Abstract
Coronary artery dissection is a rare complication of blunt chest wall trauma. We report a case of acute left anterior descending and right coronary artery dissections after a motor vehicle accident. The musculoskeletal injuries obscured the cardiac symptoms. Electrocardiogram and bedside echocardiogram revealed cardiac pathology, which prompted urgent coronary angiography and intervention. (Level of Difficulty: Advanced.)
Key Words: acute coronary syndrome, coronary angiography, dissection
Abbreviations and Acronyms: CT, computed tomography; ECG, electrocardiogram; LAD, left anterior descending coronary artery; RCA, right coronary artery; TIMI, Thrombolysis In Myocardial Infarction
History of Presentation
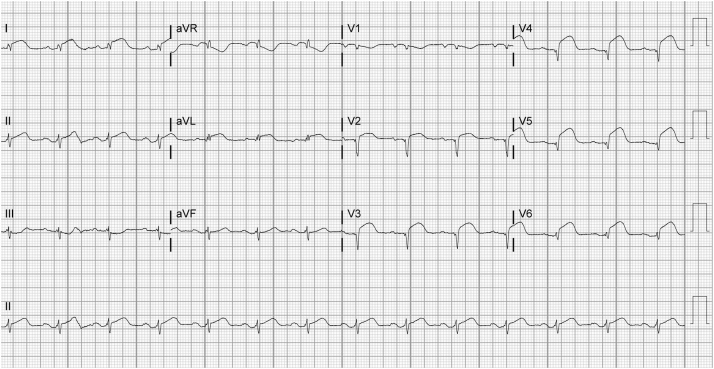
A 63-year-old man presented to our level I trauma center after a motor vehicle collision. On the scene, he was found conscious, in the driver’s seat, and had his right knee forcibly flexed to his chest. He was transported to the emergency department after a prolonged 45-min extrication. On arrival, the patient was hemodynamically stable. He was not in visible distress, but he did endorse diffuse pain throughout his chest wall and all extremities. Physical examination was significant for limb deformities and reproducible chest wall tenderness. An electrocardiogram (ECG) performed in the emergency department (Figure 1) showed sinus rhythm and ST-segment elevations in the lateral and anterior leads.
Learning Objectives
-
•
To recognize that blunt chest wall trauma may cause coronary artery dissections and cardiac ischemia.
-
•
To evaluate patients with blunt chest wall trauma for cardiac ischemia by performing a screening ECG and point-of-care echocardiography.
-
•
To coordinate with the trauma surgery team to prioritize coronary angiography and interventions if cardiac ischemia is suspected.
Figure 1.
Admission Electrocardiogram
Admission electrocardiogram demonstrating sinus rhythm and ST-segment elevations in the lateral and anterior leads.
Medical History
The patient’s medical history was significant for hypertension and hyperlipidemia.
Investigations
The patient’s initial troponin level was 0.94 ng/dl (normal <0.04 ng/dl). Thoracic imaging with chest radiograph and computed tomography (CT) scan of the thorax with contrast revealed numerous bilateral rib fractures, no sternal fracture, and no evidence of aortic dissection or transection. A bedside echocardiogram showed apical wall hypokinesis with moderately reduced left ventricular ejection fraction and a small pericardial effusion.
Differential Diagnosis
The initial differential diagnosis included ST-segment elevation myocardial infarction, cardiac contusion, and stress-induced cardiomyopathy.
Management
Emergent angiography was initially deferred in the context of polytrauma and suspected cardiac contusion. However, evidence of evolving infarction on a subsequent ECG prompted us to proceed with urgent coronary angiography after a bedside closed reduction of his dislocated right hip by orthopedic surgery to avoid femoral head necrosis.
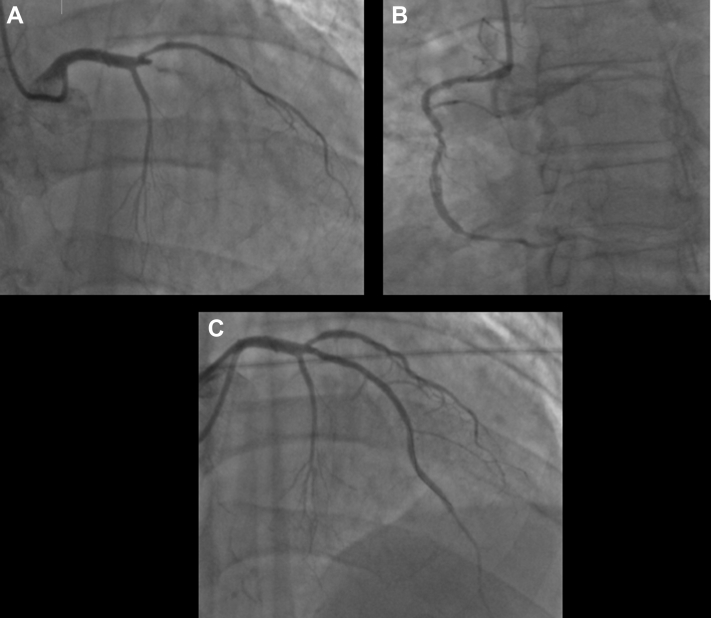
Coronary angiography (Figure 2, Video 1) showed the following: 1) an acute dissection of the proximal left anterior descending (LAD) artery with Thrombolysis In Myocardial Infarction (TIMI) flow grade 0; 2) dissection of the right coronary artery (RCA) with TIMI flow grade 3; and 3) a patent anomalous left circumflex coronary artery arising from the right coronary cusp. Successful percutaneous coronary intervention of the LAD with balloon dilation and 2 overlapping everolimus-eluting stents was performed with restoration of TIMI flow grade 3. The RCA was medically managed.
Figure 2.
Coronary Angiography
(A) Proximal left anterior descending coronary artery dissection with Thrombolysis In Myocardial Infarction flow grade 0. (B) Mid–right coronary artery dissection with Thrombolysis In Myocardial Infarction flow grade 3. (C) Post–percutaneous coronary intervention restoration of left anterior descending coronary artery flow.
Follow-Up
Repeat echocardiogram (Video 2) showed a left ventricular ejection fraction of 30% and an apical left ventricular thrombus. The patient was discharged on aspirin, ticagrelor, and warfarin. He was doing well at his follow-up appointment.
Discussion: Association With Current Guidelines/Position Papers/Current Practice
Cardiac complications of blunt chest wall trauma are increasingly seen in trauma centers as emergency medical services become more efficient in stabilizing and transporting patients. Potential cardiac complications include cardiac contusions, arrhythmias, pericardial tamponade, ventricular wall lacerations from sternal fractures, valvular lesions, and torsion or dissection of the great vessels (1). Traumatic coronary artery dissection is a less common complication described in only a few case reports. This literature suggests that the LAD is more commonly affected than the RCA and circumflex coronary arteries due to its anterior position (76% vs. 12% and 6%, respectively) (2,3). Per our review, this is 1 of 3 cases described in which simultaneous traumatic dissection occurred in multiple coronary arteries. Traumatic coronary dissections pose a diagnostic and therapeutic challenge given vague symptoms, concurrent injuries needing emergent noncardiac surgery, and the risk of worsening trauma-related bleeding with anticoagulation.
Blunt trauma causes coronary dissection by inducing rapid deceleration and shearing forces, which rupture the endothelium. The dissection is aggravated by tachycardia and hypertension stimulated by stress and pain from trauma. As in other forms of coronary artery disease, rupture of the endothelial wall induces platelet aggregation that can form a thrombus and cause acute myocardial infarction. Blunt chest trauma may also cause infarction by rupturing existing atherosclerotic coronary plaques (3). Further investigation is needed to understand whether pre-existing atherosclerosis increases the risk of a traumatic myocardial infarction.
Multiple factors may obscure the diagnosis of traumatic acute coronary dissection, and recognition requires a high index of suspicion. Review of prior data suggests that neither the mechanism nor severity of injury is predictive, as coronary dissections have been reported from severe motor vehicle accidents as well as minor sports injuries (4). Common signs and symptoms of cardiac ischemia such as chest pain, diaphoresis, and tachycardia may be attributed to significant musculoskeletal trauma, and cardiac etiologies may be overlooked. Cardiac enzyme levels have limited diagnostic utility in this scenario. Troponin enzyme levels rise to detectable amounts in the serum 4 to 6 h after myocardial injury (5), well after most patients with blunt chest trauma are initially triaged. Furthermore, cardiac enzyme levels may rise due to nonischemic causes of myocardial damage as well as skeletal muscle injury.
All patients who present with blunt chest wall trauma should be assessed for hemodynamic stability and have a screening ECG to assess for arrhythmias and ischemic changes. Any patient with persistent chest pain or ECG changes should be admitted for close cardiac monitoring with serial measurement of troponin levels. Although echocardiogram is readily available and frequently used, its role as a risk stratification tool in blunt cardiac trauma has been questioned by some investigators (6).
Patients with persistent signs of coronary ischemia even in the setting of significant trauma should be evaluated by using coronary angiography. However, interventions should be performed in close collaboration with the cardiothoracic surgery team.
CT scan of the thorax is commonly obtained for triaging patients with blunt chest wall trauma. In one case report, a traumatic coronary dissection was seen on initial CT imaging when retrospectively reviewed (7). Furthermore, there is growing evidence that CT angiography is an effective method of visualizing coronary arteries and spontaneous coronary artery dissections (8, 9, 10). In patients with suspected traumatic coronary artery dissection, CT imaging should be closely reviewed to assess for coronary abnormalities. It may evolve as an effective method to quickly assess for traumatic coronary artery dissection if initial clinical suspicion is high. However, further studies are needed to assess the efficacy of CT angiograms in this clinical scenario, particularly because ECG gating is not typically performed in the setting of trauma.
Conclusions
This case highlights the challenges of diagnosing acute coronary dissection in patients with blunt chest wall trauma and underscores the importance of having a low threshold for further cardiac evaluation if findings suggestive of coronary ischemia are present.
Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
(A) Left coronary angiography demonstrating proximal left anterior descending coronary artery dissection with Thrombolysis In Myocardial Infarction (TIMI) flow grade 0. (B) Right coronary angiography demonstrating mid–right coronary artery dissection with TIMI flow grade 3 and an anomalous left circumflex arising from the right coronary cusp. (C) Left coronary angiography post–percutaneous coronary intervention demonstrating restoration of TIMI flow grade 3 to the left anterior descending coronary artery.
(A) Left coronary angiography demonstrating proximal left anterior descending coronary artery dissection with Thrombolysis In Myocardial Infarction (TIMI) flow grade 0. (B) Right coronary angiography demonstrating mid–right coronary artery dissection with TIMI flow grade 3 and an anomalous left circumflex arising from the right coronary cusp. (C) Left coronary angiography post–percutaneous coronary intervention demonstrating restoration of TIMI flow grade 3 to the left anterior descending coronary artery.
(A) Left coronary angiography demonstrating proximal left anterior descending coronary artery dissection with Thrombolysis In Myocardial Infarction (TIMI) flow grade 0. (B) Right coronary angiography demonstrating mid–right coronary artery dissection with TIMI flow grade 3 and an anomalous left circumflex arising from the right coronary cusp. (C) Left coronary angiography post–percutaneous coronary intervention demonstrating restoration of TIMI flow grade 3 to the left anterior descending coronary artery.
(A) Apical view and (B) parasternal long view demonstrating left ventricular apical wall akinesis and a small pericardial effusion.
(A) Apical view and (B) parasternal long view demonstrating left ventricular apical wall akinesis and a small pericardial effusion.
References
- 1.Prêtre R., Chilcott M. Blunt trauma to the heart and great vessels. N Engl J Med. 1997;336:626–632. doi: 10.1056/NEJM199702273360906. [DOI] [PubMed] [Google Scholar]
- 2.Abdolrahimi S.A., Sanati H.R., Ansari-Ramandi M.M., Heris S.O., Maadani M. Acute myocardial infarction following blunt chest trauma and coronary artery dissection. J Clin Diagn Res. 2016;10:OD14–OD15. doi: 10.7860/JCDR/2016/19043.7994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lobay K.W., MacGougan C.K. Traumatic coronary artery dissection: a case report and literature review. J Emerg Med. 2012;43:e239–e243. doi: 10.1016/j.jemermed.2010.04.019. [DOI] [PubMed] [Google Scholar]
- 4.Atalar E., Açil T., Aytemir K. Acute anterior myocardial infarction following a mild nonpenetrating chest trauma: a case report. Angiology. 2001;52:279–282. doi: 10.1177/000331970105200408. [DOI] [PubMed] [Google Scholar]
- 5.Babuin L., Jaffe A.S. Troponin: the biomarker of choice for the detection of cardiac injury. CMAJ. 2005;173:1191–1202. doi: 10.1503/cmaj.050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nagy K.K., Krosner S.M., Roberts R.R., Joseph K.T., Smith R.F., Barrett J. Determining which patients require evaluation for blunt cardiac injury following blunt chest trauma. World J Surg. 2001;25:108–111. doi: 10.1007/s002680020372. [DOI] [PubMed] [Google Scholar]
- 7.Allemeersch G.J., Muylaert C., Nieboer K. Traumatic coronary artery dissection with secondary acute myocardial infarction after blunt thoracic trauma. J Belg Soc Radiol. 2018;102:4. doi: 10.5334/jbr-btr.1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vural M., Aksit Z., Kovanlikaya I., Degertekin M., Demirtas E. Can multidetector CT angiography detect coronary artery dissection? Tex Heart Inst J. 2007;34:388–389. [PMC free article] [PubMed] [Google Scholar]
- 9.Torres-Ayala S.C., Maldonado J., Bolton J.S., Bhalla S. Coronary computed tomography angiography of spontaneous coronary artery dissection: a case report and review of the literature. Am J Case Rep. 2015;16:130–135. doi: 10.12659/AJCR.892805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roura G., Ariza-Solé A., Rodriguez-Caballero I.F. Noninvasive follow-up of patients with spontaneous coronary artery dissection with CT angiography. J Am Coll Cardiol Img. 2016;9:896–897. doi: 10.1016/j.jcmg.2015.06.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) Left coronary angiography demonstrating proximal left anterior descending coronary artery dissection with Thrombolysis In Myocardial Infarction (TIMI) flow grade 0. (B) Right coronary angiography demonstrating mid–right coronary artery dissection with TIMI flow grade 3 and an anomalous left circumflex arising from the right coronary cusp. (C) Left coronary angiography post–percutaneous coronary intervention demonstrating restoration of TIMI flow grade 3 to the left anterior descending coronary artery.
(A) Left coronary angiography demonstrating proximal left anterior descending coronary artery dissection with Thrombolysis In Myocardial Infarction (TIMI) flow grade 0. (B) Right coronary angiography demonstrating mid–right coronary artery dissection with TIMI flow grade 3 and an anomalous left circumflex arising from the right coronary cusp. (C) Left coronary angiography post–percutaneous coronary intervention demonstrating restoration of TIMI flow grade 3 to the left anterior descending coronary artery.
(A) Left coronary angiography demonstrating proximal left anterior descending coronary artery dissection with Thrombolysis In Myocardial Infarction (TIMI) flow grade 0. (B) Right coronary angiography demonstrating mid–right coronary artery dissection with TIMI flow grade 3 and an anomalous left circumflex arising from the right coronary cusp. (C) Left coronary angiography post–percutaneous coronary intervention demonstrating restoration of TIMI flow grade 3 to the left anterior descending coronary artery.
(A) Apical view and (B) parasternal long view demonstrating left ventricular apical wall akinesis and a small pericardial effusion.
(A) Apical view and (B) parasternal long view demonstrating left ventricular apical wall akinesis and a small pericardial effusion.