According to the United States Renal Data System (USRDS), the number of people with end-stage kidney disease (ESKD) in the United States has increased every year between 1980 and 2018.1,2 Between 1980 and 2000, the increasing prevalence reflected mostly the rapidly increasing incidence of ESKD. Since 2000, the increasing prevalence has shifted toward improved survival among patients on maintenance dialysis, as well as those with a functioning kidney transplant. Recent forecasting of the size of the ESKD population had suggested continued growth during the 2020s.3 However, no forecast could have anticipated the novel coronavirus disease 2019 (COVID-19) pandemic. During the early part of the pandemic, all-cause mortality was 17% and 30% higher than expected among dialysis and transplant patients, respectively, whereas the number of patients who initiated kidney replacement therapy (KRT) declined sharply.2,4 Considering that the rate of COVID-19 hospitalization was approximately 40 times higher among dialysis patients than in the general population,4 it is likely that substantial mortality also occurred during the past winter. In this report, we quantified the impact of COVID-19 on the size of the ESKD population at 1 year after the declaration of a national emergency.
We analyzed data extracted from the End Stage Renal Disease Quality Reporting System (EQRS) in May 2021. For each epidemiologic week (Sunday to Saturday) from week 1 of 2015 to week 13 of 2021, we identified all patients with ESKD at the beginning of the week. We identified the KRT status (dialysis, transplant), age, and race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Asian, other) of each patient. We tabulated numbers of patients in subgroups defined by each of these factors. In each subgroup, we fit a linear regression of weekly counts from week 1 of 2015 to week 13 of 2021; the model included only calendar time, which was parameterized as a second-order (i.e., quadratic) polynomial. Fitted models were used to derive forecasted weekly counts through week 13 of 2021; forecasted weekly counts of ESKD patients were derived by summing forecasted counts of dialysis and transplant patients.
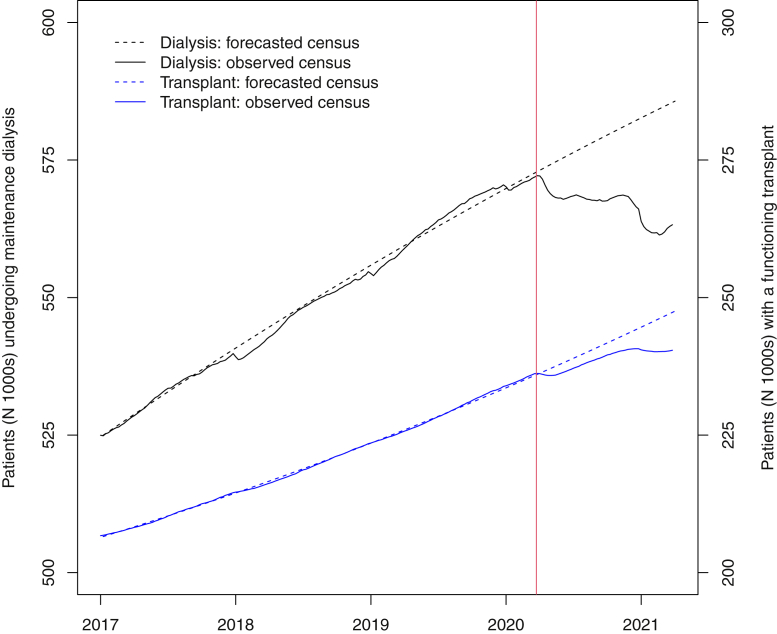
Between week 1 of 2015 and week 13 of 2020, the numbers of dialysis and transplant patients steadily increased, with little deviation from quadratic trends (Figure 1). As of week 13 of 2020, there were 808,354 ESKD patients, comprising 572,157 patients undergoing dialysis and 236,197 patients with a transplant. As of week 13 of 2021, there were 803,661 ESKD patients, representing a year-over-year decline of 0.6% and a “deficit” of 3.5%, relative to the forecast of 833,236 ESKD patients. Among patients undergoing dialysis, the year-over-year decline in census was 1.6%, representing a deficit of 3.8%, relative to forecast. In all dialysis patient subgroups except Asian patients, the census declined (Table 1). The largest deficits, relative to forecast, were observed among patients aged ≥75 years and non-Hispanic White patients. Among patients with a transplant, the census increased 1.8% between week 13 of 2020 and week 13 of 2021, but the census in week 13 of 2021 was nevertheless 2.9% lower than was forecasted. All transplant patient subgroups experienced year-over-year growth, with relatively larger growth in elderly (age ≥65 years), non-Hispanic Black, and Asian patients (Table 1). Still, all subgroups experienced lower growth than was forecasted.
Figure 1.
Forecasted and observed numbers of patients undergoing maintenance dialysis and patients with a functioning transplant in the United States, January 2017 to March 2021. The red vertical line is at March 13, 2020, when a national emergency was declared.
Table 1.
Forecasted and observed numbers of patients undergoing maintenance dialysis and patients with a functioning transplant in the United States during epidemiologic week 13 in each of 2020 and 2021, overall, by age, and by race/ethnicity
| Patients (N) |
Growth (%) 2021 wk13 vs. 2020 wk13 |
Excessa (%) Observed vs. forecasted |
|||
|---|---|---|---|---|---|
| 2020 wk13 Observed |
2021 wk13 Observed |
2021 wk13 Forecasted |
|||
| Maintenance dialysis | |||||
| Overall | 572,157 | 563,237 | 585,705 | –1.6% | –3.8% |
| By age (yr) | |||||
| 18−44 | 150,470 | 104,339 | 106,265 | –1.1% | –1.8% |
| 45−64 | 191,524 | 188,450 | 192,386 | –1.6% | –2.0% |
| 65−74 | 207,743 | 205,032 | 216,253 | –1.3% | –5.2% |
| 75−99 | 67,420 | 65,416 | 70,801 | –3.0% | –7.6% |
| By race/ethnicity | |||||
| NH White | 222,394 | 213,573 | 231,500 | –4.0% | –7.7% |
| NH Black | 184,633 | 181,329 | 184,038 | –1.8% | –1.5% |
| Hispanic | 112,476 | 111,700 | 115,459 | –0.7% | –3.3% |
| Asian | 28,420 | 28,917 | 30,034 | +1.7% | –3.7% |
| Functioning transplant | |||||
| Overall | 236,197 | 240,424 | 247,531 | +1.8% | –2.9% |
| By age (yr) | |||||
| 18−44 | 70,451 | 70,792 | 72,575 | +0.5% | –2.5% |
| 45−64 | 92,126 | 93,140 | 95,848 | +1.1% | –2.8% |
| 65−74 | 67,622 | 70,223 | 72,499 | +3.8% | –3.1% |
| 75−99 | 5,998 | 6,269 | 6,609 | +4.5% | –5.1% |
| By race/ethnicity | |||||
| NH White | 115,724 | 117,185 | 120,191 | +1.3% | –2.5% |
| NH Black | 48,183 | 49,348 | 50,972 | +2.4% | –3.2% |
| Hispanic | 36,029 | 36,700 | 38,576 | +1.9% | –4.9% |
| Asian | 11,742 | 12,308 | 12,740 | +4.8% | –3.4% |
NH, non-Hispanic; wk13, week 13.
During epidemiologic week 13 of 2021.
The President of the United States declared a national emergency on March 13, 2020. During the ensuing year, 3 large waves of COVID-19 swept the United States, resulting in nearly 600,000 deaths due to COVID-19.5 Remarkably, for the first time in history (dating to 1980), the size of the ESKD population in the United States declined, led by a 1.6% decrease in the number of patients on dialysis. Relative to what was forecasted as a function of long-run trends, the numbers of dialysis and transplant patients in week 13 of 2021 were roughly 4% and 3% lower, respectively. These deficits can be attributed to a combination of changes in ESKD incidence, kidney transplant incidence, and mortality risk. The ESKD incidence was likely lower, kidney transplant incidence was somewhat higher (despite a decrease in living donor kidney transplantation),6 and mortality risk was almost certainly higher, regardless of the type of KRT.
Variability in year-over-year changes in patient counts among strata defined by age and race/ethnicity offer a mixed picture. Relative to forecasted counts, larger deficits among elderly patients probably reflect that age is a risk factor for COVID-19 hospitalization and death. A contributing factor may be lower incidence, due to COVID-19 mortality in people with advanced chronic kidney disease (CKD) and decisions to defer dialysis initiation in those who remained alive. With respect to race/ethnicity, the story may be more nuanced. Both Black and Hispanic people have suffered greatly during the pandemic. Acute kidney injury associated with COVID-19 may have accelerated loss of kidney function in patients with CKD,7 thereby placing upward pressure on ESKD incidence and partly countering the downward pressure of COVID-19 mortality on the number of dialysis patients. The precise calculus of how incidence and mortality influenced the size of ESKD population within subgroups remains to be elucidated. Our report is preliminary, with counts subject to minor revisions as late submissions of the End Stage Renal Disease Medical Evidence Report and Death Notification are collected.
We suggest that there are 3 implications of these data. First, recent forecasts of the number of ESKD patients during the 2020s are now invalid. This has direct consequences for outpatient dialysis capacity and corresponding labor needs in the next several years, especially considering the drive toward greater adoption of home dialysis modalities. Second, due to the year-over-year decrease in the number of dialysis patients and an apparent surge in Medicare Advantage enrollment during the past open enrollment period,8 original Medicare (i.e., Parts A and B) is suddenly much less exposed to the total cost of care for dialysis patients. This shift has profound consequences not only for federal entitlement expenditures on ESKD, but also for quality measurement systems that have been built on Parts A and B claims. Third, as the base payment for an outpatient hemodialysis session covered by Part B has increased from $229.63 in 2011 to $239.33 in 2020,9 dialysis providers have relied on steadily increasing treatment volume to address treatment cost inflation. For small and rural dialysis providers, which are more likely to operate with negative margins,10 any decrease in the number of dialysis patients is a potential existential threat to operations, possibly forcing further consolidation among providers.
As the pandemic abates, it is plausible that the ESKD population in the United States will grow again. After all, the US population is aging, thereby placing upward pressure on ESKD incidence. Nevertheless, with essentially static adjusted incidence of ESKD and likely expansion of sodium-glucose cotransporter-2 inhibitor use, it is also possible that the number of dialysis patients in the country is nearing an apex, thus providing an opportunity for the ESKD population to shift away from its long-standing mixture of 70% of patients undergoing dialysis and 30% of patients with a functioning transplant.2 However, the future is admittedly uncertain. Whether the number of people with advanced CKD and high risk of progression to ESKD has declined during the past year is unknown. Even the impact of COVID-19 on outcomes during the upcoming winter is unknown. Continued surveillance will be necessary to guide the nephrology community and policymakers alike.
Disclosure
EDW reports a consulting relationship with Fresenius Medical Care North America, providing input in epidemiologic research about home dialysis; reports being employed by NxStage Medical and Fresenius Medical Care North America (after the acquisition of NxStage Medical) between March 2016 and April 2020; and reports being a scientific advisor or member via the Advisory Board of Home Dialyzors United, and the Board of Directors of the Medical Education Institute; and reports having other interests/relationships on the Scientific Methods Panel for the National Quality Forum. DTG reports having a consulting relationship with Amgen, providing general input in epidemiologic and biostatistical research; reports consultancy agreements with Amgen; and reports receiving research funding from Acadia, Amgen, AstraZeneca, DaVita, Genentech, Gilead, HRSA, Merck, National Institutes of Health, and Opko Renal. JBW reports participation in advisory boards of Aurinia Pharmaceuticals, OPKO Health, and Reata Pharmaceuticals; reports receiving honoraria for academic continuing medical education from Healio and NephSAP; reports consultancy agreements via ad hoc consulting for Bristol Myers Squibb (BMS)-Pfizer Alliance; reports receiving research funding from Amgen, AstraZeneca, BMS/Pfizer, Genentech, Merck, and OPKO Health; reports receiving honoraria from BMS-Pfizer Alliance (for advisory board activities, as noted below); and reports being a scientific advisor or member with BMS-Pfizer Alliance, and occasionally participating on ad hoc advisory boards. KLJ reports participation in the steering committee of Anemia Studies in Chronic Kidney Disease (ASCEND), a clinical trial program evaluating the efficacy and safety of daprodustat and supported by GlaxoSmithKline.
Acknowledgments
The data reported here have been supplied by the United States Renal Data System (USRDS), which is funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) through contract 75N94019C00006. This study was completed by the USRDS Coordinating Center. The originally submitted manuscript was approved by the NIDDK contracting officer representative, Dr. Kevin Abbott. The NIDDK had no role in study design, data collection, analysis, or interpretation, or writing of the report. The USRDS Coordinating Center is located at the Chronic Disease Research Group, a division of the Hennepin Healthcare Research Institute in Minneapolis, Minnesota. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the US Government.
References
- 1.Collins A.J., Foley R.N., Herzog C. US Renal Data System 2010 annual data report. Am J Kidney Dis. 2011;57 doi: 10.1053/j.ajkd.2010.10.007. A8, e1−e526. [DOI] [PubMed] [Google Scholar]
- 2.Johansen K.L., Chertow G.M., Foley R.N. US Renal Data System 2020 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2021;77:A7–A8. doi: 10.1053/j.ajkd.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCullough K.P., Morgenstern H., Saran R. Projecting ESRD incidence and prevalence in the United States through 2030. J Am Soc Nephrol. 2019;30:127–135. doi: 10.1681/ASN.2018050531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weinhandl E.D., Wetmore J.B., Peng Y. Initial effects of COVID-19 on patients with ESKD. J Am Soc Nephrol. 2021;32:1444–1453. doi: 10.1681/ASN.2021010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention COVIDView. 2020. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html Available at:
- 6.Organ Procurement and Transplantation Network National Data. 2021. https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/ Available at:
- 7.Nugent J., Aklilu A., Yamamoto Y. Assessment of acute kidney injury and longitudinal kidney function after hospital discharge among patients with and without COVID-19. JAMA Netw Open. 2021;4:e211095. doi: 10.1001/jamanetworkopen.2021.1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Q1 2021 DaVita Inc. Earnings Conference Call. Denver, CO. 2021. https://pressreleases.davita.com/2021-04-29-DaVita-Inc-1st-Quarter-2021-Results Available at:
- 9.Centers for Medicare & Medicaid Services . Department of Health and Human Services, Centers for Medicare & Medicaid Services; Baltimore, MD: 2020. Medicare program; end-stage renal disease prospective payment system, payment for renal dialysis services furnished to individuals with acute kidney injury, and end-stage renal disease quality incentive program; pp. 71398–71487. [Google Scholar]
- 10.Medicare Payment Advisory Commission March 2021 Report to the Congress: Medicare Payment Policy, Washington, DC. 2021. http://www.medpac.gov/docs/default-source/default-documentlibrary/mar21_medpac_report_to_the_congress_secv2.pdf Available at: