Ocular flutter is a form of saccadic intrusion consisting of back to back horizontal saccades. It is considered to be a subtype of opsoclonus and can be associated with a variety of disorders including paraneoplastic syndromes, encephalitis, serotonin syndrome and various infections [1]. We present a case of alcohol withdrawal seizures followed by ocular flutter and tremor which persisted for three years. To the best of our knowledge this has not been previously reported.
Case
A 32 year old right handed male with a history of schizophrenia, alcoholism, poly-substance abuse and seizure disorder was brought to the emergency department (ED) after being found down. The patient regained consciousness and according to witnesses he was responsive and interactive, talking and walking till four days after admission when he began having generalized tonic colonic seizures attributed to alcohol withdrawal requiring life support and sedation. Ocular flutter and coarse tremor in bilateral upper extremities was noted while in intensive care. His hospital course was complicated by respiratory failure, pneumonia and sepsis with elevated procalcitonin levels. He gradually improved. Encephalopathy improved. He had a residual postural tremor at time of discharge while the ocular flutter with associated oscillopsia remained unchanged. MRI brain showed cerebral and cerebellar atrophy. EEG was performed and showed diffuse background slowing consistent with a diffuse encephalopathic state. Episodes of irregular tremor were not associated with evidence of seizure.
GD1a Ab (antibodies) were modestly but not pathologically elevated, otherwise ganglioside Ab's including GQ1b Ab were normal. CSF did not show cytoalbuminological dissociation. Paraneoplastic panel was negative. Chest CT was negative for malignancy. Additional tests including Liver function test, heavy metal panel, Vitamin B12 and folate levels, Vitamin D level, retinol, neuron specific enolase, Thyroperoxidase Ab, transglutaminase Ab, Gliadin IgA and IgG, metanephrine, normetanephrine, pyridoxal phosphate and Vitamin E were all within normal limits. HIV was negative. CSF studies were negative. Urine copper was reduced, VMA was normal. See video for ocular flutter. As the underlying cause for the ocular flutter was unknown, no treatment was given.
Five months following discharge, while residing at a sober living facility, he continued to have ocular flutter. However, it was improved and noted to be present during smooth pursuit and not at primary gaze. At that time, he had a mild postural and intention tremor. He was able to pick up objects without tremor or difficulty. At ten months following discharge the ocular flutter was less prominent and noted only twice during the exam with a slight postural tremor. Three years later with continued abstinence from alcohol, he had no signs of ocular flutter or tremor.
Discussion
This case is notable for a few things. Ocular flutter is an uncommon condition. To the best of our knowledge, ocular flutter has not been reported in association with alcohol withdrawal or alcohol withdrawal seizures. Our patient did not have signs of Wernicke's encephalopathy on MRI and was treated with thiamine upon admission. However, cerebral and cerebellar atrophy were found on MRI. Both cerebral and cerebellar atrophy have been found on MRI in schizophrenia. In addition chronic alcohol use has been shown to be associated with similar findings [2].
Ocular signs in alcoholism include slower eye movement velocity and impairment of smooth pursuit, not saccadic intrusions. The same findings are also seen with acute alcohol consumption and are attributed to deficits in executive function and sensori-motor control [3].
A single case of ocular flutter associated with elevations in GD1a Ab and viral illness was reported [4]. Our patient had modestly but not pathologically elevated GD1a Ab level. Elevated GD1a levels are associated with Guillain Barre Syndrome (GBS), Miller Fisher syndrome (MFS), Chronic Inflammatory Demyelinating Polyneuropathy, multifocal motor neuropathy, lower motor neuron disease or Amyotrophic Lateral Sclerosis. His clinical condition was incompatible with these diagnoses. In addition GQ1B Ab was normal excluding the diagnosis of MFS and GBS.
The tremor was postural and with movement, consistent with alcoholic tremor and unrelated to ocular flutter. Alcoholic tremor tends to occur with abrupt discontinuation of alcohol and is described as coarse, irregular increasing with movement. It tends to subside over days but has been reported to be present over one year of abstinence [5].
Ocular flutter acquired in adulthood tends to resolve spontaneously or with treatment of the underlying cause. Our patient showed improvement in ocular flutter coincident to improvement in tremor and continued abstinence from alcohol.
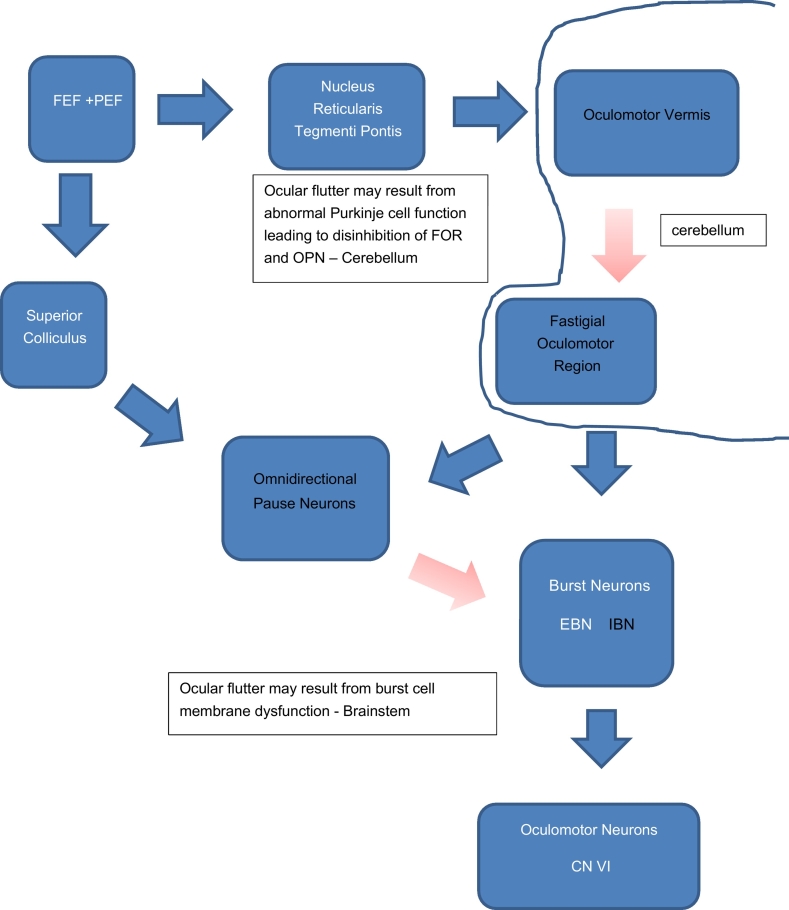
Ocular flutter is thought to be generated in either the brainstem through dysfunction of the inhibitory burst neurons which form a positive feedback loop [6] or in the cerebellum. Abnormal Purkinje cell activity in the cerebellum leads to reduced inhibition on the fastigial nucleus, which results in a loss of omnipause neuron inhibition on burst neurons within the paramedian pontine reticular formation [7]. See Fig. 1. In fact fMRI and FDG PET studies have confirmed cerebellar involvement in ocular flutter [8,9].
Fig. 1.
Diagram of saccade initiation with theories of ocular flutter generation. Legend: FEF frontal eye fields; PEF parietal eye fields; EBN excitatory burst neurons; IBN inhibitory burst neurons; FOR fastigial oculomotor region; OPN omnidirectional pause neurons.
Ocular flutter is thought to be generated either in the brainstem at the IBN through cell membrane dysfunction or in the cerebellum with Purkinje cell dysfunction leading to loss of inhibition of the FOR and OPN. The red arrows represent inhibition.
There are many causes of ocular flutter. In our patient there appeared to be an association between alcohol abuse, withdrawal and the onset and course of ocular flutter. We realize this is a rare case and although we cannot rule out other causes of the ocular flutter, none were found during an extensive work up.
The subject gave consent to be recorded for publication both in print and online.
The following is the supplementary data related to this article.
This patient displays ocular flutter, back to back, horizontal saccades, at primary gaze and during performance of smooth pursuit.
Declaration of Competing Interests
Nothing to declare.
References
- 1.Lemos J., Eggenberger E. Saccadic intrusions: review and update. Curr. Opin. Neurol. 2013;26:59–66. doi: 10.1097/WCO.0b013e32835c5e1d. [DOI] [PubMed] [Google Scholar]
- 2.Nesvag R., Frigessi A., Jonsson E.G., Agartz I. Effects of alcohol consumption and antipsychotic medication on brain morphology in schizophrenia. Schizophr. Res. 2007;90:52–61. doi: 10.1016/j.schres.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 3.Campanella S., Petit G., Maurage P., Kornreich C., Verbanic P., Noel X. Chronic alcoholism: insights from neurophysiology. Clin. Neurophysiol. 2009;39:191–207. doi: 10.1016/j.neucli.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 4.Kondoh R., Yonezawa H., Isobe C., Oikawa M., Sasaki K., Tohqi H., Kamada Y., Takahashi Y. A case of flutter-like oscillation with anti GD1a antibody after acute infection. Rinsho Shinkiqaki. 2001;41:195–197. [PubMed] [Google Scholar]
- 5.Brust J.C. Substance abuse and movement disorders. Mov. Disord. 2010;25:2010–2020. doi: 10.1002/mds.22599. [DOI] [PubMed] [Google Scholar]
- 6.Shaikh A.G., Ramat S., Optican L.M., Miura K., Leigh J., Zee D.S. Saccadic biurst cell membrane dysfunction is responsible for saccadic oscillations. J. Neuroophthalmol. 2008;4:329–336. doi: 10.1097/WNO.0b013e31818eb3a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramat S., Leigh R.J., Zee D.S., Optican L.M. What clinical disorders tell us about the neural control of saccadic eye movements. Brain. 2007;130:10–35. doi: 10.1093/brain/awl309. [DOI] [PubMed] [Google Scholar]
- 8.Helmchen C., Ranbold H., Sprenger A., Erdmann C., Binkofski F. Cerebellar activiation in opsoclonus: an FMRI study. Neurology. 2003;61:412–415. doi: 10.1212/01.wnl.0000073271.66866.51. [DOI] [PubMed] [Google Scholar]
- 9.Newey C.R., Sarwal A., Wu G. Radiological correlate of ocular flutter in a case with paraneoplastic encephalitis. J. Neuroimaging. 2013;23:251–253. doi: 10.1111/j.1552-6569.2011.00659.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This patient displays ocular flutter, back to back, horizontal saccades, at primary gaze and during performance of smooth pursuit.