Abstract
Purpose:
The aim of this study was to create vision standards for various tasks performed by hairdressers and to assess the spectacle compliance and its impact at work.
Methods:
The observational cross-sectional study enrolled hairdressers in and around Chennai, Tamil Nadu. It was done in three phases: (i) Job profiling from visual task analysis, creating vision standards for various hairdressing tasks and arriving at test protocols; (ii) Comprehensive eye examination, and (iii) Assessment of spectacle compliance and its impact on work. Descriptive analysis using Microsoft Excel and SPSS (IBM SPSS Statistics Version 21.0) was performed.
Results:
There were 305 participants with a mean age of 48 (SD ± 12) years. The visual acuity demand was found to be 6/18 and N15, for distance and near, respectively. Appropriate spectacles were prescribed for 203 (67%) hairdressers. Even with the best possible refractive correction, a few hairdressers did not meet the distance (13) and near (11) visual acuity standard. In all, 54 hairdressers were referred for further examination to a tertiary eye care center for lenticular changes, retinal abnormalities, and glaucoma screening. Among the subjects who were dispensed with spectacles, 181 (86%) were available for telephonic spectacle compliance assessment, and 164 (90%) were compliant with spectacle usage at work. Improved visual ability was reported by 133 (81%) hairdressers at work.
Conclusion:
This study provides vision standards for hairdressers. From the visual task analysis, hairdressing tasks were found to be visually demanding and hazardous. The study emphasizes that providing appropriate spectacle correction showed a clinically evident positive impact at work.
Keywords: Barbers, hairdressers, spectacle compliance, vision demands, vision standards
According to the International Standard Classification of Occupation (ISCO,2008), hairdressers are defined as workers who cut, style, color, straighten and permanently wave hair, shave or trim facial hair and treat scalp conditions.[1] Their work routine includes hair cutting/styling, moustache and beard trimming/shaving, and hair dyeing.[2] Though modern salons are emerging, traditional barbershops are still the major players in this field, mostly dominated by male workers.[3]
Visual demand is defined as the vision requirement for each particular task that varies from one occupation to another. Visual ability is the individual's personal ability to accomplish a visually demanding task. Vision standard is the minimum expected level of vision that is required for the efficient and safe performance of tasks of an individual at the workplace.[4] The abilities of the individuals to perform their tasks at work are determined by factors such as knowledge, experience, skills, and relevant training. In addition to that, the visual and ocular health of the individual also determines the ability, and accuracy of the task performance as well as the safety of the individual at work. When the visual ability of the individual does not match the visual standard, it will affect the visual task performance and thereby the productivity. Hairdressing is a visually intense task in terms of continuous near work which demands adequate near vision and associated visual skills. Uncorrected refractive error and presbyopia are known to affect task performance and productivity.[5,6] If the hairdresser is not meeting the visual demand, it will affect his productivity and customer satisfaction.
Commonly reported visual symptoms were headache, followed by blurred vision and ocular symptoms like itching, irritation, and tearing.[7,8,9] Due to the repetitive nature of the tasks and poor ergonomics, work-related lower back pain, followed by the neck, shoulder, and wrist pain were commonly observed.[7,10,11,12] There were no studies on understanding the visual demand for this occupation. This study aimed to understand the visual demand associated with the tasks performed by hairdressers and to estimate the vision standards, match the visual ability to the visual demand and understand the spectacle compliance at work.
Methods
This study was carried out by the Department of Occupational Optometry Services of a tertiary eye hospital, in Chennai. The strategy of convenience sampling was used. An association of hairdressers in Chennai was approached and informed about the need of the study. Hairdressers above 18 years of age with a minimum 1 year of experience, with willingness to participate, were recruited. Eye examinations were conducted at locations identified by the association. Consents for participation were obtained on behalf of the subjects and oral consent from the participants was also obtained, as it was done in a community setup. The study was approved by the Ethics Committee and Institutional Review Board of Vision Research Foundation and followed the principles of the Declaration of Helsinki. The study was done in three phases
Phase 1: To understand the work profile, create vision standards, and arrive at test protocols
Phase 2: Perform comprehensive eye examination to profile the visual and ocular symptoms
Phase 3: Assessment of spectacle compliance
Phase 1: After acquiring permission from proprietors, Visual Task Analysis (VTA) was carried out by two occupational optometrists in three different barbershops, using Grundy's task analysis grid [Appendix 1]. During VTA, observations on the size of the critical detail i.e., size of the hair, and working distance i.e., the distance at which the various tasks were performed, were made. Other task-related factors such as working position, the direction of gaze and the need for special accuracy/care during the task performance were recorded. The task-related clinical requirements such as the demand for binocular vision and stereopsis, visual fields and color vision were obtained. Observations on the work environment include visibility (the relationship between the size of detail working distances, contrast and time available for viewing the task), the type of lighting in use, illuminance level and presence of any hazards were also recorded during VTA.
The size of the target detail (mm) and working distance (cm) were used to arrive at the visual acuity demand for the various tasks. The size of human hair in the scalp and part of the face ranges between 0.06 and 0.1 mm in diameter.[12] Hairdressers usually gather strands of hair before they cut/trim and thus the size of hair strands was approximated to 1.0 mm. The distance vision demand was arrived using Grundy's Nomogram. Similarly, near vision demand for various tasks was arrived using the conversion table. The near visual acuity demand at 40 cm was converted to various measured working distances using the multiplication factor.[13] The visual acuity for both distance and near work was doubled from the baseline to ensure better visual comfort.[2,14]
The tasks being done at near to intermediate working distance, demand optimal accommodation, convergence and stereo-acuity for better task performance were measured, and they were calculated using the working distance and target size.
Accommodative Demand (D) = 100/Working Distance in (D)
For the continuous near work, accommodative demand was doubled to keep half of the accommodative amplitude in the reserve and the remaining used for task performance.[13]
-
Vergence Demand (Convergence)(PD): C = [10x IPD (in mm)]/[W + 2.7 mm] PD[15]
IPD – Interpupillary Distance, W – Working distance in mm,
PD = Prism Diopter
-
Stereopsis demand = (Δb) IPD/b2 (206265) arc sec[16]
Where b = is the observational distance: Δb is the standard deviation or the average of the longitudinal offset; IPD = Interpupillary distance; and 206265 conversion factors between radians and seconds of arc.
The normal central visual field is required for the task that mandates accuracy, eye-hand coordination, and safety. The peripheral visual field is required for reaching and judging the task movement.[17] The illuminance requirements for various tasks were arrived based on the nature of the task, need for speed or accuracy, age of the working population, and reflectance of the target background.[18]
Phase 2: Based on the observations from VTA, a battery of tests and questions about task-related symptoms to be incorporated in history were arrived at. All the hairdressers underwent the comprehensive eye examination: General and occupational history [Table 1], visual acuity testing for the distance using Log MAR visual acuity chart and near visual acuity testing using continuous text chart, refractive error assessment, anterior segment examination using Handheld Slit Lamp Bio-microscope, intraocular pressure measurement using non-contact tonometer and posterior segment examination using Non-Mydriatic fundus camera were done. Binocular vision assessment included near point of convergence, near point of accommodation, and stereo-acuity using Randot Stereogram. Hairdressers who deviated from required vision standards were either corrected with appropriate spectacles and/or referred for further examination. Readymade near correction was dispensed on the same day of examination if the subjects required only near correction. Other forms of spectacles were distributed two weeks later from the date of examination.
Table 1.
Occupational history for hairdressers
| OCCUPATIONAL HISTORY | |
|---|---|
| i) | Working as hairdressers since _______________ Years |
| ii) | Hours of working __________ in a day |
| iii) | Number of customers _________ in a day |
| iv) | The difficulty associated with Haircut/Shave: Yes/No |
| v) | Difficulty in picking grey hair from moustache: Yes/No |
| vi) | Difficulty in applying hair dye: Yes/No |
| vii) | History of any cut injury during haircut/shave: Yes/No |
| viii) | History of any dissatisfied customers: Yes/No |
| xi) | MSD: Pain in Neck/Shoulder/Lower back/Hip/Leg/Hand/Wrist/Fingers/General fatigue/Nil |
| x) | Breathing difficulty noted associated with haircut/hair dye application: Yes/No |
The table enumerates the questions which were arrived after visual task analysis to understand the work-related visual, ocular, and musculoskeletal symptoms among the hairdressers
Phase 3: The spectacle compliance was assessed over the telephone using the questionnaire [Appendix 2] two months later from the date of spectacle dispensing.
Statistical analysis
All the data were entered into Microsoft Excel and the analysis was done using SPSS (IBM SPSS Statistics Version 21.0). Mean (Standard Deviation) of the age, visual demand parameters (near visual acuity, the amplitude of accommodation, near point of convergence, amount of phoria for distance and near), and task illumination were calculated for vision standards. Frequency on the visual/ocular symptoms, ocular findings, and spectacle compliance were described.
Results
The results of the study are described with respect to each phase.
Phase 1: Job description, observation from VTA and Vision Standards
The job description was arrived at based on the visual task analysis and interviews with hairdressers. Their shops were usually opened early in the morning and the working hours varied from 8 hours to 12 hours per day. Their tasks involved hair cutting/trimming, cutting and styling moustache and beard, and applying hair dye. Besides, it was also observed that they have to pick and cut/remove one or more grey hairs from the moustache. All these tasks were carried out by standing, and during task performance, occasional gaze shifts upward or downwards were observed.
Based on the angular size of the target, distance vision demand was obtained. Though the tasks placed demands on near vision, the hairdresser at work also required optimal distance vision to look at the appearance of the customers in the mirror. They check for symmetry during the process of haircut, and after haircut, by holding the mirror behind the customer, to show the work done at the rear part of the head. Since the tasks involved more of near activity and mandated good eye-hand coordination, the normal central vision is important for hairdressers. Visual acuity for distance is calculated using the Grundy's Nomogram, for example for hair cutting task, the size of the detail is taken as 1 mm and distance between the eye and the object is taken as of 55 cm, the angle subtended at the eye is calculated to be 5.8 minutes of an arc, which corresponds to 6/36 visual acuity. Having twice as the demand, the required visual acuity for distance is 6/18. With the angular substance as 5.8 min of an arc, the required visual acuity for 40 cm is given as N12. For the distance of 55 cm, with the multiplication factor of 1.375, the required visual acuity for near is found to be N15. The vision standards arrived for various hairdressing tasks are elaborated in Table 2.
Table 2.
Vision standards for various tasks based on working distance and target size
| Task | Haircutting | Moustache/beard trimming | Shaving | Picking grey hair from Moustache |
|---|---|---|---|---|
| Working distance (in cm) | 55 | 50 | 60 | 50 |
| Size of detail (in mm) | 1 | 1 | 1 | 1 |
| Distance Visual Acuity | 6/18 | 6/18 | 6/18 | 6/18 |
| Near Visual Acuity | N 15@ 55 cm | N 15@ 50 cm | N 18 @ 60 cm | N 15@ 50 cm |
| Accommodative Demand (D) | 1.8 | 2 | 1.6 | 2 |
| Amplitude of Accommodation (D) | 3.6 | 4 | 2.5 | 4 |
| Convergence Demand (PD) | 12 | 12 | 10 | 12 |
| Stereopsis (Arc sec) | 40 | 50 | 30 | 50 |
| Visual field | Central | Central | Central | Central |
Visual demand for various visual skills that are required for the different occupational tasks was calculated with working distance and target size obtained from visual task analysis using Grundy’s Nomogram
The lighting at the barbershop was a combination of both daylight and artificial fluorescent light and the median illuminance level observed was 450 lux (350 lux to 520 lux). The need for speed and accuracy was observed to be important and reflectance of the task background was observed to be less than 30%. The illuminance level for various tasks was recommended to be 300 lux.[18]
Hairdressers were exposed to flying particles i.e., small hair-dust during hair cutting/trimming and chemicals from hair dye, bleach, and other hair care products. They were observed to use nose masks and gloves only during the application of hair dye.
Phase 2: Results from comprehensive eye examination
A total of 319 male hairdressers from various barbershops of Chennai participated in the study and their mean age was 48 ± 12 years (18–87 years). Among them, 14 stopped working due to various reasons like old age, health issues, musculoskeletal problems, and vision-related issues. For this study, we report the results from 305 working hairdressers. The mean years of work experience were 25 (SD: ±12) years. Most of them worked for 9 hours a day and on an average they provided hairdressing services to 15 customers in a day. From vision-related occupational history, visual disturbance related to any of the task was found in 131 (42.9%) subjects. Also, 109 (36%) had difficulty in haircutting and shaving, 102 (33.4%) had difficulty in picking grey hair from moustache, 20 (7%) reported difficulty applying hair dye and 18 (6%) reported difficulty in all three work-related tasks. Eight (2.6%) barbers reported cut injury, 11 (3.6%) reported frequent hair-dust falling in their eyes and 12 (3.9%) reported breathing difficulty during haircut and hair dye application.
No specific difficulties about workplace illuminance like poor lighting or glare at the workplace were reported. Apart from work-related vision complaints, near vision difficulty outside the work was reported by 91 (30%) hairdressers followed by distance vision difficulty by 45 (15%) hairdressers. Among 305 hairdressers, 67 (22%) were using spectacles. From the established vision standards as distance vision requirement of 6/18 and near vision requirement of N15, 44 (14.4%) did not meet the distance vision standard and 60 (20%) did not meet the near vision demand for the tasks either in one eye or both the eyes. Binocular vision parameters were assessed and we found 10 hairdressers reported to have blurring of distance vision on prolonged near work. None of the subjects reported symptoms like eye strain, double vision for near, etc., The average stereopsis was found to be 52 arcsec. Only two hairdressers exhibited near exophoria during the near cover test and they had no symptoms at work or otherwise. Other parameters for binocular vision were assessed with appropriate refractive error correction for distance and near.
The general vision and ocular symptoms reported by hairdressers are provided in Fig. 1. Anterior segment examination revealed lenticular changes with 127 (42%), pinguecula 39 (13%), meibomitis 22 (7.2%), and pseudophakia in one or both the eyes 19 (65) hairdressers. From posterior segment examination, macular scar was noted in two, drusen and hard exudates in one, RPE alteration at the macula in three, and diabetic retinopathy signs in one of the hairdressers. From optic disc evaluation, 13 (4.2%) were identified as glaucoma suspects based on Cup: Disc ratio and nerve fiber thinning. Fifty-four hairdressers were referred for further examination to tertiary eye care center: 29 (9.5%) for cataract surgery, 13 (4.2%) for glaucoma examination, eight (2.6%) for retinal examination, and three (1%) for ocular surface, and one for corneal examination. The systemic diseases among the hairdressers are shown in Fig. 2. In this study, work-related musculoskeletal disorders (WMSD) among hairdressers was found to be 35%.
Figure 1.
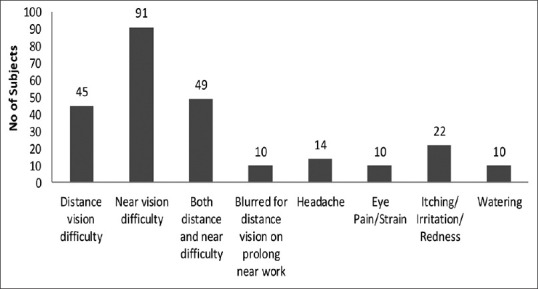
Visual and ocular symptoms associated with work among hairdressers
Figure 2.
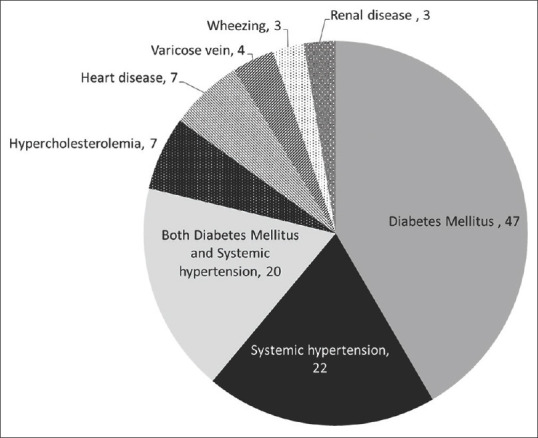
Details of systemic disease among hairdressers
A total of 203 (67%) hairdressers were prescribed spectacles. Even with appropriate refractive error and presbyopia correction, 13 hairdressers did not meet the distance vision standard and 11 did not meet the near vision standard for various occupational tasks. Those who did not meet the vision standard were observed to have lenticular changes and retinal pathology. The number of hairdressers who did not meet the required vision standards is listed in Table 3. Those who had unmet visual needs were referred for further evaluation. For this study, the compliance for referral has not been evaluated.
Table 3.
Number of individuals who did not meet the required vision standards
| Task | Required Vision Standards* | Number of people who did not meet the required vision standards at the time of presentation | Number of people did not meet the required vision standards with the intervention | Further intervention |
|---|---|---|---|---|
| Distance Visual Acuity | 6/18 | 44 | 13 | 11 Referred for cataract surgery and 2 for retinal examination |
| Near Visual Acuity | N 15@ 55 cm | 60 | 11 | 10 Referred for cataract surgery and 1 for retinal examination |
| Amplitude of Accommodation (D) | 4 | - | 10 | 9 Referred for cataract surgery and 1 for retinal examination for macular scar |
| Convergence Demand (PD) | 12 | - | 0 | |
| Stereopsis(Arc sec) | 30 | - | 18 | 3 Referred for cataract surgery and 1 for retinal examination for RPE alterations. |
*Size of the detail: 1 mm and working distance 50 cm
Phase 3: Spectacle compliance assessment
Of the 203 hairdressers who were prescribed with new spectacles, 158 (78%) claimed to be first-time spectacle wearers. Of these, 155 (76.3%) were prescribed bifocals, 21 (10%) single vision spectacles for near, 22 (10.4%) single vision spectacles for distance, and five (2%) progressive additional lenses. Spectacle compliance was assessed after two months from the date of distribution of spectacles. Totally 181 (86%) were available for tele-compliance assessment and of them, 164 (90%) were compliant to spectacle use at work. Of these, 133 (81%) reported improved visual ability at work with spectacles on.
Discussion
Studies have only concentrated on occupational demand mainly on ergonomics and dermatology among hairdressers. This study mainly established the vision standards for the hairdressers and emphasized that their visual ability improved by providing appropriate spectacle correction. In addition, it also arrived at the minimum near visual acuity demand as N15 for most of the hairdressing tasks that are done at the distance of 50-60 cm and distance visual acuity as 6/18. Hair dye application was observed to be less visually demanding, with near vision demand of N30. The accommodative and vergence demand was observed to be less, which is known to decrease with an increase in working distance. Reduced stereoacuity can be alarming when hairdressers have to take extra care about the pimples/boils/warts on the face of customers and not injure them during shaving/trimming of facial hair. Most of the time individuals with normal binocular vision were observed to have stereopsis of 50 arc seconds[14] and it is also known to decline after 50 years of age.[13] One of the hairdressers, whose stereoacuity was 200 arcsec, was observed to be pseudophakic in one eye and had cataract changes in another eye, but reported no task-related vision symptoms. However, he reported the incidence of unhappy customers on and off, through his 30 years of experience. Though it is due to age-related lenticular changes, appropriate cataract surgery and spectacle correction would have restored the normal stereoacuity.[19,20]
Optimal central visual field is required for better near task performance. Ocular pathology that causes central field loss might lead to delayed task performance, and affect safety during complex tasks.[17] Since the tasks which hairdressers perform require precision and safety, they must have a normal central field of vision. Out of the two hairdressers with macular scar, one of them reported difficulty in picking grey hair from moustache, and another reported both distance and near vision difficulty and was referred for further eye examination. Commonly reported visual/ocular symptoms as itching and irritation, headache, and eye pain/strain, and watering which is similar to most of the studies.[8,10,13,14]
Only 13 hairdressers reported difficulty in breathing during hair dye applications on customers. Among 11 hairdressers who reported frequent hair-dust falling in their eyes during haircutting, 10 were prescribed new spectacles which will act as protection from hair-dust falling. During the spectacle compliance assessment, one of the hairdressers reported that the spectacle usage reduced the hair fall into the eyes.
Near vision difficulty, both at-work and daily activities were reported only by 82 (26%) hairdressers. Of them, only five were observed to use spectacles for their near activities. A South Indian study on barriers to utilization of refraction services observed, the lack of a “Felt need” as the foremost barrier for the presbyopic population to seek refraction services and spectacle correction.[21] This, followed by a lack of awareness, together accounted for over 60% of the reasons for not seeking refraction services. Besides, the nature of the job, skilled/unskilled, and literacy were also observed to influence the spectacle seeking behavior.[21] From the spectacle compliance assessment, apart from 36% hairdressers who reported task-related vision difficulty, 81% reported improved visual ability at work with spectacles. They also appreciated the improved visual performance and reduced blur associated with tasks. It was evident from the spectacle compliance assessment that appropriate spectacle correction does have a positive impact on visual ability at work, thereby improving productivity.
Due to prolonged standing and awkward upper arm postures, hairdressers are prone to work-related musculoskeletal symptoms. Though most of the hairdressers reported more than one symptom, leg pain was most common, followed by neck and shoulder pain, lower back pain, hand pain, and general fatigue were associated with most of the tasks. From other studies, lower back pain was the most common reported symptom followed by neck and shoulder pain.[8,9,10,11,12]
The limitation of this study is that not all hairdressers were available for tele-compliance assessment for spectacles. The study has not used any quality-of-life questionnaire to assess any claim on the productivity or the visual performance. It may focus on the impact on quality of life and the visual abilities in future studies. The selection of hairdressers was through their workmen association, and this would impart a selection bias but it helped us to enroll many participants for the study in and around Chennai.
Conclusion
This study provides vision standards, job profile, vision, and ocular profile of the hairdressers. The near visual demand was not high for this occupation but the impact of the near vision correction on the performance at the job was felt by the study subjects. Thus it highlights the importance of matching visual demand and the visual ability of the individual at work for better visual-task performance by understanding the visual demand exerted by the occupation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Computer Age Management Services Limited for funding the study through their CSR support.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Dr. Anuja R Singh (Professor. – English Literature), Prof. Shankar Malhari (Professor – English Literature) - for their valuable suggestions and reviewing the manuscript.
Appendix 1
Grundy’s Visual Task Analysis Grid used for assessing the vision demand, illuminance, and hazard at the barbershop.
| Grundy Task Analysis Grid | |||
|---|---|---|---|
| Occupational Information | Clinical requirements | ||
| Working Distances | Far: Beyond 2 m | Visual Acuity | Calculated by using occupational information |
| Intermediate : 2 m - 55 cm | Binocular Vision/Steropsis | Required | |
| Near: 55 cm - 30 cm | Not important | ||
| Very near : <30 cm | Monocular vision adequate | ||
| Size of Detail | Large/medium: > 5’ | Colour Vision Requirement | Good |
| Small (3’ to 5’) | Limited | ||
| Very small (2’ to 3’) | Not required | ||
| Extremely small (1’ to 2’) | Visual Fields | Good field required | |
| Minute (<1’) | Fair field acceptable | ||
| Head Movements | Side to side | Poor | |
| Up and down | |||
| Mixture | |||
| Main Working Positions | Sitting | Environmental information | |
| Standing | Visibility | Good | |
| Moving | Fair | ||
| Mixture | Poor | ||
| Direction of Gaze | Ahead | Eye Protection Requirements | Required |
| Up | Not required | ||
| Down | Potential Danger | High risk | |
| Side | Medium risk | ||
| Mixture | Low risk | ||
| Task moment | Stationary | Hazard (s) | Present |
| Slow movement | Not present | ||
| Fast | Type of lighting in use, its | Good | |
| Changes of Gaze | Frequent | adequacy and suitability | Fair |
| Occasional | Poor | ||
| Seldom | |||
| Special Accuracy or Care | Required | ||
| Limited requirements | |||
| Not required | |||
Appendix 2
List of question enquired during spectacle compliance assessment
Received spectacles : Yes/No
Using their spectacles : Yes/No
-
If Yes, Frequency of using spectacles
- a. Using throughout the day b) On/off c) Only at the work d) Using for other activities ____________
-
Vision with spectacles
- a. Good and comfortable b) Bad and not comfortable to use
-
With spectacles on, vision during haircutting and trimming
- a. Good b) bad
-
With spectacles on, vision during shaving/bearded and moustache trimming
- a. Good b) bad
-
With spectacles on, vision during picking grey hair from moustache
- a. Good b) bad
References
- 1.International standard classification of occupations. ISCO-08. Part 3. [Last accessed on 2020 Nov 01]. Available from: https://www.ilo.org/public/english/bureau/stat/isco/docs/groupdefn08.pdf .
- 2.Wazir MS, Mehmood S, Ahmed A, Jadoon HR. Awareness among barbers about health hazards associated with their profession. J Ayub Med Coll Abbottabad. 2008;20:35–8. [PubMed] [Google Scholar]
- 3.Change among the nayindas of Karnataka. [Last accessed on 2020 July 27]. Available from: http://hdl.handle.net/10603/34375 .
- 4.Dr Santanam's Text book of Occupational. Optometry. 1st ed. Chennai: Elite School of Optometry, Unit of Medical Research Foundation; 2015. [Google Scholar]
- 5.Naidoo KS, Jaggernath J, Chinanayi FS, Chan VF. Near vision correction and work productivity among textile workers. African Vision and Eye Health. 2016;75:1–4. [Google Scholar]
- 6.Pradhan KB. Impact of uncorrected vision on productivity-A study in an industrial setting a pair of spectacles. J. Multidiscip. Res. Healthcare. 2015;1:119–31. [Google Scholar]
- 7.Bradshaw L, Harris-Roberts J, Bowen J, Rahman S, Fishwick D. Self-reported work-related symptoms in hairdressers. Occup Med. 2011;61:328–34. doi: 10.1093/occmed/kqr089. [DOI] [PubMed] [Google Scholar]
- 8.Skoufi GI, Nena E, Kostikas K, Lialios GA, Constantinidis TC, Daniil Z, et al. Work-related respiratory symptoms and airway disease in hairdressers. Int J Occup Environ Med. 2013;4:53–60. [PubMed] [Google Scholar]
- 9.Kumah DB, Mohammed A-K, Aidoo F, Walier I, Kuutiero I, Ablordeppey RK, et al. Prevalence of ocular conditions among hairdressers in the Kumasi Metropolis, Ghana. BAOJ Ophthalmol. 2017:1–6. [Google Scholar]
- 10.Kozak A, Wirth T, Verhamme M, Nienhaus A. Musculoskeletal health, work-related risk factors, and preventive measures in hairdressing: A scoping review. J Occup Med Toxicol. 2019;14:24. doi: 10.1186/s12995-019-0244-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hakim SA, MA Abdel Hamid. Occupational health risks of hairdressers: Knowledge, practice, and self-reported symptoms. Egyptian Journal of Occupational Medicine. 2019;43:161–74. [Google Scholar]
- 12. [Last accessed on 2020 Jul 27]. Available from: https://www.intechopen.com/books/hair-andscalp-disorders/anatomy-and-physiology-of-hair .
- 13.Monica R, Krishnakumar R, Santanam PP. Establishing pre-employment vision standards for goldsmiths. Indian J Occup Environ Med. 2012;16:27–33. doi: 10.4103/0019-5278.99689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Good GW, Weaver JL, Augsburger AR. Determination and application of vision standards in industry. American journal of industrial medicine. 1996;30:633–40. doi: 10.1002/(SICI)1097-0274(199611)30:5<633::AID-AJIM12>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 15.Bither PP. Determining the convergence demand for a patient who reads at a close working distance. Am J Optom Physiol Opt. 1987;64:355–60. doi: 10.1097/00006324-198705000-00009. [DOI] [PubMed] [Google Scholar]
- 16.James Saladin J. “Phorometry and Stereopsis.” Borish's Clinical Refraction. In: Benjamin WJ, Borish IM, editors. 2nd ed. Butterworth Heinemann/Elsevier; 2006. pp. 921–921. [Google Scholar]
- 17.Baker NA, Livengood H, Nau AC, Owens G, Chambers AJ, Trout J, et al. Effects of central and peripheral vision occlusion on motor performance during hand coordination tasks. IISE Transactions on Occupational Ergonomics and Human Factors. 2017;5:148–57. [Google Scholar]
- 18.Sanders MS, McCormick EJ. 7th ed. McGraw-Hill; 1993. Illumination. Human Factors in Engineering and Design; pp. 530–1. [Google Scholar]
- 19.Sucker J, Zvizdic M, Vogten H. Stereoscopic vision before and after cataract extraction with artificial lens implantation. Ophthalmologe. 2000;97:676–81. doi: 10.1007/s003470070036. [DOI] [PubMed] [Google Scholar]
- 20.Undrakonda V, Sahiti TK, Vennesh PS, Kamath YS. A comparative study of stereoacuity in patients with various grades of cataract and bilateral pseudophakia. Indian J Ophthalmol. 2019;67:1834–7. doi: 10.4103/ijo.IJO_401_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marmamula S, Keeffe JE, Raman U, Rao GN. Population-based cross-sectional study of barriers to utilisation of refraction services in South India: Rapid Assessment of Refractive Errors (RARE) Study. BMJ Open. 2011;1:e000172. doi: 10.1136/bmjopen-2011-000172. [DOI] [PMC free article] [PubMed] [Google Scholar]


