Abstract
Background: The COVID-19 outbreak harmed acute coronary syndromes. During the national lockdown in Italy, the fear of post-admission contagion translated into significant delays in seeking medical help among STEMI (ST-elevation myocardial infarction) patients. Objective and methods: Our analysis aimed to assess the ACS (Acute Coronary Syndromes) admissions during the pandemic, together with time to presentation and clinical outcomes compared to 2019 in a cardiovascular hub in Milan. Data of ACS patients admitted during the pandemic year 2020 were extracted by the hospital’s database and compared to a historical cohort of patients admitted for the same clinical indications in 2019. Results: A total of 599 ACS cases were recorded in 2020 vs. 386 cases in 2019, with a net 55% increase, associated with late clinical presentations, a threefold increase in cardiogenic shock, and a more than two-fold higher mortality rate. Conclusions: The ultimate goal of this analysis is to preserve the life-saving focus on universal and prompt STEMI diagnosis and treatment, even in a time of dynamic global crisis.
Keywords: ACS, COVID-19 outbreak, STEMI, late presentation
Introduction
The COVID-19 spreading pandemic phase in March-April 2020 was associated with preliminary observations of reduction in prompt acute coronary syndromes admissions and delayed presentations, mainly related to people’s perception of the hospital being war zones, leading to severe mechanical complications and worse clinical outcome [1]. By the time this analysis was conceived, Italy was the first most involved Country in the world for infected patients, actually ranking eighth in number (3,793,033) of confirmed COVID-19 cases and sixth in infection-related fatalities (115,088) [2].
Our Institute was selected as one of the cardiovascular emergency hubs in Milan, with an internal pathway ensuring timely, high-level cardiac care to COVID-19 and COVID-19-free patients, allowing an effective in-hospital infection spread and exposure risk prevention. The current analysis was aimed to assess the ACS admissions during the pandemic periods, together with time to presentation and clinical outcomes compared to 2019 in our Institute serving as a cardiovascular hub.
Methods
Patients’ selection
This single-center, prospective study from a public service healthcare in Milan included all consecutive patients with acute coronary syndromes admitted from January 1 to December 31, 2020 including the COVID-19 pandemic. ACS included STEMI, NSTEMI and myocardial infarction with nonobstructive coronary arteries (MINOCA), all defined according to the current European Society of Cardiology guidelines definitions [3,4].
These data were compared with the historical cohort of patients admitted for the same indications in 2019, in terms of time from symptoms onset to hospital admission, clinical characteristics, and in-hospital outcomes.
Endpoints
Primary endpoints were the rate of ACS admissions, time to presentation from symptoms onset, and in-hospital mortality rate for ACS during the pandemic period vs. the control period in 2019.
Data collection
Epidemiological data of consecutive patients admitted for ACS were anonymously extracted from the hospital’s database and checked for accuracy by the investigators. The informed consent was waived according to a specific FAQ “Data processing in clinical trials and medical research in the context of the COVID 19 health emergency”, published by the Italian Data Protection Authority. The study was carried out in accordance with the Declaration of Helsinki and approved by the local Ethic research committee of Centro Cardiologico Monzino (R1255/20-CCM 1320).
Statistical analysis
Categorical variables were reported as number, percentage and compared by means of Pearson’s Chi square test (or by Fisher exact test as appropriate). Statistical significance was set at p value < 0.05. All analyses were performed with SPSS 21 (IBM Corporation, Armonk, NY, USA) and Jamovi version 1.2.27.0 (gamlj extension).
Results
Acute coronary syndromes and time to presentation
Patients’ clinical presentation and characteristics are shown in Table 1. A total of 599 ACS cases were recorded in Covid-19 outbreak year vs. 386 cases in 2019, with a net 55% cumulative increase in emergency/urgency interventional coronary procedures (Figure 1).
Table 1.
Patients’ clinical characteristics and presentation
| Jan 1-Dec 31, 2019 (386 ACS) | Jan 1-Dec 31, 2020 (599 ACS) | P value | |
|---|---|---|---|
| STEMI, n (%) | 224 (58) | 328 (54.7) | ns |
| NSTEMI, n (%) | 162 (42) | 271 (45.3) | ns |
| Male, n (%) | 305 (79) | 498 (83) | ns |
| Mean age, years | 66.7±12.4 | 66.9±11.7 | ns |
| Diabetes, n (%) | 39 (10) | 68 (11.5) | ns |
| Smoking, n (%) | 76 (19.7) | 160 (27) | 0.005 |
| Hypertension, n (%) | 162 (41.9) | 245 (40) | ns |
| Dyslipidemia, n (%) | 114 (29.5) | 198 (33) | ns |
| Late presentation, n (%) | 70 (18) | 180 (30) | 0.003 |
| Time from symptoms onset to ER (hrs) | 4.3±2.5 | 11±18.7 | 0.02 |
| Time from ER to PCI (hrs) | 0.5±0.8 | 0.58±2.6 | ns |
| Death, n (%) | 23 (6) | 90 (15) | 0.001 |
STEMI: ST-elevation Myocardial Infarction; NSTEMI: Non-ST-elevation Myocardial Infarction; ER: Eemergency Room; PCI: Percutaneous Coronary Intervention; hrs: hours.
Figure 1.
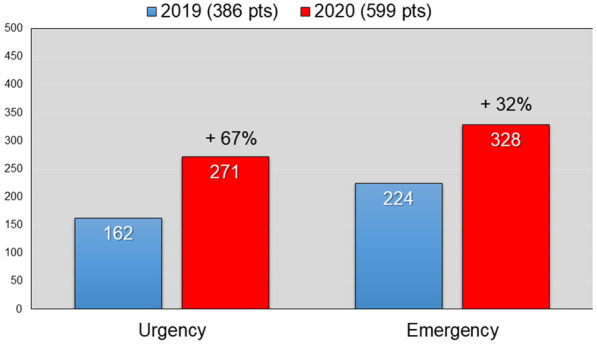
Cumulative increase in emergency (+32%) and urgency (+67%) interventional coronary procedures performed during Covid-19 pandemic outbreaks in 2020 compared to same periods in 2019.
Interestingly, ACS increase in 2020 reached the highest point with a bimodal presentation, paralleling the most contagious outbreak periods (Figure 2). During the 2020 epidemic peak periods, admission times varied over a wider range (mean time 10±16.9 hrs), and overall 30% of STEMI patients presented late (> 8 hrs) from symptoms onset, compared to 18% in 2019 (P=0.003). This delay to first medical contact translated in consequent worse clinical outcomes and fatal mechanical complications leading to higher in-hospital mortality (15% vs. 6% in 2019, P=0.001).
Figure 2.
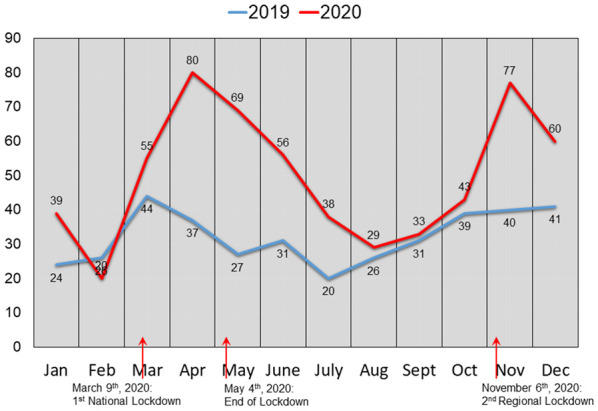
ACS increase in 2020 reached the highest point with a bimodal presentation, paralleling the most contagious outbreak periods (arrows).
Discussion
Our group firstly reported the negative impact of the Covid-19 pandemic on ACS hospitalizations during national lockdowns in Milan, with several ensuing studies confirming similar patterns across the globe [5,6]. According to a previous preliminary report [7], we observed a two-fold longer time from symptom onset to hospital presentation and almost a three-fold higher rate of cardiogenic shock during the COVID-19 outbreak in 2020 when compared with those during the previous year. Widespread fear and emotional stressors are known to precipitate acute coronary syndromes through abnormalities in autonomic tone that can increase platelet aggregation and plaque rupture [8]. Indeed, a cytokine storm associated with SARS-CoV-2 infection has been advocated to play a role in the development of severe lung involvement [9] and acute respiratory distress syndrome, as potent triggers for cardiovascular disease [10,11]. The cytokine storm occurring in COVID-19 patients induces, in concert with the imbalance of the endothelial functions, a massive cell activation with production of platelet-induced Tissue factor, which, together with a sustained platelet activation may be trigger for the hypercoagulable state during COVID-19 disease [12-14]. However, despite these hypothesis, SARS-Cov-2 nasopharyngeal swab or specific antibody (IgM/IgG) tests were found positive in 34 (5.7%) ACS patients only, while a higher ACS mortality rate was reported during this period without being fully explained by Covid-19 cases alone, as recently published [15,16].
This paramount finding outlines that mechanisms other than the ACS itself are at work accounting for the increased overall mortality risk during the Covid-19 pandemic [17]. Anecdotal evidence suggested patients may have been behaving differently during the pandemic by delaying seeking help, resulting in a reduction in demand for emergency department and a rise in adverse outcomes [18], such as out-of-hospital cardiac arrest (OHCA). An increase in incidence of OHCA and number of patients declared deceased on scene has also been reported in France and England [19,20], where disease prevalence has been particularly acute. On one hand, it should be acknowledged that patients’ avoidance of seeking medical care may have led to an underestimation of the ACS-related adverse events and deaths occurring during the pandemic outbreak, as many of these events may have occurred out-of hospital without a formal medical evaluation. Additionally, in areas severely affected by the pandemic increased incidence of OHCA, lower rates of successful resuscitation, and increased mortality have been reported. COVID-19 has significantly impacted patient outcomes through increased disease severity, decreased access to care, and the reshaping of emergency medical response and hospital-based healthcare systems and policies [21,22].
This reduction may have been fuelled by the lockdown and explained by changes in public behaviour and the key government message to ‘stay at home’.
Conclusions
These data reflect how the hospital’s hub function required to reschedule daily activity accordingly, and rewrote criteria to prioritize patients also on regular admissions, resulting in a 20% reduced capability to address the demand of elective invasive procedures, only. Anyhow, this snapshot addresses important insights underlining the need of a healthcare system reassessment in COVID+, COVID-free, which should not forget to protect and reassure with dedicated spaces and paths, those patients in the need of time-sensitive treatments.
Disclosure of conflict of interest
None.
References
- 1.De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omede P, Pennone M, Patti G, Mancone M, De Ferrari GM. Reduced rate of hospital admissions for ACS during covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P ESC Scientific Document Group. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 4.Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP, Gencer B, Hasenfuss G, Kjeldsen K, Lancellotti P, Landmesser U, Mehilli J, Mukherjee D, Storey RF, Windecker S ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-Segment elevation of the European society of cardiology (ESC) Eur Heart J. 2016;37:267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 5.Xiong TY, Redwood S, Prendergast B, Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020;41:1798–1800. doi: 10.1093/eurheartj/ehaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu J, Mamas MA, Mohamed MO, Kwok CS, Roebuck C, Humberstone B, Denwood T, Luescher T, de Belder MA, Deanfield JE, Gale CP. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2021;107:113–119. doi: 10.1136/heartjnl-2020-317912. [DOI] [PubMed] [Google Scholar]
- 7.Trabattoni D, Montorsi P, Merlino L. Late STEMI and NSTEMI patients’ emergency calling in COVID-19 outbreak. Can J Cardiol. 2020;36 doi: 10.1016/j.cjca.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wessler BS, Kent DM, Konstam MA. Fear of coronavirus disease 2019-an emerging cardiac risk. JAMA Cardiol. 2020;5:981–982. doi: 10.1001/jamacardio.2020.2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leisman DE, Ronner L, Pinotti R, Taylor MD, Sinha P, Calfee CS, Hirayama AV, Mastroiani F, Turtle CJ, Harhay MO, Legrand M, Deutschman CS. Cytokine elevation in severe and critical COVID-19: a rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes. Lancet Respir Med. 2020;8:1233–1244. doi: 10.1016/S2213-2600(20)30404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhaskar S, Sinha A, Banach M, Mittoo S, Weissert R, Kass JS, Rajagopal S, Pai AR, Kutty S. Cytokine storm in COVID-19-immunopathological mechanisms, clinical considerations, and therapeutic approaches: the REPROGRAM consortium position paper. Front Immunol. 2020;11:1648. doi: 10.3389/fimmu.2020.01648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evans PC, Rainger GE, Mason JC, Guzik TJ, Osto E, Stamataki Z, Neil D, Hoefer IE, Fragiadaki M, Waltenberger J, Weber C, Bochaton-Piallat ML, Back M. Endothelial dysfunction in COVID-19: a position paper of the ESC working group for atherosclerosis and vascular biology, and the ESC council of basic cardiovascular science. Cardiovasc Res. 2020;116:2177–2184. doi: 10.1093/cvr/cvaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Canzano P, Brambilla M, Porro B, Cosentino N, Tortorici E, Vicini S, Poggio P, Cascella A, Pengo MF, Veglia F, Fiorelli S, Bonomi A, Cavalca V, Trabattoni D, Andreini D, Omodeo Sale E, Parati G, Tremoli E, Camera M. Platelet and endothelial activation as potential mechanisms behind the thrombotic complications of COVID-19 patients. JACC Basic Transl Sci. 2021;6:202–218. doi: 10.1016/j.jacbts.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gabbai-Armelin PR, de Oliveira AB, Ferrisse TM, Sales LS, Barbosa ERO, Miranda ML, Salomao KB, Brighenti FL. Covid-19 (SARS-CoV-2) infection and thrombotic conditions: a systematic review and meta-analysis. Eur J Clin Invest. 2021;51:e13559. doi: 10.1111/eci.13559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mazzeffi MA, Chow JH, Tanaka K. COVID-19 associated hypercoagulability: manifestations, mechanisms, and management. Shock. 2021;55:465–471. doi: 10.1097/SHK.0000000000001660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olivieri A, Palo G, Sebastiani G. COVID-19 cumulative incidence, intensive care, and mortality in Italian regions compared to selected European countries. Int J Infect Dis. 2021;102:363–368. doi: 10.1016/j.ijid.2020.10.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rashid M, Wu J, Timmis A, Curzen N, Clarke S, Zaman A, Nolan J, Shoaib A, Mohamed MO, de Belder MA, Deanfield J, Gale CP, Mamas MA. Outcomes of COVID-19-positive acute coronary syndrome patients: a multisource electronic healthcare records study from England. J Intern Med. 2021 doi: 10.1111/joim.13246. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gallo E, Prosepe I, Lorenzoni G, Acar AS, Lanera C, Berchialla P, Azzolina D, Gregori D. Excess of all-cause mortality is only partially explained by COVID-19 in Veneto (Italy) during spring outbreak. BMC Public Health. 2021;21:797. doi: 10.1186/s12889-021-10832-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Handberry M, Bull-Otterson L, Dai M, Mann CN, Chaney E, Ratto J, Horiuchi K, Siza C, Kulkarni A, Gundlapalli AV, Boehmer TK. Changes in Emergency Medical Services before and during COVID-19 in the United States, January 2018-December 2020. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab373. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, Sharifzadehgan A, Waldmann V, Beganton F, Narayanan K, Lafont A, Bougouin W, Jouven X. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Charlton K, Limmer M, Moore H. Incidence of emergency calls and out-of-hospital cardiac arrest deaths during the COVID-19 pandemic: findings from a cross-sectional study in a UK ambulance service. Emerg Med J. 2021;38:446–449. doi: 10.1136/emermed-2020-210291. [DOI] [PubMed] [Google Scholar]
- 21.Ong J, O’Connell F, Mazer-Amirshahi M, Pourmand A. An international perspective of out-of-hospital cardiac arrest and cardiopulmonary resuscitation during the COVID-19 pandemic. Am J Emerg Med. 2021;47:192–197. doi: 10.1016/j.ajem.2021.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kovach CP, Perman SM. Impact of the COVID-19 pandemic on cardiac arrest systems of care. Curr Opin Crit Care. 2021;27:239–245. doi: 10.1097/MCC.0000000000000817. [DOI] [PMC free article] [PubMed] [Google Scholar]


