosis (table 3). Fifty patients (22.5%) had at least 1 hospital admission within the 90 days preceding the index hospital admission for RCVS (table 2). Sixteen patients (7.2%) were hospitalized at least once with a primary neurologic diagnosis, including epilepsy, status migrainosus, abnormal findings on CNS imaging, cerebral infarction, nontraumatic SAH, nontraumatic ICH, and PRES. Pregnancy-related diagnoses were also a common reason for hospital admission prior to RCVS diagnosis, with 18 patients (8.1%) with at least 1 hospital admission for preeclampsia or other complications related to childbirth. These 50 patients had 68 total hospital admissions preceding their index RCVS diagnosis (table 3).
Table 3.
Diagnoses Associated With Reversible Cerebral Vasoconstriction Syndrome (RCVS), Listed by Total Number of Visits for Each Diagnosis

During a mean 5.2 (±3.5) months of follow-up data after their index hospital admission for RCVS, 70 patients (31.5%) had at least 1 subsequent ED visit (table 2). Thirty-three patients (14.8%) had at least 1 ED visit for a neurologic diagnosis. These 70 patients had 131 total ED visits after their index RCVS hospitalization (table 3). There were 53 patients (23.8%) who had at least 1 hospital admission after the index RCVS hospitalization (table 2). Thirty-one patients (14.0%) had at least 1 hospital admission with a neurologic primary discharge diagnosis, most commonly migraine, cerebral infarction or its sequelae, ICH or its sequelae, or SAH or its sequelae. There were few subsequent ED visits or hospital admissions for non-neurologic conditions after discharge from the index RCVS hospital admission. Approximately half of the subsequent hospital admissions and more than 80% of the subsequent ED visits involved patients who had been discharged home from their index RCVS hospital admission and not discharged to rehabilitation or nursing facilities.
Discussion
Using administrative claims data from a large, heterogeneous population, we estimated that the incidence of RCVS cases leading to hospitalization is approximately 3 per million adults per year. When analyzed separately based on sex, the incidence in women is approximately 4 times higher than in men. Hospital admissions for RCVS were frequently preceded by ED visits for headache, and although most patients with RCVS were able to return home, there was a substantial rate of neurovascular complications, particularly SAH and ICH. After the index RCVS hospital admission, there was a substantial rate of utilization of emergency and hospital-based care.
In prior case series, the incidence of RCVS has been reported among various subpopulations, such as 0.25% of patients presenting to a stroke unit and emergency headache clinic5 and 8.8% of patients presenting with thunderclap headache,12 but these prior studies were unable to define the incidence of RCVS in the general population. Preliminary findings from an analysis of administrative claims data involving a sampling methodology suggested an overall incidence of RCVS of approximately 4.5 per million adults per year, but final results are not yet published.20 In this context, our study provides novel findings that the population-level incidence of hospitalization for RCVS is approximately 3 per million adults per year.
Although RCVS is benign and self-limited in approximately 90% of cases,8,11,14 clinical worsening and poor functional outcomes can occur and are most commonly associated with infarction.11 Given the risk of serious complications including hemorrhage (ICH and SAH), seizure, and ischemia during the first 3 weeks after diagnosis, most patients diagnosed with RCVS are hospitalized for close monitoring.4,5,8,11,21 Consistent with prior studies and case series of patients with RCVS, our population-based analysis found that patients with RCVS were typically women in their 40s,22 several were peripartum,23,24 and many presented with headache prior to diagnosis and continued to return with headache after discharge.4,14 Similar to past reports, the majority of patients were discharged home after their hospital admission for RCVS,14,25 but many patients experienced other serious neurologic and cerebrovascular complications of RCVS during and after their initial hospital admission.5,11
Our study should be considered in light of its limitations. First, we used administrative claims data to establish diagnoses, which could potentially result in misclassification of diagnoses. Our validity assessment of the RCVS diagnosis code indicated that it should be a valid proxy for RCVS diagnoses. However, the validation was performed by a single investigator and involved a limited sample of patients from 2 hospitals with findings that may not be representative of small hospitals. Even if the diagnosis code validly captures cases that were diagnosed, it does not mean that there were not many undiagnosed or misdiagnosed cases as RCVS is a clinical diagnosis with potential mimics. The potential for misclassification may have been especially significant outside of tertiary care centers, which regularly receive referrals for RCVS and therefore have greater experience with its diagnosis. We lacked data on whether hospitals were tertiary care centers or had access to relevant specialists such as neurologists. Second, administrative claims data do not provide granular clinical information related to our diagnoses of interest, such as details of neuroimaging or laboratory tests. Therefore, we may have missed cases of concomitant brain infarcts or hemorrhages. Third, the information on claims related to RCVS cases both before and after diagnosis may be skewed given that it involved only patients diagnosed with RCVS and not those RCVS cases that went undiagnosed. Fourth, we lacked data from the entire United States, particularly from Western states. Therefore, a selection bias from the inclusion of these particular states cannot be excluded. Fifth, we lacked long-term data on preceding and follow-up events.
In a large, heterogeneous sample of patients in the United States, we found that the age- and sex-standardized incidence of RCVS leading to hospitalization in US adults is approximately 3 per million per year. We found a substantial rate of neurovascular complications in patients with RCVS, emphasizing the importance of timely diagnosis of RCVS.
Acknowledgment
The authors thank Kelsey Lansdale for copyediting and manuscript preparation.
Glossary
- CI
confidence interval
- ED
emergency department
- ICD-10
International Classification of Diseases–10
- IQR
interquartile range
- PRES
posterior reversible encephalopathy syndrome
- RCVS
reversible cerebral vasoconstriction syndrome
- SAH
subarachnoid hemorrhage
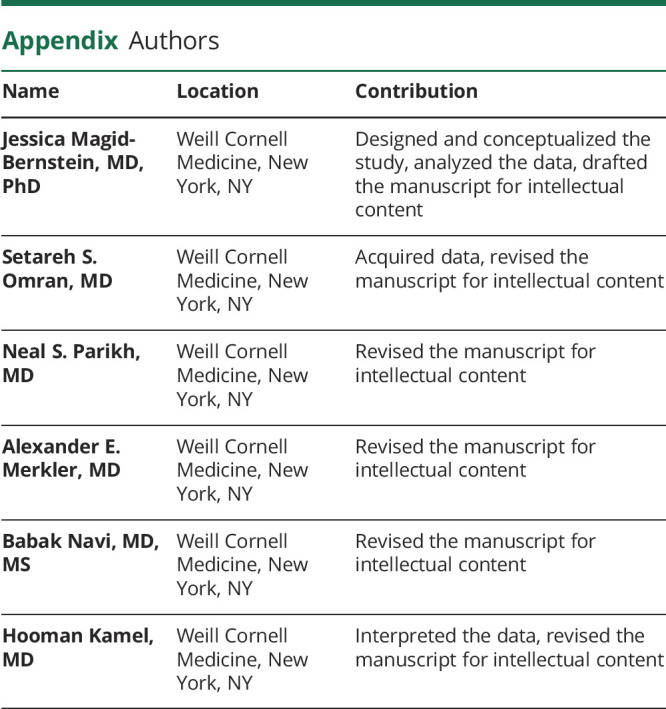
Appendix. Authors
Footnotes
CME Course: NPub.org/cmelist
Podcast: NPub.org/nq4cfl
Study Funding
N. Parikh was supported by the New York State Empire Clinical Research Investigator Program and the Leon Levy Foundation in Neuroscience. A. Merkler is supported by the American Heart Association grant 18CDA34110419 and the Leon Levy Foundation in Neuroscience. B. Navi is supported by the NIH (K23NS091395) and the Florence Gould Endowment for Discovery in Stroke.
Disclosure
A. Merkler has received personal fees for medicolegal consulting on neurologic disorders. B. Navi serves as a member of the data and safety monitoring board for the PCORI-funded TRAVERSE trial and has received personal fees for medicolegal consulting on stroke. H. Kamel serves as co-PI for the NIH-funded ARCADIA trial, which receives in-kind study drug from the BMS-Pfizer Alliance and in-kind study assays from Roche Diagnostics, serves as Deputy Editor for JAMA Neurology, serves as a steering committee member of Medtronic's Stroke AF trial (uncompensated), and serves on an endpoint adjudication committee for a trial of empagliflozin for Boehringer-Ingelheim and has served on an advisory board for Roivant Sciences related to Factor XI inhibition. Go to Neurology.org/N for full disclosures.
References
- 1.Call GK, Fleming MC, Sealfon S, Levine H, Kistler JP, Fisher CM. Reversible cerebral segmental vasoconstriction. Stroke. 1988;19(10):1159-1170. [DOI] [PubMed] [Google Scholar]
- 2.Calabrese LH, Dodick DW, Schwedt TJ, Singhal AB. Narrative review: reversible cerebral vasoconstriction syndromes. Ann Intern Med. 2007;146(1):34-44. [DOI] [PubMed] [Google Scholar]
- 3.Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629-808. [DOI] [PubMed] [Google Scholar]
- 4.Ducros A, Boukobza M, Porcher R, Sarov M, Valade D, Bousser MG. The clinical and radiological spectrum of reversible cerebral vasoconstriction syndrome: a prospective series of 67 patients. Brain. 2007;130(pt 12):3091-3101. [DOI] [PubMed] [Google Scholar]
- 5.Ducros A, Fiedler U, Porcher R, Boukobza M, Stapf C, Bousser MG. Hemorrhagic manifestations of reversible cerebral vasoconstriction syndrome: frequency, features, and risk factors. Stroke. 2010;41(11):2505-2511. [DOI] [PubMed] [Google Scholar]
- 6.Cheng YC, Kuo KH, Lai TH. A common cause of sudden and thunderclap headaches: reversible cerebral vasoconstriction syndrome. J Headache Pain. 2014;15(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen SP, Fuh JL, Lirng JF, Chang FC, Wang SJ. Recurrent primary thunderclap headache and benign CNS angiopathy: spectra of the same disorder? Neurology. 2006;67(12):2164-2169. [DOI] [PubMed] [Google Scholar]
- 8.Singhal AB, Hajj-Ali RA, Topcuoglu MA, et al. Reversible cerebral vasoconstriction syndromes: analysis of 139 cases. Arch Neurol. 2011;68(8):1005-1012. [DOI] [PubMed] [Google Scholar]
- 9.Robert T, Kawkabani Marchini A, Oumarou G, Uské A. Reversible cerebral vasoconstriction syndrome identification of prognostic factors. Clin Neurol Neurosurg. 2013;115(11):2351-2357. [DOI] [PubMed] [Google Scholar]
- 10.Sheikh HU, Mathew PG. Reversible cerebral vasoconstriction syndrome: updates and new perspectives. Curr Pain Headache Rep. 2014;18(5):414. [DOI] [PubMed] [Google Scholar]
- 11.Katz BS, Fugate JE, Ameriso SF, et al. Clinical worsening in reversible cerebral vasoconstriction syndrome. JAMA Neurol. 2014;71(1):68-73. [DOI] [PubMed] [Google Scholar]
- 12.Grooters GS, Sluzewski M, Tijssen CC. How often is thunderclap headache caused by the reversible cerebral vasoconstriction syndrome? Headache. 2014;54(4):732-735. [DOI] [PubMed] [Google Scholar]
- 13.Chen SP, Fuh JL, Lirng JF, Wang YF, Want SJ. Recurrence of reversible cerebral vasoconstriction syndrome: a long-term follow-up study. Neurology. 2015;84(15):1552-1558. [DOI] [PubMed] [Google Scholar]
- 14.John S, Singhal AB, Calabrese L, et al. Long-term outcomes after reversible cerebral vasoconstriction syndrome. Cephalalgia. 2016;36(2):387-394. [DOI] [PubMed] [Google Scholar]
- 15.Lee MJ, Choi HA, Choi H, Chung CS. Serial testing of the ICHD-3 beta diagnostic criteria for probable reversible cerebral vasoconstriction syndrome: a prospective validation study. Cephalalgia. 2018;38(10):1665-1671. [DOI] [PubMed] [Google Scholar]
- 16.Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality. Accessed February 13, 2020. https://www.hcup-us.ahrq.gov. [PubMed]
- 17.Barrett M, Steiner C, Andrews R, Kassed C, Nagamine M. Methodological Issues When Studying Readmissions and Revisits Using Hospital Administrative Data. HCUP Methods Series Report 2011-01; online March 9, 2011. Agency for Healthcare Research and Quality; 2011. [Google Scholar]
- 18.Benchimol EI, Smeeth L, Guttmann A, et al. ; RECORD Working Committee. The Reporting of Studies Conducted Using Observational Routinely Collected Health Data (RECORD) statement. PLOS Med. 2015;12(10):e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rocha EA, Topcuoglu MA, Silva GS, Singhal AB. RCVS2 score and diagnostic approach for reversible cerebral vasoconstriction syndrome. Neurology. 2019;92(7):e639-e647. [DOI] [PubMed] [Google Scholar]
- 20.Patel SD, Otite FO, Lima J, Khandelwal P, Ollenschleger M. Abstract WP207: current incidence, epidemiological and clinical characteristics of reversible cerebral vasoconstriction in the United States. Stroke. 2020;51:AWP207. [Google Scholar]
- 21.Ducros A, Wolff V. The typical thunderclap headache of reversible cerebral vasoconstriction syndrome and its various triggers. Headache. 2016;56(4):657-673. [DOI] [PubMed] [Google Scholar]
- 22.Ducros A. Reversible cerebral vasoconstriction syndrome. Lancet Neurol. 2012;11(10):906-917. [DOI] [PubMed] [Google Scholar]
- 23.Skeik N, Porten BR, Kadkhodayan Y, McDonald W, Lahham F. Postpartum reversible cerebral vasoconstriction syndrome: review and analysis of the current data. Vasc Med. 2015;20(3):256-265. [DOI] [PubMed] [Google Scholar]
- 24.Miller EC, Yaghi S, Boehme AK, Willey JZ, Elkind MSV, Marshall RS. Mechanisms and outcomes of stroke during pregnancy and the postpartum period: a cross-sectional study. Neurol Clin Pract. 2016;6(1):29-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller TR, Shivashankar R, Mossa-Basha M, Gandhi D. Reversible cerebral vasoconstriction syndrome, part 1: epidemiology, pathogenesis, and clinical course. Am J Neuroradiol. 2015;36(8):1392-1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this study are government data by a data use agreement and cannot be shared directly by the authors. The data are available by request to the Agency for Healthcare Research and Quality. The analysis code will be shared with investigators upon reasonable request to the corresponding author.



