Abstract
Immunoglobulin G4 (IgG4)–related pericarditis, an immune-mediated fibro-inflammatory condition, is a rare yet life-threatening disease presenting with constrictive pericarditis. We describe a case of IgG4-related pericarditis presenting with epicardial nodules successfully treated with corticosteroids. This case highlights the clinical significance of assessing IgG4-related pericarditis in the diagnostic workup of pericardial masses. (Level of Difficulty: Advanced.)
Key Words: cardiac magnetic resonance, computed tomography, immunoglobulin G4–related disease, immunoglobulin G4–related pericarditis, pericardial effusion
Abbreviations and Acronyms: CCTA, coronary computed tomography angiography; CMR, cardiac magnetic resonance; CP, constrictive pericarditis; FDG PET/CT, fluorodeoxyglucose positron-emission tomography/computed tomography; IgG4, immunoglobulin G4; IgG4-RD, immunoglobulin G4–related disease; PE, pericardial effusion
Graphical abstract
Immunoglobulin G4 (IgG4)–related pericarditis, an immune-mediated fibro-inflammatory condition, is a rare yet life-threatening disease presenting…
History of Presentation
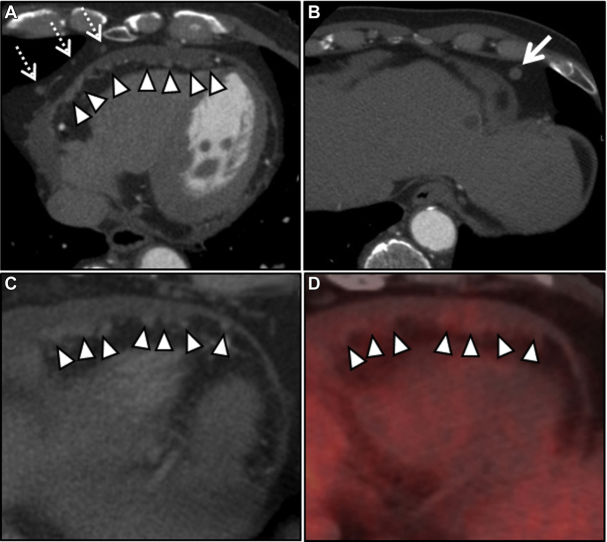
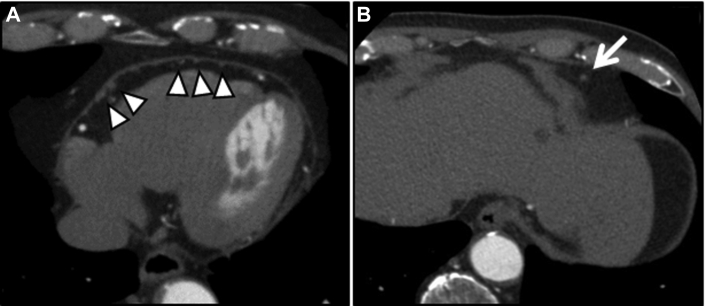
A 75-year-old man with a 20-year history of diabetes underwent percutaneous coronary intervention for angina. Cardiac enzyme levels were elevated, and minor electrocardiographic abnormalities were observed although the patient was asymptomatic during follow-up. We suspected myocardial ischemia and performed coronary computed tomography angiography (CCTA) because the patient was unable to exercise. His vital signs were: blood pressure, 130/80 mm Hg; heart rate, 66 beats/min; respiratory rate, 12 breaths/min; and temperature, 36.0°C. Physical examination results were unremarkable. CCTA revealed no significant coronary artery stenosis, but pericardial masses were detected incidentally. We also noted multiple visceral pericardial nodules adjacent to epicardial fat, concurrent with localized pericardial thickening and pericardial and paraphrenic lymph node enlargement (Figures 1A and 1B).
Learning Objectives
-
•
To understand early clinical manifestations of IgG4-related pericarditis.
-
•
To understand the imaging findings in IgG4-related pericarditis.
-
•
To review the causes of pericardial masses.
Figure 1.
Pericardial Masses
(A, B) Coronary computed tomography angiography reveals multiple epicardial nodules (A, arrowheads), a localized thickened pericardium, enlarged pericardial lymph nodes (A, dashed arrows), and an enlarged paraphrenic lymph node (B, arrow). (C, D) Fluorodeoxyglucose (FDG) positron-emission tomography/computed tomography reveals mildly increased FDG uptake in epicardial nodules, suggesting increased metabolic activity (arrowheads).
Medical History
The patient had a history of diabetes mellitus, dementia, and angina.
Differential Diagnosis
Differential diagnoses based on cardiac magnetic resonance (CMR) findings include metastatic neoplasm (lung or breast carcinoma and lymphoma), primary neoplasm (malignant lymphoma and mesothelioma), tuberculous pericarditis, or cardiac sarcoidosis.
Investigations
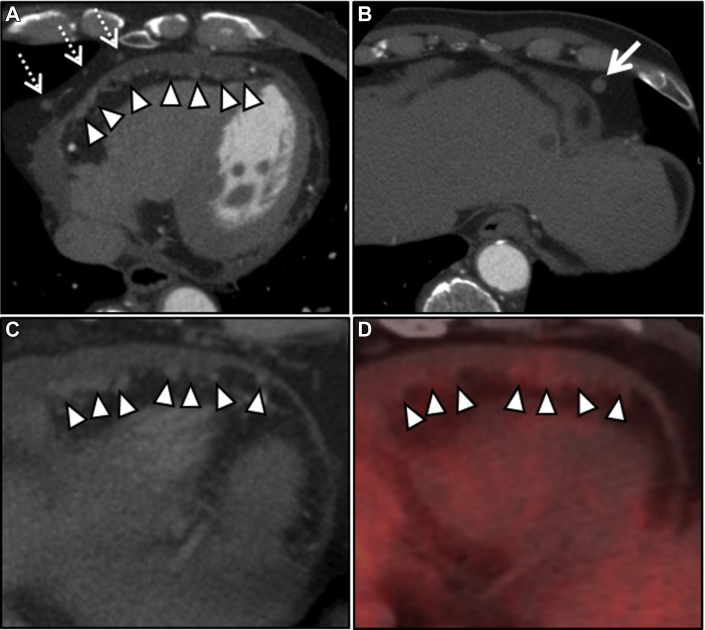
Fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) revealed weak metabolic activity in the same nodular lesions, suggesting malignancy or infection (e.g., tuberculosis) (Figures 1C and 1D). CMR screening revealed epicardial thickening with inhomogeneous gadolinium enhancement and pericardial effusion (PE) (Figure 2).
Figure 2.
Cardiac Magnetic Resonance Image
Axial cardiac magnetic resonance with late gadolinium enhancement revealing delayed enhancement of the visceral (arrowheads) and parietal pericardium (arrow) and pericardial effusion.
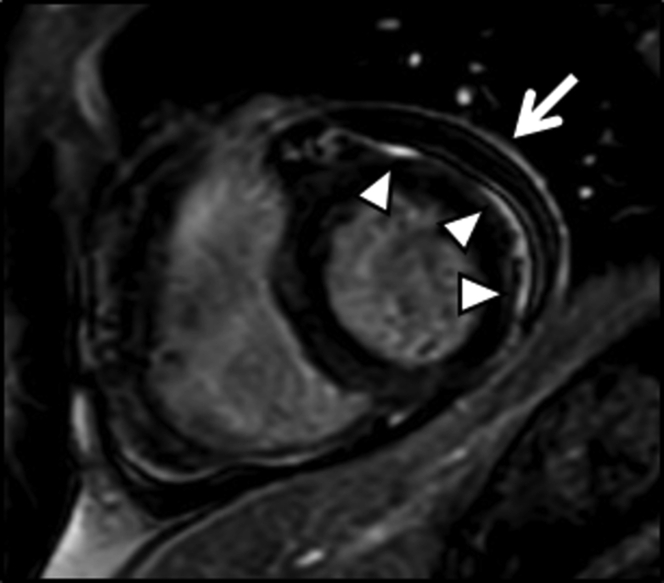
Results of cardiac catheterization and hemodynamic study were unremarkable, with no evidence of constrictive physiology. Laboratory tests revealed elevated serum immunoglobulin G4 (IgG4) (212 mg/dl, normal range: 4 to 108 mg/dl), high-sensitivity cardiac troponin T (0.058 ng/ml, normal range: 0 to 0.010 ng/ml), IgE (69,303 IU/ml, normal range: 0 to 170 IU/ml), and soluble interleukin-2 receptor (1,574 U/ml, normal range: 122 to 496 U/ml) levels. An open surgical biopsy was performed for diagnosis. The pericardium was diffusely reddish. The resected thickened pericardium was stiff (Figure 3A). PE analysis revealed lymphocyte-predominant exudates and elevated IgG4 levels (395 mg/dl). The adenosine deaminase activity in PE was 45 U/l, suggesting tuberculous pericarditis; polymerase chain reaction test for Mycobacterium tuberculosis was negative. PE cytology as well as bacterial and fungal cultures were unremarkable. Pathologic examination of the specimen revealed fibrous thickening, patchy lymphoplasmacytic infiltration with eosinophils, and hemorrhage (Figure 3B). Immunostaining revealed increased numbers of IgG4-positive plasma cells (mean 29/high-power field counted from 3 active spots) and an IgG4/IgG-positive plasma cell ratio of 51% (Figure 3C). These findings met the comprehensive criteria for IgG4-related disease (IgG4-RD) following exclusion of IgG4-RD mimics (malignancies, infectious diseases, autoimmune diseases, Churg–Strauss syndrome, or Castleman disease). Moreover, fluorodeoxyglucose positron-emission tomography/computed tomography (FDG PET/CT) ruled out involvement of other organs in IgG4-RD.
Figure 3.
Pericardial Biopsy
(A) Resected pericardium. (B) Photomicrograph with hematoxylin and eosin stain (Bar: 200 μm). (C) Photomicrograph with immunostaining against immunoglobulin G4 (Bar: 400 μm).
Management
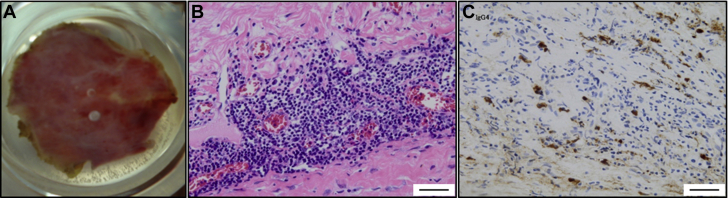
A subsequent high-dose corticosteroid treatment (prednisolone 30 mg daily) exhibited a dramatic beneficial response on the pericardial lesion (Figure 4). CCTA following a 6-month course of treatment showed significant reduction in the number and size of epicardial nodules and the enlarged paraphrenic lymph node. Moreover, the enlarged pericardial lymph nodes and PE disappeared. The prednisolone dose was gradually tapered to 2.5 mg daily.
Figure 4.
Therapeutic Effect
(A, B) Coronary computed tomography angiography following a 6 months course of corticosteroid treatment reveals a marked reduction in the number and size of epicardial nodules (arrowheads) and the enlarged paraphrenic lymph node (arrow). Note the disappearance of enlarged pericardial lymph nodes and pericardial effusion.
Discussion
IgG4-RD is a systemic fibro-inflammatory disorder characterized by an elevated serum IgG4 level and histologic findings of IgG4-positive lymphoplasmacytic infiltration (1). Although pericardial involvement is rare, IgG4-related pericarditis manifests as chronic pericarditis associated with PE. Etiologies of PE are diverse and poorly understood despite exhaustive examination. Therefore, IgG4-related pericarditis may remain undiagnosed or misdiagnosed as idiopathic pericarditis, and patients might receive inappropriate treatment. If left untreated, serious complications such as cardiac tamponade and constrictive pericarditis (CP) may occur at an advanced stage (2,3). However, early diagnosis is extremely challenging because of the lack of specific signs or symptoms in early disease stages. Herein, we describe a patient with IgG4-related pericarditis presenting with epicardial nodules.
This case may offer several valuable clinical lessons. IgG4-related pericarditis can present as epicardial nodules and not CP, which is recognized as its more typical presentation (4). Although most patients present with symptoms and signs of right-sided heart failure, our patient exhibited pericardial masses; this has been reported for the first time per our knowledge.
The pericardial biopsy was useful for the definitive diagnosis. Histologic analysis of the pericardium is available in a limited number of cases (2, 3, 4, 5). IgG4 immunoprofile showed that cases with CP tended to show more IgG4-positive cells and higher IgG4/IgG ratios than our case. Because the number of IgG4-positive cells can decrease as fibrosis formation progresses to an advanced stage, differences in immunoprofile might not reflect accurate IgG4-pericarditis activity.
Generally, patients with IgG4-RD respond well to corticosteroid treatment. However, a corticosteroid trial for diagnostic purposes should be strictly avoided because it may mask or exacerbate the clinical picture of IgG4-RD mimics, leading to delayed or incorrect diagnosis (6). The pericardial biopsy enabled us in timely diagnosis of IgG4-related pericarditis, resulting in complete recovery with corticosteroid treatment. The pericardial biopsy suggested that the parietal pericardial lesion initiated concurrently with epicardial nodule formation. Although the precise mode of action remains unknown, epicardial nodules might be the first step in the pathogenesis of IgG4-related pericarditis. Further reports should be assessed to verify the early diagnostic value and prove the validity of this manifestation.
CMR was also helpful for the diagnosis of early-stage IgG4-related pericarditis. CMR enables anatomical and dynamic evaluation of the pericardium, providing detailed information on PE location and characterization and pericardial thickening (7). Thus, CMR screening should be considered for all patients with pericardial masses because early-stage IgG4-related pericarditis may be undiagnosed.
Patients with IgG4-related pericarditis respond well to corticosteroids (2,3). However, high relapse rates during and after corticosteroid tapering are major concerns. Moreover, there is a risk of serious adverse effects of prolonged treatment, such as diabetes, Cushing syndrome, and infections. Rituximab can be used as maintenance therapy following steroid tapering or as a potential promising therapy in high-risk patients with steroid intolerance (8). Other immunomodulators such as cyclophosphamide are also effective in combination with steroids (9). Conversely, nonsteroidal anti-inflammatory drugs plus colchicine is the first-line therapy for chronic pericarditis of idiopathic or viral origin (10). Whether these drugs show similar beneficial effects on IgG4-related pericarditis remains unclear; however, these were not useful in IgG4-related pericarditis according to a case report (5). The future challenge is to establish site-specific diagnostic and therapeutic methods for IgG4-related pericarditis.
Follow-Up
The patient remains symptom-free during the follow-up examinations.
Conclusions
Herein, we describe a case of biopsy-proven early-stage IgG4-related pericarditis successfully treated with corticosteroids. IgG4-related pericarditis can present as epicardial nodules; CMR is helpful for the diagnosis of this clinical entity. Although IgG4-related pericarditis is rare, it can cause a potentially lethal cardiac disease which can be cured if treated properly at an early stage. Tissue diagnosis is essential for early diagnostic testing and appropriate treatment. Therefore, all clinicians should recognize the clinical significance of IgG4-RD in the diagnostic workup of pericardial mass and should not hesitate to perform a pericardial biopsy.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
References
- 1.Kamisawa T., Zen Y., Pillai S., Stone J.H. IgG4-related disease. Lancet. 2015;385:1460–1471. doi: 10.1016/S0140-6736(14)60720-0. [DOI] [PubMed] [Google Scholar]
- 2.Morita T., Izawa A., Hamano H. Significant pericardial involvement of immunoglobulin G4-related disease. Ann Thorac Surg. 2014;98:e47–e49. doi: 10.1016/j.athoracsur.2014.04.069. [DOI] [PubMed] [Google Scholar]
- 3.Sekiguchi H., Horie R., Suri R.M., Yi E.S., Ryu J.H. Constrictive pericarditis caused by immunoglobulin G4-related disease. Circ Heart Fail. 2012;5:e30–e31. doi: 10.1161/CIRCHEARTFAILURE.111.966408. [DOI] [PubMed] [Google Scholar]
- 4.Ibe T., Nakamura T., Taniguchi Y., Momomura S. IgG4-related effusive constrictive pericarditis. Eur Heart J Cardiovasc Imaging. 2016;17:707. doi: 10.1093/ehjci/jew056. [DOI] [PubMed] [Google Scholar]
- 5.Yassi U., Iqbal F., Stevenson H.L. IgG4-related sclerosing pericarditis in a young man with recurrent chest pain. Ann Thorac Surg. 2019 Oct;108:e261–e263. doi: 10.1016/j.athoracsur.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 6.Umehara H., Okazaki K., Masaki Y. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012;22:21–30. doi: 10.1007/s10165-011-0571-z. [DOI] [PubMed] [Google Scholar]
- 7.Bogaert J., Francone M. Cardiovascular magnetic resonance in pericardial diseases. J Cardiovasc Magn Reson. 2009;11:14. doi: 10.1186/1532-429X-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perugino C.A., Wallace Z.S., Meyersohn N., Oliveira G., Stone J.R., Stone J.H. Large vessel involvement by IgG4-related disease. Medicine (Baltimore) 2016;95:e3344. doi: 10.1097/MD.0000000000003344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yunyun F., Yu C., Panpan Z. Efficacy of cyclophosphamide treatment for immunoglobulin G4-related disease with addition of glucocorticoids. Sci Rep. 2017;7:6195. doi: 10.1038/s41598-017-06520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imazio M., Gaita F., LeWinter M. Evaluation and treatment of pericarditis: a systematic review. JAMA. 2015;314:1498–1506. doi: 10.1001/jama.2015.12763. [DOI] [PubMed] [Google Scholar]