Abstract
We describe a case of an adult patient with embolization of a varicocele coil (7 × 70 mm) to the right ventricle. We review the multimodality imaging techniques used to identify location and the importance of a multidisciplinary approach in determining management. (Level of Difficulty: Advanced.)
Key Words: foreign body, right heart, 3-dimensional imaging, tricuspid valve, varicocele coil
Graphical abstract
History of Presentation
A 29-year-old male patient presented with atypical left-sided chest pain and cold fingers and hands. The patient maintained a high level of physical activity. He had a history of smoking. His physical examination was unremarkable.
Learning Objectives
-
•
Migration of a varicocele coil is a rare but important complication.
-
•
Three-dimensional echocardiography is useful in determining exact location and to guide surgical options.
-
•
Multidisciplinary input, including patient participation, is important, particularly given the lack of data on long-term sequelae of migration.
Past Medical History
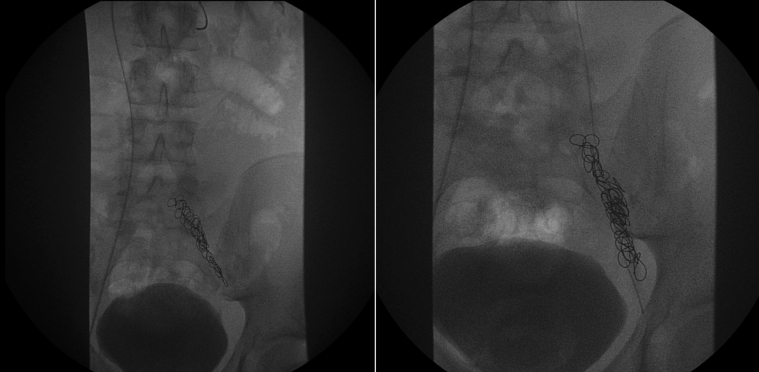
In 2005, at age 15 years, he had a varicocele operation. This was his only past medical history. Reviewing his surgical documentation, this was noted as a difficult procedure. The first attempt was abandoned. He had further radiologic studies to assess feasibility of inserting a microcoil versus a more invasive procedure. It was thought at this point that his anatomy would support a further attempt at coiling the testicular vein. He had approximately 14 microcoils inserted measuring 7 × 70 mm (Figure 1).
Figure 1.
Radiograph
Varicocele procedure.
Differential Diagnosis
He was referred to the rheumatology team in 2015 to investigate the cause of his peripheral vasospastic symptoms and exclude a connective tissue disorder, vasculitis, or primary Raynaud phenomenon. It is unclear if this was the time of embolization.
Investigations
He had a chest radiograph that revealed a foreign structure (Figure 2).
Figure 2.
Chest Radiograph
Foreign object in the heart.
Further cardiac investigations including cardiac magnetic resonance imaging, a 3-dimensional transthoracic echocardiogram, and a computed tomogram were performed. The computed tomography confirmed a foreign body in the heart; however, we could not localize the mass because of artefact from the foreign body (Figure 3). It was also difficult to assess exact location on cardiac magnetic resonance imaging (Figure 4); however, a small metallic artefact was seen.
Figure 3.
Computed Tomography Scan
Varicocele coil in the right side of the heart. The exact location could not be identified because of artefact from the coil.
Figure 4.
Cardiac Magnetic Resonance Imaging
Varicocele coil in the right heart. The exact location could not be identified because of artefact from the coil.
A 2-dimensional and 3-dimensional transthoracic echocardiogram (Figure 5, Videos 1, 2, 3, and 4) identified a well-defined 3.3-cm foreign object in the basal right ventricle attached to the posterior annulus of the tricuspid valve measuring. There was mild tricuspid insufficiency. The biventricular size and function were normal.
Figure 5.
2-Dimensional/3-Dimensional Echocardiogram
Varicocele coil embedded into the tricuspid valve annulus in the right ventricle.
Management
He was discussed in a heart valve multidisciplinary meeting. The options of surgical extraction, percutaneous extraction, and conservative management were considered. On balance with a perceived long-term risk of infective endocarditis, potential risk of thrombi formation, risk of further embolization to the lungs, and potential for tricuspid insufficiency, and the patient’s wish for removal, the decision was made to proceed with removal of this varicocele coil. The method of extraction was discussed in depth. Given the size of the foreign body (7 × 70 mm, 14 coils), the location next to the tricuspid valve apparatus with a suggestion that the coil was embedded into the right ventricle, and that the exact timing of the embolization was unclear (first presentation of symptoms was 2015), there was concern regarding damage to the tricuspid valve apparatus using percutaneous methods and need for emergency surgical intervention. The consensus was that the perceived risk of tricuspid valve injury was high, therefore surgical option was preferred.
Surgical extraction of the coil was performed via a median sternotomy using full cardiopulmonary bypass and arrest of the heart with antegrade cardioplegia. The right atrium was opened and the coil was identified in the subtricuspid valvular apparatus of the right ventricle in close proximity to the septal and posterior leaflets (Figure 6). The coil was carefully removed and the tricuspid was repaired with a 4.0 Prolene commissural stitch. The varicocele had scar tissue associated with it, suggesting that embolization was likely to have occurred a significant time before this presentation.
Figure 6.
Perioperative Images
Varicocele coil at the subtricuspid apparatus and post-extraction.
Discussion
Percutaneous embolization of the testicular vein with coils is a commonly performed treatment of varicocele. Reports of intravascular migration of embolization coils are rare. In a review of 20 cases series (n = 574) and 115 case reports (n = 127) involving iatrogenic intravascular foreign bodies, just 20 were a result of coil embolization (1). Two previous cases of varicocele coil embolization have been reported to the pulmonary artery. Fu and Hsia (2) report a case of embolization to the left pulmonary artery which resulted in a small distal pulmonary infarct. The coil was managed conservatively because of the risk of retrieval. Chomyn et al. (3) had previously reported a similar case of coil embolization to the right lower lobe pulmonary artery that was successfully retrieved using a percutaneous approach. Such percutaneous retrieval has become the mainstay of management of such migrated devices (4).
The current case report is unique in that the coil became lodged within the right ventricle of the heart in close proximity to the tricuspid valve. The need to remove an intracardiac foreign body stems from the symptoms that it causes or from the complications that might arise from it remaining in the heart or embolizing downstream. The patient presented with atypical chest pain and it was unclear whether the malpositioned coil was related, therefore the decision was based on the potential for serious complications if left in situ. A multidisciplinary approach was taken to advise on whether removal was indicated. The use of multimodality imaging allowed the exact location of the coil to be determined. A percutaneous retrieval was not deemed suitable because of the coil’s close proximity to the tricuspid valve and that it was partially embedded in the ventricular wall. As such, the multidisciplinary team recommended surgical removal.
Because of the relative rarity and heterogeneous presentation of intracardiac metallic foreign bodies, no consensus management guidelines exist and there is a lack of evidence on the long-term outcomes of such patients. However, a literature review by Wang et al. (5) concludes that most evidence favors early removal of the intracardiac foreign bodies to prevent complications, such as infection, thrombosis, and further distal embolization. Fisher and Ferreyro (6) performed a review of patient outcomes in cases of catheter embolization, and report a 71% incidence of death or serious complication in patients in whom the fragment was not removed. The majority of fatal complications involved foreign objects in the cardiac chambers. More recent reports argue that asymptomatic intracardiac metallic foreign bodies that are clean, smooth, <10 mm in size, in the right side of the heart or completely embedded within myocardium are less likely to be life-threatening and may be left alone (7, 8, 9). Where this is not the case, removing intracardiac foreign bodies seems justified when a less invasive percutaneous approach is possible. The decision is more complex where the foreign body is in a position that prevents percutaneous removal, as in the current case. If open removal is necessary, the associated risk of sternotomy and cardiopulmonary bypass must be weighed against the risk of complications from a conservative approach.
Follow-Up
The patient weaned from cardiopulmonary bypass without the need for inotropic support and made an uncomplicated recovery. Three days post-procedure, an echocardiogram revealed a normal size right ventricle, with reduced radial and longitudinal function. The tricuspid repair was functioning well, with no restriction and trivial regurgitation. He was discharged home on the fifth post-operative day.
Conclusions
Varicocele coil embolization is a rare complication. Embolization to the right ventricle has never been reported in the literature. The potential risk of having a foreign body in the right ventricle, and patient wish, were key to making a decision for surgical removal. The use of imaging techniques, such as 3-dimensional echocardiography, were important in determining location and surgical options.
Author Disclosures
All authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
Sarah Moharem-Elgamal, MD, PhD, served as Guest Editor-in-Chief for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
3-dimensional ECHO images, revealing a foreign body in the right ventricle.
2-dimensional ECHO images, revealing a foreign body in the right ventricle.
2-dimensional ECHO images, revealing a foreign body in the right ventricle.
2-dimensional ECHO images, revealing a foreign body in the right ventricle.
References
- 1.Schechter M.A., O’Brien P.J., Cox M.W. Retrieval of iatrogenic intravascular foreign bodies. J Vasc Surg. 2013;57:276–281. doi: 10.1016/j.jvs.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Fu J., Hsia D. Embolization coil migration: an unusual cause of pulmonary embolism. Chest. 2015;148:997A. [Google Scholar]
- 3.Chomyn J.J., Craven W.M., Groves B.M., Durham J.D. Percutaneous removal of a Gianturco coil from the pulmonary artery with use of flexible intravascular forceps. J Vasc Interv Radiol. 1991;2:105–106. doi: 10.1016/s1051-0443(91)72481-0. [DOI] [PubMed] [Google Scholar]
- 4.Gabelmann A., Kramer S., Gorich J. Percutaneous retrieval of lost or misplaced intravascular objects. AJR Am J Roentgenol. 2001;176:1509–1513. doi: 10.2214/ajr.176.6.1761509. [DOI] [PubMed] [Google Scholar]
- 5.Wang X., Zhao X., Du D., Xiang X. Management of metallic foreign bodies in the heart. J Card Surg. 2012;27:704–706. doi: 10.1111/jocs.12005. [DOI] [PubMed] [Google Scholar]
- 6.Fisher R.G., Ferreyro R. Evaluation of current techniques for nonsurgical removal of intravascular iatrogenic foreign bodies. AJR Am J Roentgenol. 1978;130:541–548. doi: 10.2214/ajr.130.3.541. [DOI] [PubMed] [Google Scholar]
- 7.LeMaire S.A., Wall M.J., Jr., Mattox K.L. Needle embolus causing cardiac puncture and chronic constrictive pericarditis. Ann Thorac Surg. 1998;65:1786–1787. doi: 10.1016/s0003-4975(98)00246-x. [DOI] [PubMed] [Google Scholar]
- 8.Symbas P.N., Symbas P.J. Missiles in the cardiovascular system. Chest Surg Clin N Am. 1997;7:343–356. [PubMed] [Google Scholar]
- 9.Datta G., Sarkar A., Mukherjee D. A foreign body in the heart. Arch Cardiovasc Dis. 2011;104:684–685. doi: 10.1016/j.acvd.2011.04.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
3-dimensional ECHO images, revealing a foreign body in the right ventricle.
2-dimensional ECHO images, revealing a foreign body in the right ventricle.
2-dimensional ECHO images, revealing a foreign body in the right ventricle.
2-dimensional ECHO images, revealing a foreign body in the right ventricle.