Abstract
A 28-year-old woman with resistant hypertension was given a diagnosis of fibromuscular dysplasia with 100% occlusion of a right renal artery branch supplying an atrophied lower pole, collateralized by the right adrenal artery. Successful adrenal collateral coil embolization restored normotension, but hypertension recurred, necessitating right partial heminephrectomy with blood pressure normalization off medications. (Level of Difficulty: Intermediate.)
Key Words: arterial embolization, fibromuscular dysplasia, partial nephrectomy, resistant hypertension
Abbreviations and Acronyms: BP, blood pressure; CTA, computed tomography arteriography; FMD, fibromuscular dysplasia
Graphical abstract
History of Presentation
A 28-year-old woman with a history of Hashimoto thyroiditis presented to our Comprehensive Hypertension Center (at the University of Chicago, Chicago, Illinois) with new-onset, rapidly rising blood pressure (BP) resistant to multiple medications, including losartan 100 mg, carvedilol 25 mg twice a day, hydrochlorothiazide 25 mg daily, and amlodipine 5 mg daily. Her BP ranged from 140 to 160 mm Hg over 90 to 100 mm Hg despite changes to previous medications. Before this, rising blood pressures had been noted during primary care visits, although no medications were prescribed. She was symptomatic, with periodic headaches and fatigue. Physical examination was unremarkable: no cardiomegaly, murmurs, or abdominal bruits.
Learning Objectives
-
•
To make a differential diagnosis of renal artery stenosis and FMD.
-
•
To understand the role of the renin-angiotensin system in FMD.
-
•
To illustrate the role of partial or complete nephrectomy for the management of resistant hypertension in patients with renal FMD who had undergone failed revascularization procedures or were not candidates for revascularization procedures.
Past Medical History
She had a history of Hashimoto thyroiditis, now with subclinical hypothyroidism, and a history of positive antinuclear antibody.
Differential Diagnosis
The differential diagnoses for resistant hypertension in young adults include primary hyperaldosteronism, pheochromocytoma, renovascular disease, and congenital aortic diseases such as aortic coarctation.
Investigations
Initial work-up noted hypokalemia (2.9 mEq/l; 3.5 to 5 mEq/l), elevated seated aldosterone (93 ng/dl; 0 to 30 ng/dl), and renin (19 ng/dl; 0.6 to 4.3 ng/dl); the ratio of aldosterone to renin was 4.9. Therefore, although this testing eliminated the diagnosis of primary hyperaldosteronism, it raised concerns for possible secondary hyperaldosteronism. Renal ultrasound Doppler imaging revealed questionable stenosis in the main right renal artery with an abnormal elevation of the peak renal arterial systolic velocity above threshold 180 cm/s (235.2 cm/s) and a discrepancy in size between the right kidney (3.12 cm × 4.88 cm × 8.69 cm) and the left kidney (5.03 cm × 5.37 cm × 11.89 cm). Of note, kidneys are generally similar in size, with normal differences being <1 cm in length. On renal computed tomography angiography (CTA), a right main renal artery stenosis was found with a beaded appearance of the distal right renal artery beginning 1.5 cm from the ostium (Figure 1), a finding compatible with and pathognomonic for fibromuscular dysplasia (FMD). The branch to the lower pole was completely occluded and reconstituted by collateral vessels of the right adrenal artery (Videos 1 and 2). The presumptive diagnosis was renovascular hypertension secondary to chronic ischemia of the lower pole of the right kidney.
Figure 1.
CTA of the Abdomen
Beaded appearance of the distal right renal artery beginning 1.5 cm from the ostium (red arrow, left). CTA = computed tomography angiography.
Management
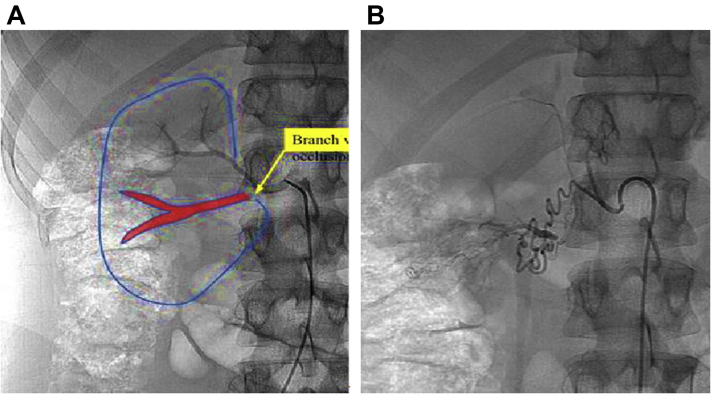
The patient was referred to interventional cardiology for renal artery branch vessel recanalization. A diagnostic renal angiogram (Figures 2A and 2B) confirmed the previous CTA result. Recanalization of the chronically occluded branch was not technically feasible because of the distal site and ambiguous cap of the occlusion with resultant perforation risk. The decision was made to attempt selective embolization of the small collateral noted on CTA to be feeding the lower pole of the right kidney. The right adrenal artery was cannulated using coaxial microcatheters to advance the catheters past the point of occlusion and superselectively embolize the lower pole with microspheres (100 to 300 μm) to produce an intentional infarct of the ischemic segment of the kidney. Extreme tortuosity combined with the small caliber of collateral vessels (<1 mm in diameter) precluded superselective catheterization. Thus, microsphere embolization could not be safely performed because of the risk of nontarget embolization (i.e., infused particles could flow to the normal portions of the kidney and/or the adrenal gland and cause complete renal and/or adrenal infarction). Instead, embolization microcoils (Figure 3) were deployed as both a diagnostic and a therapeutic maneuver with the rationale being that if blood flow was decreased to the lower pole of the kidney and that alleviated hypertension, it would confirm the renovascular origin of hypertension even though it may not have long-term benefit.
Figure 2.
Diagnostic Renal and Adrenal Angiogram
(A) Completely occluded renal branch to the lower pole of the right kidney (red drawing) and (B) reconstituted through collateral vessels from the right adrenal artery.
Figure 3.
Adrenal Angiogram and Coil Embolization
Cannulation of the right adrenal artery, which gives off collateral vessels to the lower pole of the right kidney (left) and therapeutic microcoil embolization (right).
Because coils are deployed in a more controlled fashion than particles, in this patient, they were thought to constitute a “safer” embolic strategy with the risk of unintentional infarction generally avoided. The post-coil embolization angiogram showed no immediate blood flow to the lower pole of the right kidney (Figure 3).
The patient was discharged the next day and arranged to follow up with our center in 2 weeks. Despite a dramatic initial improvement in BP after the procedure, hypertension recurred approximately 2 weeks later, with BP values reported in the 150/90 mm Hg, range despite frequent adjustment to her medications, including the addition of telmisartan 80 mg daily. She was referred to urology for a partial right heminephrectomy to remove the ischemic lower pole because transient interruption of flow had resulted in the desired therapeutic outcome, albeit transiently. The surgery and recovery were uneventful. Two weeks after surgery, her BP improved gradually to ∼110/70 mm Hg, thus mandating reduction and ultimately discontinuance of all BP medical therapy. Six months after the heminephrectomy, the patient reported normal BP without the need to restart antihypertensive medications on a routine basis.
Discussion
FMD of the renal arteries accounts for 5% to 10% of cases in adults who present with renovascular hypertension. The disease is usually diagnosed and confirmed radiologically, whereas histopathologic examination is no longer part of the work-up to reach the diagnosis (1). Although some patients with FMD achieve BP control with medical therapy, most remain unresponsive and may require a revascularization strategy (2). In our patient, the disease process involved an occluded vessel extending into the lower pole of the right kidney. Interestingly, this lower pole was instead supplied by collateral vessels from the right adrenal artery, an adaptation described in humans and animal models in response to renal artery occlusion (3). In contrast to other organs such as the heart, the effectiveness of collateral vessels in preserving kidney function remains controversial and depends largely on the degree of the stenotic vessel (3). In our report, these collateral vessels failed to supply the lower pole of the right kidney adequately and alleviate ischemia, thus stimulating activation of the renin-angiotensin system, as evident by increasing levels of renin and aldosterone. In a perfect case scenario, targeting the stenotic vessel will undo ischemic responses and probably diminish molding forces for collateral vessel formation.
In our patient, the anatomic location was not amenable to revascularization, and therefore, a different approach was implemented, targeting the collateral circulation from the right adrenal gland to induce a partial “functional nephrectomy.” Although this approach proved helpful initially, it lost effectiveness over 6 weeks, likely because of enlargement of small collateral vessels that could not be embolized. If more selective microsphere embolization could have been safely performed, the likelihood of success would have been much higher because this type of embolic strategy would result in tissue infarction.
Unlike small-caliber microspheres (100 to 300 μm), microcoils (2 to 4 mm) do not tend to induce infarction because of their larger size and more proximal occlusion. Our approach, to intervene surgically and remove the ischemic portion of the right kidney, was therefore clinically justified given the localization of the disease and intact other branches of the right renal artery.
Geyskes et al. (4) reported a case in the 1970s that bears a resemblance to our patient with left renal artery branch obstruction and infarction of that portion of the kidney. The investigators then pursued a left nephrectomy, resulting in a cure of resistant hypertension. Histological examination revealed hyperplasia in the juxtaglomerular apparatus and increased renin levels in the center portion of the ischemic kidney. Additionally, before surgery, these investigators obtained 3 biopsy specimens, including 1 specimen from the center of the ischemic area. After a few hours of incubation, the angiotensin level was measured in each tissue extract. Extract from the ischemic area yielded higher angiotensin activity and produced a prolonged BP response typical of renin after being injected directly into the animal model.
The involvement of renin in the pathophysiology of hypertension following partial renal infarction has also been reported by several other investigators. McDonald et al. (5) described a patient with resistant hypertension who had right renal artery thrombosis resulting in multiple renal infarcts. The patient underwent a total nephrectomy that subsequently cured his BP. The renin content in the removed kidney was 30 times higher than normal kidney renin content. This observation may partially explain why renin-angiotensin system blockade provides incomplete BP response at maximal therapeutic doses in patients with renal artery disease. Taken together, these experiments demonstrated clear evidence of hypertension being quelled following the removal of the ischemic part of the kidney. This is a viable option for patients who failed to meet the criteria for minimal surgical interventions, as in this case.
Follow-Up
At 6 months after surgery, the patient continues to have normal BP <130/80 mm Hg without BP medications. She does have occasional elevations up to 160/95 mm Hg during periods of extreme mental stress, however. These episodes are treated with meditation and deep breathing exercises and resolve within 15 to 20 min.
Conclusions
Partial or complete nephrectomy should be considered in patients with FMD who have not responded to other minimal surgical interventions to control BP.
Author Disclosures
Dr. Bakris is a consultant for Merck, Relypsa, KBP Biosciences, and In Regen; and is on the steering committee for clinical trials, with support paid to his employer, the University of Chicago Medicine, for Bayer, Vascular Dynamics, and Novo Nordisk. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Renal Angiogram
Completely occluded renal branch to the lower pole of the right kidney.
Adrenal Angiogram
Collateral vessels from the right adrenal artery to the lower pole of the right kidney.
References
- 1.Piercy K.T., Hundley J.C., Stafford J.M. Renovascular disease in children and adolescents. J Vasc Surg. 2005;41:973–982. doi: 10.1016/j.jvs.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Trinquart L., Mounier-Vehier C., Sapoval M., Gagnon N., Plouin P.F. Efficacy of revascularization for renal artery stenosis caused by fibromuscular dysplasia: a systematic review and meta-analysis. Hypertension. 2010;56:525–532. doi: 10.1161/HYPERTENSIONAHA.110.152918. [DOI] [PubMed] [Google Scholar]
- 3.Lohse J.R., Shore R.M., Belzer F.O. Acute renal artery occlusion: the role of collateral circulation. Arch Surg. 1982;117:801–804. doi: 10.1001/archsurg.1982.01380300043010. [DOI] [PubMed] [Google Scholar]
- 4.Geyskes G.G., Misage J.R., Bron K., Haas J.E., Berg G., Shapiro A.P. Malignant hypertension following renal artery branch obstruction. JAMA. 1972;222:457–459. [PubMed] [Google Scholar]
- 5.Mc Donald R.T., Szilagyi E., Smith R.F. Nephrogenic hypertension (Goldblatt+ kidney) following operative trauma to the renal artery. Circulation. 1958;18:71–75. doi: 10.1161/01.cir.18.1.71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Renal Angiogram
Completely occluded renal branch to the lower pole of the right kidney.
Adrenal Angiogram
Collateral vessels from the right adrenal artery to the lower pole of the right kidney.