Abstract
Objectives
To report the refractive and visual outcomes of small incision lenticule extraction (SMILE) with the thinnest corneal thickness (CCT) of less than 500 µm and evaluate it in terms of safety and efficacy.
Setting
Refractive Surgery Clinic of University of Health Sciences Beyoglu Eye Training and Research Hospital, Istanbul, Turkey.
Design
Retrospective case series.
Methods
The pre-and-postoperative examinations of all patients with thin corneas (preoperative CCT <500 µm) who underwent the SMILE procedure and had a minimum of 24 months of follow-up records were reviewed from medical files. The main outcome measures of the refractive and visual outcomes and the effect on corneal high order aberrations (HOAs) were evaluated.
Results
The study included 55 eyes of 39 patients. The mean preoperative uncorrected visual acuity (UDVA) was 1.3 ± 1.5 logMAR, and the mean postoperative UDVA was significantly improved to 0.05 ± 0.80 logMAR at the last visit (p < 0.001). At the last follow-up, 84% of the eyes were within ± 0.50D, and 96% of the eyes were within ±1.00D of attempted SE refraction. The HOAs of coma (p < 0.001), secondary astigmatism (p = 0.015), spherical aberration (p < 0.001), and RMS (p < 0.001) aberrations increased significantly from the baseline to the postoperative last visit. The increase in trefoil was not significant (p = 0.32). No sight threatening complications or ectasia were observed during the follow-up time.
Conclusion
SMILE is a safe and effective technique with long-term stability for treatment of myopia in eyes with a thin cornea, and satisfactory results can be obtained if candidates for surgery are selected carefully with particular emphasis on normal preoperative corneal topography.
Subject terms: Outcomes research, Refractive errors
Introduction
Small incision lenticule extraction (SMILE) is a relatively new surgical technique which includes a minimally invasive flap-free procedure for correction of myopia and myopic astigmatism. Since it was first introduced by Sekundo et al. in 2011 [1, 2], promising clinical results have been reported [3–9], and long-term results continue to be evaluated [10–13]. However, SMILE results on specific patient groups like patients with thin corneas need to be evaluated in order to thoroughly assess the safety and efficacy of the procedure.
There are several studies in the literature that investigate the results of other refractive surgery procedures such as photorefractive keratectomy (PRK) or laser in situ keratomileusis (LASIK) on patients with thinnest corneal thickness (CCT) less than 500 µm [14–19]. There are also studies about the clinical results and morphologic results of small incision lenticule extraction (SMILE) when combined with accelerated crosslinking [20, 21]. However, to the best of our knowledge, there is a lack of data in the literature focusing SMILE results on thin cornea eyes alone.
The aim of this study was to report the refractive and visual outcomes of SMILE with CCT less than 500 µm and evaluate it in terms of safety and efficacy.
Material and methods
The medical records of all patients with thin corneas (preoperative CCT < 500 µm) who underwent the SMILE procedure at the Refractive Surgery Department of University of Health Sciences Beyoglu Eye Training and Research Hospital were evaluated retrospectively. This study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the institutional ethical committee board of University of Health Sciences Okmeydani Training and Research Hospital, Istanbul. Written informed consent was obtained from each patient before the procedure. All patients were over the age of 18 and had a normal corneal topographic pattern and stable refraction for at least 1 year preoperatively. None of the eyes had a calculated postoperative residual stromal bed thickness (RSBT) below 250 µm. Patients who had any ocular pathology other than refractive error or history of ocular surgery and patients with a follow-up of less than 24 months were excluded from the study.
Preoperative and postoperative examinations
All patients had a complete preoperative ophthalmic examination including UDVA and CDVA, manifest refraction and cycloplegic refraction measurements (KR-1 Auto Kerato- Refractometer, Topcon, Japan), Goldmann applanation tonometry, and thorough slit-lamp evaluation and dilated fundus examination. In addition, corneal topography, ocular wavefront analysis, corneal wavefront analysis, dynamic infrared pupillography with a Scheimpflug camera combined with placido-disk corneal topography and aberrometry system (6-mm pupil diameter, Sirius, Costruzioni Strumenti Oftalmici, Florence, Italy) were performed. Patients wearing contact lenses were instructed to stop their use at least 2 weeks prior to the examination.
The patients were followed-up postoperatively at routine 1-day, 1-week, 1-month, 6-month and 12-month visits. Annual routine visits were scheduled for the patients thereafter. Postoperative examinations included UDVA, CDVA, manifest refraction, slit-lamp evaluation, corneal topography, and recordings for any adverse effects or complications. The root mean square (RMS) values of the total high order aberration (HOA), spherical aberration, secondary astigmatism as well as coma and trefoil aberrations at 6-mm diameter central corneal zone were obtained from the topography data. The cases were divided into two groups according to both preoperative refractive status (<−4 Dioptres, ≥ −4 Dioptres) and central CCT (470–485 µm; 485–500 µm). Despite the analysis for all the eyes; further comparisons were performed for subgroups in terms of postoperative refractive features and CCT.
Surgical technique
All surgical procedures within the scope of this study were performed using the VisuMax (Carl Zeiss Meditec, Germany) femtosecond laser platform using the same laser settings as described in detail in the literature. The following settings were used for all procedures: a spot size of 3 μm was used for lamellar incisions and 2 μm for side-cuts, a spot energy of 140 nanojoules (nJ) was used along with a minimum lenticule side-cut thickness of 15 μm, lenticule side-cut angle of 120°, and optical zone of 6.5 mm. The cap diameter was planned to have a 7.5 mm diameter with a 50° side-cut angle in the superior region. The cap thickness (CT) was planned as 120 μm for all eyes. A small-sized interface was used for all patients. All patients were informed for the surgical limits, and the maximum intended refraction was −1.0 D for eyes that would seem to have postoperative RSBT very close to 250 μm. After the lenticule cut and side-cut were completed, any remaining tissue bridges were removed with a thin blunt spatula, and the lenticule was extracted mechanically with a pair of forceps. The postoperative regimen included moxifloxacin 0.5% ophthalmic solution for 5 days and dexamethasone 0.1% ophthalmic solution for two weeks, each four times a day. Preservative-free artificial tear drops were continued for at least one month subsequently.
Statistical analysis
All statistical analyses were performed using SPSS software (version 21.0; IBM, Armonk, NY). The distribution of the variables was analyzed using the Kolmogorov-Smirnov test. Mean, standard deviation, minimum-maximum and frequency values were used in descriptive statistical analyses. The paired sample t-tests and correlations were used to evaluate the results, where applicable. The safety index (postoperative CDVA/preoperative CDVA ratio) and efficacy index (postoperative UCVA/preoperative CDVA ratio) were calculated.
All visual acuity data were converted to logarithmic scale (logarithm of the minimum angle of resolution-logMAR) prior to statistical analysis. A p value < 0.05 was considered to denote the results as statistically significant. The included graphics were constructed using Microsoft Excel templates (2013, Microsoft Corporation, Seattle, WA, USA) designed by London Vision Clinic (London, W1G 7LA, UK).
Results
A total of 55 eyes of 39 patients (39 women, 16 men) with CCT of less than 500 µm who underwent the SMILE procedure for myopia were included in the study. The mean age was 26.9 ± 3.7 years (range 20–37 years), and the mean follow-up time was 33.3 ± 11.4 months (range 24–78 months). The preoperative and postoperative findings of the patients are summarized in Table 1.
Table 1.
Summary of preoperative and postoperative data.
| Parameters | Mean ± SD (Range) | p value | |
|---|---|---|---|
| Preoperative | Postoperative | ||
| UDVA (logMAR) | 1.3 ± 1.5 (0.7 to 2.0) | 0.05 ± 0.80 (−0.10 to 0.40) | p < 0.001 |
| CDVA (logMAR) | 0.05 ± 1.00 (0 to 0.2) | 0.0 ± 1.00 (−0.10 to 0.15) | p = 0.001 |
| Sphere (D) | −4.51 ± 1.25 (−2.25 to −6.50) | −0.1 ± 0.30 (−1.75 to 0.00) | p < 0.001 |
| Cylinder (D) | −0.53 ± 0.56 (0 to −2.00) | −0.17 ± 0.33 (−1.50 to 0.00) | p < 0.001 |
| SE (D) | −4.81 ± 1.22 (−2.50 to −7.50) | −0.19 ± 0.39 (−2.00 to 0.00) | p < 0.001 |
| CCT (µm) | 491.4 ± 7.40 (471 to 499) | 393.6 ± 19.3 (355 to 432) | p < 0.001 |
| Kapex (D) | 45.47 ± 1.74 (41.58 to 48.64) | 40.23 ± 3.45 (43.81 to 48.00) | p < 0.001 |
| Kmean (D) | 44.15 ± 1.68 (40.67 to 47.41) | 40.13 ± 1.50 (36.36 to 42.62) | p < 0.001 |
| Kvb | 10.14 ± 2.50 (5 to 15) | 12.85 ± 3.05 (6 to 22) | p < 0.001 |
| Corneal cylinder (D) | −0.93 ± 0.35 (−0.10 to −1.86) | −0.82 ± 0.38 (−0.20 to −1.87) | p = 0.119 |
Visual acuity
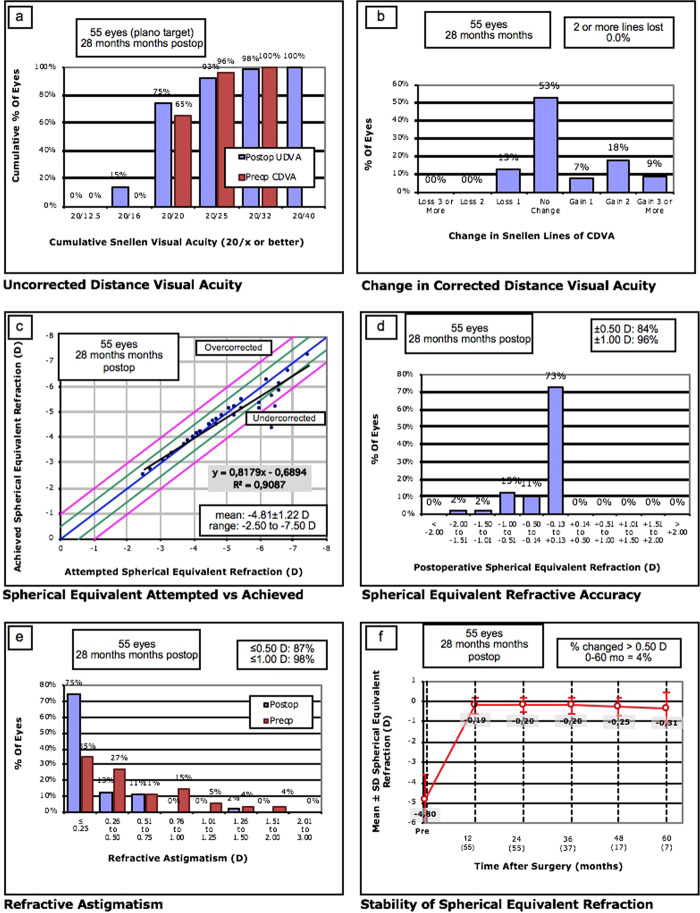
The mean preoperative UDVA was 1.3 ± 1.5 logMAR, and the mean postoperative UDVA was significantly improved to 0.05 ± 0.80 logMAR at the last visit (p < 0.001). At the last visit examination of the 55 eyes, 51 eyes (92.7%) had UDVA of 20/25 or better, and 41 eyes (74.5%) had UDVA of 20/20 or better (Fig. 1a). The mean preoperative CDVA was 0.05 ± 1.00 logMAR. At the baseline examination of the 55 eyes; 53 eyes (96.4%) had CDVA of 20/25 or better, and 36 eyes (65.5%) had CDVA of 20/20 or better (Fig. 1a).The comparison of the results according to preoperative refractive status was summarized in Table 2.
Fig. 1. Analysis of the pre-and-postoperative data of the eyes that underwent SMILE procedure.
a The cumulative Snellen visual acuity for SMILE on thin corneas. CDVA: corrected distance visual acuity, UDVA: uncorrected distance visual acuity. b Change in lines of corrected distance visual acuity after SMILE on thin corneas. CDVA: corrected distance visual acuity. c Attempted versus achieved spherical equivalent refraction after SMILE on thin corneas. d Spherical equivalent refraction after SMILE on thin corneas. e Refractive astigmatism after SMILE on thin corneas. f Time course of spherical equivalent refraction after SMILE on thin corneas.
Table 2.
Visual acuity and refractive status changes due to preoperative values.
| <−4 D (n:13) | ≥−4 D (n:42) | P* value | |
|---|---|---|---|
| Preoperative UCVA | 0.08 ± 0.02 (0.05–0.1) | 0.03 ± 0.02 (0.01–0.2) | <0.001 |
| Preoperative BCVA | 0.96 ± 0.07 (0.8–1.0) | 0.92 ± 0.11 (0.6–1.0) | 0.155 |
| Preoperative SE | −3.25 ± 0.6 (−4.0-(-)2.5) | −5.2 ± 0.92 (−7.5–(−)4.1) | <0.001 |
| Postoperative UCVA | 0.92 ± 0.07 (0.8–1.0) | 0.89 ± 0.18 (0.4–1.2) | 0.623 |
| Postoperative BCVA | 0.96 ± 0.05 (0.9–1.0) | 1.00 ± 0.11 (0.7–1.2) | 0.210 |
| Postoperative SE | 0.00 ± 0 (0–0) | −0.24 ± 0.42 (−2–0) | 0.046 |
UCVA Uncorrected Visual Acuity, BCVA Best Corrected Visual Acuity, SE Spherical Equivalent.
*Student t test.
Efficacy
The mean preoperative UDVA and CDVA were 1.3 ± 1.5 (ranging from 0.7 to 2.0) logMAR and 0.05 ± 1.0 (ranging from 0 to 0.2) logMAR, respectively. At the last follow-up visit, the mean UDVA improved to 0.05 ± 0.80 (ranging from −0.10 to 0.40) logMAR, and efficacy index (post-operative UDVA/pre-operative CDVA) was 0.97 ± 0.15. Figure 1a shows the cumulative Snellen visual acuities.
Safety
At the last follow-up visit, the mean CDVA was 0.0 ± 1.00 (ranging from −0.10 to 0.15) logMAR, and the safety index (post-operative CDVA/pre-operative CDVA) was 1.07 ± 0.15. Figure 1b shows the changes in the CDVA lines. At the last follow-up examination, no patient showed a loss of two or more lines of CDVA. Seven eyes (12.7%) with one line CDVA loss was intentionally undercorrected in order to respect the RSBT of 250 µm. No vision-threatening complications or ectasia were observed during surgery or the postoperative follow-up period.
Predictability
Figure 1c presents a scatter plot of the attempted versus achieved correction of 55 eyes in terms of spherical equivalent refraction. At the last follow-up examination, 84% of the eyes were within ± 0.50 D, and 96% of the eyes were within ±1.00 D of attempted SE refraction. Figure 1d demonstrates the postoperative SE refraction of the eyes at the last visit. At the last follow-up examination, 87% of the eyes had an astigmatism ≤0.50 D, and 98% of the eyes had an astigmatism ≤1.00 D. Figure 1e demonstrates pre and postoperative astigmatism refraction of the 55 eyes.
Stability
Figure 1f shows the stability of spherical equivalent refraction in terms of the difference in SE between the intended and achieved correction over the post-operative period of time.
Corneal high-order aberrations
Data of the corneal high order aberrations (HOAs) are summarized in Table 3. The HOAs of coma (p < 0.001), secondary astigmatism (p = 0.015), spherical aberration (p < 0.001), and RMS (p < 0.001) aberrations increased significantly from the baseline to the postoperative last visit examination. The increase in trefoil was not significant (p = 0.32).
Table 3.
Preoperative and postoperative corneal high order aberrations.
| Parameters | Mean ± SD (Range) | p value | |
|---|---|---|---|
| Preoperative | Postoperative | ||
| RMS | 0.41 ± 0.12 (0.22 to 0.74) | 0.61 ± 0.20 (0.34 to 1.16) | p < 0.001 |
| Trefoil | 0.14 ± 0.09 (0.02 to 0.37) | 0.17 ± 0.08 (0.05 to 0.42) | p = 0.32 |
| Coma | 0.24 ± 0.14 (0.02 to 0.59) | 0.43 ± 0.23 (0.03 to 0.99) | p < 0.001 |
| Secondary astigmatism | 0.05 ± 0.04 (0.01 to 0.19) | 0.08 ± 0.05 (0.01 to 0.23) | p = 0.015 |
| Spherical aberration | 0.23 ± 0.07 (0.03 to 0.35) | 0.31 ± 0.12 (0.07 to 0.65) | p < 0.001 |
Thinnest corneal thickness (TCT)
The mean preoperative and postoperative TCT were 491.4 ± 7.40 (range from 471 to 499) and 393.6 ± 19.3 (range from 355 to 432) µm, respectively. The mean lenticule thickness (LT) was 96.7 ± 19.1 µm (range from 56 to 131). The mean RSBT value was found to be 264.7 ± 11.7 µm, which was calculated using the CT and maximum LT subtracted from the preoperative TCT. The comparison of the results due to preoperative central CCT was summarized in Table 4.
Table 4.
Central corneal thickness and posterior elevation changes due to preoperative values.
| 470–485 µm(n:10) | 485–500 µm (n:45) | P* value | |
|---|---|---|---|
| Preoperative CCT (µm) | 477 ± 4.69 (471–485) | 494.4 ± 3.32 (486–499) | <0.001 |
| Preoperative Kvb (µm) | 11.0 ± 1.63 (9–13) | 9.94 ± 2.6 (5–15) | 0.230 |
| Postoperative CCT (µm) | 393.3 ± 21.3 (361–424) | 393.6 ± 19 (355–432) | 0.957 |
| Postoperative Kvb(µm) | 13.3 ± 4.9 (6–22) | 12.75 ± 2.52 (6–17) | 0.614 |
| RSBT(µm) | 277.1 ± 17.5 (261–306) | 274.2 ± 17.05 (250–312) | 0.630 |
CCT Central corneal thickness, Kvb Posterior elevation, RSBT residual stromal bed thickness.
*Student t test.
Targeted undercorrection
Seven (12.7%) of the eyes were left uncorrected intentionally in order to respect the RSBT of 250 µm. For these 7 eyes, the mean preoperative SE refraction value was changed from −6.35 ± 0.26 (ranging from −6.62 to −6.00) to −1.03 ± 0.46 (ranging from −2.00 to −0.75), postoperatively. The mean preoperative and postoperative CDVA were 0.1 ± 0.9 (ranging from 0.2 to 0) and 0 ± 0.8 (ranging from 0.1 to −0.1) logMAR, respectively. The mean postoperative UDVA was 0.2 ± 0.8 (ranging from 0.4 to 0.1) logMAR. The mean RSBT was 253 ± 2.9 (251–259) µm. The efficacy index for this subgroup was 0.77 ± 0.16 (0.44–0.87); despite this relatively lower efficacy, the safety index was higher than the total group: 1.26 ± 0.20 (0.89–1.50). The efficacy index for the remaining eyes when this undercorrected group is excluded is 0.99 ± 0.13 (0.80–1.50).
Discussion
Since Seiler et al. first reported iatrogenic ectasia after LASIK in 1998 [22, 23]; corneal ectasia has been one of the most important and serious postoperative complications after refractive surgery, causing visual loss and refractive aberrations. Its prevention has been a major concern for refractive surgeons, thus comprehension of its causes and risk factors has gained importance in terms of surgical predictability. Operating on eyes with low preoperative CCT and postoperative low RSBT are suggested as significant risk factors for postoperative ectasia [24].
As an alternative to LASIK, the SMILE technique for treatment of myopia has demonstrated reduced biomechanical impact on corneal strength, resulting in lower risk of iatrogenic ectasia when compared to LASIK. There are only four cases of post-SMILE ectasia reported in the literature, three of which showed preoperative abnormal topography findings [25]. The mean preoperative TCT value for these cases was 520 ± 29 µm (ranging from 513 to 559 µm), and all were above 500 µm [25], suggesting preoperative topographic abnormality but not low preoperative TCT as the responsible risk factor for progression to postoperative ectasia, at least in three of the cases.
In our study, the mean preoperative TCT and the mean RSBT were 491.4 ± 7.40 µm and 264.7 ± 11.7 µm, respectively. All of the preoperative topography examinations showed no abnormality. At the last follow-up, no cases of ectasia were observed in any of our patients. We preferred to perform the SMILE procedure in all of the cases since collagen networks of anterior stroma and biomechanical integrity of the cornea are preserved better in SMILE with respect to LASIK [25].
There are several studies in the literature that focus on outcomes of refractive surgical procedures, PRK and LASIK, on patients with thin corneas. Hashemi et al. demonstrated the results of PRK in patients with CCT <500 µm and found that PRK is a safe, effective, and predictable procedure on thin corneas but precipitates an increase in HOAs [15]. Their results of improvement of vision and refraction were similar to our study; they found the efficacy and safety of the procedure to be 1.00 ± 0.05 and 1.01 ± 0.05, whereas we found 0.97 ± 0.15 and 1.07 ± 0.15, respectively. Our study is also similar to this study in terms of the statistically significant increase in HOAs. In another study reporting the long-term results (1–3 years) of PRK on 68 eyes with thin corneas, PRK was suggested as a safe and predictable technique for myopic refractive corrections [14]. In another report from our country analyzing the long-term safety and efficacy of PRK in eyes with thin residual thickness (<400 µm), there was no sight-threatening haze or ectasia at the end of follow-up period (24 to 66 months) [26].
Although operating on eyes with thin corneas is considered as a risk factor for post-LASIK ectasia, Caster et al. encountered no postoperative ectasia in their study on 109 eyes with thin corneas (CCT 450–500 µm) but without any known risk factors for keratectasia [27]. In another study comparing thin corneas that underwent LASIK with thicker corneas, CDVA of 20/20 or better at the last follow-up was found in 99.1% of eyes, whereas we found it in 74.5% of eyes in our study [18]. We believe that the difference is due to their high mean preoperative CDVA value of −0.22 ± 0.07 logMAR, whereas it was 0.05 ± 1.00 logMAR in our study. Furthermore, they concluded that there were no significant differences in terms of safety, efficacy, and long-term stability of LASIK between the thin cornea group and control group [18]. Song et al. investigated the long term safety of LASIK on eyes with thin corneas; they found efficacy and safety index values of the procedure to be 0.99 and 1.09, respectively, which is similar to our results [19]. In their study, 71% and 88% of eyes were within ±0.50 D and ±1.00 D of attempted SE refraction, respectively. In the present study, our outcomes were similar yet slightly better as we found 84% and 96% of eyes within ±0.50 D and ±1.00 D of attempted SE refraction, respectively. The difference probably stems from their high preoperative SE value of −6.17 ± 2.56 D (ranging from −1.50 to −15.00) when compared to ours; they included 79 eyes (45.1%) with SE > −6.00 D, whereas we only had 10 eyes (18.2%). Djodeyre et al. reported results of LASIK with microkeratome on eyes with CCT < 470 µm and found it to be safe, effective, and predictable with a significantly better safety index (1.07 ± 0.12) when compared to the group treated with laser surface ablation methods [28]. The important issue is that all eyes in all these studies had normal topographical pattern and RSBT over 250 µm; so the most remarkable point is that the topographical pattern precedes CCT in terms of safety for LASIK and the other keratorefractive techniques [29].
To the best of our knowledge, our study is the first to report the clinical and refractive outcomes of SMILE on thin corneas. We were comfortable choosing the SMILE technique for treating myopia in our patients with thin corneas, since it results in less injury to subbasal nerve plexus and less impact on the corneal biomechanical integrity with the advantage of being a minimally invasive and flap-less procedure. As a consequence, it has the benefit of less dry eye symptoms and lack of flap-related complications as it is demonstrated in several previous studies in the literature [1, 4, 11, 25]. On the other hand, increase in corneal (HOAs) is an expected result of the SMILE procedure as well as other corneal refractive surgery techniques. In the prospective study by Shah et al. that investigated the results of the SMILE technique, the increase detected in the HOAs was the same as found in our study, including significant increases in coma, spherical aberration, and secondary astigmatism but not in the trefoil [1].
In the current study, 84% and 96% of eyes were within ±0.50 D and ±1.00 D of attempted SE refraction, respectively. In another study from our clinic, Agca and his colleagues reported that 98% of eyes with mild to moderate myopia were within ±0.50 D of attempted SE refraction postoperatively [13]. This is because of our tendency for undercorrection when preoperative TCT is below 500 µm and it is a priority to not exceed the limits for residual stromal thickness. When the patients with targeted undercorrection are left out, the efficacy index (0.99 ± 0.13) is comparable with other studies [30–32], which report results of SMILE for corneas with central CCT of 550 ± 30 in low to moderate myopia. So this residual SE refraction does not deteriorate the uncorrected distance visual acuities of the participants and does not reduce the efficacy of this procedure for thin corneas if only it is less than 0.75 D.
Limitations of our study include its retrospective nature of design and small sample of eyes studied. Also, the postoperative follow-up time interval may not be sufficient in order to evaluate iatrogenic ectasia development. Thus, our inclusion criteria required a minimum of 24 months; we have participants with 78 months of follow-up time and the mean follow- up time was 33 months. More substantial interpretations can be made in the presence of a comparison group of eyes either with normal CCT or with thin corneas undergoing different refractive surgery methods other than SMILE. Furthermore, we did not obtain any proof about corneal biomechanical stability because we did not evaluate corneal hysteresis or corneal resistance factor by an ocular response analyser or another novel technology dynamic Scheimpflug Analyzer (Corvis ST) [33]. Further reports with these examinations are necessary to assess the biomechanical stability with more remarkable proofs rather than the lack of ectasia.
In conclusion, our results demonstrate that SMILE is a safe and effective technique with a minimum 2-years stability for treatment of myopia in eyes with a thin cornea. Although 500 µm has generally been regarded as a “cut-off value” for safe refractive surgery by many surgeons, we claim that satisfactory results can be obtained from treatment of myopia in eyes with thin cornea using the SMILE technique if candidates for surgery are selected carefully with particular emphasis on normal preoperative corneal topography [14]. Further prospective randomized comparative studies with a large number of eyes and longer follow-up periods are needed in order to confirm the outcomes of this present study.
Summary
What was known before
Small incision lenticule extraction (SMILE) is a safe and effective procedure with long-term stability for treatment of myopia, however its outcomes in patients with thin corneas has not been studied.
What this study adds
Although 500 μm has generally been regarded as a cut-off value for safe refractive surgery by many surgeons so far, SMILE technique can be performed in eyes with preoperative CCT <500 μm with satisfactory outcomes and a minimum 1-year stability for treatment of myopia if special attention is paid for the presence of normal preoperative corneal topography.
Supplementary information
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version of this article (10.1038/s41433-020-01256-5) contains supplementary material, which is available to authorized users.
References
- 1.Shah R, Shah S, Sengupta S. Results of small incision lenticule extraction: all-in-one femtosecond laser refractive surgery. J Cataract Refract Surg. 2011;37:127–37. doi: 10.1016/j.jcrs.2010.07.033. [DOI] [PubMed] [Google Scholar]
- 2.Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol. 2011;95:335–9. doi: 10.1136/bjo.2009.174284. [DOI] [PubMed] [Google Scholar]
- 3.Reinstein DZ, Carp GI, Archer TJ, Gobbe M. Outcomes of small incision lenticule extraction (SMILE) in low myopia. J Refract Surg. 2014. 10.3928/1081597X-20141113-07. [DOI] [PubMed]
- 4.Vestergaard A, Ivarsen AR, Asp S, Hjortdal JO. Small-incision lenticule extraction for moderate to high myopia: Predictability, safety, and patient satisfaction. J Cataract Refract Surg. 2012;38:2003–10. doi: 10.1016/j.jcrs.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 5.Hjortdal J, Vestergaard AH, Ivarsen A, Ragunathan S, Asp S. Predictors for the outcome of small-incision lenticule extraction for myopia. J Refract Surg. 2012;28:865–71. doi: 10.3928/1081597X-20121115-01. [DOI] [PubMed] [Google Scholar]
- 6.Kim JR, Kim BK, Mun SJ, Chung YT, Kim HS. One-year outcomes of small-incision lenticule extraction (SMILE): Mild to moderate myopia vs. high myopia. BMC Ophthalmol. 2015. 10.1186/s12886-015-0051-x. [DOI] [PMC free article] [PubMed]
- 7.Xu Y, Yang Y. Small-incision lenticule extraction for myopia: results of a 12-month prospective study. Optom Vis Sci. 2015. 10.1097/OPX.0000000000000451. [DOI] [PubMed]
- 8.Aǧca A, Demirok A, Çankaya KI, Yaşa D, Demircan A, Yildirim Y, et al. Comparison of visual acuity and higher-order aberrations after femtosecond lenticule extraction and small-incision lenticule extraction. Contact Lens Anterior Eye. 2014. 10.1016/j.clae.2014.03.001. [DOI] [PubMed]
- 9.Sekundo W, Gertnere J, Bertelmann T, Solomatin I. One-year refractive results, contrast sensitivity, high-order aberrations and complications after myopic small-incision lenticule extraction (ReLEx SMILE). Graefe’s Arch Clin Exp Ophthalmol. 2014. 10.1007/s00417-014-2608-4. [DOI] [PubMed]
- 10.Blum M, Täubig K, Gruhn C, Sekundo W, Kunert KS. Five-year results of small incision lenticule extraction (ReLEx SMILE) Br J Ophthalmol. 2016;100:1192–5. doi: 10.1136/bjophthalmol-2015-306822. [DOI] [PubMed] [Google Scholar]
- 11.Han T, Zheng K, Chen Y, Gao Y, He L, Zhou X. Four-year observation of predictability and stability of small incision lenticule extraction. BMC Ophthalmol. 2016;16:149. doi: 10.1186/s12886-016-0331-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burazovitch J, Naguzeswski D, Beuste T, Guillard M. Predictability of SMILE over four years in high myopes. J Fr Ophtalmol. 2017. 10.1016/j.jfo.2017.05.001. [DOI] [PubMed]
- 13.Ağca A, Tülü B, Yaşa D, Yıldırım Y, Yıldız BK, Demirok A. Long-term (5 years) follow-up of small-incision lenticule extraction in mild-to-moderate myopia. J Cataract Refract Surg. 2019. 10.1016/j.jcrs.2018.11.010. [DOI] [PubMed]
- 14.Donnenfeld E. Long-term results of thin corneas after refractive laser surgery. Evidence-Based Ophthalmol. 2008. 10.1097/IEB.0b013e31816c7b78.
- 15.Hashemi H, Miraftab M, Asgari S. Photorefractive keratectomy results in myopic patients with thin cornea eyes. Oman J Ophthalmol. 2015. 10.4103/0974-620X.149860. [DOI] [PMC free article] [PubMed]
- 16.Kremer I, Bahar I, Hirsh A, Levinger S. Clinical outcome of wavefront-guided laser in situ keratomileusis in eyes with moderate to high myopia with thin corneas. J Cataract Refract Surg. 2005. 10.1016/j.jcrs.2004.12.055. [DOI] [PubMed]
- 17.Cardona G, Sabino-Borreguero S, Juárez-Escalona E, Fornieles A. Visual and refractive outcome of epi-LASIK for myopia in thin corneas: a 12-month follow-up. Eur J Ophthalmol. 2012. 10.5301/ejo.5000170. [DOI] [PubMed]
- 18.Tomita M, Watabe M, Mita M, Waring GO IV. Long-term observation and evaluation of femtosecond laser-assisted thin-flap laser in situ keratomileusis in eyes with thin corneas but normal topography. J Cataract Refract Surg. 2014. 10.1016/j.jcrs.2013.07.054. [DOI] [PubMed]
- 19.Song YW, He R, Ma JX, Koch DD, Wang L. Long-term safety of laser in situ keratomileusis in eyes with thin corneas: 5-year follow-up. Int J Ophthalmol. 2018. 10.18240/ijo.2018.07.25. [DOI] [PMC free article] [PubMed]
- 20.Ganesh S, Brar S. Clinical outcomes of small incision lenticule extraction with accelerated cross-linking (ReLEx SMILE Xtra) in patients with thin corneas and borderline topography. J Ophthalmol. 2015;2015:263412. doi: 10.1155/2015/263412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou Y, Liu M, Zhang T, Zheng H, Sun Y, Yang X, et al. In vivo confocal laser microscopy of morphologic changes after small incision lenticule extraction with accelerated cross-linking (SMILE Xtra) in patients with thin corneas and high myopia. Graefes Arch Clin Exp Ophthalmol. 2018;256:199–207. doi: 10.1007/s00417-017-3811-x. [DOI] [PubMed] [Google Scholar]
- 22.Seiler T, Quurke AW. Iatrogenic keratectasia after LASIK in a case of forme fruste keratoconus. J Cataract Refract Surg. 1998. 10.1016/S0886-3350(98)80057-6. [DOI] [PubMed]
- 23.Seiler T, Koufala K, Richter G. Iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg. 1998;14:312–7. doi: 10.3928/1081-597X-19980501-15. [DOI] [PubMed] [Google Scholar]
- 24.Randleman JB, Trattler WB, Stulting RD. Validation of the ectasia risk score system for preoperative laser in situ keratomileusis screening. Am J Ophthalmol. 2008. 10.1016/j.ajo.2007.12.033. [DOI] [PMC free article] [PubMed]
- 25.Moshirfar M, Albarracin JC, Desautels JD, Birdsong OC, Linn SH, Hoopes PC. Ectasia following small-incision lenticule extraction (SMILE): a review of the literature. Clin Ophthalmol. 2017. 10.2147/OPTH.S147011. [DOI] [PMC free article] [PubMed]
- 26.Kocamış Sİ, Çakmak HB, Gerçeker S, Çağıl N. Long-term clinical outcomes of myopic patients having thin residual corneal thickness after excimer laser surface ablation. Semin Ophthalmol. 2017;32:474–81. doi: 10.3109/08820538.2015.1120755. [DOI] [PubMed] [Google Scholar]
- 27.Caster AI, Friess DW, Potvin RJ. Absence of keratectasia after LASIK in eyes with preoperative central corneal thickness of 450 to 500 microns. J Refract Surg. 2007;23:728–8. doi: 10.3928/1081-597X-20071001-07. [DOI] [PubMed] [Google Scholar]
- 28.Djodeyre MR, Ortega-Usobiaga J, Beltran J, Baviera J Long-term comparison of laser in situ keratomileusis versus laser surface ablation in corneas thinner than 470 μm. J Cataract Refract Surg. 2012. 10.1016/j.jcrs.2011.12.036. [DOI] [PubMed]
- 29.Tomita M, Watabe M, Mita M, Waring GO., 4th Long-term observation and evaluation of femtosecond laser-assisted thin-flap laser in situ keratomileusis in eyes with thin corneas but normal topography. J Cataract Refract Surg. 2014;40:239–50. doi: 10.1016/j.jcrs.2013.07.054. [DOI] [PubMed] [Google Scholar]
- 30.Taneri S, Kießler S, Rost A, Schultz T, Dick HB. Clinical outcomes of small incision lenticule extraction versus advanced surface ablation in low myopia. Eur J Ophthalmol. 2019. 10.1177/1120672119865699. [DOI] [PubMed]
- 31.Hansen RS, Lyhne N, Grauslund J, Vestergaard AH. Small-incision lenticule extraction (SMILE): outcomes of 722 eyes treated for myopia and myopic astigmatism. Graefe’s Arch Clin Exp Ophthalmol. 2016. 10.1007/s00417-015-3226-5. [DOI] [PubMed]
- 32.Ivarsen A, Asp S, Hjortdal J. Safety and complications of more than 1500 small-incision lenticule extraction procedures. Ophthalmology. 2014. 10.1016/j.ophtha.2013.11.006. [DOI] [PubMed]
- 33.Herber R, Terai N, Pillunat KR, Raiskup F, Pillunat LE, Spörl E. Dynamic Scheimpflug Analyzer (Corvis ST) for measurement of corneal biomechanical parameters: a praxis-related overview. Ophthalmologe. 2018. 10.1007/s00347-018-0716-y. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.