Abstract
Purpose:
To evaluate outcomes of anterior chamber intraocular lens (ACIOL) implantation with vitrectomy in eyes with surgical or traumatic aphakia, and subluxated or dislocated lens.
Methods:
In this retrospective study, we evaluated patients who underwent pars plans vitrectomy with ACIOL implantation from April 2016 to March 2019. Patients with minimum follow-up period of 1 year and operated by single surgeon were included. Ophthalmic history, indication for surgery, BCVA, IOP, slit-lamp examination, and fundus assessment findings were noted. Postoperatively best-corrected visual acuity (BCVA), intraocular pressure (IOP) and complications if any were noted.
Results:
Ninety eyes of 88 patients were included in the study. The mean age of the patients was 60.2 ± 10.2 yrs. Majority (75.6%) were males and 24.4% were females. Indications for pars-plana vitrectomy (PPV) with ACIOL implantation were nucleus drop in 16.6%, IOL drop in 25.5%, large posterior capsular rupture (PCR) with vitreous disturbance or zonular dehiscence (ZD) during cataract surgery in 33.3%, more than 180° subluxation of lens in 10% and traumatic lens or intraocular lens (IOL) drop in 14.4% cases. Preoperative and postoperative mean Log MAR visual acuity was 1.59 ± 0.44 and 0.36 ± 0.33 respectively, with few complications like cystoid macular edema (CME) in 8.8%, persistently raised IOP in 4.4%, persistent uveitis in 2.2%, retinal detachment (RD) in 2.2%, and tilted IOL in 1.1% cases.
Conclusion:
Out of different options available for secondary IOL implantation in patients with poor capsular support ACIOL has the advantages of cost-effectiveness, small learning curve, faster surgical time with a lesser rate of complications like IOL tilt, vitreous hemorrhage, and suture erosion as compared to scleral-fixated IOL (SF-IOL). Comparable visual outcome can be obtained by proper patient selection in these cases.
Keywords: AC IOL, PPV, SF IOL, surgical aphakia, traumatic aphakia
In the case of surgical aphakia due to cataract surgery complication or trauma with insufficient or no capsular support the option of intraocular lens (IOL) implantation can be scleral fixation, iris claw or anterior chamber IOL (ACIOL). Pars Plana Vitrectomy (PPV) is often undertaken in patients with a history of complicated cataract extraction with retained lens material in the posterior segment, IOL dislocation, subluxation of lens following trauma or associated systemic illness.
Early closed-loop ACIOLs were initially reported to have good short-term results, but were later found to be associated with several complications, including cystoid macular edema (CME), glaucoma, uveitis, hyphema, irreversible endothelial cell loss, and corneal decompensation.[1,2,3,4,5,6] However, new and improved open-loop ACIOL designs have eliminated the vast majority of these complications.[7,8,9,10] Data on the outcomes of open-loop ACIOLs in vitrectomised eyes are lacking. As a community-based eye hospital and cataract surgery training institute we got ample of patients with surgical aphakia with little or no capsular support as a result of cataract surgery complication. The principal aim of this study is to analyze complications and visual outcomes of ACIOL placement in vitrectomised eyes. A good number of patients with long follow-up data is utilized to describe the results.
Methods
A retrospective review of hospital records was conducted to evaluate consecutive patients who underwent ACIOL placement in the setting of concurrent vitreoretinal surgery from April 2016 to March 2019 in a community-based hospital in eastern India. Institutional Scientific and Ethical Committee approval was taken. Patients were included in this study if they underwent concurrent vitrectomy and ACIOL placement with a minimum follow-up period of 1 year and were operated by a single retinal surgeon. Patients were excluded if they had significant corneal edema preoperatively, prior history of glaucoma, or a history of severe trauma resulting in ocular sequelae such as corneal scar, or retinal detachment (RD). Patients having less than 1 year follow-up period were excluded. All study patients underwent a complete ophthalmic examination that included measurement of best-corrected visual acuity (BCVA) as determined on the Snellen visual acuity chart, measurement of intraocular pressure (IOP), slit-lamp examination, and fundus assessment by slit-lamp biomicroscopy and indirect ophthalmoscopy. Preoperative data collected included BCVA and prior ocular history of glaucoma, corneal disease, retinal detachment, or any other significant ocular complaint. Postoperative optical coherence tomography (OCT) results were obtained and reviewed at each visit. In few patients, however, preoperative OCT were not available as they were taken up for management of cataract surgery complication. The primary outcome measure was the occurrence of postoperative complications after ACIOL placement. The following complications were documented if they occurred within 1 year of postoperative period like elevated IOP, new macular edema, IOL dislocation, retinal detachment, vitreous hemorrhage or endophthalmitis. BCVA was reported as a secondary outcome. Postoperative follow-up were done at day-1, 1 week, 1 month, 6 month and 1 year. To standardize the follow-up period for all eyes included, postoperative visual acuity and P value calculations were assessed at 1 year. Similarly, postoperative complications, and OCT features were assessed up to 1 year postoperatively, as this was the maximum period of follow-up available for all eyes. Beyond this period, it was felt that complications could potentially be unrelated to the ACIOL surgery. Descriptive statistics were computed separately for each of the comparison groups. Chi-square analyses were used to compare categorical variables, and a paired t test was used to compare BCVA preoperatively and at last follow-up. A P value of <0.05 was considered statistically significant.
Surgical procedure
All surgeries were performed by single vitreoretinal surgeon. The following procedure was performed: A standard infusion line was placed infero temporally followed by superotemporal and superonasal opening. In cases of complicated cataract extraction, retained lens fragments were removed using the vitreous cutter or fragmantome for dense nuclear fragments. In cases with a dislocated lens, vitrectomy was performed to free the lens of any vitreous adhesions, and the lens is subsequently delivered to the anterior chamber. PPV and lensectomy was performed in the case of subluxated natural lens and/or bag complex. A corneal paracentesis was made, and pilocarpine is injected into the anterior chamber. A peripheral iridotomy was made with the vitreous cutter. The infusion pressure lowered to 10 mmHg. The horizontal white-to-white diameter of the cornea is measured intra-operatively with Casterveijo caliper by placing each tip on limbus just beyond the clear cornea and by adjusting the caliper under microscope and the ACIOL length sized at 1 mm greater than the horizontal white-to-white dimension. A superior scleral tunnel was made for the placement of the ACIOL if it was not there, as this incision allows for greater control of the anterior chamber and less postoperative astigmatism. AC IOL surface was made upside down to avoid endothelial touch and providing a good anterior chamber depth and to keep the IOL at equidistance from corneal endothelium and anterior surface of iris. A lens glide was placed across the pupil to aide in lens placement as and when required. McPherson forceps were used to grasp the lens including the trailing haptic and about halfway across the optic and the lens was inserted into the anterior chamber. The trailing haptic then tucked into the angle under the wound. A Sinskey hook was used to rotate the ACIOL counterclockwise so that the haptics are oriented 90 away from the scleral tunnel incision at the 3 and 9 O’clock orientation. The ACIOL should ideally be positioned in the iridocorneal angle with the footplates in contact with the scleral spur. Care was taken to assure the pupil is round and there is no pupil peaking ensuring complete removal of vitreous from the anterior chamber. The cannulas were then removed and the sclerotomies are sutured. After the wound is watertight and the chamber well maintained, the peritomy was closed using 8.0 vicryl. A representative case of dropped IOL and postoperative ACIOL is shown in Fig. 1.
Figure 1.
(a) Intraoperative photograph of dropped IOL. (b) Postoperative photograph after placement of ACIOL
Results
Ninety eyes of 88 patients were included in the study. Mean age of the patients was 60.2 ± 10.2 yrs. Almost one fourth (24.4%) were females and majority (75.6%) were males of which in 2 patients both eyes were operated due to subluxated lens with associated Marfans syndrome. Indications for PPV with ACIOL implantation were as follows. Nucleus drop in 15 eyes (16.6%) and IOL drop in 23 eyes (25.5%) and large PCR with vitreous disturbance or ZD during cataract surgery in 30 eyes (33.3%) in which 14 eyes had signs of pseudo exfoliation and 4 patients had history of uveitis. More than 180 degree subluxation of IOL was seen preoperatively in 9 eyes (10%) in which 3 eyes had pseudoexfoliation and 6 had Marfans syndrome. Thirteen eyes (14.4%) had history of trauma following which there was lens or IOL drop, in this 2 patients had vitreous hemorrhage and 1 had hyphema preoperatively. Preoperative and post-operative mean LogMAR visual acuity was 1.59 ± 0.44 and 0.36 ± 0.33 respectively. Postoperative complications included cystoid macular edema (CME) in 8 (8.8%) eyes, persistently raised IOP in 4 (4.4%) eyes [Fig. 2], persistent uveitis in 2 eyes (2.2%), RD in 2 eyes (2.2%) and tilted IOL in 1 eye (1.1%). In patients with CME 1 patient had history of uveitis and 2 had history of trauma. Of 4 eyes with persistently raised IOP 2 patients had signs of pseudo exfoliation and one had history of uveitis preoperatively. The mean spherical equivalent was 1.5D and the difference in final postoperative and target refraction was found to be 0.5D. In all 4 patients with raised IOP it was under control by one to three topical antiglaucoma medications which included timolol, brinzolamide or brimonidine. Visual outcomes and complications of surgery were shown in Table 1 and percentage of eyes with complications is represented as pie chart in Fig. 3.
Figure 2.

Pie chart showing percentage of eyes with raised IOP
Table 1.
Baseline characteristics, pre- and postop BCVA and complications
| Parameters | Numbers/ Percentage |
|---|---|
| Total eyes | 90 |
| Mean age | 60.2±10.2 years |
| Gender-wise Distribution | |
| Males | 75.60% |
| Females | 24.40% |
| Indications for surgery n, (%) | |
| Nucleus drop | 15, (16.6%) |
| IOL drop | 23, (25.5%) |
| PCR/ZD | 30, (33.3%) |
| Subluxated lens | 9, (10%) |
| Traumatic IOL drop or dislocated/Subluxated lens | 13, (14.4%) |
| Mean visual acuity in LogMAR | |
| Preoperative | 1.59±0.44 |
| Postoperative | 0.36+/_0.33 |
| Postop complications, n, (%) | |
| Cystoid macular edema | 8, (8.8%) |
| Persistent elevated IOP | 4, (4.4%) |
| Persistent uveitis | 2, (2.2%) |
| Retinal detachment | 2, (2.2%) |
| Tilted IOL | 1, (1.1%) |
Figure 3.
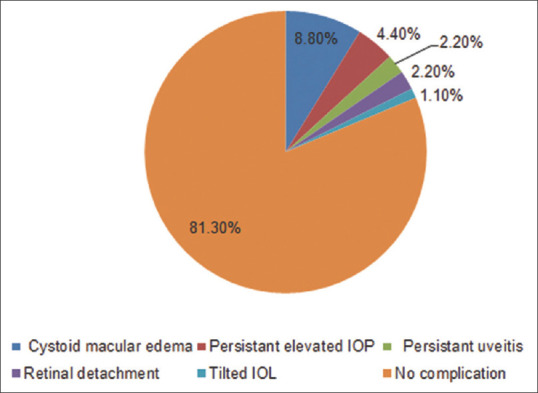
Pie chart of postop complication
Discussion
Numerous studies have looked at the safety of patients undergoing ACIOL implantation alone.[2,3,11] There are limited studies on PPV combined with ACIOL implantation. In our study we analyzed the outcomes of PPV with ACIOL implantation done by single surgeon and with large sample size and longer follow-up. Mean log MAR visual acuity in our study is comparable to other studies[12,13,14,15] on ACIOL and also to studies on SFIOL [Table 2].[13,16] The comparison is limited by indications of surgery, type of surgery, sample size, and follow-up period. The rate of macular edema in different studies range from 8-24%.[12,16] In our study the percentage of macular edema was 8.8%, which is comparable to other studies on ACIOL and SFIOL implantation.[16,17] After ACIOL insertion in non-vitrectomised eyes the rate of both short and long-term rise in IOP varies greatly between studies. For example, one study on primary ACIOL implantation was done with anterior vitrectomy found 100% patients had a long-term IOP rise,[18] while in another study where secondary IOL implantation was done with proper vitrectomy it was found that only 4.1% of patients developed late secondary glaucoma.[19] The rate of raise in IOP in our study is 4.4% which is correlating with some studies.[14,19] In contradiction a study by GS Negrettei et al.,[15] 32% patients developed postop long-term raise in IOP following ACIOL implantation in vitrectomised eyes. It is possible to conclude, that the chance of raise in IOP is less in patients undergoing proper vitrectomy. Also patients need to be properly counseled before ACIOL insertion about the risks of raised IOP and its management needs careful patient selection and monitoring after surgery. Several studies found that there is no statistically significant difference in raised IOP between ACIOL and SFIOL.[16,17,18,19] The rate of retinal detachment varies in different studies ranges from 0- 6%.[14,15,16] The rate of retinal detachment in our study is 2.2%. The rate of other complications like postop uveitis, instability in IOL are corresponding to different studies.[13,14,15,16] Also the results of persistent uveitis in our study is corresponding with the studies on SFIOL.[16,18,19] Recently, there has been an emphasis on SFIOLs in the setting of vitrectomy, either by sutured or sutureless techniques. This technique may be better suited to some patients, particularly those with iris tissue defects, significant corneal disease, or history of severe trauma. However, potential complications with this technique are numerous and include lens tilt, variability in lens location, suture erosion, lens dislocation, and potential opacification with air or gas.[20,21,22,23,24,25,26,27,28] Khan et al.[16] described 84 eyes undergoing Gore-Tex suture scleral fixation of secondary IOL in the setting of PPV, with a similar rate of ocular hypertension occurring in their study: 3.6% of eyes vs. 4.4% in our study. Notably, they reported an increased rate of vitreous hemorrhage (7.1%) but a lower rate of postoperative CME (4.8%), compared with 0% and 8.8% in our study respectively. Budoff et al.[22] report on 19 eyes undergoing SFIOLs, showed IOL decentration occurred in 3 eyes, Vitreous hemorrhage occurred in 4 eyes, and CME occurred in 4 eyes. Abbey et al.[20] reported 23 eyes with sutureless scleral fixation of IOLs, with similar rates of macular edema (8.7%) compared with our study and a similar rate of vitreous hemorrhage compared with Budoff et al.[22] and Khan et al.[16] None of their patients had significant preoperative ocular comorbidities.[20,21,22,23,24,25,26,27,28,29] Whereas the reported rates of complications are variable, the SFIOL techniques may be associated with a higher rate of vitreous hemorrhage but a potentially lower rate of macular edema compared with those of ACIOL placement.
Table 2.
Comparison of outcomes of ACIOL with other studies
| Parameters | Our study | Finn et al.[14] | Negretti GS et al. | Khan MA et al. |
|---|---|---|---|---|
| Sample size (n) | 90 | 50 | 271 | 33 |
| Preoperative mean Log MAR VA | 1.59±0.44 | 0.96±0.77 | 1.27±0.77 | 1.66±0.74 |
| Postoperative mean Log MAR VA | 0.36±0.33 | 0.28±0.27 | 0.51±0.66 | 0.4±0.39 |
| Complications (%) | ||||
| Corneal decompensation | - | 2 | 6 | - |
| Persistently raised IOP | 4.4 | 8 | 23 | 3 |
| Persistant uveitis | 2.2 | 2 | - | - |
| IOL tilt/displacement | 1.1 | - | 7 | - |
| Cystoid macular edema | 8.8 | 14 | 15 | 3 |
| Epiretinal membrane | - | 4 | 6.1 | |
| Retinal detachment | 2.2 | - | 6 | - |
A study by Khan et al.[16] found that transient corneal edema in the early postoperative period was more common with use of an ACIOL, but long-term corneal edema or bullous keratopathy was not observed with PPV with vortex suture fixated SFIOL or ACIOL. Corneal decompensation has been a theoretical concern with ACIOL placement since they were first introduced. There are relatively less number of patients developing corneal decompensation[5,11,19,30] particularly if it is performed along with PPV as done in our study and it is reassuring that with open loop anterior chamber lenses corneal problems occur rarely, even in patients with multiple previous vitreoretinal procedures. Many also argue, conversely, that ACIOL surgery results in increased endothelial cell count loss, a substantial shortcoming for the procedure.[18,31,32,33] However, this point is under debate, with new research pointing to surgical trauma in general resulting in the endothelial cell count loss rather than specifically the implanted ACIOL[17] In our study no patient developed persistent corneal edema or bullous keratopathy. The main limitation of our study is we didn’t assess corneal endothelial cell count to look for endothelial decompensation. As several publications reported corneal complications like bullous keratopathy after implantation of ACIOL it would be ideal to go for corneal endothelial count preoperatively and use chondroitin sulfate based OVD to coat the corneal endothelium before implantation of ACIOL. Future studies on corneal endothelial cell count preoperatively and postoperatively following ACIOL implantation with long follow-up period are required to estimate the endothelial cell loss.
Conclusion
To conclude, out of different options available for secondary IOL implantation in patients with poor or no capsular support, ACIOL with simultaneous vitrectomy with some modification in technique like upside-down placement of IOL has the advantages of cost-effectiveness, small learning curve, faster surgical time with lesser rate of complications like IOL tilt, vitreous hemorrhage, and suture erosion as compared to SFIOL. Hence, it can be considered as a viable option for secondary IOL implantation preferably in community-based hospitals.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Smith PW, Wong SK, Stark WJ, Gottsch JD, Terry AC, Bonham RD. Complications of semiflexible, closed-loop anterior chamber intraocular lenses. Arch Ophthalmol. 1987;105:52–7. doi: 10.1001/archopht.1987.01060010058031. [DOI] [PubMed] [Google Scholar]
- 2.Biro Z. Results and complications of secondary intraocular lens implantation. J Cataract Refract Surg. 1993;19:64–7. doi: 10.1016/s0886-3350(13)80284-2. [DOI] [PubMed] [Google Scholar]
- 3.Drolsum L. Long-term follow-up of secondary flexible, open-loop, anterior chamber intraocular lenses. J Cataract Refract Surg. 2003;29:498–503. doi: 10.1016/s0886-3350(02)01614-0. [DOI] [PubMed] [Google Scholar]
- 4.Hennig A, Johnson GJ, Evans JR, Lagnado R, Poulson A, Pradhan D, et al. Long term clinical outcome of a randomised controlled trial of anterior chamber lenses after high volume intracapsular cataract surgery. Br J Ophthalmol. 2001;85:11–7. doi: 10.1136/bjo.85.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donaldson KE, Gorscak JJ, Budenz DL, Feuer WJ, Benz MS, Forster RK. Anterior chamber and sutured posterior chamber intraocular lenses in eyes with poor capsular support. J Cataract Refract Surg. 2005;31:903–909. doi: 10.1016/j.jcrs.2004.10.061. [DOI] [PubMed] [Google Scholar]
- 6.Ravalico G, Botteri E, Baccara F. Long-term endothelial changes after implantation of anterior chamber intraocular lenses in cataract surgery. J Cataract Refract Surg. 2003;29:1918–23. doi: 10.1016/s0886-3350(02)02052-7. [DOI] [PubMed] [Google Scholar]
- 7.Lim ES, Apple DJ, Tsai JC, Morgan RC, Wasserman D, Assia EI. An analysis of flexible anterior chamber lenses with special reference to the normalized rate of lens explantation. Ophthalmology. 1991;98:243–6. doi: 10.1016/s0161-6420(91)32310-8. [DOI] [PubMed] [Google Scholar]
- 8.Solomon KD, Apple DJ, Mamalis N, Gwin TD, Wilbandt HH, Hansen SO, et al. Complications of intraocular lenses with special reference to an analysis of 2500 explanted intraocular lenses (IOLs) J Cataract Refract Surg. 1991;3:195–200. [Google Scholar]
- 9.Weene LE. Flexible open-loop anterior chamber intraocular lens implants. Ophthalmology. 1993;100:1636–9. doi: 10.1016/s0161-6420(13)31445-6. [DOI] [PubMed] [Google Scholar]
- 10.Auffarth GU, Wesendahl TA, Brown SJ, Apple DJ. Are there acceptable anterior chamber intraocular lenses for clinical use in the 1990s? An analysis of 4104 explanted anterior chamber intraocular lenses. Ophthalmology. 1994;101:1913–22. doi: 10.1016/s0161-6420(94)31083-9. [DOI] [PubMed] [Google Scholar]
- 11.Chan TC, Lam JK, Jhanji V, Li EY. Comparison of outcomes of primary anterior chamber versus secondary scleral-fixated intraocular lens implantation in complicated cataract surgeries. Am J Ophthalmol. 2015;159:221–6.e2. doi: 10.1016/j.ajo.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 12.Kazemi S, Wirostko WJ, Sinha S, Mieler WF, Koenig SB, Sheth BP. Combined pars plana lensectomy-vitrectomy with open-loop flexible anterior chamber intraocular lens (AC IOL) implantation for subluxated lenses. Trans Am Ophthalmol Soc. 2000;98:247–53. [PMC free article] [PubMed] [Google Scholar]
- 13.Melamud A, Topilow JS, Cai L, He X. Pars plana vitrectomy combined with either secondary scleral-fixated or anterior chamber intraocular lens implantation. Am J Ophthalmol. 2016;168:177–82. doi: 10.1016/j.ajo.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Finn AP, Feng HL, Kim T, Mahmoud TH. Outcomes of anterior chamber intraocular lens implantation in patients undergoing pars plana vitrectomy. Ophthalmol Retina. 2018;2:895–9. doi: 10.1016/j.oret.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 15.Negretti GS, Lai M, Petrou P, Walker R, Charteris D. Anterior chamber lens implantation in vitrectomised eyes. Eye (Lond) 2018;32:597–601. doi: 10.1038/eye.2017.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khan MA, Gupta OP, Pendi K, Chiang A, Vander J, Regillo CD, et al. Pars plana vitrectomy with anterior chamber versus gore-tex sutured posterior chamber intraocular lens placement: Long-Term Outcomes. Retina. 2019;39:860–6. doi: 10.1097/IAE.0000000000002042. [DOI] [PubMed] [Google Scholar]
- 17.Radke N, Liu S, Chen L. Pars plana vitrectomy combined with either secondary scleral-fixated or anterior chamber intraocular lens implantation. Am J Ophthalmol. 2017;176:261–2. doi: 10.1016/j.ajo.2017.01.029. [DOI] [PubMed] [Google Scholar]
- 18.Kwong YY, Yuen HKL, Lam RF, Lee VY, Rao SK, Lam DS. Comparison of outcomes of primary scleral-fixated versus primary anterior chamber intraocular lens implantation in complicated cataract surgery. Ophthalmology. 2007;114:80–5. doi: 10.1016/j.ophtha.2005.11.024. [DOI] [PubMed] [Google Scholar]
- 19.Evereklioglu C, Er H, Bekir NA, Borazan M, Zorlu F. Comparison of secondary implantation of flexible open-loop anterior chamber and scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg. 2003;29:301–8. doi: 10.1016/s0886-3350(02)01526-2. [DOI] [PubMed] [Google Scholar]
- 20.Abbey AM, Hussain RM, Shah AR, Faia LJ, Wolfe JD, Williams GA. Sutureless scleral fixation of intraocular lenses: Outcomes of two approaches. The 2014 Yasuo Tano Memorial Lecture. Graefes Arch Clin Exp Ophthalmol. 2015;253:1–5. doi: 10.1007/s00417-014-2834-9. [DOI] [PubMed] [Google Scholar]
- 21.Maggi R, Maggi C. Sutureless scleral fixation of intraocular lenses. J Cataract Refract Surg. 1997;23:1289–94. doi: 10.1016/s0886-3350(97)80104-6. [DOI] [PubMed] [Google Scholar]
- 22.Budoff G, Miller CG, Halperin SJ, Jeng-Miller KW, Fine HF, Wheatley HM, et al. One year outcomes of a novel technique for rescuing and scleral fixating a posterior dislocated intraocular lens–bag complex without conjunctival opening (HOFFMAN POCKETS) Retina. 2016;36:1935–40. doi: 10.1097/IAE.0000000000001039. [DOI] [PubMed] [Google Scholar]
- 23.Price MO, Price FW, Jr, Werner L, Berlie C, Mamalis N. Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refract Surg. 2005;31:1320–6. doi: 10.1016/j.jcrs.2004.12.060. [DOI] [PubMed] [Google Scholar]
- 24.Fu AD, McDonald HR, Jumper JM, Aaberg TM, Sr, Smiddy WE, Robertson JE, et al. Recurrent vitreous hemorrhage after sutured posterior chamber intraocular lenses. Retina. 2004;24:193–8. doi: 10.1097/00006982-200404000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Kjeka O, Bohnstedt J, Meberg K, Seland JH. Implantation of scleral-fixated posterior chamber intraocular lenses in adults. Acta Ophthalmol. 2008;86:537–42. doi: 10.1111/j.1600-0420.2007.01095.x. [DOI] [PubMed] [Google Scholar]
- 26.Forlini M, Orabona GD, Bratu AI, Rossini P, Cavallini GM, Forlini C. Akreos Adapt AO intraocular lens opacification: A case report. Case Rep Ophthalmol. 2013;4:151–4. doi: 10.1159/000355414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walker NJ, Saldanha MJ, Sharp JA, Porooshani H, McDonald BM, Ferguson DJ, et al. Calcification of hydrophilic acrylic intraocular lenses in combined phaco vitrectomy surgery. J Cataract Refract Surg. 2010;36:1427–31. doi: 10.1016/j.jcrs.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 28.Lee CE, Kim YC, Chang SD. Opacification of the optic of an Akreos Adapt intraocular lens. Korean J Ophthalmol. 2010;24:371–3. doi: 10.3341/kjo.2010.24.6.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dajee KP, Abbey AM, Williams GA. Management of dislocated intraocular lenses in eyes with insufficient capsular support. Curr Opin Ophthalmol. 2016;27:191–5. doi: 10.1097/ICU.0000000000000260. [DOI] [PubMed] [Google Scholar]
- 30.Brunin G, Khandelwal S, Coffee RE, Orengo-Nania S, Biggerstaff KS. Outcomes of anterior chamber intraocular lenses placed by surgeons in training. J Cataract Refract Surg. 2015;41:2102–6. doi: 10.1016/j.jcrs.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Pechméja J, Guinguet J, Colin J, Binder PS. Severe endothelial cell loss with anterior chamber phakic intraocular lenses. J Cataract Refract Surg. 2012;38:1288–92. doi: 10.1016/j.jcrs.2012.04.022. [DOI] [PubMed] [Google Scholar]
- 32.Bading G, Hillenkamp J, Sachs HG, Gabel VP, Framme C. Long-term safety and functional outcome of combined pars plana vitrectomy and scleral-fixated sutured posterior chamber lens implantation. Am J Ophthalmol. 2007;144:371–7. doi: 10.1016/j.ajo.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 33.Olsen TW, Pribila JT. Pars plana vitrectomy with endoscope-guided sutured posterior chamber intraocular lens implantation in children and adults. Am J Ophthalmol. 2011;151:287–96.e2. doi: 10.1016/j.ajo.2010.08.026. [DOI] [PubMed] [Google Scholar]



