Abstract
Providing the greater public with the current coronavirus (SARS-CoV-2) vaccines is time-consuming and research-intensive; intermediately, some essential ways to reduce the transmission include social distancing, personal hygiene, testing, contact tracing, and universal masking. The data suggests that universal masking, especially using multilayer surgical face masks, offers a powerful efficacy for indoor places. These layers have different functions including antiviral/antibacterial, fluid barrier, particulate and bacterial filtration, and fit and comfort. However, universal masking poses a serious environmental threat since billions of them are disposed on a daily basis; the current coronavirus disease (COVID-19) has put such demands and consequences in perspective. This review focuses on surgical face mask structures and classifications, their impact on our environment, some of their desirable functionalities, and the recent developments around their biodegradability. The authors believe that this review provides an insight into the fabrication and deployment of effective surgical face masks, and it discusses the utilization of multifunctional structures along with biodegradable materials to deal with future demands in a more eco-friendly fashion.
Keywords: COVID-19, Surgical face mask, Biodegradable, Antiviral, Antibacterial, Multifunctional
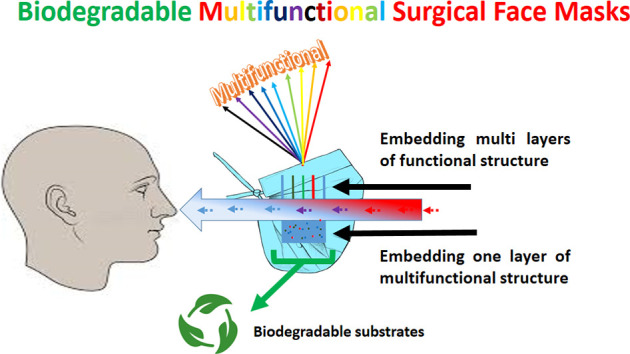
Graphical abstract
1. Introduction
Global concerns caused by the recent respiratory coronavirus disease (COVID-19), urged the widespread use of personal protective equipment (PPE) by people around the globe (Cheng et al., 2020; Cui et al., 2019). These include face masks, gloves, gowns, aprons, hoods, eye-shields, and shoes covers (Cook, 2020; WHO, 2020a), which are currently used by the healthcare workers (HCWs). Among the mentioned PPE for viral respiratory diseases, face masks are useful in controlling the transmission of particulate matters (PMs) (Huang et al., 2020a; Pacitto et al., 2019; Prather et al., 2020).
Transmission of the severe acute respiratory syndrome coronavirus (SARS-CoV-2) is more prominent where there are frequent close contacts, for instance between the HCWs and infected patients. This transmission happens through droplets (>5–10 μm) and bioaerosols (≤5 μm) in the form of PMs (Pivato et al., 2021; Prather et al., 2020). The human-to-human spread of SARS-CoV-2 occurs through direct and indirect pathways (Checchi et al., 2021; Huang et al., 2020a; Prather et al., 2020). Direct pathways include the airborne spread through breathing, talking, sneezing and coughing with different gas flow velocities (1-100 ms-1) (Checchi et al., 2021; Xie et al., 2007). While indirect pathways transmit PMs (fomite) by close contact routes, such as saliva droplets and contact with contaminated surfaces (Huang et al., 2020a; Prather et al., 2020).
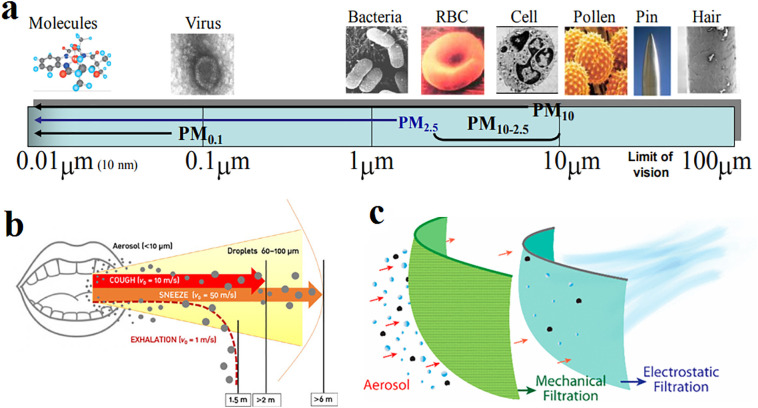
Some of the recommended face masks include surgical face masks, particulate matter surgical face masks (PM1, PM2.5, PM10), and respirators (N95, FFP2 and FFP3) (Oberg and Brosseau, 2008; Tebyetekerwa et al., 2020). The efficacy of these face masks in blocking virus nanoparticles with a size of around 100 nm in diameter (Huang et al., 2020a) is an ongoing topic of research. Fig. 1 depicts the size distribution of PMs, the aerosols spreading pattern during exhalation, and the filtration mechanism in surgical face masks.
Fig. 1.
a) size distribution of PMs (Brook, 2008), b) schematic view of exhalation distances of aerosol and droplets molecules (Checchi et al., 2021) and c) schematic view of aerosols filtration mechanism in common face mask (Konda et al., 2020).
Community-wide masking controls the virus transmission by reducing the trajectory of the above-mentioned aerosolized droplets and infected saliva (Cheng et al., 2020; Rab et al., 2020). In the case of SARS-CoV-2, health organizations report that universal masking is an effective way to protect the greater public (Huang et al., 2020a; Leung et al., 2020; Prather et al., 2020). Previous studies about influenza and Ebola have also shown the significant protection that masking offers to block the transmission of viruses (Brienen et al., 2010; MacIntyre et al., 2014). Sufficient masking and appropriate use guidelines as non-pharmaceutical interventions (NPIs) could have saved many HCWs through breaking the chain of SARS-CoV-2 infection (Rowan and Laffey, 2020). Masking is particularly important in the case of COVID-19, since infected individuals are highly contagious for many days, peaking on or before symptoms occur, leading to wider/uncontrollable spreads. Aside from universal masking, social distancing, personal hygiene, testing (identification & isolation of asymptomatic individuals), and contact tracing are important measures in controlling the spread (Kai et al., 2020; Prather et al., 2020; WHO, 2020a). The high concentration of bioaerosols and droplets in crowded indoor areas such as hospitals, restaurants, airplanes, and workplaces demands higher filtration efficiency structures compare to outdoor areas where there is a constant flow of fresh air (Checchi et al., 2021; Wei and Li, 2016; Xie et al., 2007; Zhou et al., 2018).
Following the above masking guidelines, it is estimated that, only in Asia, over 2.2 billion face masks are used and thrown away every day (Sangkham, 2020); adjusted for the world population, this would be over 3.7 billion masks per day. One study estimated that this would add up to around 66,000 tons of plastic waste per year, only in the United Kingdom (Allison et al., 2020). Assuming that each face mask weighs only 3 g, this would translate to around 4.1 million tons of plastic waste per year globally. A staggering 80% portion of such waste goes into our marine environment, and unfortunately, this waste has already found its way to our water streams (Haque et al., 2021). Disposable surgical face masks are made of synthetic precursors and their wide usage poses a serious threat to our environment (Aragaw, 2020; Fadare and Okoffo, 2020; Silva et al., 2020). On the other hand, such huge demands have resulted in severe face mask shortages in many countries (Ji et al., 2020). Therefore, biodegradability and life cycle analysis (LCA) of surgical face masks are of prime concern.
Some strategies to deal with the environmental and supply-demand challenges include, proper mask-wearing protocols, disinfecting and reusing N95 respirators, use of cloth masks with disposable inserts (CDC, 2020; Dennis et al., 2020), and even mask allocation strategies based on different age ranges and risk levels (Worby and Chang, 2020). On the one hand, face masks are considered disposable since they gradually lose their filtration efficiency (Zhang et al., 2021), and become contaminated hosting sites for virus particles and microorganisms (Zhiqing et al., 2018). On the other hand, up to two-thirds of the filtration efficiency is provided by the embedded electrostatic charges (Kilic et al., 2015; Konda et al., 2020) (see Fig. 1c), which decays significantly over time, based on the using conditions (Konda et al., 2020; Leung and Sun, 2020; Martin and Moyer, 2000). Some studies report that contaminated masks may be disinfected and reused (Dennis et al., 2020; Juang and Tsai, 2020); however, the means for such a process is not accessible to the greater public. As shown in the current COVID-19 pandemic, viruses are among the biggest threats to humanity that can shut down the world. Viruses have also evolved in such a way that they are difficult to kill, and therefore introducing a high-performance surgical face mask is vital.
This review aims to address the mentioned environmental toll by discussing materials options for more eco-friendly face masks, and analyzing additional functionalities, such as antibacterial, antiviral, and self-disinfection characteristics. Using biodegradable precursors along with such multifunctional properties may be a new approach for controlling the pandemic while caring for our planet and people. The present review focuses on the general filtration mechanisms, manufacturing technologies used to make face mask media, characterization of different surgical face mask structures, biodegradable materials that have been used, desired added functionalities, and the future demands for such effective biodegradable multifunctional face masks.
To accomplish the above, our approach was to briefly review the available surgical face masks, their environmental impacts during the COVID-19 pandemic, the materials and processes available to make such structures, and the innovations thereof. In addition, the same was done to understand the scope of available functions in current face masks, and the emerging materials and technologies that have been explored. The intent is not to provide a given solution, but rather provide insight, connect the research community in this field, and spark new ideas to solve these issues together.
2. Filtration materials and process
Air filtration takes place through a combination of different mechanisms including gravitation, straining, inertial impaction, interception, (Brownian) diffusion, intermolecular interaction, and electrostatic interactions. The particle capture capacity of fibrous filtering media depends on the interactions between the PMs, individual fibers, the tortuous filter structure, and the fluid molecules and their kinetic parameters; this is described by the single-fiber particle collection theory (Hinds, 1999; Mao, 2017).
The efficiency of each filtration mechanisms is a function of the particle size (Barhate and Ramakrishna, 2007). Therefore, the size of the target airborne SARS-CoV-2 bioaerosols and microorganisms must be considered while designing the porosity and tortuosity of the filter media (Li et al., 2016). The most penetrating particle size (MPPS) is a characteristic size of around 0.3 μm, where the particles are too large to be captured via diffusion and too small for interception effects (Chuanfang, 2012). The high collection efficiency for particles larger than 1.0 μm is thanks to interception and inertial impaction mechanisms (Chuanfang, 2012; Mao, 2017).
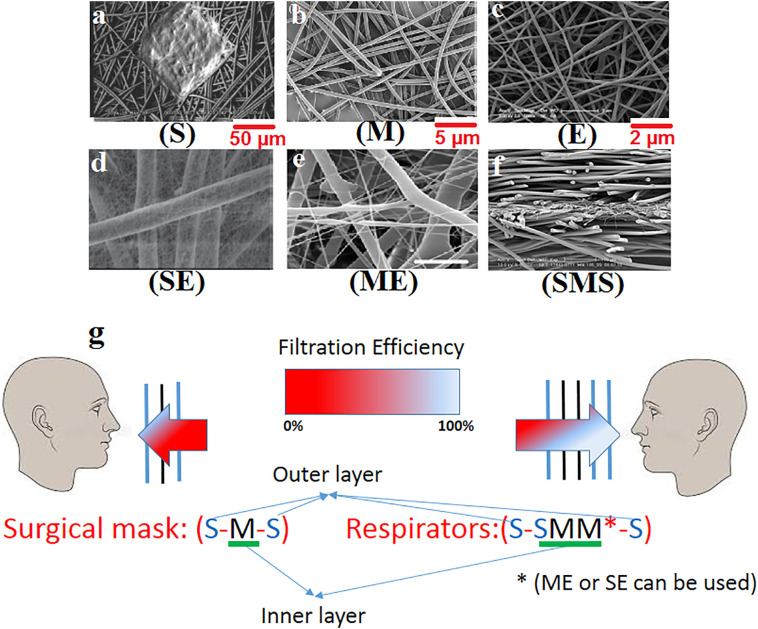
Nonwoven media used in surgical face masks are multilayer structures that are made by processes such as spunbond (S) (Nanjundappa and Bhat, 2005), meltblown (M) (Ellison et al., 2007), electrospun (E) (Desai et al., 2009) and the combinations thereof (Khayan et al., 2021; Lee et al., 2019; Mukhopadhyay, 2014). Some of the common polymers that are used are polyethylene (PE), polypropylene (PP), polyamide (PA), polyethylene terephthalate (PET), polyacrylonitrile (PAN), and polylactic acid (PLA). Electrospun layers are commonly laid over the final substrate such as meltblown (ME) or spunbond (SE) to gain the necessary mechanical properties needed in the final application (Erben et al., 2016).
Composite nonwovens can be used to enhance the mechanical integrity of high efficiency filtering layers through consecutive processes (Amid et al., 2016). Composite structures usually consist of multiple layers, each layer serving a specific performance in the separation/filtration process (Mukhopadhyay, 2014). The most popular combinations of such structures are spunbond–meltblown–spunbond (SMS), spunbond–meltblown–meltblown–spunbond (SMMS), spunbond–meltblown (SM), spunbond–spunbond (SS), spunbond–spunbond–spunbond (SSS), and spunbond–spunbond–meltblown–meltblown–spunbond (SSMMS) in different weight ranges (Ajmeri and Ajmeri, 2011; Chellamani et al., 2013; Zobel and Gries, 2010). Fig. 2a-f show the scanning electron microscopy (SEM) images of spunbond, meltblown, and electrospun nonwovens, along with their combined layers. Some of the other well-known products from these nonwovens include industrial wipes, diapers, oil spill sorbents, feminine hygiene, surgical face masks, respirators, air and liquid filters, and gowns (Ajmeri and Ajmeri, 2011; Mukhopadhyay, 2014; Rasouli et al., 2019). As shown in Fig. 2g, although surgical face masks are made with one filtering layer (S-M—S), respirators contain three filtering layers (S-SMM(E)-S) with higher weights and higher filtration efficiencies. Other composite structures, including SM, SMS, ME, SE can be used in the filtration of PM in nano and micron sizes to meet a high degree of filtration (Mukhopadhyay, 2014; Xiong et al., 2021).
Fig. 2.
SEM images of nonwoven composite structures in surgical face mask applications; the approximate scale bar added for better comparison. a) PP spunbond (S) (Nanjundappa and Bhat, 2005), b) PBT meltblown (M) (Ellison et al., 2007), c) PVA electrospun (E) (Oktay et al., 2014), d) PVA/SAP spunbond-electrospun (SE) (Sivri, 2018), e) PCL meltblown-electrospun (ME) (Erben et al., 2016), and f) Hydroentangled spunbond-meltblown-spunbond (SMS) (Mukhopadhyay, 2014), g) Schematic example of commercial face masks structure: surgical face masks and respirators.
3. Surgical face masks
Surgical face masks are regulated by the food and drug administration (FDA) in the United States of America. The FDA Guidance document has adopted a number of American society for testing and materials (ASTM) standards for establishing the criteria for the classification of masks (Pourdeyhimi, 2020). There are various types of surgical masks available on the market which are used in the current pandemic. Surgical masks and respirators have different structures (see Fig. 2g) and properties which are summarized in Table 1 . Respirators are designed to protect the wearer against hazardous atmosphere (airborne infectious aerosols containing viruses), while surgical face masks mainly protect the public from the infected wearer (Ji et al., 2020; Oberg and Brosseau, 2008). There are two reasons behind the distinctive and superior functionality of respirators over surgical masks: 1) the more efficient filter structure, and 2) the better fit of the respirators (Bowen, 2010; Coia et al., 2013; Junter and Lebrun, 2017). Some models have an exhalation valve that makes exhalation easier and helps reduce the build-up of heat and humidity. Masks with exhalation valves are less efficient in protecting the public from an infected wearer, since the valve does not filter the exhaled contaminated air (Pourdeyhimi, 2020).
Table 1.
Specifications of different face mask structures.
| Face masks | PM's diameter | % particle filtration efficiency | Characteristics and features |
|---|---|---|---|
| i) Surgical mask ii) PM0.1, 2.5, 10 surgical mask ASTM F2100-11 |
<10 μm Large respiratory droplets |
>95 | Loose fitting Three-layer, (S-M—S), flat design pleated and non-pleated Inward leakage Fine and ultrafine dusts Fluid-resistant Physical barrier for droplets Disposable/single use Good breathability |
| Respirator PM0.3 i) aN (P, R) 95, 99, 100 United States standard (NIOSH) ii) bFFP,1,2,3 European standard c(EN149:2001 + A1) |
<0.3 μm (MPPS) High penetrating aerosols |
a95, 99, 99.97 b80, 94, 99 |
Tight fitting (close facial fit) Multi-layer, (S-SMM(E)-S) flat and cone or cup design Sealed (when properly donned and fitted) Most penetrating particle size (MPPS) High performance filtering mask Fluid-resistant Filtration barrier for droplets and aerosols Higher pressure drop With or without valve Discard after each use, but can be used up to 5 times Poor breathability |
N: not oil resistant, R: oil resistant, P: oil proof.
Filtering face pieces.
Face masks filtration efficiency evaluation encompasses three types of tests: (1) particle filtration efficiency (PFE), (2) bacteria filtration efficiency (BFE), and (3) virus filtration efficiency (VFE) (Bayersdorfer et al., 2020; Konda et al., 2020; Leonas et al., 2003; Pragadheeswari et al., 2014). These are reviewed in greater detail in Section 5, but are important to bear in mind when comparing surgical face masks versus respirators.
Face masks consist of multiple layers of filter media which are used as protection devices in respiratory diseases (Mukhopadhyay, 2014; Xiong et al., 2021). The whole structure includes an outer layer (droplet and stain resistant), inner or middle layer(s) (the filtering layer), an outer layer (comfort layer for the skin touch), inner and outer nosepieces (foam and flexible coated aluminum, respectively, to provide better sealing), and headbands/earloops (elastic rubber straps) (Mueller et al., 2018; Oberg and Brosseau, 2008; Tebyetekerwa et al., 2020).
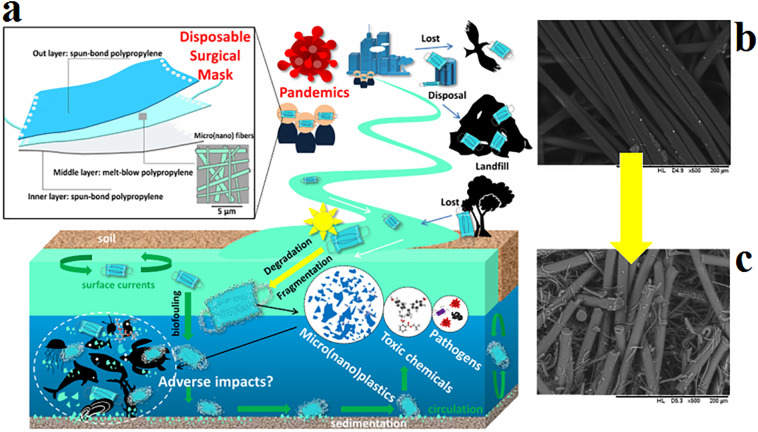
3.1. Environmental aspects
Most of the commercial surgical face masks are made of synthetic precursors and are intended to be disposable (Rubio-Romero et al., 2020). Disposable surgical face masks are manufactured based on conventional synthetic polymers which are sterilized, packaged, and used. They are then disposed of in dumpsites and landfills, and some are just littered in the public, and unfortunately they end up in coastal, marine, and terrestrial environment, causing massive quantities of polymeric wastes (Rubio-Romero et al., 2020; Saberian et al., 2021). Fig. 3a shows the environmental impacts of disposable surgical face masks during the COVID-19 pandemic. The staggering increase in the number of disposable masks being used in universal masking exacerbates the environmental risk connected to improper disposal. Experimental results indicated that a single surgical mask may release up to 173,000 fibers per day into the environment (Saliu et al., 2021). Fig. 3b, c shows the SEM images of surgical face mask taken before and after experimental fragmentation and degradation treatment. The presence of loosely attached micro-/nano-sized plastics on the surface of fragments is clear. Such disposed microplastics can be easily ingested by organisms, such as fish in the aquatic life, affect the food chain, and cause chronic health problems to humans (Aragaw, 2020; Fadare and Okoffo, 2020).
Fig. 3.
a) The potential environmental fates and impacts of disposable surgical masks during COVID-19 (Xu and Ren, 2021), b, c) SEM images of surgical face mask taken before and after application of experimental fragmentation and degradation treatment (Saliu et al., 2021).
Studies show the likelihood that the household wastes that are generated from infected patients may be contaminated by SARS-CoV-2. The infectious waste generated by the surgical face mask during COVID-19 outbreak has posed a major environmental and health concern in many countries. Currently, billions of contaminated face masks, gloves and materials used for diagnosing, detecting, and treating SARS-CoV-2 are already considered as infectious waste. Moreover, while coping with the COVID-19 pandemic, healthcare facilities tend to generate larger amounts of infectious waste; the threat that improper disposal of medical waste could spill over into environmental pollution is palpable and immediate (Sangkham, 2020). Infectious waste streams may serve as routes for viral spreading of the virus, not only to the environment, but also to the operators directly involved in waste management (Nzediegwu and Chang, 2020).
It is therefore worthwhile to develop new ways to decrease and control the waste, introduce biodegradable face masks (Das et al., 2020), and/or introduce alternative waste management processes based on reducing (controlling the overuse and misuse) (Public Health England, 2020), reusing (Jeong et al., 2017; Lee et al., 2019; Liu et al., 2015; Quan et al., 2017; Ullah et al., 2020) and recycling (Achilias et al., 2007; Šišková et al., 2020) scenarios. The overuse of face masks is a form of misuse in itself. On the one hand, such misuse depletes the limited stocks, leads to avoidable shortages, and increases demand for face masks, thus high volumes of wastes (Eckl and Hansch, 2020; Public Health England, 2020). On the other hand, the disposed contaminated face mask is a potential source of biological waste and a means for the community-wide transmission of COVID-19. Multiple studies show the great potential for using biodegradable polymers as substitutes for the traditional materials used in the manufacturing of face masks (Das et al., 2020; Majchrzycka, 2014).
4. Biodegradable aspects of surgical face masks
Although the protective constituents of surgical face masks are durable enough for multiple uses, they are mainly intended for the disposable market. Thus, the environmental impacts of universal making using such disposable media should be considered. The development of reusable or substitute fibrous products based on green and biodegradable precursors can be one of the solutions to alleviate this problem (Das et al., 2020; Desai et al., 2009; Neisiany et al., 2020; C. Wang et al., 2016).
4.1. Biodegradable polymers
Due to environmental reasons, there is a significant interest in moving away from biostable (non-degradable) materials to biodegradable (enzymatically and hydrolytically degradable) materials (especially polymers) for medical applications, e.g., tissue engineering and drug delivery (Nair and Laurencin, 2007). Recent studies show the development of a new generation of synthetic biodegradable polymers and analogous natural polymers for biomedical purposes. The driving force, is the emergence of novel biomedical technologies, e.g., tissue engineering, gene therapy, regenerative medicine, bio-nanotechnology, and controlled drug delivery, which requires biodegradable materials to build a platform (Nair and Laurencin, 2007). Biodegradation of biomaterials (biopolymers) starts with the cleavage of enzymatically or hydrolytically sensitive bonds, leading to a complete erosion in the polymer structure (Nair and Laurencin, 2007). Biodegradable materials decompose through natural biological processes into non-toxic gases, water, and carbonaceous soil over time (Leja and Lewandowicz, 2010).
Based on the degradation mechanisms, biopolymers can be further classified into enzymatically degradable polymers and hydrolytically degradable polymers. Also, biodegradable polymeric materials can be classified into natural and synthetic polymers. Most of the natural biopolymers undergo enzymatic degradation (Nair and Laurencin, 2007). Natural (e.g., chitosan, alginate, collagen, and gelatin) and synthetic (e.g., polyvinyl alcohol (PVA), polyethylene oxide (PEO), polycaprolactone (PCL), and poly-lactic acid (PLA)) polymers are the main polymers for fiber production through technologies like melt-spinning, wet-spinning and/or electrospinning. Natural fibers have better biocompatibility while synthetic fibers benefit from easier processing with better mechanical properties. Some studies have shown the effectiveness of blending strategies for optimum performance as well. Biodegradable polymers can be good raw material candidates for the fabrication of future filtration media such as surgical face masks with a sustainable perspective. The next section describes the biopolymers with applications in face masks and explains their biodegradation aspects.
4.2. Biodegradable face masks
Majority of the PPE fabrics cannot withstand reusing, laundering, or other cleaning methods commonly used for woven and knitted fabrics (Collier, 2010). Different bio-based filtration media use cellulose, protein, chitosan, gelatin, and polylactic acid (PLA), and have been patented and launched as biodegradable surgical face masks in the recent years. Table 2 summarizes the existing and potential filtration media in bio-based surgical face masks. Also, different combinations of biopolymers are used to achieve higher filtration efficiencies and more functionalities, including polylactic acid/polyhydroxybutyrate (PLA/PHB) (Nicosia et al., 2015), Sericin/Poly Vinyl Alcohol (PVA)/Clay (Cloisite 30B) (Purwar et al., 2016), cellulose/poly(ethylenimine) (PEI) (Tiliket et al., 2011), and Ag nanoparticles.
Table 2.
Existing and potential applications of bio-based media in surgical face masks.
| No. | Bio-based media | Structure and materials | Application | Ref. |
|---|---|---|---|---|
| 1 | Protein | Keratin/polyamide 6 nanofiber | Water and air filtration | (Aluigi et al., 2009) |
| Electrospun Sericin nanofibrous mats | Air filtration mask | (Purwar et al., 2016) | ||
| Silk nanofibers | Air filtration mask | (C. Wang et al., 2016) | ||
| Gluten nanofiber | Face mask | (Das et al., 2020) | ||
| Soy protein isolate/polyvinyl alcohol hybrid nanofiber | Air filtration mask | (Fang et al., 2016) | ||
| 2 | Cellulose | Nanomembrane lyocell fibrous | Surgical face mask | (Pragadheeswari et al., 2014) |
| Cellulose non-woven layers | Surgical face mask | (Tiliket et al., 2011) | ||
| Cellulose acetate (CA) nanofibers | Air filtration | (De Almeida et al., 2020) | ||
| 3-ply cotton-PLA-cotton layered | Face mask | (Patil et al., 2021) | ||
| Fungal hyphae and cellulose fibers (Wood and Hemp) | Alternative to synthetic melt and spun-blown materials for PPE | (Filipova et al., 2021) | ||
| Banana stem fiber | Face mask | (Sen et al., 2021) | ||
| Non-woven cellulosic fiber | Face mask | (Catel-Ferreira et al., 2015) | ||
| 3 | Chitosan | Nanofibrous chitosan non-woven | Water and air filtration | (Desai et al., 2009) |
| Chitosan nanowhiskers and poly(butylene succinate)-based microfiber and nanofiber | Face mask filter | (Choi et al., 2021) | ||
| 4 | Poly lactic acid (PLA) | Poly(lactic acid) fibrous membranes | Air filtration | (Z. Wang et al., 2016) |
| 3D printed and electrospun polylactic acid | Face mask filter | (He et al., 2020) | ||
| 5 | Gelatin | Gelatin/β–cyclodextrin composite nanofiber | Respiratory filter | (Kadam et al., 2021) |
| 6 | Polyhydroxyalkanoates (PHAs) | Nano fibroustructure | Face mask | (Al-Hazeem, 2021) |
5. Multifunctional surgical face masks
While the development of multifunctional filter media for face masks is ongoing (Pourdeyhimi, 2020), the existing face masks must fulfil some basic criteria. These include: (1) high filtration efficiency against bioaerosols, (2) fluid barrier properties, (3) low differential pressure (air permeability), (4) ability to kill microorganisms captured in the structure, and (5) excellent wearing properties (comfort, high fit, and minimal leakage) (Barbosa and Graziano, 2006; Majchrzycka, 2014; Pourdeyhimi, 2020; Wang et al., 2018). These basic requirements are vital, since they help reduce the airborne viral concentrations and the transmission of pathogens (bacteria and viruses) in crowded indoor and outdoor communities, protecting us from SARS-CoV-2 (Booth et al., 2013; Chuanfang, 2012; Fadare and Okoffo, 2020; Garibaldi et al., 2019; Prather et al., 2020). The shortage of PPE during the COVID-19 pandemic continues to be severe (WHO, 2020b), and multifunctional face masks may help alleviate this issue.
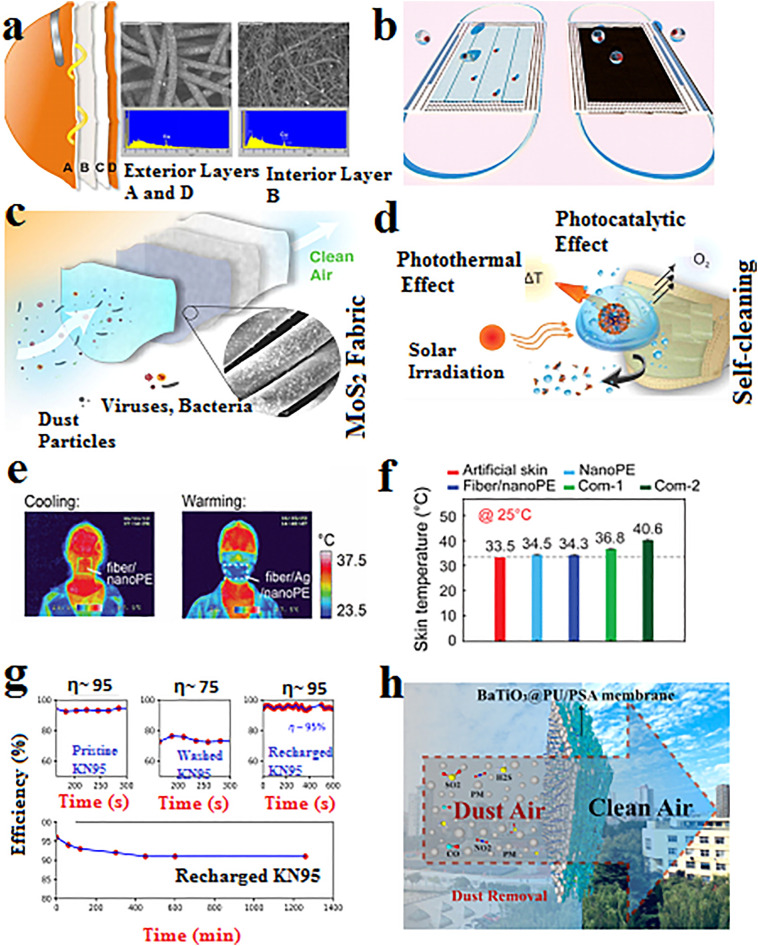
Several high performance multifunctional face masks (including bioaerosols filtration, antibacterial, antiviral) have been developed and patented during the past 15 years. The majority of these products, some of which commercially available, are composite nonwoven structures that are composed of functional materials. Fig. 4 shows the functionalities required for face masks that are effective against respiratory diseases. Some of them are already incorporated in surgical face masks, and the others are needed currently and/or in the near future.
Fig. 4.
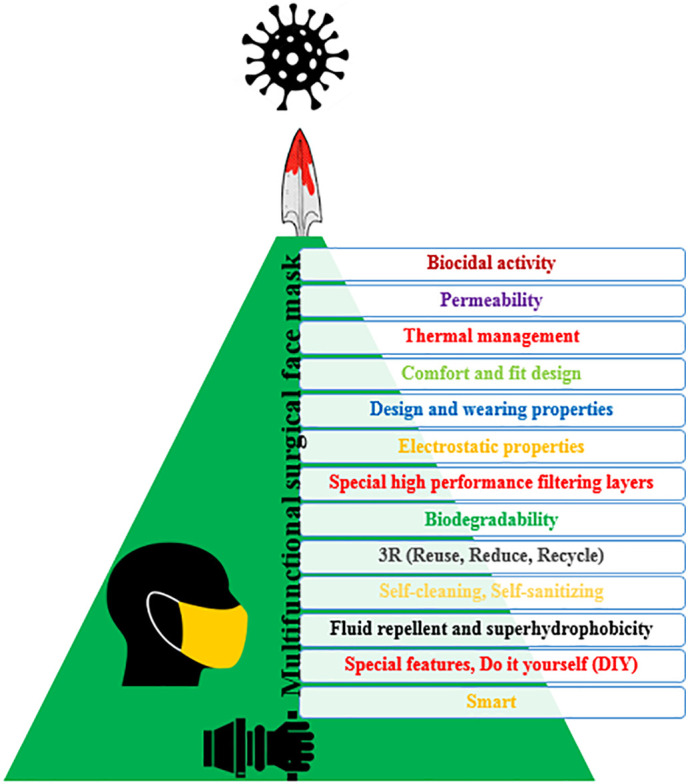
Desired functions of a high performance surgical face mask.
Multifunctional properties can be implemented by embedding (1) a single layer of a multifunctional structure or (2) using multiple layers of functional structures into the conventional surgical face masks. An example of such functional modifications is the application of chemically-bonding materials that filter and sanitize the exhaled bioaerosols (Huang et al., 2020b). Multifunctional PAN nano-fibrous layers containing TiO2 fillers show high PM filtration efficiency, ultraviolet filtration, and antibacterial activities (Chen et al., 2019). Electrospun polyimide/metal-organic framework (MOF) nano-fibrous membranes exhibit superior thermal stability, high mechanical properties, and low pressure drop for efficient PM capture in harsh conditions (Hao et al., 2019). Next section reviews some of these functional face masks in greater detail.
5.1. Antibacterial
The antibacterial activity of surgical face masks has been investigated based on various ranges of pathogens e.g., Escherichia coli, Pseudomonas aeruginosa, Candida albicans, Enterococcus faecalis, and Staphylococcus aureus etc. Majority of these studies have utilized quaternary ammonium (Nicosia et al., 2015; Purwar et al., 2016; Tseng et al., 2016), metals nanoparticles (Hiragond et al., 2018; Li et al., 2006), and N-halamines (Demir et al., 2015; Ren et al., 2018); which are all well-known antibacterial agents that have been used for infection control before. Desirable characteristics of such antibacterial agents include effective inhibition against a broad spectrum of bacteria, non-toxic to the consumer, compatibility with resident skin microbiota, avert from irritations and allergies, and applicable with no adverse effects on the quality or appearance of the surgical face masks.
The reduction percent in bacterial count or BFE is calculated through the ratio of the viable count at a specific period (Li et al., 2006). It is found that the bioburden of surgical face masks increased with wearing duration, making them a potential infection source due to bacterial shedding (Liu et al., 2019). Surgical face masks with the lowest mean pore size have shown the highest BFE against the bacteria (Leonas et al., 2003). Also, antimicrobial electrospun air filtration membranes from PLA and other components (Nicosia et al., 2015; Z. Wang et al., 2016) such as Sericin/PVA/Clay (Purwar et al., 2016) have shown high filtration efficiencies along with the good antimicrobial activity. The BFE of a typical disposable surgical face mask with 95% microbial barrier has shown efficacy reduction just after 4 h of wearing (Barbosa and Graziano, 2006).
5.2. Antiviral
Viruses are responsible for respiratory diseases which can easily escape through filtration systems and cause severe infections (Tiliket et al., 2011). SARS-CoV-2 viral particles are categorized as small bioaerosols with an elliptical or spherical shape and sizes lower than 150 nm (El-Atab et al., 2020). Most of the conventional surgical face masks do not provide the best protection due to their large pore sizes and poor fit characteristics; meanwhile, respirators (e.g., FFP2 or FFP3 and N95) provide efficient protection against airborne viruses (Tiliket et al., 2011). In addition to capturing the droplets and large aerosols by filter media, it is also beneficial to deactivate viruses with antiviral or sanitizing molecules, when they pass through a face mask (Borkow et al., 2010; Huang et al., 2020a; Tiliket et al., 2011). Applying different antiviral agents can provide antiviral performance through direct disinfection, receptor inactivation, and indirect disinfection mechanisms. Some of the reported agents include natural viral inhibitors (Lin et al., 2005, Lin et al., 2014; Yu et al., 2012), metal and metal oxide nanoparticles (Borkow et al., 2010; Galdiero et al., 2011), sodium chloride (Quan et al., 2017), poly(ethylenimine) (PEI) (Tiliket et al., 2011), and polyphenol (Catel-Ferreira et al., 2015).
The ratio of live viruses sampled outside and inside the face masks determines the surgical face masks virus filtration efficiency (VFE) (Booth et al., 2013). Although surgical face masks have been demonstrated to block the spread of viruses, COVID-19 may survive over a day on the surface of the mask (Chin and Poon, 2020). Ideally, the surgical face mask materials should capture and, simultaneously, inactivate those viruses.
5.3. Other functionalities
Although the filtration efficiency of surgical face masks is their primary functionality, more functions makes for a better PPE package in such severe pandemic situations (Lin et al., 2021; Yang et al., 2020; Zhong et al., 2020). Some of the desired functionalities of such surgical face masks are classified and summarized in Table 3 . These functionalities have been developed to increase the filtration performance and the biocidal activity, and to gain a better user experience (air permeability, thermal management, design options). Natural and synthetic materials have been used to incorporate some of these functionalities in surgical face masks. Face masks that contained activated carbon are reported to protect the wearer from vaporized anticancer drug inhalation, thanks to their high adsorptive capacity (Sato et al., 2016). Carbon nanotubes (CNT)-based filters have shown higher biological aerosol PFE versus their total aerosol PFE (Zou and Yao, 2015).
Table 3.
Multifunctional properties of surgical face mask during severe pandemic outbreak (HCWS and people).
| No. | Functionalities | Description (Materials and/or scope of use and effects) |
Ref. |
|---|---|---|---|
| 1 | Biocidal activity (antibacterial, antiviral) | Increase the protection efficiency against respiratory diseases outbreak, effective antiviral and antibacterial mask. Quaternary ammonium, clay |
(Nicosia et al., 2015; Purwar et al., 2016; Tseng et al., 2016) |
| Nanostructures (CuO, Ag, Ag/TiO2, PLA/TiO2) | (Borkow et al., 2010; Hiragond et al., 2018; Li et al., 2006; Z. Wang et al., 2016) | ||
| Chitosan | (Desai et al., 2009) | ||
| N-halamine | (Demir et al., 2015; Ren et al., 2018) | ||
| Polyphenol (Catechin) | (Catel-Ferreira et al., 2015) | ||
| Salts (NaCl) | (Quan et al., 2017) | ||
| Poly (ethylenimine) (PEI) | (Tiliket et al., 2011) | ||
| Natural viral inhibitors (Isatis Indigotica) | (Lin et al., 2005) | ||
| 2 | Permeability (air, water vapor) | Increases the breathing and comfort properties, especially for people with asthma. Increases the inhaling rate and blood oxygen level. Reduces mask-induced hypercapnia. |
(Lee et al., 2020; Li and Gong, 2015; Zou and Yao, 2015) |
| 3 | Design and wearing properties (thermal and comfort properties, fit design) | Allows for longer comfortable wearing time and thermal management of exhalation by using thermally conductive materials. Well-designed face mask to improve filtration efficiency with lower leakage, comfort properties and ease of the donning and doffing process. Absorb the sweat in the vapor form without transforming into liquid (using superabsorbent polymer). |
(Garibaldi et al., 2019; He et al., 2020; Lee et al., 2020; Sivri, 2018; Swennen et al., 2020; Yang et al., 2017) |
| 4 | Electrostatic properties | Recharging and rejuvenation of used or disinfected surgical face masks, increasing the effective use time of disposable face mask. | (Hossain et al., 2020; Wang et al., 2020) |
| 5 | Special high performance filtering layers | Increases the filtration efficiency (nanofiber, hollow fiber, carbon nanotubes, activated carbon, graphene). | (Khayan et al., 2021; Lin et al., 2021; Sato et al., 2016; Zou and Yao, 2015) |
| 6 | Biodegradability | Eco-friendly face mask | See Table 3 |
| 7 | 3R (reuse, reduce, recycle) | Reducing through extended mask service time. Reusing through easy disinfection or recharging procedure. Recycling through enhanced disposal procedure and management. |
(El-Atab et al., 2020; Kumar et al., 2021, Kumar et al., 2020; Lee et al., 2020; Lin et al., 2021; Wang et al., 2020; Yang et al., 2020; Zhong et al., 2020) |
| 8 | Self-cleaning Self-disinfecting Self-sanitizing Self-decontaminating |
Photo-sterilize, thermal-sterilize Applying photo (UV) or thermal disinfecting procedure to introduce self-sterilization and enable reusability. |
(Banerjee et al., 2021; Kumar et al., 2021, Kumar et al., 2020; Lin et al., 2021; Zhong et al., 2020) |
| 9 | Fluid repellent and superhydrophobicity | Increases the effective use time in different conditions specially for HCWs (anti-splash, …) | (El-Atab et al., 2020; Lin et al., 2021; Zhong et al., 2020) |
| 10 | Special features (smart) | Uses special materials or designs to increase the performance and appearance of face masks. The transparent look can help avoid the threatening appearance of the mask and can allow lip reading for people with mutism or hearing impairment. Do it yourself (DIY) face mask with changeable layers. |
(Cheng et al., 2017; He et al., 2020; Sarkar et al., 2020; Yang et al., 2020) |
Graphical results of some studies on multifunctional structures for face masks are shown in Fig. 5 . As shown, the hydrophobic hybrid filter structure allows for antibacterial/antiviral properties. Also, with the integration of photo-thermal treatment the created heat currents can efficiently self-disinfect the face masks (Fig. 5a, b, c, d).
Fig. 5.
Multifunctional surgical face masks. a) Anti-influenza multilayer containing copper oxide face masks with corresponding SEM and XPS analysis (Borkow et al., 2010), b) reusable and recyclable graphene-coated superhydrophobic, self-cleaning and photothermal face masks (Zhong et al., 2020), c) reusable MoS2-modified durable antibacterial and photothermal self-disinfection face masks (Kumar et al., 2021), d) reusable copper nanoparticles (CuNPs) antiviral and photo-thermal self-disinfecting face masks (Kumar et al., 2020), e) multifunctional face masks to protect people from PM pollutants and simultaneously achieve personal thermal comfort (Yang et al., 2017), f) skin temperature when covered with multifunctional face masks and two commercial face masks (Yang et al., 2017), g) filtration efficiency of a new KN95 mask, washed and dried mask, and recharged mask for 60 min. Decay of the efficiency of the recharged mask over the course of a day (Hossain et al., 2020), h) multifunctional mask by using BaTiO3@PU/PSA membrane achieved the high capture efficiency, low pressure drop, good mechanical property, sufficient flexibility, high thermal stability, favorable flame-retardancy as well as superior chemical resistance against acid and alkali (Yang et al., 2020).
Surgical face masks comfort characteristics call for optimal liquid absorption capacities, air and water vapor permeability, design, and wearing properties especially for people with breathing issues (Lee et al., 2020; Sivri, 2018; Yang et al., 2017). Face masks comfort and performance depend on various parameters such as the nature of the textile, fiber diameter, special surface treatments and finishes, fitting performance, microclimate, number of layers or thickness (Lee et al., 2020; Sivri, 2018), and their composition (such as the presence of high surface area activated carbons) (Konda et al., 2020). Increasing the absorption capacity of such face masks can further enhance their comfort by absorbing the sweat in the vapor form without transforming it into liquid (Sivri, 2018). Some nanofiber filter structures, and custom-made 3D printed filters and respirators have been developed to increase the comfort and design fit to increase the wearing time (He et al., 2020; Li and Gong, 2015; Swennen et al., 2020). Filter modification through electroless-plating of Ag enabled high filtration efficiency, low pressure drop, and excellent radiative cooling properties in hot conditions; where cooling effect was achieved by reflecting most of the human body radiation (Yang et al., 2017). It has been reported that wearing face masks in hot and humid conditions increases heat stress, sweating, and can even act as breeding sites for microorganisms (Yang et al., 2017) (Fig. 5e, f).
There are several reports about the fabrication of novel electret filter structures in combination with bulky and open structures that allows for recharging and rejuvenating after disinfection (Hossain et al., 2020; Wang et al., 2020) (Fig. 5g). These structures use different polymeric materials to deliver high porosity and high filtration efficiencies without increasing the differential pressure (Fedorova and Pourdeyhimi, 2007; Quan et al., 2017). These structures are highly breathable, and the thermal comfort filter layers consist of electret polyethersulfone/barium titanate nano-fibrous membrane (PES/BaTiO3 NFM) and polysulfonamide/polyacrylonitrile-boehmite (PSA/PAN-B) composites (Neisiany et al., 2020; Yu et al., 2012). Also, smart facial masks have been developed, where the electrospun polyether imide (PEI) electret nonwoven provides dual functionalities (Cheng et al., 2017). It has been reported that a combination of various commonly available fabrics used in cloth masks can potentially provide significant protection against the transmission of aerosol particles by mechanical and electrostatic filtering (Konda et al., 2020). New barium titanate@polyurethane/polysulfonamide (BaTiO3@PU/PSA) composite nano-fibrous membranes have also shown good mechanical properties, favorable flame-retardancy, and sufficient flexibility (Yang et al., 2020) (Fig. 5h). Reusable polybenzimidazole nanofiber membranes are also reported to be suitable filters with high breathability and PM dust capture (Lee et al., 2019).
6. Future perspectives and possible challenges
Surgical face masks that incorporate new functionalities, along with their efficient PFE, can provide high performance PPE to protect the people in severe conditions. Due to the high consumption rate of surgical face masks and the severe pandemic, it is needed to design and produce special bio-based structures. In the case of COVID-19, encapsulated systems can be incorporated into the filtering layer to provide a means for in-situ disinfection and drug delivery. This may help treat the infected wearers as they breathe through such special smart face masks.
Currently, surgical face masks are creating massive amounts of biological wastes that may cause irreversible impacts on our environment; this makes the fully biodegradable and self-sanitizing masks an interesting subject for future investigations. Bio-nanomaterial finishing (or coatings) is one way to impart biodegradability in surgical face masks. Biodegradable, reusable, and antivirus masks have gotten special attention as a sustainable solution to alleviate the current shortage. Besides filtering and blocking the inhaled aerosols, chemical deactivation of droplets with antiviral, antibacterial or sanitizing molecules, as they pass through the fibrous layers, is another sought-after characteristic in face masks. These molecules need to be released in moisturized and warm air during exhalation, but can stay fixed on the mask surface during the inhalation of dry and cold air.
Regarding the exhaled aerosols, it is also useful to engineer non-toxic durable self-sanitizing surfaces that can slowly release disinfecting chemicals to mitigate fomite transmission. Fomite contamination is a well-known problem that is currently solved with chemical and physical sanitization e.g., wiping or through spraying. It is difficult to trace fomite transmission, but it is common for many respiratory diseases (Huang et al., 2020a). Furthermore, patterned surfaces can avoid capillary condensation of water, which can bring additional self-desiccation properties to deactivate viruses (Huang et al., 2020a). Therefore, multifunctional PPE suits have been developed and reported where they take advantage of smart devices e.g., wireless communication capabilities, actuators and microsensors for detecting viruses, temperature and humidity setting, and monitoring physiological conditions without a protective function (Huang et al., 2020a). Taking advantage of such smart technologies, face masks could change color if the wearer's body temperature rises above the certain level associated with the current pandemic.
After all, the appearance of surgical face masks is another interesting topic that may increase people's tendency to wear them. The possible challenges for introducing biodegradable multifunctional surgical face masks include: the limited sources in supplying bio-based substrate for such a huge consumption, the price of the final face mask to be affordable as in universal masking, the toxicity of the different high performance materials, large-scale manufacturability, and also the durability of such effective materials on a surgical face mask. In a future perspective, these issues should be addressed to develop non-toxic and high performance durable biodegradable multifunctional surgical face masks.
7. Conclusions
In the recent century, presence of bacteria and viruses in respiratory aerosols has played an important role in diseases transmission, especially with the COVID-19 global pandemic. Face masks (surgical face masks and respirators) have been used globally to protect both healthcare providers and patients in the recent pandemic. This has resulted in more than four million tons of plastic waste on a daily basis. Using biodegradable polymers in surgical face mask production can significantly help protect both the people and our environment at the same time. This paper has reviewed the viable biodegradable materials options, along with their respective processing requirements and their final performance. In addition, it is discussed that high-efficiency face masks can be further functionalized to incorporate other values and benefits beyond biodegradability, including temperature/health monitoring, antibacterial, antiviral, self-sanitizing properties, and fit and comfort. Each of these functionalities has been reviewed and potential materials, technologies, and protocols available to the industry and public have been proposed. While this review provides a broad perspective on the current status of multifunctional and biodegradable nonwoven face masks, it also sheds light on some of the current challenges and the future opportunities.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to thank Ms. Derakhshan Radbareh for English editing of the paper. Also, they acknowledge respected reviewers and the editor for their valuable comments.
Editor: Jay Gan
References
- Achilias D., Roupakias C., Megalokonomos P., Lappas A., Antonakou ?. Chemical recycling of plastic wastes made from polyethylene (LDPE and HDPE) and polypropylene (PP) J. Hazard. Mater. 2007;149:536–542. doi: 10.1016/j.jhazmat.2007.06.076. [DOI] [PubMed] [Google Scholar]
- Ajmeri J., Ajmeri C.J. Handbook of Medical Textiles. Elsevier; 2011. Nonwoven materials and technologies for medical applications; pp. 106–131. [Google Scholar]
- Al-Hazeem N. Manufacture of fibroustructure facemask to protect against coronavirus using electrospinning. Medico Res. Chron. 2021;8:103–110. [Google Scholar]
- Allison A.L., Ambrose-Dempster E., Aparsi T.D., Bawn M., Casas Arredondo M., Chau C., Chandler K., Dobrijevic D., Hailes H., Lettieri P. 2020. The Environmental Dangers of Employing Single-use Face Masks as Part of a COVID-19 Exit Strategy. [Google Scholar]
- Aluigi A., Vineis C., Tonin C., Tonetti C., Varesano A., Mazzuchetti G. Wool keratin-based nanofibres for active filtration of air and water. J. Biobased Mater. Bioenergy. 2009;3:311–319. [Google Scholar]
- Amid H., Mazé B., Flickinger M.C., Pourdeyhimi B. Hybrid adsorbent nonwoven structures: a review of current technologies. J. Mater. Sci. 2016;51:4173–4200. [Google Scholar]
- Aragaw T.A. Surgical face masks as a potential source for microplastic pollution in the COVID-19 scenario. Mar. Pollut. Bull. 2020;159 doi: 10.1016/j.marpolbul.2020.111517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee R., Roy P., Das S., Paul M.K. A hybrid model integrating warm heat and ultraviolet germicidal irradiation might efficiently disinfect respirators and personal protective equipment. Am. J. Infect. Control. 2021;49:309–318. doi: 10.1016/j.ajic.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbosa M.H., Graziano K.U. Influence of wearing time on efficacy of disposable surgical masks as microbial barrier. Braz. J. Microbiol. 2006;37:216–217. [Google Scholar]
- Barhate R.S., Ramakrishna S. Nanofibrous filtering media: filtration problems and solutions from tiny materials. J. Membr. Sci. 2007;296:1–8. [Google Scholar]
- Bayersdorfer J., Giboney S., Martin R., Moore A., Bartles R. Novel manufacturing of simple masks in response to international shortages: bacterial and particulate filtration efficiency testing. Am. J. Infect. Control. 2020;48:1543–1545. doi: 10.1016/j.ajic.2020.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth C.M., Clayton M., Crook B., Gawn J. Effectiveness of surgical masks against influenza bioaerosols. J. Hosp. Infect. 2013;84:22–26. doi: 10.1016/j.jhin.2013.02.007. [DOI] [PubMed] [Google Scholar]
- Borkow G., Zhou S.S., Page T., Gabbay J. A novel anti-influenza copper oxide containing respiratory face mask. PloS One. 2010;5 doi: 10.1371/journal.pone.0011295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen L.E. Does that face mask really protect you? Appl. Biosaf. 2010;15:67–71. [Google Scholar]
- Brienen N.C., Timen A., Wallinga J., Van Steenbergen J.E., Teunis P.F. The effect of mask use on the spread of influenza during a pandemic. Risk Anal. Int. J. 2010;30:1210–1218. doi: 10.1111/j.1539-6924.2010.01428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook R.D. Cardiovascular effects of air pollution. Clin. Sci. 2008;115:175–187. doi: 10.1042/CS20070444. [DOI] [PubMed] [Google Scholar]
- Catel-Ferreira M., Tnani H., Hellio C., Cosette P., Lebrun L. Antiviral effects of polyphenols: development of bio-based cleaning wipes and filters. J. Virol. Methods. 2015;212:1–7. doi: 10.1016/j.jviromet.2014.10.008. [DOI] [PubMed] [Google Scholar]
- CDC Implementing filtering facepiece respirator (FFR) reuse, including reuse after decontamination, when there are known shortages of N95 respirators. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html
- Checchi V., Bellini P., Bencivenni D., Consolo U. COVID-19 dentistry-related aspects: a literature overview. Int. Dent. J. 2021;71:21–26. doi: 10.1111/idj.12601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chellamani K., Veerasubramanian D., Balaji R.V. Surgical face masks: manufacturing methods and classification. J. Acad. Ind. Res. 2013;2:320–324. [Google Scholar]
- Chen K.-N., Sari F.N.I., Ting J.-M. Multifunctional TiO2/polyacrylonitrile nanofibers for high efficiency PM2.5 capture, UV filter, and anti-bacteria activity. Appl. Surf. Sci. 2019;493:157–164. [Google Scholar]
- Cheng Y., Wang C., Zhong J., Lin S., Xiao Y., Zhong Q., Jiang H., Wu N., Li W., Chen S. Electrospun polyetherimide electret nonwoven for bi-functional smart face mask. Nano Energy. 2017;34:562–569. [Google Scholar]
- Cheng V.C.-C., Wong S.-C., Chuang V.W.-M., So S.Y.-C., Chen J.H.-K., Sridhar S., To K.K.-W., Chan J.F.-W., Hung I.F.-N., Ho P.-L. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020;81:107–114. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin A.W., Poon L.L. Stability of SARS-CoV-2 in different environmental conditions–authors’ reply. Lancet Microbe. 2020;1 doi: 10.1016/S2666-5247(20)30095-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi S., Jeon H., Jang M., Kim H., Shin G., Koo J.M., Lee M., Sung H.K., Eom Y., Yang H. Biodegradable, efficient, and breathable multi‐use face mask filter. Adv. Sci. 2021;8 doi: 10.1002/advs.202003155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuanfang Y. Aerosol filtration application using fibrous media—an industrial perspective. Chin. J. Chem. Eng. 2012;20:1–9. doi: 10.1016/S1004-9541(12)60356-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coia J.E., Ritchie L., Adisesh A., Booth C.M., Bradley C., Bunyan D., Carson G., Fry C., Hoffman P., Jenkins D., Phin N., Taylor B., Nguyen-Van-Tam J.S., Zuckerman M. Guidance on the use of respiratory and facial protection equipment. J. Hosp. Infect. 2013;85:170–182. doi: 10.1016/j.jhin.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collier B. Applications of Nonwovens in Technical Textiles. Elsevier; 2010. Nonwovens in specialist and consumer apparel; pp. 120–135. [Google Scholar]
- Cook T. Personal protective equipment during the coronavirus disease (COVID) 2019 pandemic–a narrative review. Anaesthesia. 2020;75:920–927. doi: 10.1111/anae.15071. [DOI] [PubMed] [Google Scholar]
- Cui J., Li F., Shi Z.-L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019;17:181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das O., Neisiany R.E., Capezza A.J., Hedenqvist M.S., Försth M., Xu Q., Jiang L., Ji D., Ramakrishna S. The need for fully bio-based facemasks to counter coronavirus outbreaks: a perspective. Sci. Total Environ. 2020;736 doi: 10.1016/j.scitotenv.2020.139611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Almeida D.S., Martins L.D., Muniz E.C., Rudke A.P., Squizzato R., Beal A., de Souza P.R., Bonfim D.P.F., Aguiar M.L., Gimenes M.L. Biodegradable CA/CPB electrospun nanofibers for efficient retention of airborne nanoparticles. Process. Saf. Environ. Prot. 2020;144:177–185. doi: 10.1016/j.psep.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demir B., Cerkez I., Worley S., Broughton R., Huang T.-S. N-halamine-modified antimicrobial polypropylene nonwoven fabrics for use against airborne bacteria. ACS Appl. Mater. Interfaces. 2015;7:1752–1757. doi: 10.1021/am507329m. [DOI] [PubMed] [Google Scholar]
- Dennis R., Pourdeyhimi B., Cashion A., Emanuel S., Hubbard D. Durability of disposable N95 mask material when exposed to improvised ozone gas disinfection. J. Sci. Med. 2020;2 [Google Scholar]
- Desai K., Kit K., Li J., Davidson P.M., Zivanovic S., Meyer H. Nanofibrous chitosan non-wovens for filtration applications. Polymer. 2009;50:3661–3669. [Google Scholar]
- Eckl L., Hansch S. Gender-and age-related differences in misuse of face masks in COVID-19 prevention in central European cities. medRxiv. 2020:1–6. doi: 10.1101/2020.11.11.20224030. November 08. [DOI] [Google Scholar]
- El-Atab N., Qaiser N., Badghaish H., Shaikh S.F., Hussain M.M. Flexible nanoporous template for the design and development of reusable anti-COVID-19 hydrophobic face masks. ACS Nano. 2020;14:7659–7665. doi: 10.1021/acsnano.0c03976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellison C.J., Phatak A., Giles D.W., Macosko C.W., Bates F.S. Melt blown nanofibers: fiber diameter distributions and onset of fiber breakup. Polymer. 2007;48:3306–3316. [Google Scholar]
- Erben J., Jencova V., Chvojka J., Blazkova L., Strnadova K., Modrak M., Kostakova E.K. The combination of meltblown technology and electrospinning–The influence of the ratio of micro and nanofibers on cell viability. Mater. Lett. 2016;173:153–157. [Google Scholar]
- European Committee for Standardization (CEN) 2009. EN 149:2001+A1:2009: Respiratory Protective Devices. Filtering Half Masks to Protect Against Particles. Requirements, Testing, Marking. May 2009. [Google Scholar]
- Fadare O.O., Okoffo E.D. Covid-19 face masks: a potential source of microplastic fibers in the environment. Sci. Total Environ. 2020;737 doi: 10.1016/j.scitotenv.2020.140279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang Q., Zhu M., Yu S., Sui G., Yang X. Studies on soy protein isolate/polyvinyl alcohol hybrid nanofiber membranes as multi-functional eco-friendly filtration materials. Mater. Sci. Eng. B. 2016;214:1–10. doi: 10.1016/j.mseb.2016.08.004. [DOI] [Google Scholar]
- Fedorova N., Pourdeyhimi B. High strength nylon micro-and nanofiber based nonwovens via spunbonding. J. Appl. Polym. Sci. 2007;104:3434–3442. [Google Scholar]
- Filipova I., Irbe I., Spade M., Skute M., Dāboliņa I., Baltiņa I., Vecbiskena L. Mechanical and air permeability performance of novel biobased materials from fungal hyphae and cellulose fibers. Materials. 2021;14:136. doi: 10.3390/ma14010136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galdiero S., Falanga A., Vitiello M., Cantisani M., Marra V., Galdiero M. Silver nanoparticles as potential antiviral agents. Molecules. 2011;16:8894–8918. doi: 10.3390/molecules16108894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garibaldi B.T., Ruparelia C., Shaw-Saliba K., Sauer L.M., Maragakis L.L., Glancey M., Subah M., Nelson A.R., Wilkason C., Scavo L. A novel personal protective equipment coverall was rated higher than standard ebola virus personal protective equipment in terms of comfort, mobility and perception of safety when tested by health care workers in Liberia and in a United States biocontainment unit. Am. J. Infect. Control. 2019;47:298–304. doi: 10.1016/j.ajic.2018.08.014. [DOI] [PubMed] [Google Scholar]
- Hao Z., Wu J., Wang C., Liu J. Electrospun polyimide/metal-organic framework nanofibrous membrane with superior thermal stability for efficient PM2.5 capture. ACS Appl. Mater. Interfaces. 2019;11:11904–11909. doi: 10.1021/acsami.8b22415. [DOI] [PubMed] [Google Scholar]
- Haque M.S., Sharif S., Masnoon A., Rashid E. SARS-CoV-2 pandemic-induced PPE and single-use plastic waste generation scenario. Waste Manag. Res. 2021;39:3–17. doi: 10.1177/0734242X20980828. [DOI] [PubMed] [Google Scholar]
- He H., Gao M., Illés B., Molnar K. 3D printed and electrospun, transparent, hierarchical polylactic acid mask nanoporous filter. Int. J. Bioprinting. 2020;6 doi: 10.18063/ijb.v6i4.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds W.C. 2nd Ed. Y. John Wiley Sons Press N; 1999. pp. 182–204. (Properties, behavior, and measurement of airborne particles. Aerosol Technol). [Google Scholar]
- Hiragond C.B., Kshirsagar A.S., Dhapte V.V., Khanna T., Joshi P., More P.V. Enhanced anti-microbial response of commercial face mask using colloidal silver nanoparticles. Vacuum. 2018;156:475–482. [Google Scholar]
- Hossain E., Bhadra S., Jain H., Das S., Bhattacharya A., Ghosh S., Levine D. Recharging and rejuvenation of decontaminated N95 masks. Phys. Fluids. 2020;32 doi: 10.1063/5.0023940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang H., Fan C., Li M., Nie H.-L., Wang F.-B., Wang H., Wang R., Xia J., Zheng X., Zuo X. COVID-19: a call for physical scientists and engineers. ACS Nano. 2020;14:3747–3754. doi: 10.1021/acsnano.0c02618. [DOI] [PubMed] [Google Scholar]
- Huang H., Park H., Liu Y., Huang J. On-mask chemical modulation of respiratory droplets. Matter. 2020;3:1791–1810. doi: 10.1016/j.matt.2020.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong S., Cho H., Han S., Won P., Lee H., Hong S., Yeo J., Kwon J., Ko S.H. High efficiency, transparent, reusable, and active PM2.5 filters by hierarchical ag nanowire percolation network. Nano Lett. 2017;17:4339–4346. doi: 10.1021/acs.nanolett.7b01404. [DOI] [PubMed] [Google Scholar]
- Ji D., Fan L., Li X., Ramakrishna S. Addressing the worldwide shortages of face masks. BMC Mater. 2020;2:1–11. doi: 10.1186/s42833-020-00015-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juang P.S., Tsai P. N95 respirator cleaning and reuse methods proposed by the inventor of the N95 mask material. J. Emerg. Med. 2020;58:817–820. doi: 10.1016/j.jemermed.2020.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junter G.-A., Lebrun L. Cellulose-based virus-retentive filters: a review. Rev. Environ. Sci. Biotechnol. 2017;16:455–489. doi: 10.1007/s11157-017-9434-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadam V., Truong Y.B., Schutz J., Kyratzis I.L., Padhye R., Wang L. Gelatin/β–cyclodextrin bio–nanofibers as respiratory filter media for filtration of aerosols and volatile organic compounds at low air resistance. J. Hazard. Mater. 2021;403 doi: 10.1016/j.jhazmat.2020.123841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kai D., Goldstein G.-P., Morgunov A., Nangalia V., Rotkirch A. Universal masking is urgent in the covid-19 pandemic: Seir and agent based models, empirical validation, policy recommendations. ArXiv Prepr. 2020;ArXiv200413553 1:1–19. [Google Scholar]
- Khayan K., Anwar T., Wardoyo S., Puspita W.L. Respiratory mask using a combination of spunbond, meltblown, and activated carbon materials for reducing exposure to CO: an in vivo study. Environ. Sci. Pollut. Res. 2021;28:18989–18994. doi: 10.1007/s11356-020-09476-8. [DOI] [PubMed] [Google Scholar]
- Kilic A., Shim E., Pourdeyhimi B. Electrostatic capture efficiency enhancement of polypropylene electret filters with barium titanate. Aerosol Sci. Technol. 2015;49:666–673. doi: 10.1080/02786826.2015.1061649. [DOI] [Google Scholar]
- Konda A., Prakash A., Moss G.A., Schmoldt M., Grant G.D., Guha S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano. 2020;14:6339–6347. doi: 10.1021/acsnano.0c03252. [DOI] [PubMed] [Google Scholar]
- Kumar S., Karmacharya M., Joshi S.R., Gulenko O., Park J., Kim G.-H., Cho Y.-K. Photoactive antiviral face mask with self-sterilization and reusability. Nano Lett. 2020;21:337–343. doi: 10.1021/acs.nanolett.0c03725. [DOI] [PubMed] [Google Scholar]
- Kumar P., Roy S., Sarkar A., Jaiswal A. Reusable MoS2-modified antibacterial fabrics with photothermal disinfection properties for repurposing of personal protective masks. ACS Appl. Mater. Interfaces. 2021;13:12912–12927. doi: 10.1021/acsami.1c00083. [DOI] [PubMed] [Google Scholar]
- Lee S., Cho A.R., Park D., Kim J.K., Han K.S., Yoon I.-J., Lee M.H., Nah J. Reusable polybenzimidazole nanofiber membrane filter for highly breathable PM2. 5 dust proof mask. ACS Appl. Mater. Interfaces. 2019;11:2750–2757. doi: 10.1021/acsami.8b19741. [DOI] [PubMed] [Google Scholar]
- Lee K.-P., Yip J., Kan C.-W., Chiou J.-C., Yung K.-F. Reusable face masks as alternative for disposable medical masks: factors that affect their wear-comfort. Int. J. Environ. Res. Public Health. 2020;17:6623. doi: 10.3390/ijerph17186623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leja K., Lewandowicz G. Polymer biodegradation and biodegradable polymers-a review. Pol. J. Environ. Stud. 2010;19:255–266. [Google Scholar]
- Leonas K.K., Jones C.R., Hall D. The relationship of fabric properties and bacterial filtration efficiency for selected surgical face masks. JTATM. 2003;3:1–8. [Google Scholar]
- Leung W.W.F., Sun Q. Electrostatic charged nanofiber filter for filtering airborne novel coronavirus (COVID-19) and nano-aerosols. Sep. Purif. Technol. 2020;250 doi: 10.1016/j.seppur.2020.116886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung N.H.L., Chu D.K.W., Shiu E.Y.C., Chan K.-H., McDevitt J.J., Hau B.J.P., Yen H.-L., Li Y., Ip D.K.M., Peiris J.S.M., Seto W.-H., Leung G.M., Milton D.K., Cowling B.J. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Gong Y. Design of polymeric nanofiber gauze mask to prevent inhaling PM2.5 particles from haze pollution. J. Chem. 2015:460392. doi: 10.1155/2015/460392. [DOI] [Google Scholar]
- Li Y., Leung P., Yao L., Song Q., Newton E. Antimicrobial effect of surgical masks coated with nanoparticles. J. Hosp. Infect. 2006;62:58–63. doi: 10.1016/j.jhin.2005.04.015. [DOI] [PubMed] [Google Scholar]
- Li Q., Xu Y., Wei H., Wang X. An electrospun polycarbonate nanofibrous membrane for high efficiency particulate matter filtration. RSC Adv. 2016;6:65275–65281. [Google Scholar]
- Lin C.-W., Tsai F.-J., Tsai C.-H., Lai C.-C., Wan L., Ho T.-Y., Hsieh C.-C., Chao P.-D.L. Anti-SARS coronavirus 3C-like protease effects of Isatis indigotica root and plant-derived phenolic compounds. Antivir. Res. 2005;68:36–42. doi: 10.1016/j.antiviral.2005.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin L.-T., Hsu W.-C., Lin C.-C. Antiviral natural products and herbal medicines. J. Tradit. Complement. Med. 2014;4:24–35. doi: 10.4103/2225-4110.124335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Z., Wang Z., Zhang X., Diao D. Superhydrophobic, photo-sterilize, and reusable mask based on graphene nanosheet-embedded carbon (GNEC) film. Nano Res. 2021;14:1110–1115. doi: 10.1007/s12274-020-3158-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B., Zhang S., Wang X., Yu J., Ding B. Efficient and reusable polyamide-56 nanofiber/nets membrane with bimodal structures for air filtration. J. Colloid Interface Sci. 2015;457:203–211. doi: 10.1016/j.jcis.2015.07.019. [DOI] [PubMed] [Google Scholar]
- Liu Z., Yu D., Ge Y., Wang L., Zhang J., Li H., Liu F., Zhai Z. Understanding the factors involved in determining the bioburdens of surgical masks. Ann. Transl. Med. 2019;7 doi: 10.21037/atm.2019.11.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre C.R., Chughtai A.A., Seale H., Richards G.A., Davidson P.M. Respiratory protection for healthcare workers treating ebola virus disease (EVD): are facemasks sufficient to meet occupational health and safety obligations? Int. J. Nurs. Stud. 2014;51:1421. doi: 10.1016/j.ijnurstu.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majchrzycka K. Evaluation of a new bioactive nonwoven fabric for respiratory protection. Fibres Text. East. Eur. 2014;22:81–88. [Google Scholar]
- Mao N. Fibrous Filter Media. Elsevier; 2017. Nonwoven fabric filters; pp. 133–171. [Google Scholar]
- Martin S.B., Jr., Moyer E.S. Electrostatic respirator filter media: filter efficiency and most penetrating particle size effects. Appl. Occup. Environ. Hyg. 2000;15:609–617. doi: 10.1080/10473220050075617. [DOI] [PubMed] [Google Scholar]
- Mueller W., Horwell C.J., Apsley A., Steinle S., McPherson S., Cherrie J.W., Galea K.S. The effectiveness of respiratory protection worn by communities to protect from volcanic ash inhalation. part I: filtration efficiency tests. Int. J. Hyg. Environ. Health. 2018;221:967–976. doi: 10.1016/j.ijheh.2018.03.012. [DOI] [PubMed] [Google Scholar]
- Mukhopadhyay A. Composite Non-Woven Materials. Elsevier; 2014. Composite nonwovens in filters: applications; pp. 164–210. [Google Scholar]
- Nair L.S., Laurencin C.T. Biodegradable polymers as biomaterials. Prog. Polym. Sci. 2007;32:762–798. [Google Scholar]
- Nanjundappa R., Bhat G.S. Effect of processing conditions on the structure and properties of polypropylene spunbond fabrics. J. Appl. Polym. Sci. 2005;98:2355–2364. [Google Scholar]
- Neisiany R.E., Enayati M.S., Kazemi-Beydokhti A., Das O., Ramakrishna S. Multilayered bio-based electrospun membranes: a potential porous media for filtration applications. Front. Mater. 2020;7:67. [Google Scholar]
- Nicosia A., Gieparda W., Foksowicz-Flaczyk J., Walentowska J., Wesolek D., Vazquez B., Prodi F., Belosi F. Air filtration and antimicrobial capabilities of electrospun PLA/PHB containing ionic liquid. Sep. Purif. Technol. 2015;154:154–160. [Google Scholar]
- Nzediegwu C., Chang S.X. Improper solid waste management increases potential for COVID-19 spread in developing countries. Resour. Conserv. Recycl. 2020;161 doi: 10.1016/j.resconrec.2020.104947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberg T., Brosseau L.M. Surgical mask filter and fit performance. Am. J. Infect. Control. 2008;36:276–282. doi: 10.1016/j.ajic.2007.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oktay B., Kayaman-Apohan N., Erdem-Kuruca S. Presented at the IOP Conference Series: Materials Science and Engineering. IOP Publishing; 2014. Fabrication of nanofiber mats from electrospinning of functionalized polymers; p. 012011. [Google Scholar]
- Pacitto A., Amato F., Salmatonidis A., Moreno T., Alastuey A., Reche C., Buonanno G., Benito C., Querol X. Effectiveness of commercial face masks to reduce personal PM exposure. Sci. Total Environ. 2019;650:1582–1590. doi: 10.1016/j.scitotenv.2018.09.109. [DOI] [PubMed] [Google Scholar]
- Patil N.A., Gore P.M., Prakash N.J., Govindaraj P., Yadav R., Verma V., Shanmugarajan D., Patil S., Kore A., Kandasubramanian B. Needleless electrospun phytochemicals encapsulated nanofibre based 3-ply biodegradable mask for combating COVID-19 pandemic. Chem. Eng. J. 2021;416 doi: 10.1016/j.cej.2021.129152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pivato A., Amoruso I., Formenton G., Maria F.D., Bonato T., Vanin S., Marion A., Baldovin T. Evaluating the presence of SARS-CoV-2 RNA in the particulate matters during the peak of COVID-19 in Padua, northern Italy. Sci. Total Environ. 2021;784 doi: 10.1016/j.scitotenv.2021.147129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourdeyhimi B. Surgical mask particle filtration efficiency (PFE) J. Sci. Med. 2020;2:1–11. [Google Scholar]
- Pragadheeswari R., Arunkumar K., Rajakumar R., Sangeetha K. Nano membrane fibrous on lyocell non-woven fabric for bacterial filitration efficiency in surgical face mask. J. Nanosci. Nanotechnol. 2014;2:598–599. [Google Scholar]
- Prather K.A., Wang C.C., Schooley R.T. Reducing transmission of SARS-CoV-2. Science. 2020;368:1422–1424. doi: 10.1126/science.abc6197. [DOI] [PubMed] [Google Scholar]
- Public Health England When to use a surgical face mask or FFP3 respirator. 2020. https://www.fbu.org.uk/circular/2020hoc0204ad/official-guidance-when-use-surgical-face-mask-or-ffp3-respirator
- Purwar R., Goutham K.S., Srivastava C.M. Electrospun Sericin/PVA/Clay nanofibrous mats for antimicrobial air filtration mask. Fibers Polym. 2016;17:1206–1216. [Google Scholar]
- Quan F.-S., Rubino I., Lee S.-H., Koch B., Choi H.-J. Universal and reusable virus deactivation system for respiratory protection. Sci. Rep. 2017;7:1–10. doi: 10.1038/srep39956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rab S., Javaid M., Haleem A., Vaishya R. Face masks are new normal after COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14:1617–1619. doi: 10.1016/j.dsx.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasouli R., Barhoum A., Bechelany M., Dufresne A. Nanofibers for biomedical and healthcare applications. Macromol. Biosci. 2019;19:1800256. doi: 10.1002/mabi.201800256. [DOI] [PubMed] [Google Scholar]
- Ren T., Dormitorio T.V., Qiao M., Huang T.-S., Weese J. N-halamine incorporated antimicrobial nonwoven fabrics for use against avian influenza virus. Vet. Microbiol. 2018;218:78–83. doi: 10.1016/j.vetmic.2018.03.032. [DOI] [PubMed] [Google Scholar]
- Rowan N.J., Laffey J.G. Challenges and solutions for addressing critical shortage of supply chain for personal and protective equipment (PPE) arising from coronavirus disease (COVID19) pandemic–case study from the Republic of Ireland. Sci. Total Environ. 2020;725 doi: 10.1016/j.scitotenv.2020.138532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio-Romero J.C., del Carmen Pardo-Ferreira M., Torrecilla-García J.A., Calero-Castro S. Disposable masks: disinfection and sterilization for reuse, and non-certified manufacturing, in the face of shortages during the COVID-19 pandemic. Saf. Sci. 2020;129 doi: 10.1016/j.ssci.2020.104830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saberian M., Li J., Kilmartin-Lynch S., Boroujeni M. Repurposing of COVID-19 single-use face masks for pavements base/subbase. Sci. Total Environ. 2021;769 doi: 10.1016/j.scitotenv.2021.145527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saliu F., Veronelli M., Raguso C., Barana D., Galli P., Lasagni M. The release process of microfibers: from surgical face masks into the marine environment. Environ. Adv. 2021;4 doi: 10.1016/j.envadv.2021.100042. [DOI] [Google Scholar]
- Sangkham S. Face mask and medical waste disposal during the novel COVID-19 pandemic in Asia. Case Stud. Chem. Environ. Eng. 2020;2 doi: 10.1016/j.cscee.2020.100052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar S., Mukhopadhyay A., Sen S., Mondal S., Banerjee A., Mandal P., Ghosh R., Megaridis C.M., Ganguly R. Leveraging wettability engineering to develop three-layer diy face masks from low-cost materials. Trans. Indian Natl. Acad. Eng. 2020;5:393–398. doi: 10.1007/s41403-020-00115-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato J., Kogure A., Kudo K. Effectiveness of activated carbon masks in preventing anticancer drug inhalation. J. Pharm. Health Care Sci. 2016;2:1–7. doi: 10.1186/s40780-016-0062-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen B., Paul S., Bhowmik K.K., Pradhan S.N., Ali S.I. Development of novel respiratory face masks prepared from banana stem fiber against bio-aerosols: an eco-friendly approach. History. 2021;10:1993–2002. [Google Scholar]
- Silva A.L.P., Prata J.C., Walker T.R., Campos D., Duarte A.C., Soares A.M.V.M., Barcelò D., Rocha-Santos T. Rethinking and optimising plastic waste management under COVID-19 pandemic: policy solutions based on redesign and reduction of single-use plastics and personal protective equipment. Sci. Total Environ. 2020;742 doi: 10.1016/j.scitotenv.2020.140565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Šišková A.O., Frajová J., Nosko M. Recycling of poly (ethylene terephthalate) by electrospinning to enhanced the filtration efficiency. Mater. Lett. 2020;278 [Google Scholar]
- Sivri Ç. Improvement of protective and comfort properties of face masks using superabsorbent polymer containing nanofibers. Int. J. Cloth. Sci. Technol. 2018;30:668–686. [Google Scholar]
- Swennen G.R., Pottel L., Haers P.E. Custom-made 3D-printed face masks in case of pandemic crisis situations with a lack of commercially available FFP2/3 masks. Int. J. Oral Maxillofac. Surg. 2020;49:673–677. doi: 10.1016/j.ijom.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tebyetekerwa M., Xu Z., Yang S., Ramakrishna S. Electrospun nanofibers-based face masks. Adv. Fiber Mater. 2020;2:161–166. doi: 10.1007/s42765-020-00049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiliket G., Le Sage D., Moules V., Rosa-Calatrava M., Lina B., Valleton J., Nguyen Q., Lebrun L. A new material for airborne virus filtration. Chem. Eng. J. 2011;173:341–351. [Google Scholar]
- Tseng C.-C., Pan Z.-M., Chang C.-H. Application of a quaternary ammonium agent on surgical face masks before use for pre-decontamination of nosocomial infection-related bioaerosols. Aerosol Sci. Technol. 2016;50:199–210. [Google Scholar]
- Ullah S., Ullah A., Lee J., Jeong Y., Hashmi M., Zhu C., Joo K.I., Cha H.J., Kim I.S. Reusability comparison of melt-blown vs nanofiber face mask filters for use in the coronavirus pandemic. ACS Appl. Nano Mater. 2020;3:7231–7241. doi: 10.1021/acsanm.0c01562. [DOI] [PubMed] [Google Scholar]
- Wang C., Wu S., Jian M., Xie J., Xu L., Yang X., Zheng Q., Zhang Y. Silk nanofibers as high efficient and lightweight air filter. Nano Res. 2016;9:2590–2597. [Google Scholar]
- Wang Z., Pan Z., Wang J., Zhao R. A novel hierarchical structured poly (lactic acid)/titania fibrous membrane with excellent antibacterial activity and air filtration performance. J. Nanomater. 2016;2016:39–56. [Google Scholar]
- Wang N., Cai M., Yang X., Yang Y. Electret nanofibrous membrane with enhanced filtration performance and wearing comfortability for face mask. J. Colloid Interface Sci. 2018;530:695–703. doi: 10.1016/j.jcis.2018.07.021. [DOI] [PubMed] [Google Scholar]
- Wang D., Sun B.-C., Wang J.-X., Zhou Y.-Y., Chen Z.-W., Fang Y., Yue W.-H., Liu S.-M., Liu K.-Y., Zeng X.-F., Chu G.-W., Chen J.-F. Can masks be reused after hot water decontamination during the COVID-19 Pandemic? Engineering. 2020;6:1115–1121. doi: 10.1016/j.eng.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei J., Li Y. Airborne spread of infectious agents in the indoor environment. Am. J. Infect. Control. 2016;44:S102–S108. doi: 10.1016/j.ajic.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2020. Rational Use of Personal Protective Equipment (PPE) for Coronavirus Disease (COVID-19): Interim Guidance, 19 March 2020. [Google Scholar]
- WHO Shortage of personal protective equipment endangering health workers worldwide. 2020. https://www.who.int/news/item/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide
- Worby C.J., Chang H.-H. Face mask use in the general population and optimal resource allocation during the COVID-19 pandemic. Nat. Commun. 2020;11:4049. doi: 10.1038/s41467-020-17922-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Li Y., Chwang A., Ho P., Seto W. How far droplets can move in indoor environments–revisiting the Wells evaporation–falling curve. Indoor Air. 2007;17:211–225. doi: 10.1111/j.1600-0668.2007.00469.x. [DOI] [PubMed] [Google Scholar]
- Xiong S.-W., Fu P., Zou Q., Chen L., Jiang M., Zhang P., Wang Z., Cui L., Guo H., Gai J.-G. Heat conduction and antibacterial hexagonal boron nitride/polypropylene nanocomposite fibrous membranes for face masks with long-time wearing performance. ACS Appl. Mater. Interfaces. 2021;13:196–206. doi: 10.1021/acsami.0c17800. [DOI] [PubMed] [Google Scholar]
- Xu E.G., Ren Z.J. Preventing masks from becoming the next plastic problem. Front. Environ. Sci. Eng. 2021;15:125. doi: 10.1007/s11783-021-1413-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang A., Cai L., Zhang R., Wang J., Hsu P.-C., Wang H., Zhou G., Xu J., Cui Y. Thermal management in nanofiber-based face mask. Nano Lett. 2017;17:3506–3510. doi: 10.1021/acs.nanolett.7b00579. [DOI] [PubMed] [Google Scholar]
- Yang X., Pu Y., Zhang Y., Liu X., Li J., Yuan D., Ning X. Multifunctional composite membrane based on BaTiO3@ PU/PSA nanofibers for high-efficiency PM2. 5 removal. J. Hazard. Mater. 2020;391 doi: 10.1016/j.jhazmat.2020.122254. [DOI] [PubMed] [Google Scholar]
- Yu M.-S., Lee J., Lee J.M., Kim Y., Chin Y.-W., Jee J.-G., Keum Y.-S., Jeong Y.-J. Identification of myricetin and scutellarein as novel chemical inhibitors of the SARS coronavirus helicase, nsP13. Bioorg. Med. Chem. Lett. 2012;22:4049–4054. doi: 10.1016/j.bmcl.2012.04.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Xu Q., Bai S., Hai J., Cheng L., Xu G., Qin Y. Enhancing the filtration efficiency and wearing time of disposable surgical masks using TENG technology. Nano Energy. 2021;79 doi: 10.1016/j.nanoen.2020.105434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhiqing L., Yongyun C., Wenxiang C., Mengning Y., Yuanqing M., Zhenan Z., Haishan W., Jie Z., Kerong D., Huiwu L. Surgical masks as source of bacterial contamination during operative procedures. J. Orthop. Transl. 2018;14:57–62. doi: 10.1016/j.jot.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong H., Zhu Z., Lin J., Cheung C.F., Lu V.L., Yan F., Chan C.-Y., Li G. Reusable and recyclable graphene masks with outstanding superhydrophobic and photothermal performances. ACS Nano. 2020;14:6213–6221. doi: 10.1021/acsnano.0c02250. [DOI] [PubMed] [Google Scholar]
- Zhou S.S., Lukula S., Chiossone C., Nims R.W., Suchmann D.B., Ijaz M.K. Assessment of a respiratory face mask for capturing air pollutants and pathogens including human influenza and rhinoviruses. J. Thorac. Dis. 2018;10:2059. doi: 10.21037/jtd.2018.03.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zobel S., Gries T. Applications of Nonwovens in Technical Textiles. Elsevier; 2010. The use of nonwovens as filtration materials; pp. 160–183. [Google Scholar]
- Zou Z., Yao M. Airflow resistance and bio-filtering performance of carbon nanotube filters and current facepiece respirators. J. Aerosol Sci. 2015;79:61–71. [Google Scholar]