Abstract
Obstructive sleep apnea (OSA) is characterized by repeated episodes of intermittent hypoxia (IH) and is recognized as an independent risk factor for vascular diseases that are mediated by a multitude of mechanistic pathophysiological cascades including procoagulant factors. The pro-coagulant state contributes to the development of blood clots and to the increase in the permeability of the blood–brain barrier (BBB). Such alteration of BBB may alter brain function and increase the risk of neurodegenerative diseases. We aim to provide a narrative review of the relationship between the hypercoagulable state, observed in OSA and characterized by increased coagulation factor activity, as well as platelet activation, and the underlying neural dysfunction, as related to disruption of the BBB. We aim to provide a critical overview of the existing evidence about the effect of OSA on the coagulation balance (characterized by increased coagulation factor activity and platelet activation) as on the BBB. Then, we will present the emerging data on the effect of BBB disruption on the risk of underlying neural dysfunction. Finally, we will discuss the potential of OSA therapy on the coagulation balance and the improvement of BBB.
Keywords: obstructive sleep apnea (OSA), coagulation, blood–brain barrier, procoagulant states, neurodegenerative diseases
1. Introduction
Obstructive sleep apnea (OSA) is a highly prevalent medical disease that imposes large arrays with adverse socioeconomic impacts, particularly in developed countries [1]. It affects, albeit differently, both sexes and all age groups in the population. Middle-aged patients with OSA who are also evaluated at high risk for cardiovascular diseases are a particularly important group to diagnose and treat in light of their uniquely elevated risk of both cardiovascular and cerebrovascular morbidity and mortality [2]. In this high-risk group, there also appears to be a significant and independent association between OSA and cognitive complaints, as well as neurodegenerative diseases [3,4].
According to the World Health Organization, about 18 million people will die each year due to cardiovascular diseases (CVD), accounting for 31% of all deaths around the world [5]. Thrombosis, due to an abnormally activated coagulation cascade, is an important part of their pathophysiological mechanisms [6,7]. In parallel with the prominent role played by CVD, an overview of the studies performed to date clearly shows a significant relationship between untreated, severe OSA and all-cause mortality [8].
The changes in coagulation balance observed in OSA could have potential consequences on the cardiovascular system but may also directly affect the brain [9]. Increased activity of clotting factors and platelets may also negatively impact the blood–brain barrier (BBB) by an increase in its permeability [10,11]. As a result, compounds that are potentially harmful to the brain and usually blocked by the BBB may contribute to the development or worsening of neurodegenerative diseases [12].
Based on the aforementioned considerations, this paper aims to provide a comprehensive narrative review of the potential links between OSA, abnormally activated coagulation, and platelets, as their potential consequences on the brain, because of BBB disruption.
2. OSA: Definition, Clinical Consequences, and Treatments
Among the vast spectrum of sleep-related breathing disorders (SRBD), OSA is the most frequent condition. A recent study has estimated that nearly a billion people worldwide suffer from OSA [13]. OSA is characterized by recurrent obstruction of the upper airway during sleep leading to either apnea (cessation of airflow) or hypopnea (substantial decrease of the airflow with consequent oxyhemoglobin desaturation and/or electroencephalographic arousal). These apneas/hypopneas lead to sleep fragmentation and its downstream daytime functional consequences. The severity of the disease is reported using the apnea and hypopnea index (AHI), i.e., the number of respiratory events per hour of sleep.
The dominant nocturnal symptom of OSA is snoring with a prevalence of 75–90% in OSA patients [14]. Furthermore, nocturnal symptoms can also include apnea observed by bed partners, paroxysmal dyspnoea, frequent awakenings, excessive perspiration, restlessness, and nightmares. Daytime symptoms characteristically consist of excessive sleepiness and unexplained fatigue. Moreover, patients report morning headaches (12–18%), dryness of the oral mucous membranes, impairment of cognitive functions [15], recurrent problems with memory and concentration, mood deterioration, and a tendency towards depressive symptoms [16].
Repeated episodes of hypoxia–reoxygenation in these patients promote oxidative stress, which is the result of excessive production of reactive oxygen species (ROS). Moreover, oxidative stress is involved in the regulation of cellular transcription through the activation of transcription factors such as HIF-1 (hypoxia-inducible factor-1), which is activated by hypoxia and is responsible for the activation of several genes, including vascular endothelial growth factor (VEGF) [17]. Indeed, high serum levels of HIF-1α protein are compatible with the diagnosis of OSA, whereas low levels may exclude severe OSA with high probability [18]. HIF-1 α can also stimulate the transcription factor NF-κB involved in the regulation of inflammatory responses [19]. Stimulation of systemic inflammatory pathways favors the induction of endothelial dysfunction, increased blood coagulability, insulin resistance, activation of monocytes and macrophages fostering the development of atherosclerosis, as well as stimulation of the renin–angiotensin–aldosterone system [20].
Overnight polysomnography remains the “gold standard” for the diagnosis of OSA, even if ambulatory polysomnography and particularly respiratory polygraphic recordings have superseded in-lab studies in general clinical practice [21].
Current therapies for OSA, such as continuous positive airway pressure (CPAP) and oral appliances, have relatively poor long-term adherence as well as variable efficacy. The risk:benefit ratio of such interventions for cardiovascular event prevention (primary or secondary) is still under debate, with randomized clinical studies yielding negative results [22,23]. However, in stroke secondary prevention, the efficacy of CPAP is well recognized when the mean night CPAP treatment duration is 4 > h/night [24]. When patients have mild to moderate sleep apnea and CPAP is frequently poorly tolerated, an endo-buccal device may be an alternative treatment. This is a so-called advancement or retention mandibular orthosis that holds the tongue and lower jaw forward, thus facilitating the retropharyngeal airflow passage [25]. This treatment is less restrictive, but also less effective, than CPAP for severe forms of the syndrome. Other treatments exist, such as surgery, to increase the cross-sectional area of the upper airways by removing excess tissue or advancing the upper and lower jaws [26]. Moreover, bilevel positive airway pressure (BiPAP) is a better option for some people. This noninvasive ventilation treatment delivers an adaptative inspiratory pressure and an expiratory pressure level [27]. The search for novel therapeutic approaches for OSA, including pharmacological agents, has been actively pursued over the past years, further highlighting the importance of cell or animal models of OSA, their applicability, and limitations [28].
3. OSA and the “Hypercoagulable State”
OSA increases the risk of cardiovascular diseases via different pathways, including oxidative stress, inflammation, and coagulation abnormalities. Hypoxia can directly activate clotting [29], especially in IH, such as occurs in chronic obstructive pulmonary disease exacerbations [30,31,32]. Furthermore, in some patients with heart failure, the vascular endothelium seems to have procoagulant properties [33]. In patients with OSA, several factors are altered, including hematocrit [34] and blood viscosity [35,36,37], but these two are not linked to BBB damage. Thus, in this section, we will delineate the main factors affected during OSA that are involved in the alteration of the BBB.
3.1. Factors Contributing to a Procoagulant State in OSA
3.1.1. Clotting Factors
The thrombin–antithrombin (TAT) complex is formed in response to a high level of thrombin suggesting increased coagulation. Thus, the TAT complex is a good indicator for measuring the level of thrombin in the blood. Several studies [38,39], including one randomized study with 220 patients who suffered from OSA [38], have demonstrated that levels of TAT were higher in patients with OSA.
Other important clotting factors are factors VII (FVIIa) and XII (FXIIa). They are essential components of the coagulation cascade. Interestingly, both FVIIa [40] and FXIIa [41,42] have been associated with an increase in arterial disease, and elevated levels of these factors have been reported in randomized trials in patients with OSA [38,43] and might account for high cardiovascular morbidity of OSA.
Fibrinogen is also a major coagulation protein; once converted into fibrin, it allows for clot formation and influences platelet aggregation. Thus, fibrinogen levels appear to be an important risk factor for cardiovascular disease [44,45]. Various studies have found that fibrinogen is increased in patients with OSA [35,46,47,48,49,50,51] and circulating fibrinogen levels are linearly correlated with AHI in different case–control studies [52,53,54,55].
3.1.2. Platelets
Platelets are a blood component whose major function is to agglutinate during a blood vessel injury, triggering the formation of a blood clot to stop the bleeding. After the adhesion of platelets to the endothelium, platelet activation is observed. Platelets contain many cell adhesion and inflammatory factors that can be released when they are activated, including soluble CD40 ligand (sCD40L) and P-selectin. In different studies, subjects with OSA have found platelet activity to be increased in these patients [56,57,58] and correlated with an increase in sCD40L [59,60,61] and P-selectin [62,63,64,65] levels. A few minutes after activation, platelet aggregation is observed. During this stage, several factors are released, including platelet-activating factor (PAF) and adenosine diphosphate (ADP), both of which contribute to the maintenance of platelet aggregation. In patients with OSA, platelet aggregation is increased in nonrandomized studies [46,57,66,67,68], particularly induced by an increase of ADP [67,69]. In an in vitro model study, hypoxia–reoxygenation (H/R) induced increases in PAF levels [70]. In a mouse model of OSA, transgenic mice that were deficient in the cell surface receptor for PAF (PAFR-/-) showed attenuated elevations of inflammatory signaling [71]. It would therefore appear that a coordinated activity of all these elements contributes to the development and propagation of thrombotic phenomena in the context of OSA [72]. Given their involvement in inflammation, several data confirm that blood platelets in OSA patients are a therapeutic target to reduce the risk of cardiovascular disease [17].
3.1.3. Von Willebrand Factor
Von Willebrand factor (VWF) is an adhesion molecule that circulates in plasma and has a central role in primary hemostasis. It mediates platelet adhesion during vascular injury and allows the transport and stabilization of circulating factor VIII [73]. Although some studies show no differences between healthy subjects and OSA patients [38,74], more recent studies have shown a significant increase in VWF in sleep apnea [49,75,76,77].
Notwithstanding, it is important to emphasize that there are many confounding factors that cooccur among OSA patients, such as hypertension, diabetes, smoking, and obesity, all of which can also directly affect the blood clotting system. Thus, based on the extant evidence, it is possible that OSA may accelerate this process.
3.2. Effects of CPAP on Coagulation Balance
The effect of CPAP on the hypercoagulable state associated with OSA has been evaluated in numerous biological studies. CPAP treatment was accompanied by a decrease in FVII [43], fibrinogen [43,46], and VWF (57). However, no beneficial effects were observed regarding factor XII [38] and thrombin [38]. Concerning platelet activation, a significant decrease in sCD40L [59,61] and P-selectin [63] was observed. Platelet aggregation also decreased in several studies [46,66,67] (see Table 1). The clinical impact of such improvement is still poorly evaluated. Moreover, as with any treatment, the beneficial effects of CPAP are intimately related and dependent on adherence, the impact of possible comorbidities, as well as on the underlying severity of OSA. Moreover, they could come in part from the chronic restoration of a normal nocturnal respiratory function.
Table 1.
Hemorheological and coagulation findings in obstructive sleep apnea (OSA) and the effect of continuous positive airway pressure (CPAP).
| Increased Factors in Osa | Authors | Type of Study—Subjects | CPAP Used? (>4 hours/night) Effects |
|---|---|---|---|
| FVII and FXII | Chin, 1998 [43] | Nonrandomized, controlled trial—15 males with OSA | Yes, decreased FVII levels after six months of CPAP |
| Robinson, 2004 [38] | Randomized controlled trial—220 patients with OSA | Yes, no effects on FVII or FVIIa levels after one month CPAP | |
| Thrombin | Robinson, 2004 [38] | Randomized controlled trial—220 patients with OSA | Yes, no effects on thrombin levels after one month |
| Von Kanel, 2005 [39] | Uncontrolled intervention study—32 patients with OSA | No | |
| Fibrinogen | Bouloukaki, 2017 [55] | Cross-sectional study—858 patients with OSA | No |
| Chin, 1998 [43] | Uncontrolled intervention study—11 patients with OSA | Yes, decreased in fibrinogen levels after one night | |
| Comondore, 2009 [48] | Randomized crossover trial—13 patients with OSA | Yes, no effects in fibrinogen after 4 weeks CPAP | |
| Hizli, 2020 [50] | Randomized crossover trial—126 patients with OSA | No | |
| Mehra, 2010 [51] | Cross-sectional study—537 patients with OSA | No | |
| Nobili, 2000 [47] | Case-control study—12 patients with OSA | No | |
| Reinhart, 2002 [35] | Case-control study—13 patients with OSA | Yes, no effects in fibrinogen level after one night | |
| Shamsuzzaman, 2014 [54] | Case-control study—36 men with OSA | No | |
| Steiner, 2005 [52] | Case-control study—63 patients with OSA | No | |
| Von Kanel, 2016 [49] | Longitudinal study—329 patients with OSA | No | |
| Wessendorf, 2000 [53] | Case-control study—69 patients with OSA | No | |
| Zhang, 2003 [46] | Nonrandomized—41 patients with OSA | Yes, decreased in fibrinogen levels, after 30 days CPAP | |
| Platelet activation | Bokinsky, 1995 [57] | Non-randomized study—6 patients with OSA | Yes, no effects |
| Geiser, 2002 [56] | Case-control study—12 patients with OSA | No | |
| sCD40L | Akinnusi, 2009 [59] | Non-randomized study—12 patients with OSA | Yes, decreased in sCD40L after 8 weeks |
| Kobayashi, 2006 [61] | Case-control study—35 patients with OSA | Yes, decreased in sCD40L after 1 night | |
| Kosacka, 2015 [60] | Case-control study—79 OSA patients | No | |
| P-selectin | Cofta, 2013 [62] | Group comparaison study—80 patients with OSA | No |
| Horváth, 2020 [64] | Case-control study—51 patients with OSA | No | |
| Shimizu, 2002 [63] | Non-randomized study—94 patients with OSA | Yes, decreased in P-selectin after 1 month | |
| Winiarska, 2020 [65] | Group comparaison study—48 patients with OSA | No | |
| Platelet aggregation | Bokinsky, 1995 [57] | Non-randomized study—6 patients with OSA | Yes, no effects |
| Sanner, 2000 [66] | Non-randomized study—17 patients with OSA | Yes, decreased after 6 months | |
| Zhang, 2003 [46] | Non-randomized study—41 patients with OSA | Yes, decreased after 30 days | |
| Kontos, 2020 [68] | Non-randomized study—30 children with SDB | No | |
| ADP | Alkhiary, 2017 [69] | Case-control study—64 patients with OSA | No |
| Oga, 2009 [67] | Non-randomized study—58 patients with OSA | Yes, decreased in platelet aggregation | |
| VWF | El Solh, 2008 [76] | Non-randomized study—35 patients with OSA | No |
| Phillips, 2012 [77] | Randomized, placebo-controlled crossover study—28 patients | Yes, decreased in VWF level after 2 months | |
| Von Kanel, 2007 [75] | Cross-sectional study—135 patients | No | |
| Von Kanel, 2016 [49] | Longitudinal study—329 patients with OSA | No |
ADP: adenosine diphosphate, PAF: platelet-activating factor, sCD40L: soluble CD40 ligand, vWF: von Willebrand factor.
4. Impact of OSA on BBB
4.1. Blood–Brain Barrier
A recent review and other studies have shown that the blood–brain barrier (BBB) could be altered by several mechanisms that are present during OSA [78,79,80]. The BBB secludes the brain from the undesired transfer of substances that may be in the bloodstream while allowing the passage of nutrients that are essential for brain function. This protective barrier is constituted by several elements that are essential for maintaining the tightness between the capillary and the cerebral space, as well as regulate the transport between these two compartments. Among these elements, endothelial cells, astrocytes, pericytes, and neurons account for the most important [78]. Endothelial cells are held together by tight junctions (TJs), which create a paracellular barrier of high resistance to limit permeability. The transmembrane proteins that make up the TJs (zonula occludens (ZO)-1, claudin-5, etc.) limit the paracellular transfer of molecules. TJs also interact with adherent basal junctions (e.g., vascular endothelial cadherin) to strengthen the interactions between endothelial cells [81].
Many polarized metabolites enter the brain by facilitated diffusion. However, the BBB also has an exceptional ability to protect the brain from potentially toxic xenobiotics and metabolites through efflux transporters. For this reason, endothelial cells also express transport proteins such as ATP binding cassette (ABC) transporters [82]. These proteins are mainly located on the luminal membrane of the brain microvessels and they recognize a wide range of different substrates, allowing them to be transported from the central nervous system (CNS) to the bloodstream. They include P-glycoprotein, breast cancer resistance protein, and multidrug resistance proteins [82]. All those microstructural cell elements are essential to ensure the integrity of the BBB.
Dysfunction of the BBB will lead to an increase in membrane permeability and the potential entry of cells and molecules into CNS, resulting in neuronal dysfunction and degeneration [83].
4.2. OSA: Adverse Effects on BBB Function
Alterations in BBB in the context of OSA are thought to promote the emergence of cognitive impairments and may be associated with several neurodegenerative diseases [78].
Oxidative stress, as induced by OSA, is characterized by increases in ROS generation and propagation and causing reducing nitric oxide production [84]. In addition to oxidative stress, another pathway through which IH can alter cell function is via changes in molecular oxygen sensors. Indeed, HIF-1α transcription is stabilized during the early stages of IH [85], and its binging to the promoter regions of regulated genes enhances the transcription of such genes, which are involved in various biological processes such as inflammation or cancer [78]. Furthermore, chronic inflammation may occur in the BBB in response to IH and act as another mechanism leading to cognitive impairments. IH results in the activation of the transcription factor NFκB [86] and other transcription factors underlying immune responses, resulting in increased levels of proinflammatory cytokines among OSA patients [87,88].
The consequences of the aforementioned process on the BBB are multiple and are primarily characterized by changes in the permeability of the BBB capillary network, as well as modifications in ABC transporters [78]. There is also leakage through the paracellular pathway and therefore through TJs [78]. Studies in mice exposed to IH have shown increases in parenchymal water in the brain, as well as alterations in aquaporin expression, leading to increased permeability of the BBB [89]. Changes in the permeability of the BBB were also inferred from studies in adult patients with OSA [90].
Very recent studies have shown that endothelial cells secrete exosomes and that endothelial cells can also be targeted by exosomes derived from different cell types. Exosomes are a class of very small extracellular vesicles, with a diameter of 30–100 nanometers [91]. It is now recognized that stress conditions can disrupt the endothelial TJs of the brain and affect cognition via exosome-related biological activities [92]. Recently, Khalyfa et al. [93] demonstrated that extracellular vesicles (EVs) (including exosomes) are increased in the plasma of children with OSA. These EVs disrupt the integrity of the BBB by imposing adverse effects on the integrity of the monolayer of the endothelial barrier while also disrupting the TJ structure.
4.3. Hypercoagulability and Possible Effects on BBB
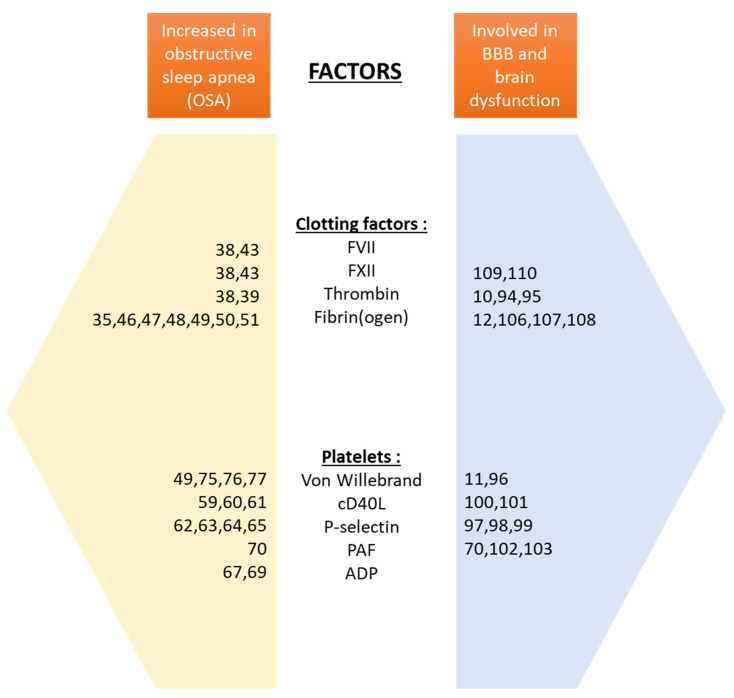
Currently, we are unaware of any studies establishing a direct link between OSA, a prothrombotic state, and alterations in BBB function and structure. However, several studies involving conditions unrelated to OSA have demonstrated an alteration of the BBB when the concentrations of procoagulant factors are increased (see Figure 1).
Figure 1.
Summary of the major studies investigating the factors increased during obstructive sleep apnea (OSA) and factors involved in blood–brain barrier (BBB)–brain dysfunction. ADP: adenosine diphosphate, PAF: platelet-activating factor, cD40L: cD40 ligand.
In a study evaluating biomarkers leading to BBB dysfunction in cognitively impaired patients, serum thrombin levels were found to be abnormally elevated. The direct effects of this molecule on the integrity of the BBB were tested in vitro using microvascular endothelial cells. The permeability of the BBB was altered, demonstrating the role of thrombin and its ability to disrupt BBB function [10]. In adults rats, thrombin injection resulted in disruption of brain microvascular endothelial cells and the BBB, as evidenced by increased permeability of the BBB and increased brain water content [94]. Another study showed that after the injection of thrombin into the basal ganglia in rats, there was a significant increase in the expression of matrix metalloproteinases, which are involved in the disruption of the BBB. This perturbation of the BBB is then associated with the formation of CNS edema in this experimental model [95].
VWF is also known to alter the BBB. In a mouse model subjected to hypoxia–reoxygenation (H/R) episodes, VWF deficiency showed an increased expression of claudin-5 in endothelial cells. VWF deficiency thus confers partial preservation of the integrity of the BBB after H/R [96]. Another study identified a critical role of VWF in brain inflammation associated with altered BBB after intracerebral hemorrhage. On the other hand, antibodies blocking VWF allowed limiting the lesions observed after hemorrhage [11].
Over-activated platelets, including the multiple factors they secrete, also play a significant role in BBB damage. Soluble P-selectin (sP-selectin) is a biomarker of platelet activation and is considered a risk factor for vascular disease. One study used a mouse model in which the endogenous P-selectin gene was replaced by a mutant that produces abnormally high plasma levels of sP-selectin. These mice then showed a higher permeability of the BBB that was associated with a higher risk of brain infarction and with the development of atherosclerotic lesions [97]. The increase in sP-selectin in these mice was also associated with shorter plasma clotting times and increased fibrin deposition on platelet thrombi, reflecting a procoagulant phenotype. Moreover, increased fibrin deposition in the brain in a mouse model of Alzheimer’s disease (AD) has been found to be associated with increased BBB permeability [98]. Another study confirmed that P-selectin expression contributed to early BBB dysfunction after stroke by using multimodality imaging approaches consisting of molecular magnetic resonance imaging and immunohistochemistry [99].
A study looking at the potential effects of sCD40L on the BBB used an in vitro model of human brain microvascular endothelial cells. The permeability of the cellular monolayer in this model was increased by the administration of sCD40L. Thus, sCD40L induces more severe inflammation of the CNS by disrupting the BBB [100]. Another study revealed that sCD40L levels were elevated in the circulation of HIV-infected and cognitively impaired individuals, compared to controls. Using microscopy and quantitative analyses in CD40L-deficient wild-type mice, it was found that the HIV trans-activator of transcription (Tat) can induce increased permeability of the BBB in a CD40L-dependent manner. The increased BBB permeability was found to be the consequence of abnormal platelet activation induced by Tat since pretreatment platelet depletion reversed the effects on BBB permeability [101].
In an in vitro study of the BBB consisting of rat brain microvessel-derived endothelial cells (RBMEC), an increase in PAF was demonstrated after H/R episodes. This increase was associated with endothelial cell damage. In addition, pretreatment with a PAF inhibitor suppressed the deleterious effects of PAF, leading to a protective effect on the BBB [70]. Moreover, immunohistochemical studies on RBMEC revealed that PAF reduced the immunostaining of ZO-1 (tight-junction-associated protein), increased F-actin fibers, creating leakage through the paracellular pathway [102]. In vivo studies have also indicated that PAF increases the permeability of BBB, as evaluated by sodium fluorescein and Evans blue methods [102]. Finally, intravenous infusion of PAF induced a transient opening of the BBB in rats, as reflected by an increased leakage of Evans blue and slight brain edema formation. PAF may also induce a transient and reversible opening of the BBB by a sharp decrease in regional cerebral blood flow [103].
Taken together, these studies show that a variety of procoagulant factors alter the permeability of the BBB via activation of multiple mechanisms, all of which may be relevant for inflammatory disorders of the CNS as well as deleterious to cognitive functioning.
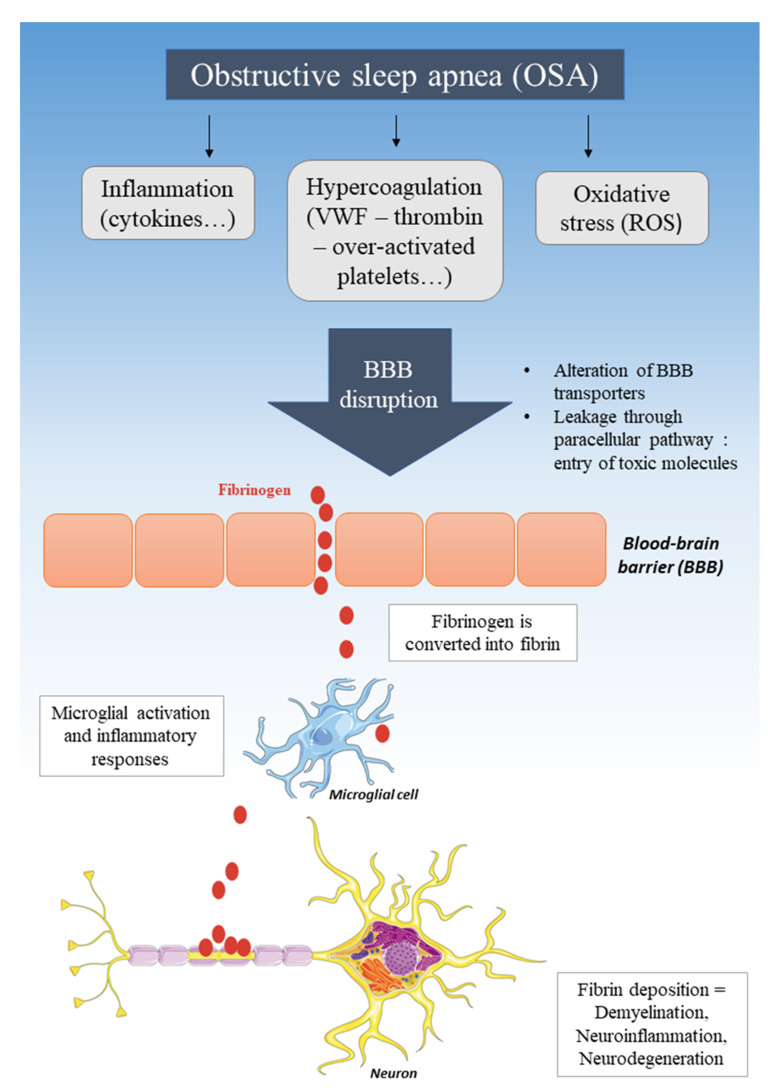
4.4. BBB Disruption, Entry of Fibrinogen, and Neurodegenerative Diseases
Numerous studies have shown significant associations between neurodegenerative diseases and OSA. Indeed, in patients suffering from multiple sclerosis (MS) [104] or Alzheimer’s [105], the risk of OSA seems to be high. Numerous studies have suggested that after the BBB is disrupted, fibrinogen comes into contact with the white matter. Then, under those conditions, fibrinogen is converted to fibrin plaques and is then deposited on the CNS tissue. Fibrin induces neuroinflammation by activating microglia and by promoting the recruitment, migration, and activation of peripheral inflammatory macrophages [106]. The appearance of these fibrin plaques and the inflammatory cells that infiltrate the brain after a breach of the BBB is then associated with demyelination and neuronal dysfunction observed in these neurodegenerative diseases [12,107,108] (see Figure 2).
Figure 2.
Pathogenic mechanism of obstructive sleep apnea (OSA) leading to blood–brain barrier (BBB) disruption and neurodegeneration. ROS: reactive oxygen species, VWF: von Willebrand factor.
Several studies showed that this conversion of fibrinogen is possible through factor XII. In a mouse model of AD, FXII plays a key role in inflammatory-mediated neuronal damage and cognitive impairments [109]. In addition, similar to fibrinogen depletion, FXII depletion decreases neuroinflammatory responses and the resulting brain pathology [110].
Moreover, recent studies have indicated that REM-sleep-related apnea/hypopnea without atonia is very common in OSA and may represent an increased risk for neurodegenerative disease [4].
5. Potential Therapies
OSA has been identified as an independent risk factor for a large number of diseases. Among these, acute coronary syndrome (ACS) [111], atrial fibrillation (AF) [112,113], stroke [114], and venous thromboembolism (VTE) [115,116] are prominently represented.
As previously discussed, OSA is associated with an increased level of platelet volume indices and with platelet reactivity linked to the AHI index [111,117]. These findings may have direct involvement in the elevated prevalence of ischemic complications among ACS patients with OSA. In ACS patients with OSA, dual aspirin and clopidogrel therapy may be effective in reducing thromboembolic complications. However, in a clinical trial, there was a reduction in the antiplatelet effects induced by clopidogrel and a greater occurrence of high residual platelet reactivity during treatment in apneic patients [111]. These findings may explain why some ACS patients with OSA have a worse clinical prognosis than those in whom OSA is not present, suggesting the need to differentiate ACS patients with and without OSA for improved precision therapeutics [111]. In addition, patients with OSA required a significantly higher dose of warfarin than their non-OSA counterparts to limit the risk of recurrent pulmonary embolism [118].
In addition, in preclinical studies, dabigatran, apixaban, and rivaroxaban demonstrated a decrease in the opening of the BBB in cases of vascular dysfunction such as bleeding conditions [119,120,121,122,123]. Based on these results, several authors posited that such treatments may promote the preservation of cognitive function. AD and OSA show similarities in vascular dysfunction that contribute to dementia and cognitive impairments, including disruption of the BBB [124]. Several preclinical studies have demonstrated that the use of dabigatran, a direct thrombin inhibitor may be beneficial in AD, and could also be of value as adjuvant therapy in OSA patients manifesting cognitive dysfunction. In AD mice, long-term use of dabigatran has been shown to preserve memory and brain perfusion with an improvement in the integrity of the BBB [125]. These positive effects are associated with decreased levels of fibrin, amyloid deposition, and neuroinflammatory activity in the brains of these mice [125].
6. Conclusions
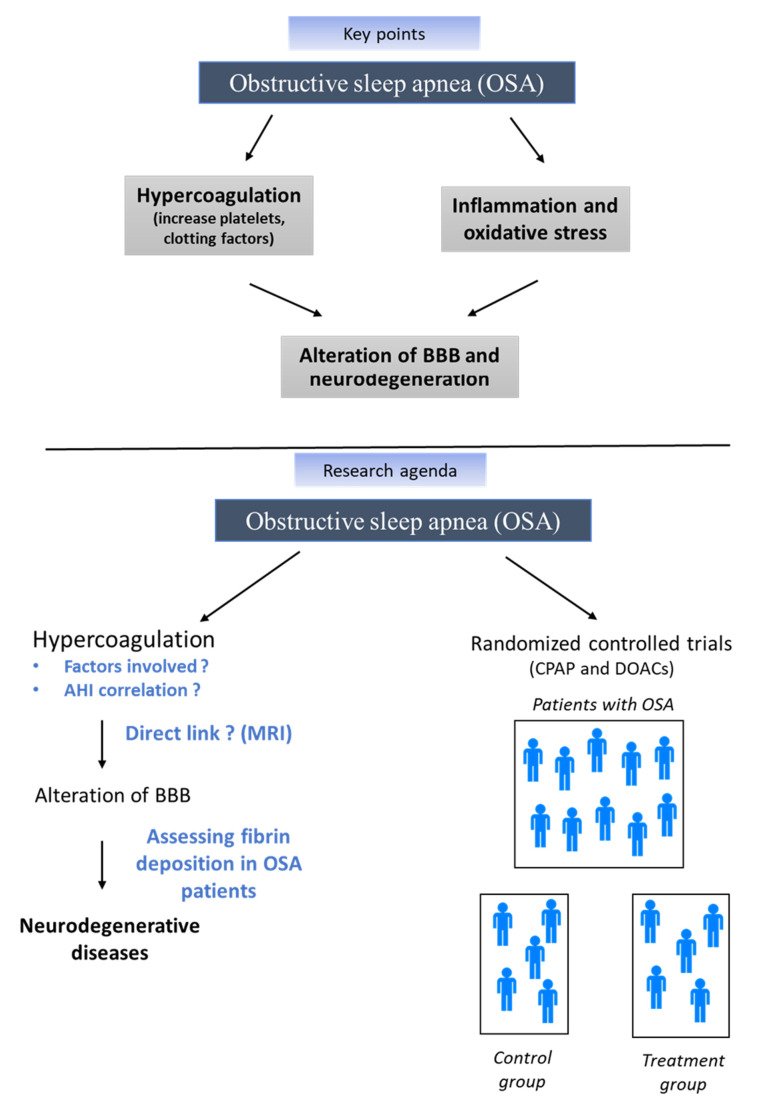
We have summarized the evidence showing that OSA may promote a prothrombotic state that can lead to BBB damage. Oxidative stress, inflammation, and hypercoagulation pathways generated by OSA are not inconsequential and can all lead to an alteration of the BBB. We have further highlighted a disruption of the BBB in the context of increased concentrations of procoagulant factors, which then facilitate the entry of compounds potentially damaging to the brain, such as fibrinogen, deposition of fibrin on neurons, ultimately promoting accelerated neurodegeneration, as found in several diseases such as AD or MS. OSA is an eminently complex chronic disease associated with different phenotypes and therefore is involved in subsequent complications and increased risk of neurodegenerative diseases, which vary greatly from one patient to another. Then, it is important to note that a multiplicity of factors interact in OSA patients to create hypercoagulable and proinflammatory states that could influence BBB disruption and thus increase the risk of such neurodegenerative diseases. Thus, both individual factors and differences (demographic, genetic, and other early life risk markers) [126], modifiable risk factors (mood, sleep, diet, and lifestyle), and other vascular comorbidities that have been separately associated with downstream risk of hypercoagulable states should be considered in future studies. This detailed individual risk assessment will undoubtedly be a key element in the predictive medicine of tomorrow in OSA [127]. This will undoubtedly help the clinician to choose the most suitable treatment for OSA but also complementary drug therapies. For this reason, further studies need to be conducted to investigate the direct impact of OSA associated with hypercoagulation on brain tissue and to evaluate the impact of CPAP on the occurrence of thrombotic and cerebral pathologies (see Figure 3).
Figure 3.
Key points and future directions, AHI: apnea–hypopnea index, BBB: blood–brain barrier, CPAP: continuous positive airway pressure, MRI: magnetic resonance imaging, OSA: obstructive sleep apnea.
Funding
DG is supported by NIH grant AG061824, by the Leda J. Sears Foundation, and by Tier 2 and TRIUMPH grants from the University of Missouri.
Conflicts of Interest
The authors have no relevant conflict of interest to declare in relation to the content of this manuscript.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Senaratna C.V., Perret J.L., Lodge C.J., Lowe A.J., Campbell B.E., Matheson M.C., Hamilton G.S., Dharmage S.C. Prevalence of Obstructive Sleep Apnea in the General Population: A Systematic Review. Sleep Med. Rev. 2017;34:70–81. doi: 10.1016/j.smrv.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 2.Bonsignore M.R., Baiamonte P., Mazzuca E., Castrogiovanni A., Marrone O. Obstructive Sleep Apnea and Comorbidities: A Dangerous Liaison. Multidiscip. Respir. Med. 2019;14:8. doi: 10.1186/s40248-019-0172-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bahia C.M.C.D.S., Pereira J.S. Obstructive Sleep Apnea and Neurodegenerative Diseases: A Bidirectional Relation. Dement. Neuropsychol. 2015;9:9–15. doi: 10.1590/S1980-57642015DN91000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lajoie A.C., Lafontaine A.-L., Kimoff R.J., Kaminska M. Obstructive Sleep Apnea in Neurodegenerative Disorders: Current Evidence in Support of Benefit from Sleep Apnea Treatment. J. Clin. Med. 2020;9:297. doi: 10.3390/jcm9020297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cardiovascular Diseases. [(accessed on 26 April 2020)]; Available online: https://www.who.int/westernpacific/health-topics/cardiovascular-diseases.
- 6.Obermayer G., Afonyushkin T., Binder C.J. Oxidized Low-Density Lipoprotein in Inflammation-Driven Thrombosis. J. Thromb. Haemost. 2018;16:418–428. doi: 10.1111/jth.13925. [DOI] [PubMed] [Google Scholar]
- 7.Blokhin I.O., Lentz S.R. Mechanisms of Thrombosis in Obesity. Curr. Opin. Hematol. 2013;20:437–444. doi: 10.1097/MOH.0b013e3283634443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Punjabi N.M., Caffo B.S., Goodwin J.L., Gottlieb D.J., Newman A.B., O’Connor G.T., Rapoport D.M., Redline S., Resnick H.E., Robbins J.A., et al. Sleep-Disordered Breathing and Mortality: A Prospective Cohort Study. PLoS Med. 2009;6:e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toraldo D.M., Peverini F., De Benedetto M., De Nuccio F. Obstructive Sleep Apnea Syndrome: Blood Viscosity, Blood Coagulation Abnormalities, and Early Atherosclerosis. Lung. 2013;191:1–7. doi: 10.1007/s00408-012-9427-3. [DOI] [PubMed] [Google Scholar]
- 10.Festoff B.W., Sajja R.K., van Dreden P., Cucullo L. HMGB1 and Thrombin Mediate the Blood-Brain Barrier Dysfunction Acting as Biomarkers of Neuroinflammation and Progression to Neurodegeneration in Alzheimer’s Disease. J. Neuroinflamm. 2016;13:194. doi: 10.1186/s12974-016-0670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhu X., Cao Y., Wei L., Cai P., Xu H., Luo H., Bai X., Lu L., Liu J.-R., Fan W., et al. Von Willebrand Factor Contributes to Poor Outcome in a Mouse Model of Intracerebral Haemorrhage. Sci. Rep. 2016;6:35901. doi: 10.1038/srep35901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petersen M.A., Ryu J.K., Akassoglou K. Fibrinogen in Neurological Diseases: Mechanisms, Imaging and Therapeutics. Nat. Rev. Neurosci. 2018;19:283–301. doi: 10.1038/nrn.2018.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benjafield A.V., Ayas N.T., Eastwood P.R., Heinzer R., Ip M.S.M., Morrell M.J., Nunez C.M., Patel S.R., Penzel T., Pépin J.-L., et al. Estimation of the Global Prevalence and Burden of Obstructive Sleep Apnoea: A Literature-Based Analysis. Lancet Respir. Med. 2019;7:687–698. doi: 10.1016/S2213-2600(19)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heinzer R., Vat S., Marques-Vidal P., Marti-Soler H., Andries D., Tobback N., Mooser V., Preisig M., Malhotra A., Waeber G., et al. Prevalence of Sleep-Disordered Breathing in the General Population: The HypnoLaus Study. Lancet Respir. Med. 2015;3:310–318. doi: 10.1016/S2213-2600(15)00043-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martin M.S., Sforza E., Roche F., Barthélémy J.C., Thomas-Anterion C. PROOF study group Sleep Breathing Disorders and Cognitive Function in the Elderly: An 8-Year Follow-up Study. The Proof-Synapse Cohort. Sleep. 2015;38:179–187. doi: 10.5665/sleep.4392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sforza E., Saint Martin M., Barthélémy J.C., Roche F. Mood Disorders in Healthy Elderly with Obstructive Sleep Apnea: A Gender Effect. Sleep Med. 2016;19:57–62. doi: 10.1016/j.sleep.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 17.Gabryelska A., Łukasik Z.M., Makowska J.S., Białasiewicz P. Obstructive Sleep Apnea: From Intermittent Hypoxia to Cardiovascular Complications via Blood Platelets. Front. Neurol. 2018;9:635. doi: 10.3389/fneur.2018.00635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gabryelska A., Szmyd B., Panek M., Szemraj J., Kuna P., Białasiewicz P. Serum Hypoxia-Inducible Factor-1α Protein Level as a Diagnostic Marker of Obstructive Sleep Apnea. Pol. Arch. Intern. Med. 2020;130:158–160. doi: 10.20452/pamw.15104. [DOI] [PubMed] [Google Scholar]
- 19.Rius J., Guma M., Schachtrup C., Akassoglou K., Zinkernagel A.S., Nizet V., Johnson R.S., Haddad G.G., Karin M. NF-KappaB Links Innate Immunity to the Hypoxic Response through Transcriptional Regulation of HIF-1alpha. Nature. 2008;453:807–811. doi: 10.1038/nature06905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pratt-Ubunama M.N., Nishizaka M.K., Boedefeld R.L., Cofield S.S., Harding S.M., Calhoun D.A. Plasma Aldosterone Is Related to Severity of Obstructive Sleep Apnea in Subjects with Resistant Hypertension. Chest. 2007;131:453–459. doi: 10.1378/chest.06-1442. [DOI] [PubMed] [Google Scholar]
- 21.Sforza E., Roche F., Chapelle C., Pichot V. Internight Variability of Apnea-Hypopnea Index in Obstructive Sleep Apnea Using Ambulatory Polysomnography. Front. Physiol. 2019;10:849. doi: 10.3389/fphys.2019.00849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yu J., Zhou Z., McEvoy R.D., Anderson C.S., Rodgers A., Perkovic V., Neal B. Association of Positive Airway Pressure With Cardiovascular Events and Death in Adults With Sleep Apnea: A Systematic Review and Meta-Analysis. JAMA. 2017;318:156–166. doi: 10.1001/jama.2017.7967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Labarca G., Dreyse J., Drake L., Jorquera J., Barbe F. Efficacy of Continuous Positive Airway Pressure (CPAP) in the Prevention of Cardiovascular Events in Patients with Obstructive Sleep Apnea: Systematic Review and Meta-Analysis. Sleep Med. Rev. 2020;52:101312. doi: 10.1016/j.smrv.2020.101312. [DOI] [PubMed] [Google Scholar]
- 24.Khot S.P., Davis A.P., Crane D.A., Tanzi P.M., Li Lue D., Claflin E.S., Becker K.J., Longstreth W.T., Watson N.F., Billings M.E. Effect of Continuous Positive Airway Pressure on Stroke Rehabilitation: A Pilot Randomized Sham-Controlled Trial. J. Clin. Sleep Med. 2016;12:1019–1026. doi: 10.5664/jcsm.5940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramar K., Dort L.C., Katz S.G., Lettieri C.J., Harrod C.G., Thomas S.M., Chervin R.D. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015. J. Clin. Sleep Med. 2015;11:773–827. doi: 10.5664/jcsm.4858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carvalho B., Hsia J., Capasso R. Surgical Therapy of Obstructive Sleep Apnea: A Review. Neurotherapeutics. 2012;9:710–716. doi: 10.1007/s13311-012-0141-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sedlák V., Kudela O., Kopecký M., Svarc M., Smolík P., Havel V. Factors Influencing Efficacy of BiPAP Therapy in Severe Obstructive Sleep Apnea. Eur. Respir. J. 2013;42:P4040. [Google Scholar]
- 28.Kim L.J., Freire C., Fleury Curado T., Jun J.C., Polotsky V.Y. The Role of Animal Models in Developing Pharmacotherapy for Obstructive Sleep Apnea. J. Clin. Med. 2019;8:49. doi: 10.3390/jcm8122049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paterson G.G., Young J.M., Willson J.A., Graham C.J., Dru R.C., Lee E.W., Torpey G.S., Walmsley S.R., Chan M.V., Warner T.D., et al. Hypoxia Modulates Platelet Purinergic Signalling Pathways. Thromb. Haemost. 2020;120:253–261. doi: 10.1055/s-0039-3400305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maclay J.D., McAllister D.A., Johnston S., Raftis J., McGuinnes C., Deans A., Newby D.E., Mills N.L., MacNee W. Increased Platelet Activation in Patients with Stable and Acute Exacerbation of COPD. Thorax. 2011;66:769–774. doi: 10.1136/thx.2010.157529. [DOI] [PubMed] [Google Scholar]
- 31.Sabit R., Thomas P., Shale D.J., Collins P., Linnane S.J. The Effects of Hypoxia on Markers of Coagulation and Systemic Inflammation in Patients with COPD. Chest. 2010;138:47–51. doi: 10.1378/chest.09-2764. [DOI] [PubMed] [Google Scholar]
- 32.Jankowski M., Undas A., Kaczmarek P., Butenas S. Activated Factor XI and Tissue Factor in Chronic Obstructive Pulmonary Disease: Links with Inflammation and Thrombin Generation. Thromb. Res. 2011;127:242–246. doi: 10.1016/j.thromres.2010.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Popovic B., Zannad F., Louis H., Clerc-Urmès I., Lakomy C., Gibot S., Denis C.V., Lacolley P., Regnault V. Endothelial-Driven Increase in Plasma Thrombin Generation Characterising a New Hypercoagulable Phenotype in Acute Heart Failure. Int. J. Cardiol. 2019;274:195–201. doi: 10.1016/j.ijcard.2018.07.130. [DOI] [PubMed] [Google Scholar]
- 34.Fan Z., Lu X., Long H., Li T., Zhang Y. The Association of Hemocyte Profile and Obstructive Sleep Apnea. J. Clin. Lab. Anal. 2019;33:e22680. doi: 10.1002/jcla.22680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reinhart W.H., Oswald J., Walter R., Kuhn M. Blood Viscosity and Platelet Function in Patients with Obstructive Sleep Apnea Syndrome Treated with Nasal Continuous Positive Airway Pressure. Clin. Hemorheol. Microcirc. 2002;27:201–207. [PubMed] [Google Scholar]
- 36.Dikmenoğlu N., Çiftçi B., İleri E., Güven S.F., Seringeç N., Aksoy Y., Ercil D. Erythrocyte Deformability, Plasma Viscosity and Oxidative Status in Patients with Severe Obstructive Sleep Apnea Syndrome. Sleep Med. 2006;7:255–261. doi: 10.1016/j.sleep.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 37.Tazbirek M., Slowinska L., Skoczynski S., Pierzchala W. Short-Term Continuous Positive Airway Pressure Therapy Reverses the Pathological Influence of Obstructive Sleep Apnea on Blood Rheology Parameters. Clin. Hemorheol. Microcirc. 2009;41:241–249. doi: 10.3233/CH-2009-1175. [DOI] [PubMed] [Google Scholar]
- 38.Robinson G.V., Pepperell J.C.T., Segal H.C., Davies R.J.O., Stradling J.R. Circulating Cardiovascular Risk Factors in Obstructive Sleep Apnoea: Data from Randomised Controlled Trials. Thorax. 2004;59:777–782. doi: 10.1136/thx.2003.018739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.von Känel R., Loredo J.S., Powell F.L., Adler K.A., Dimsdale J.E. Short-Term Isocapnic Hypoxia and Coagulation Activation in Patients with Sleep Apnea. Clin. Hemorheol. Microcirc. 2005;33:369–377. [PubMed] [Google Scholar]
- 40.Olson N.C., Raffield L.M., Lange L.A., Lange E.M., Longstreth W.T., Chauhan G., Debette S., Seshadri S., Reiner A.P., Tracy R.P. Associations of Activated Coagulation Factor VII and Factor VIIa-Antithrombin Levels with Genome-Wide Polymorphisms and Cardiovascular Disease Risk. J. Thromb. Haemost. 2018;16:19–30. doi: 10.1111/jth.13899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nickel Katrin F., Long Andy T., Fuchs Tobias A., Butler Lynn M. Renné Thomas Factor XII as a Therapeutic Target in Thromboembolic and Inflammatory Diseases. Arterioscler. Thromb. Vasc. Biol. 2017;37:13–20. doi: 10.1161/ATVBAHA.116.308595. [DOI] [PubMed] [Google Scholar]
- 42.Johansson K., Jansson J.-H., Johansson L., Bylesjö I., Nilsson T.K., Eliasson M., Söderberg S., Lind M. Factor XII as a Risk Marker for Hemorrhagic Stroke: A Prospective Cohort Study. Cerebrovasc. Dis. Extra. 2017;7:84–94. doi: 10.1159/000468994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chin K., Kita H., Noguchi T., Otsuka N., Tsuboi T., Nakamura T., Shimizu K., Mishima M., Ohi M. Improvement of Factor VII Clotting Activity Following Long-Term NCPAP Treatment in Obstructive Sleep Apnoea Syndrome. QJM. 1998;91:627–633. doi: 10.1093/qjmed/91.9.627. [DOI] [PubMed] [Google Scholar]
- 44.Folsom A.R., Lutsey P.L., Astor B.C., Cushman M. C-Reactive Protein and Venous Thromboembolism. A Prospective Investigation in the ARIC Cohort. Thromb. Haemost. 2009;102:615–619. doi: 10.1160/TH09-04-0274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stec James J., Silbershatz H., Tofler Geoffrey H., Matheney Travis H., Sutherland P., Lipinska I., Massaro Joseph M., Wilson Peter F.W., Muller James E., D’Agostino Ralph B. Association of Fibrinogen With Cardiovascular Risk Factors and Cardiovascular Disease in the Framingham Offspring Population. Circulation. 2000;102:1634–1638. doi: 10.1161/01.CIR.102.14.1634. [DOI] [PubMed] [Google Scholar]
- 46.Zhang X., Yin K., Wang H., Su M., Yang Y. Effect of Continuous Positive Airway Pressure Treatment on Elderly Chinese Patients with Obstructive Sleep Apnea in the Prethrombotic State. Chin. Med. J. 2003;116:1426–1428. [PubMed] [Google Scholar]
- 47.Nobili L., Schiavi G., Bozano E., De Carli F., Ferrillo F., Nobili F. Morning Increase of Whole Blood Viscosity in Obstructive Sleep Apnea Syndrome. Clin. Hemorheol. Microcirc. 2000;22:21–27. [PubMed] [Google Scholar]
- 48.Comondore V.R., Cheema R., Fox J., Butt A., John Mancini G.B., Fleetham J.A., Ryan C.F., Chan S., Ayas N.T. The Impact of CPAP on Cardiovascular Biomarkers in Minimally Symptomatic Patients with Obstructive Sleep Apnea: A Pilot Feasibility Randomized Crossover Trial. Lung. 2009;187:17–22. doi: 10.1007/s00408-008-9115-5. [DOI] [PubMed] [Google Scholar]
- 49.von Känel R., Malan N.T., Hamer M., Lambert G.W., Schlaich M., Reimann M., Malan L. Three-Year Changes of Prothrombotic Factors in a Cohort of South Africans with a High Clinical Suspicion of Obstructive Sleep Apnea. Thromb. Haemost. 2016;115:63–72. doi: 10.1160/TH15-03-0206. [DOI] [PubMed] [Google Scholar]
- 50.Hizli O., Cayir S., Coluk Y., Kayabasi S., Yildirim G. The Novel Indicators of Moderate to Severe Sleep Apnea: Fibrinogen to Albumin Ratio vs. CRP to Albumin Ratio. Eur. Arch. Otorhinolaryngol. 2020 doi: 10.1007/s00405-019-05770-5. [DOI] [PubMed] [Google Scholar]
- 51.Mehra R., Xu F., Babineau D.C., Tracy R.P., Jenny N.S., Patel S.R., Redline S. Sleep-Disordered Breathing and Prothrombotic Biomarkers. Am. J. Respir. Crit. Care Med. 2010;182:826–833. doi: 10.1164/rccm.201001-0020OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Steiner S., Jax T., Evers S., Hennersdorf M., Schwalen A., Strauer B.E. Altered Blood Rheology in Obstructive Sleep Apnea as a Mediator of Cardiovascular Risk. Cardiology. 2005;104:92–96. doi: 10.1159/000086729. [DOI] [PubMed] [Google Scholar]
- 53.Wessendorf T.E., Thilmann A.F., Wang Y.M., Schreiber A., Konietzko N., Teschler H. Fibrinogen Levels and Obstructive Sleep Apnea in Ischemic Stroke. Am. J. Respir. Crit. Care Med. 2000;162:2039–2042. doi: 10.1164/ajrccm.162.6.2001048. [DOI] [PubMed] [Google Scholar]
- 54.Shamsuzzaman A., Amin R.S., Calvin A.D., Davison D., Somers V.K. Severity of Obstructive Sleep Apnea Is Associated with Elevated Plasma Fibrinogen in Otherwise Healthy Patients. Sleep Breath. 2014;18:761–766. doi: 10.1007/s11325-014-0938-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bouloukaki I., Mermigkis C., Tzanakis N., Kallergis E., Moniaki V., Mauroudi E., Schiza S.E. Evaluation of Inflammatory Markers in a Large Sample of Obstructive Sleep Apnea Patients without Comorbidities. Mediat. Inflamm. 2017;2017:4573756. doi: 10.1155/2017/4573756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Geiser T., Buck F., Meyer B.J., Bassetti C., Haeberli A., Gugger M. In Vivo Platelet Activation Is Increased during Sleep in Patients with Obstructive Sleep Apnea Syndrome. Respiration. 2002;69:229–234. doi: 10.1159/000063625. [DOI] [PubMed] [Google Scholar]
- 57.Bokinsky G., Miller M., Ault K., Husband P., Mitchell J. Spontaneous Platelet Activation and Aggregation during Obstructive Sleep Apnea and Its Response to Therapy with Nasal Continuous Positive Airway Pressure. A Preliminary Investigation. Chest. 1995;108:625–630. doi: 10.1378/chest.108.3.625. [DOI] [PubMed] [Google Scholar]
- 58.von Känel R., Dimsdale J.E. Hemostatic Alterations in Patients with Obstructive Sleep Apnea and the Implications for Cardiovascular Disease. Chest. 2003;124:1956–1967. doi: 10.1378/chest.124.5.1956. [DOI] [PubMed] [Google Scholar]
- 59.Akinnusi M.E., Paasch L.L., Szarpa K.R., Wallace P.K., El Solh A.A. Impact of Nasal Continuous Positive Airway Pressure Therapy on Markers of Platelet Activation in Patients with Obstructive Sleep Apnea. Respiration. 2009;77:25–31. doi: 10.1159/000158488. [DOI] [PubMed] [Google Scholar]
- 60.Kosacka M., Brzecka A., Piesiak P., Korzeniewska A., Jankowska R. Soluble Ligand CD40 and Uric Acid as Markers of Atheromatosis in Patients with Obstructive Sleep Apnea. Adv. Exp. Med. Biol. 2015;839:55–60. doi: 10.1007/5584_2014_44. [DOI] [PubMed] [Google Scholar]
- 61.Kobayashi K., Nishimura Y., Shimada T., Yoshimura S., Funada Y., Satouchi M., Yokoyama M. Effect of Continuous Positive Airway Pressure on Soluble CD40 Ligand in Patients with Obstructive Sleep Apnea Syndrome. Chest. 2006;129:632–637. doi: 10.1378/chest.129.3.632. [DOI] [PubMed] [Google Scholar]
- 62.Cofta S., Wysocka E., Dziegielewska-Gesiak S., Michalak S., Piorunek T., Batura-Gabryel H., Torlinski L. Plasma Selectins in Patients with Obstructive Sleep Apnea. Adv. Exp. Med. Biol. 2013;756:113–119. doi: 10.1007/978-94-007-4549-0_15. [DOI] [PubMed] [Google Scholar]
- 63.Shimizu M., Kamio K., Haida M., Ono Y., Miyachi H., Yamamoto M., Shinohara Y., Ando Y. Platelet Activation in Patients with Obstructive Sleep Apnea Syndrome and Effects of Nasal-Continuous Positive Airway Pressure. Tokai. J. Exp. Clin. Med. 2002;27:107–112. [PubMed] [Google Scholar]
- 64.Horváth P., Lázár Z., Gálffy G., Puskás R., Kunos L., Losonczy G., Mészáros M., Tárnoki Á.D., Tárnoki D.L., Bikov A. Circulating P-Selectin Glycoprotein Ligand 1 and P-Selectin Levels in Obstructive Sleep Apnea Patients. Lung. 2020;198:173–179. doi: 10.1007/s00408-019-00299-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Winiarska H.M., Cofta S., Bielawska L., Płóciniczak A., Piorunek T., Wysocka E. Circulating P-Selectin and Its Glycoprotein Ligand in Nondiabetic Obstructive Sleep Apnea Patients. Adv. Exp. Med. Biol. 2020 doi: 10.1007/5584_2020_501. [DOI] [PubMed] [Google Scholar]
- 66.Sanner B.M., Konermann M., Tepel M., Groetz J., Mummenhoff C., Zidek W. Platelet Function in Patients with Obstructive Sleep Apnoea Syndrome. Eur. Respir. J. 2000;16:648–652. doi: 10.1034/j.1399-3003.2000.16d14.x. [DOI] [PubMed] [Google Scholar]
- 67.Oga T., Chin K., Tabuchi A., Kawato M., Morimoto T., Takahashi K., Handa T., Takahashi K., Taniguchi R., Kondo H., et al. Effects of Obstructive Sleep Apnea with Intermittent Hypoxia on Platelet Aggregability. J. Atheroscler. Thromb. 2009;16:862–869. doi: 10.5551/jat.2188. [DOI] [PubMed] [Google Scholar]
- 68.Kontos A., Willoughby S., Lushington K., Martin J., Wabnitz D., Dorrian J., Kennedy D. Increased Platelet Aggregation in Children and Adolescents with Sleep-Disordered Breathing. Am. J. Respir. Crit. Care Med. 2020;202:1560–1566. doi: 10.1164/rccm.201911-2229OC. [DOI] [PubMed] [Google Scholar]
- 69.Alkhiary W., Morsy N.E., Yousef A.M., El-Saddik A.M., Arram E.O. Adenosine Diphosphate-Induced Platelets Aggregability in Polysomnographically Verified Obstructive Sleep Apnea. Clin. Appl. Thromb. Hemost. 2017;23:360–366. doi: 10.1177/1076029615600790. [DOI] [PubMed] [Google Scholar]
- 70.Deng Y., Fang W., Li Y., Cen J., Fang F., Lv P., Gong S., Mao L. Blood-Brain Barrier Breakdown by PAF and Protection by XQ-1H Due to Antagonism of PAF Effects. Eur. J. Pharmacol. 2009;616:43–47. doi: 10.1016/j.ejphar.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 71.Row B.W., Kheirandish L., Li R.C., Guo S.Z., Brittian K.R., Hardy M., Bazan N.G., Gozal D. Platelet-Activating Factor Receptor-Deficient Mice Are Protected from Experimental Sleep Apnea-Induced Learning Deficits. J. Neurochem. 2004;89:189–196. doi: 10.1111/j.1471-4159.2004.02352.x. [DOI] [PubMed] [Google Scholar]
- 72.Liak C., Fitzpatrick M. Coagulability in Obstructive Sleep Apnea. Can. Respir. J. 2011;18:338–348. doi: 10.1155/2011/924629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Reininger A.J. Function of von Willebrand Factor in Haemostasis and Thrombosis. Haemophilia. 2008;14:11–26. doi: 10.1111/j.1365-2516.2008.01848.x. [DOI] [PubMed] [Google Scholar]
- 74.von Känel R., Loredo J.S., Ancoli-Israel S., Dimsdale J.E. Association between Sleep Apnea Severity and Blood Coagulability: Treatment Effects of Nasal Continuous Positive Airway Pressure. Sleep Breath. 2006;10:139–146. doi: 10.1007/s11325-006-0060-3. [DOI] [PubMed] [Google Scholar]
- 75.von Känel R., Loredo J.S., Ancoli-Israel S., Mills P.J., Natarajan L., Dimsdale J.E. Association between Polysomnographic Measures of Disrupted Sleep and Prothrombotic Factors. Chest. 2007;131:733–739. doi: 10.1378/chest.06-2006. [DOI] [PubMed] [Google Scholar]
- 76.El Solh A.A., Akinnusi M.E., Berim I.G., Peter A.M., Paasch L.L., Szarpa K.R. Hemostatic Implications of Endothelial Cell Apoptosis in Obstructive Sleep Apnea. Sleep Breath. 2008;12:331–337. doi: 10.1007/s11325-008-0182-x. [DOI] [PubMed] [Google Scholar]
- 77.Phillips C.L., McEwen B.J., Morel-Kopp M.-C., Yee B.J., Sullivan D.R., Ward C.M., Tofler G.H., Grunstein R.R. Effects of Continuous Positive Airway Pressure on Coagulability in Obstructive Sleep Apnoea: A Randomised, Placebo-Controlled Crossover Study. Thorax. 2012;67:639–644. doi: 10.1136/thoraxjnl-2011-200874. [DOI] [PubMed] [Google Scholar]
- 78.Lim D.C., Pack A.I. Obstructive Sleep Apnea and Cognitive Impairment: Addressing the Blood–Brain Barrier. Sleep Med. Rev. 2014;18:35–48. doi: 10.1016/j.smrv.2012.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Khalyfa A., Gozal D., Kheirandish-Gozal L. Plasma Exosomes Disrupt the Blood–Brain Barrier in Children with Obstructive Sleep Apnea and Neurocognitive Deficits. Am. J. Respir. Crit. Care Med. 2018;197:1073–1076. doi: 10.1164/rccm.201708-1636LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Voirin A.-C., Celle S., Perek N., Roche F. Sera of Elderly Obstructive Sleep Apnea Patients Alter Blood–Brain Barrier Integrity in Vitro: A Pilot Study. Sci. Rep. 2020;10:11309. doi: 10.1038/s41598-020-68374-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Daneman R., Prat A. The Blood–Brain Barrier. Cold Spring Harb. Perspect. Biol. 2015;7 doi: 10.1101/cshperspect.a020412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mahringer A., Fricker G. ABC Transporters at the Blood–Brain Barrier. Expert Opin. Drug Metab. Toxicol. 2016;12:499–508. doi: 10.1517/17425255.2016.1168804. [DOI] [PubMed] [Google Scholar]
- 83.Daneman R. The Blood-Brain Barrier in Health and Disease. Ann. Neurol. 2012;72:648–672. doi: 10.1002/ana.23648. [DOI] [PubMed] [Google Scholar]
- 84.Zhou L., Chen P., Peng Y., Ouyang R. Role of Oxidative Stress in the Neurocognitive Dysfunction of Obstructive Sleep Apnea Syndrome. Oxid. Med. Cell. Longev. 2016;2016:9626831. doi: 10.1155/2016/9626831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gozal D., Gileles-Hillel A., Cortese R., Li Y., Almendros I., Qiao Z., Khalyfa A.A., Andrade J., Khalyfa A. Visceral White Adipose Tissue after Chronic Intermittent and Sustained Hypoxia in Mice. Am. J. Respir. Cell Mol. Biol. 2017;56:477–487. doi: 10.1165/rcmb.2016-0243OC. [DOI] [PubMed] [Google Scholar]
- 86.Israel L.P., Benharoch D., Gopas J., Goldbart A.D. A Pro-Inflammatory Role for Nuclear Factor Kappa B in Childhood Obstructive Sleep Apnea Syndrome. Sleep. 2013;36:1947–1955. doi: 10.5665/sleep.3236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nadeem R., Molnar J., Madbouly E.M., Nida M., Aggarwal S., Sajid H., Naseem J., Loomba R. Serum Inflammatory Markers in Obstructive Sleep Apnea: A Meta-Analysis. J. Clin. Sleep Med. 2013;9:1003–1012. doi: 10.5664/jcsm.3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kheirandish-Gozal L., Gozal D. Obstructive Sleep Apnea and Inflammation: Proof of Concept Based on Two Illustrative Cytokines. Int. J. Mol. Sci. 2019;20:459. doi: 10.3390/ijms20030459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kim L.J., Martinez D., Fiori C.Z., Baronio D., Kretzmann N.A., Barros H.M.T. Hypomyelination, Memory Impairment, and Blood-Brain Barrier Permeability in a Model of Sleep Apnea. Brain Res. 2015;1597:28–36. doi: 10.1016/j.brainres.2014.11.052. [DOI] [PubMed] [Google Scholar]
- 90.Kilicarslan R., Alkan A., Sharifov R., Akkoyunlu M.E., Aralasmak A., Kocer A., Kart L. The Effect of Obesity on Brain Diffusion Alteration in Patients with Obstructive Sleep Apnea. Sci. World J. 2014;2014:768415. doi: 10.1155/2014/768415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.György B., Szabó T.G., Pásztói M., Pál Z., Misják P., Aradi B., László V., Pállinger É., Pap E., Kittel Á., et al. Membrane Vesicles, Current State-of-the-Art: Emerging Role of Extracellular Vesicles. Cell Mol. Life Sci. 2011;68:2667–2688. doi: 10.1007/s00018-011-0689-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wood M.J.A., O’Loughlin A.J., Samira L. Exosomes and the Blood-Brain Barrier: Implications for Neurological Diseases. Ther. Deliv. 2011;2:1095–1099. doi: 10.4155/tde.11.83. [DOI] [PubMed] [Google Scholar]
- 93.Khalyfa A., Gozal D., Kheirandish-Gozal L. Plasma Extracellular Vesicles in Children with OSA Disrupt Blood-Brain Barrier Integrity and Endothelial Cell Wound Healing in Vitro. Int. J. Mol. Sci. 2019;20:6233. doi: 10.3390/ijms20246233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Liu D.-Z., Ander B.P., Xu H., Shen Y., Kaur P., Deng W., Sharp F.R. Blood-Brain Barrier Breakdown and Repair by Src after Thrombin-Induced Injury. Ann. Neurol. 2010;67:526–533. doi: 10.1002/ana.21924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kawakita K., Kawai N., Kuroda Y., Yasashita S., Nagao S. Expression of Matrix Metalloproteinse-9 in Thrombin-Induced Brain Edema Formation in Rats. J. Stroke Cerebrovasc. Dis. 2006;15:88–95. doi: 10.1016/j.jstrokecerebrovasdis.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 96.Suidan G.L., Brill A., De Meyer S.F., Voorhees J.R., Cifuni S.M., Cabral J.E., Wagner D.D. Endothelial Von Willebrand Factor Promotes Blood-Brain Barrier Flexibility and Provides Protection from Hypoxia and Seizures in Mice. Arterioscler. Thromb. Vasc. Biol. 2013;33:2112–2120. doi: 10.1161/ATVBAHA.113.301362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kisucka J., Chauhan A.K., Zhao B.-Q., Patten I.S., Yesilaltay A., Krieger M., Wagner D.D. Elevated Levels of Soluble P-Selectin in Mice Alter Blood-Brain Barrier Function, Exacerbate Stroke, and Promote Atherosclerosis. Blood. 2009;113:6015–6022. doi: 10.1182/blood-2008-10-186650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Paul J., Strickland S., Melchor J.P. Fibrin Deposition Accelerates Neurovascular Damage and Neuroinflammation in Mouse Models of Alzheimer’s Disease. J. Exp. Med. 2007;204:1999–2008. doi: 10.1084/jem.20070304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jin A.Y., Tuor U.I., Rushforth D., Kaur J., Muller R.N., Petterson J.L., Boutry S., Barber P.A. Reduced Blood Brain Barrier Breakdown in P-Selectin Deficient Mice Following Transient Ischemic Stroke: A Future Therapeutic Target for Treatment of Stroke. BMC Neurosci. 2010;11:12. doi: 10.1186/1471-2202-11-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Masuda H., Mori M., Umehara K., Furihata T., Uchida T., Uzawa A., Kuwabara S. Soluble CD40 Ligand Disrupts the Blood–Brain Barrier and Exacerbates Inflammation in Experimental Autoimmune Encephalomyelitis. J. Neuroimmunol. 2018;316:117–120. doi: 10.1016/j.jneuroim.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 101.Davidson D.C., Hirschman M.P., Sun A., Singh M.V., Kasischke K., Maggirwar S.B. Excess Soluble CD40L Contributes to Blood Brain Barrier Permeability in Vivo: Implications for HIV-Associated Neurocognitive Disorders. PLoS ONE. 2012;7:e51793. doi: 10.1371/journal.pone.0051793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Brailoiu E., Barlow C.L., Ramirez S.H., Abood M.E., Brailoiu G.C. Effects of Platelet-Activating Factor on Brain Microvascular Endothelial Cells. Neuroscience. 2018;377:105–113. doi: 10.1016/j.neuroscience.2018.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Fang W., Zhang R., Sha L., Lv P., Shang E., Han D., Wei J., Geng X., Yang Q., Li Y. Platelet Activating Factor Induces Transient Blood-Brain Barrier Opening to Facilitate Edaravone Penetration into the Brain. J. Neurochem. 2014;128:662–671. doi: 10.1111/jnc.12507. [DOI] [PubMed] [Google Scholar]
- 104.Abdel Salam O.A., Ghonimi N.A.M., Ismail M.H. Risk of Obstructive Sleep Apnea in Multiple Sclerosis: Frequency, Clinical and Radiological Correlates. Mult. Scler. Relat. Disord. 2019;28:184–188. doi: 10.1016/j.msard.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 105.Andrade A., Bubu O.M., Varga A.W., Osorio R.S. The Relationship between Obstructive Sleep Apnea and Alzheimer’s Disease. J. Alzheimers Dis. 2018;64:S255–S270. doi: 10.3233/JAD-179936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ryu J.K., McLarnon J.G. A Leaky Blood–Brain Barrier, Fibrinogen Infiltration and Microglial Reactivity in Inflamed Alzheimer’s Disease Brain. J. Cell. Mol. Med. 2009;13:2911–2925. doi: 10.1111/j.1582-4934.2008.00434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ryu J.K., Petersen M.A., Murray S.G., Baeten K.M., Meyer-Franke A., Chan J.P., Vagena E., Bedard C., Machado M.R., Rios Coronado P.E., et al. Blood Coagulation Protein Fibrinogen Promotes Autoimmunity and Demyelination via Chemokine Release and Antigen Presentation. Nat. Commun. 2015;6:8164. doi: 10.1038/ncomms9164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ziliotto N., Bernardi F., Jakimovski D., Zivadinov R. Coagulation Pathways in Neurological Diseases: Multiple Sclerosis. Front. Neurol. 2019;10:409. doi: 10.3389/fneur.2019.00409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Merlini M., Akassoglou K. Alzheimer Disease Makes New Blood Contacts. Blood. 2017;129:2462–2463. doi: 10.1182/blood-2017-03-772087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chen Z.-L., Revenko A.S., Singh P., MacLeod A.R., Norris E.H., Strickland S. Depletion of Coagulation Factor XII Ameliorates Brain Pathology and Cognitive Impairment in Alzheimer Disease Mice. Blood. 2017;129:2547–2556. doi: 10.1182/blood-2016-11-753202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gong W., Wang X., Fan J., Nie S., Wei Y. Impact of Obstructive Sleep Apnea on Platelet Function Profiles in Patients With Acute Coronary Syndrome Taking Dual Antiplatelet Therapy. J. Am. Heart Assoc. 2018;7:e008808. doi: 10.1161/JAHA.118.008808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Latina J.M., Estes N.A.M., Garlitski A.C. The Relationship between Obstructive Sleep Apnea and Atrial Fibrillation: A Complex Interplay. Pulm. Med. 2013;2013:621736. doi: 10.1155/2013/621736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Marti-Almor J., Marques P., Jesel L., Garcia R., Girolamo E.D., Locati F., Defaye P., Venables P., Dompnier A., Barcelo A., et al. Incidence of Sleep Apnea and Association with Atrial Fibrillation in an Unselected Pacemaker Population: Results of the Observational RESPIRE Study. Heart Rhythm. 2020;17:195–202. doi: 10.1016/j.hrthm.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 114.Jehan S., Farag M., Zizi F., Pandi-Perumal S.R., Chung A., Truong A., Jean-Louis G., Tello D., McFarlane S.I. Obstructive Sleep Apnea and Stroke. Sleep Med. Disord. 2018;2:120–125. [PMC free article] [PubMed] [Google Scholar]
- 115.García-Ortega A., Mañas E., López-Reyes R., Selma M.J., García-Sánchez A., Oscullo G., Jiménez D., Martínez-García M.Á. Obstructive Sleep Apnoea and Venous Thromboembolism: Pathophysiological Links and Clinical Implications. Eur. Respir. J. 2019;53:1800893. doi: 10.1183/13993003.00893-2018. [DOI] [PubMed] [Google Scholar]
- 116.Alonso-Fernández A., Suquia A.G., Peña M.D.L., Casitas R., Pierola J., Barceló A., Soriano J.B., Fernández-Capitán C., Martinez-Ceron E., Carrera M., et al. OSA is a Risk Factor for Recurrent VTE. Chest. 2016;150:1291–1301. doi: 10.1016/j.chest.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 117.Jiang X.-M., Qian X.-S., Gao X.-F., Ge Z., Tian N.-L., Kan J., Zhang J.-J. Obstructive Sleep Apnea Affecting Platelet Reactivity in Patients Undergoing Percutaneous Coronary Intervention. Chin. Med. J. Engl. 2018;131:1023–1029. doi: 10.4103/0366-6999.230732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Xie J., Wei Y.-X., Liu S., Zhang W., Zhang X.-F., Li J. Obstructive Sleep Apnea Hypopnea Syndrome as a Reason for Active Management of Pulmonary Embolism. Chin. Med. J. Engl. 2015;128:2147–2153. doi: 10.4103/0366-6999.162498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hawkins B.T., Gu Y.-H., Izawa Y., del Zoppo G.J. Dabigatran Abrogates Brain Endothelial Cell Permeability in Response to Thrombin. J. Cereb. Blood Flow Metab. 2015;35:985–992. doi: 10.1038/jcbfm.2015.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ploen R., Sun L., Zhou W., Heitmeier S., Zorn M., Jenetzky E., Veltkamp R. Rivaroxaban Does Not Increase Hemorrhage after Thrombolysis in Experimental Ischemic Stroke. J. Cereb. Blood Flow Metab. 2014;34:495–501. doi: 10.1038/jcbfm.2013.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sun L., Zhou W., Ploen R., Zorn M., Veltkamp R. Anticoagulation with Dabigatran Does Not Increase Secondary Intracerebral Haemorrhage after Thrombolysis in Experimental Cerebral Ischaemia. Thromb. Haemost. 2013;110:153–161. doi: 10.1160/TH12-12-0942. [DOI] [PubMed] [Google Scholar]
- 122.Pétrault M., Ouk T., Pétrault O., Bastide M., Bordet R., Bérézowski V. Safety of Oral Anticoagulants on Experimental Brain Microbleeding and Cognition. Neuropharmacology. 2019;155:162–172. doi: 10.1016/j.neuropharm.2019.05.030. [DOI] [PubMed] [Google Scholar]
- 123.Puech C., Delavenne X., He Z., Forest V., Mismetti P., Perek N. Direct Oral Anticoagulants are Associated with Limited Damage of Endothelial Cells of the Blood-Brain Barrier Mediated by the Thrombin/PAR-1 Pathway. Brain Res. 2019;1719:57–63. doi: 10.1016/j.brainres.2019.05.024. [DOI] [PubMed] [Google Scholar]
- 124.Sweeney M.D., Sagare A.P., Zlokovic B.V. Blood-Brain Barrier Breakdown in Alzheimer Disease and Other Neurodegenerative Disorders. Nat. Rev. Neurol. 2018;14:133–150. doi: 10.1038/nrneurol.2017.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Cortes-Canteli M., Kruyer A., Fernandez-Nueda I., Marcos-Diaz A., Ceron C., Richards A.T., Jno-Charles O.C., Rodriguez I., Callejas S., Norris E.H., et al. Long-Term Dabigatran Treatment Delays Alzheimer’s Disease Pathogenesis in the TgCRND8 Mouse Model. J. Am. Coll. Cardiol. 2019;74:1910–1923. doi: 10.1016/j.jacc.2019.07.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mukherjee S., Saxena R., Palmer L.J. The Genetics of Obstructive Sleep Apnoea. Respirology. 2018;23:18–27. doi: 10.1111/resp.13212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Roche F., Mouhli L., Pichot V., Celle S. OSAHS Phenotypes after Night Sleep Recordings: How to Get to Precision Medicine in 2021. Sleep. 2021:zsab154. doi: 10.1093/sleep/zsab154. [DOI] [PubMed] [Google Scholar]