Unilateral axillary lymphadenopathy is now recognized as a common finding following administration of the COVID-19 vaccination.1., 2., 3. As such, it has become a confounding variable in breast imaging, particularly in high-risk women, as the differentiation between COVID-19 vaccine-related lymphadenopathy and metastatic disease has become difficult. Furthermore, management recommendations vary widely with some radiologists advocating for a benign assessment, while others suggest short-term follow-up or biopsy.2., 3., 4.
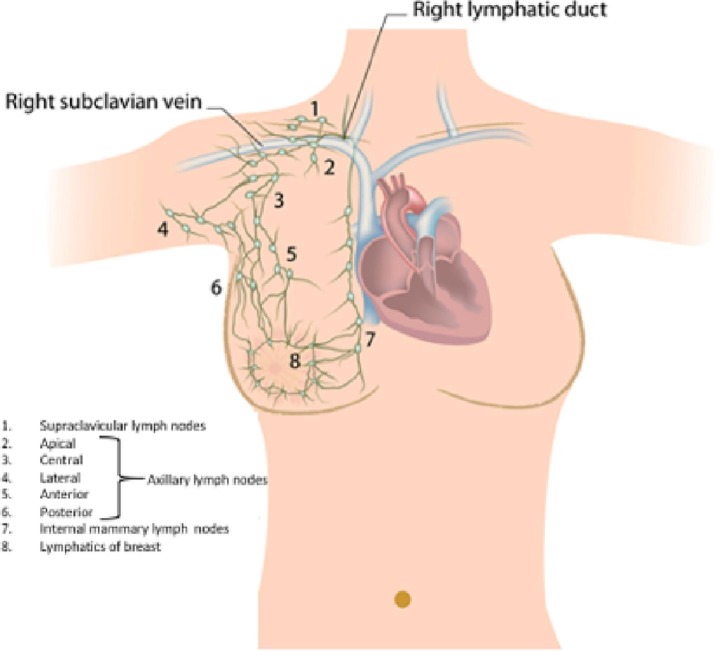
Review of the anatomy of axillary lymphatic drainage reminds us that there exist five groups that coalesce to drain the upper limb and superior thoracic region: anterior (pectoral), posterior (subscapular), lateral (humeral), central, and apical.5 The anterior nodes drain the anterior thoracic wall, including the breast. The posterior nodes drain the posterior thoracic wall and the lateral nodes drain the upper limb. These three groups drain into the central nodes before reaching their ultimate destination, the apical nodes. Fig. 1 illustrates these described axillary lymphatic groups.
Fig. 1.
Illustration of the lymphatic drainage groups of the upper torso and upper extremity, including the breast.
Breast MRI provides an advantage over mammography and ultrasound because its larger field of view gives a more complete picture of the anatomic landscape of the axilla. Knowing that the COVID-19 vaccine is administered intramuscularly in the deltoid muscle of the upper arm and understanding the lymphatic drainage pattern of the breast and upper extremity we suggest that a pattern of unilateral axillary lymphadenopathy involving the lateral, central, and/or apical groups with relative sparing of the anterior group is typical for vaccine-related lymphadenopathy. This notion is validated through numerous cadaveric studies, functional studies on lymph drainage, and axillary reverse mapping.6
The following is a brief representative example of the typical pattern of axillary adenopathy presenting on breast MRI after vaccination that warrants a benign assessment in view of the known anatomy and lymphatic drainage: A 63-year-old asymptomatic female undergoes routine screening breast MRI having had recent COVID-19 second vaccine dose given to the left arm six days prior to the exam. No suspicious enhancement is present in the left breast (Fig. 2 ). Fig. 3 demonstrates morphologically abnormal high level II/III axillary lymph nodes (central and apical group) in the presence of normal low level I axillary lymph nodes (anterior group) (Fig. 4 ).
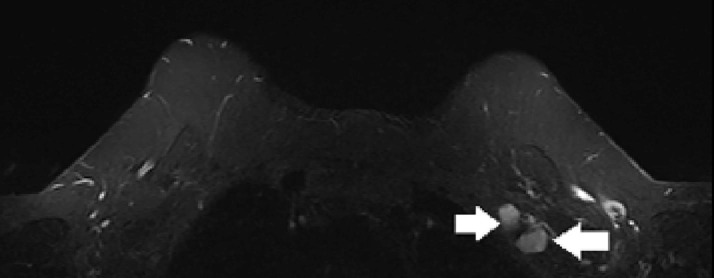
Fig. 2.
Axial first post contrast subtraction maximum intensity projection image demonstrating no suspicious enhancement within the breasts.
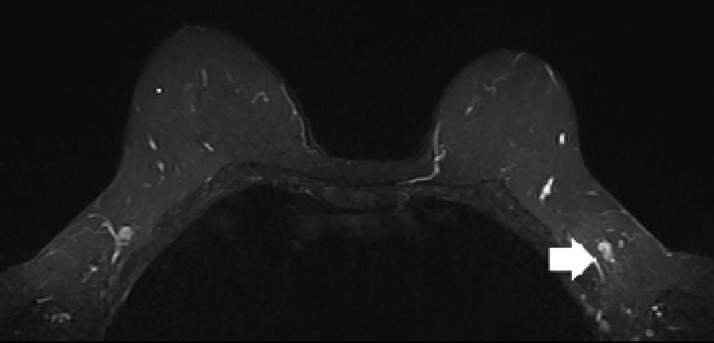
Fig. 3.
Axial STIR image demonstrating enlarged morphologically abnormal level 2 and level 3 lymph nodes (central/apical groups) marked by white arrows.
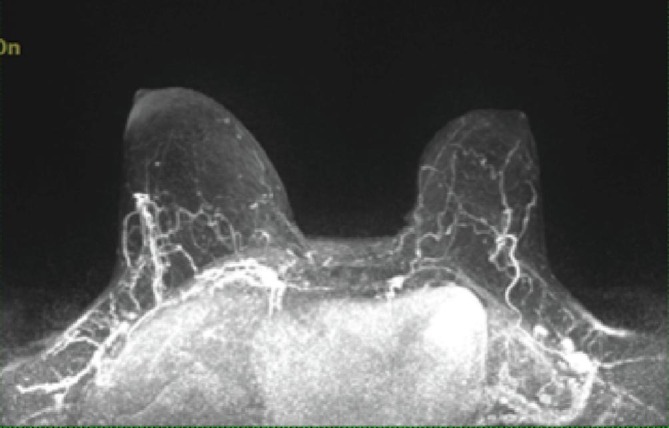
Fig. 4.
Axial STIR image demonstrating a representative morphologically normal low level I axillary lymph node (anterior group) marked by a white arrow.
Identifying this pattern of unilateral axillary adenopathy in the setting of ipsilateral COVID-19 vaccine administration and a negative screening breast MRI allows one to confidently give a benign assessment in keeping with a pragmatic approach and; thereby, reducing the number of unnecessary follow-ups and/or biopsies performed and obviating the need to delay breast MRI screening for recent vaccination.
Importantly, we acknowledge that there are some caveats to this approach as it is geared towards asymptomatic women at high lifetime risk for breast cancer with otherwise no significant medical history. On the other hand, even when this imaging pattern is present, management of oncology patients should be personalized on the basis of the cancer type, lymph node drainage pathway, and risk of metastasis with engagement of the multidisciplinary team.7 A final consideration is that anterior and lateral group nodes are both level I axillary lymph nodes and although they can sometimes be traced to a particular artery; they often are seen isolated in the axillary fat such that even with cross sectional imaging, they cannot always be readily differentiated.8
References
- 1.Özütemiz C., Krystosek L.A., Church A.L., et al. Lymphadenopathy in COVID-19 vaccine recipients: diagnostic dilemma in oncology patients. Radiology. 2021:210275. doi: 10.1148/radiol.2021210275. Published online February 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edmonds C.E., Zuckerman S.P., Conant E.F. Management of unilateral axillary lymphadenopathy detected on breast MRI in the era of coronavirus disease (COVID-19) vaccination. Am J Roentgenol. 2021 doi: 10.2214/ajr.21.25604. Published online February 5. [DOI] [PubMed] [Google Scholar]
- 3.Lehman C.D., Lamb L.R., D’Alessandro H.A. Mitigating the impact of coronavirus disease (COVID-19) vaccinations on patients undergoing breast imaging examinations: a pragmatic approach. Am J Roentgenol. 2021 doi: 10.2214/ajr.21.25688. Published online February 22. [DOI] [PubMed] [Google Scholar]
- 4.Lehman C.D., D'Alessandro H.A., Mendoza D.P., Succi M.D., Kambadakone A., Lamb L.R. Unilateral lymphadenopathy after COVID-19 vaccination: a practical management plan for radiologists across specialties. J Am Coll Radiol. 2021 doi: 10.1016/j.jacr.2021.03.001. S1546-1440(21)00212-X. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kyriacou H., Khan Y.S. StatPearls [Internet] StatPearls Publishing; Treasure Island (FL): 2021. Anatomy, shoulder and upper limb, axillary lymph nodes. [Updated 2021 Feb 13]https://www.ncbi.nlm.nih.gov/books/NBK559188/ [PubMed] [Google Scholar]
- 6.Cirocchi R., Amabile M.I., De Luca A., et al. New classifications of axillary lymph nodes and their anatomical-clinical correlations in breast surgery. World J Surg Onc. 2021;19:93. doi: 10.1186/s12957-021-02209-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Becker A.S., Perez-Johnston R., Chikarmane S.A., Chen M.M., El Homsi M., Feigin K.N., Gallagher K.M., Hanna E.Y., Hicks M., Ilica A.T., Mayer E.L., Shinagare A.B., Yeh R., Mayerhoefer M.E., Hricak H., Vargas H.A. Multidisciplinary recommendations regarding post-vaccine adenopathy and radiologic imaging: radiology scientific expert panel. Radiology. 2021:210436. doi: 10.1148/radiol.2021210436. Feb 24. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ecanow J.S., Abe H., Newstead G.M., Ecanow D.B., Jeske J.M. Axillary staging of breast cancer: what the radiologist should know. Radiographics. 2013 Oct;33(6):1589–1612. doi: 10.1148/rg.336125060. [DOI] [PubMed] [Google Scholar]