Abstract
Treatment with a combination of norepinephrine and doxazosin was effective in a patient with pheochromocytoma who had blood pressure fluctuation, hypotension, and recurrent syncope. After adrenalectomy, his blood pressure, heart rate, and plasma levels of catecholamines remained normal and stable without any medication. (Level of Difficulty: Beginner.)
Key Words: adrenalectomy, doxazosin, fluctuation of blood pressure, norepinephrine, pheochromocytoma
Abbreviations and Acronyms: BP, blood pressure; DOA, dopamine; EPI, epinephrine; HR, heart rate; NE, norepinephrine; Pheo, pheochromocytoma
Graphical abstract
Treatment with a combination of norepinephrine and doxazosin was effective in a patient with pheochromocytoma who had blood pressure fluctuation…
Pheochromocytoma (Pheo) is a rare tumor. It is a neoplasm of chromaffin cells in the adrenal gland, and it secretes a large amount of catecholamines, leading to hypertension. A few patients with Pheo have hypotension and syncope that may be due to hypotension despite having high circulating levels of catecholamines (1, 2, 3, 4, 5). Stabilization of blood pressure (BP) by medication is difficult in such patients.
Learning Objectives
-
•
In patients with pheochromocytoma, hypotension and BP fluctuation are rare phenomena.
-
•
Treatment with a combination of NE and doxazosin was effective in a patient with Pheo who had BP fluctuation, hypotension, and recurrent syncope.
-
•
After adrenalectomy, the patient’s BP, HR, and plasma levels of catecholamines remained normal and stable without any medication.
History of Presentation
An 84-year-old man suffered from recurrent syncope when sitting upright following transurethral resection of the prostate.
Past Medical History
The patient had a history of benign prostate hypertrophy and bronchial asthma. He had no history of hypertension.
Differential Diagnosis
It is well known that syncope has many causes including diseases, injuries, and drugs. In this case, differential diagnoses included vasovagal syncope, carotid sinus syncope, situational syncope, autonomic failure, volume deletion, cardiac arrhythmias, structural cardiac or cardiopulmonary disease, and cerebrovascular disease.
Investigations
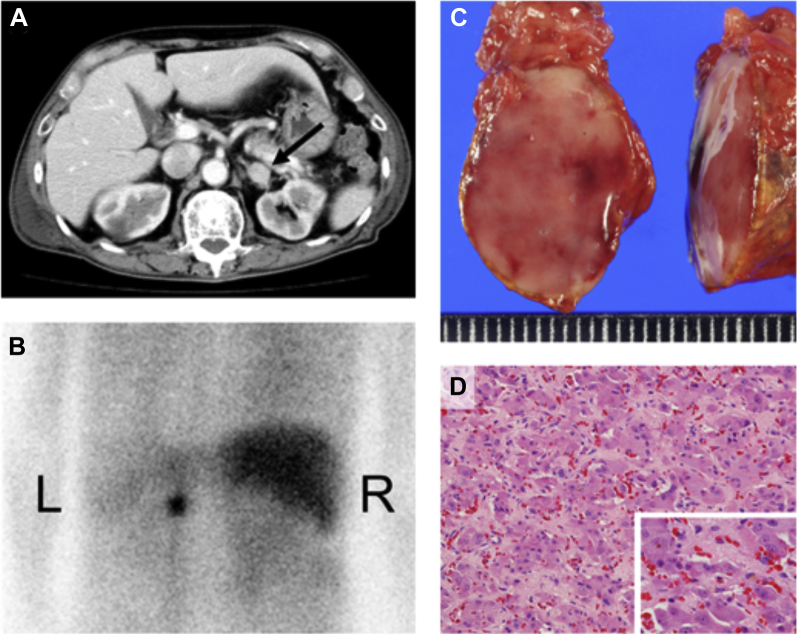
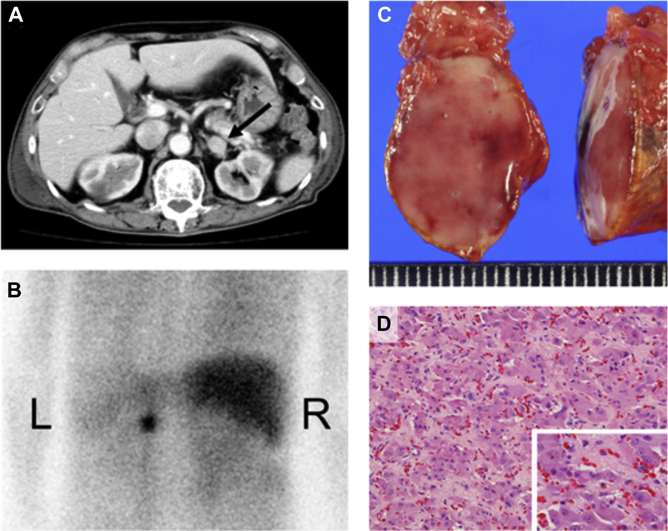
Plasma levels of and 24-h excretion levels of catecholamines, including norepinephrine (NE), epinephrine (EPI), and dopamine (DOA), were increased. Abdominal contrast-enhanced computed tomography showed a left adrenal mass (Figure 1A). A 123I-metaiodobenzlguanidine scan showed intensive uptake in the left adrenal lesion (Figure 1B). Laparoscopic left adrenalectomy was performed. A 22 × 20 × 15 mm solid tumor was excised. A mahogany-colored tumor with an overlying normal adrenal cortex was seen (Figure 1C). Histological examination of the resected adrenal tumor revealed that tumor cells were arranged in a zellballen pattern (Figure 1D). He was diagnosed with adrenal Pheo.
Figure 1.
Contrast-Enhanced Computed Tomography Scan, 123I-Metaiodobenzlguanidine Scan, Macroscopy of the Tumor, and Hematoxylin and Eosin Staining
(A) A contrast-enhanced computed tomography scan showing a left adrenal mass (arrow). (B)123I-metaiodobenzlguanidine scan displaying intensive uptake in the adrenal mass. A tumor of 22 × 20 × 15 mm in size was excised. (C) A mahogany-colored tumor with an overlying normal adrenal cortex was. (D) Hematoxylin and eosin–stained section (200×) of the resected adrenal tumor. Tumor cells in the pheochromocytoma were arranged in a zellballen pattern.
Management
After being hospitalized, intra-arterial BP and heart rate (HR) were monitored because fluctuations (oscillation pattern) of BP and HR were found. Intra-arterial systolic BP (Figure 2A, red line) and HR (Figure 2A, green line) fluctuated from 50 to 180 mm Hg and from 80 to 120 beats/min, respectively, with a 30-min cycle, and systolic BP and HR changed reciprocally. Black bars in Figure 2A shows BP measured by using a mercury sphygmomanometer. After intravenous administration of NE at a dose of 0.6 mg/h on day 3, fluctuations of BP and HR were improved (Figure 2B, arrow). However, on day 4, fluctuation cycles of BP and HR appeared again after 8 h of disappearance of fluctuations of BP and HR during treatment with NE (Figure 2C). Fluctuation cycles of BP and HR became gradually longer and irregular on day 6 (Figure 2D). Doxazosin mesilate at a dose of 2 mg/day was orally administered from day 7 under intravenous administration of NE, resulting in complete disappearance of fluctuation cycles of BP and HR on day 9 (Figure 2E). The NE infusion dose was gradually reduced, and infusion was discontinued 15 days after the start of treatment. Ringer’s lactate solution was co-infused with NE at a fixed infusion rate of 20 ml/h using 2 luminal central venous catheters until the discontinuation of NE infusion. Plasma levels of catecholamines were increased during both the high- and low-BP periods on day 2 before NE infusion (NE of 19,876 pg/ml, EPI of 15,607 pg/ml, and DOA of 816 pg/ml; and NE of 18,788 pg/ml, EPI of 16,079 pg/ml, and DOA of 798 pg/ml, respectively). Plasma levels of catecholamines were almost the same in the high- and low-BP periods. The 24-h urinary excretion levels of catecholamines were increased (NE of 1,437.5 μg/day, EPI of 774.0 μg/day, and DOA of 668.0 μg/day) on admission day.
Figure 2.
Changes in Blood Pressure and Heart Rate After Hospitalization Until Adrenalectomy
(A) Fluctuations of intra-arterial blood pressure and heart rate were found after hospitalization. (B) After administration of norepinephrine, fluctuations of blood pressure and heart rate were improved on day 3 (arrow). (C) Fluctuation cycles of blood pressure and heart rate appeared again on day 4. (D) Fluctuation cycles of blood pressure and heart rate became longer and irregular on day 6. (E) Oral administration of doxazosin completely stopped the fluctuation cycle on day 9.
Discussion
In patients with Pheo, hypotension and BP fluctuation are rare phenomena (3, 4, 5, 6, 7, 8). It is thought that down-regulation of catecholamine receptors and a decrease in blood volume caused by inhibition of the renin-angiotensin-aldosterone system contribute to hypotension in patients with Pheo (9). However, the mechanisms by which hypotension and BP fluctuation occur in these patients despite an increase in catecholamine level remain unclear. In addition, there is no consensus concerning management of hypotension and BP fluctuation due to Pheo. Interestingly, in the present case, plasma levels of catecholamines were increased during both the hypertension and hypotension periods. Adrenalectomy normalized and stabilized his BP, HR and plasma levels of catecholamines. These findings suggest that increases in plasma levels of catecholamines contributed to, at least in part but not directly, his symptoms. However, we do not know the precise mechanisms by which hypotension and BP fluctuation occurred in the patient.
It has been shown that the alpha-/beta-1-adrenergic receptor antagonist NE and the alpha-adrenergic receptor antagonist phentolamine improve hypotension in patients with Pheo (1, 2, 3, 4,8). Conversely, there are some reports showing that phentolamine had no effect on hypotension and BP fluctuation in patients with Pheo (4,5). Unfortunately, there is no gold standard strategy or management for improving fluctuation of BP and hypotension-induced syncope in patients with Pheo. We had learned from a previous similar patient that intravenous administration of NE was useful for improvement of fluctuation of BP, especially hypotension (4). Thus, as the first step of treatment for BP fluctuation and severe hypotension with syncope, we selected treatment with intravenous administration of NE, not phentolamine or a beta-adrenergic receptor antagonist, which may provoke aggravation of hypotension. Fortunately, BP, fluctuation hypotension, and recurrent syncope were controlled well by treatment with a combination of NE and doxazosin in the present case. Consideration should be given to the use of NE and doxazosin for treatment of BP fluctuation in patients with Pheo because both agents are a double-wedged sword for control of BP in these patients. After administration of NE, his BP was stabilized, and then we could safely administer doxazosin and finally perform adrenalectomy. In cases such as the present case, in which a unilateral adrenal secretes large amounts of catecholamines and causes BP fluctuation, hypotension, and recurrent syncope, adrenalectomy should be performed after stabilization of BP.
In the patient, we measured 24-h urinary excretion of catecholamines only once on admission day. Repeated measurements of 24-h urinary excretion levels of catecholamines or metanephrines would enable more specific conclusions concerning the role of catecholamines in the pathophysiology of the BP fluctuation in the patient to be drawn.
Follow-Up
After adrenalectomy, his BP, HR, and plasma levels of catecholamines remained normal and stable without any medication.
Conclusions
We presented a case of Pheo in a patient who had no history of hypertension and who suffered from recurrent syncope when sitting upright following transurethral resection of the prostate. Treatment with a combination of NE and doxazosin was effective for BP fluctuation, hypotension, and recurrent syncope. Adrenalectomy resulted in complete stabilization of his BP, HR, and plasma levels of catecholamines without any medication.
Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Parkinson T. Pheochromocytoma presenting as postural hypotension. Proc R Soc Med. 1964;57:673–674. doi: 10.1177/003591576405700806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baxter M.A., Hunter P., Thompson G.R. Phaeochromocytomas as a cause of hypotension. Clin Endocrinol. 1992;37:304–306. doi: 10.1111/j.1365-2265.1992.tb02326.x. [DOI] [PubMed] [Google Scholar]
- 3.Ueda T., Oka N., Matsumoto A. Pheochromocytoma presenting as recurrent hypotension and syncope. Intern Med. 2005;44:222–227. doi: 10.2169/internalmedicine.44.222. [DOI] [PubMed] [Google Scholar]
- 4.Pesek J., Treska V., Ferda J. Unusual case of pheochromocytoma with a surprising response to the intravenous administration of norepinephrine. Circulation. 2005;112:e327–e328. doi: 10.1161/CIRCULATIONAHA.105.531509. [DOI] [PubMed] [Google Scholar]
- 5.Bengt H. Sustained hypotension and shock due to an adrenaline-secreting pheochromocytoma. Lancet. 1962;21:123–124. doi: 10.1016/s0140-6736(62)90006-5. [DOI] [PubMed] [Google Scholar]
- 6.Ganguly A., Grim C.E., Weinberger M.H. Rapid cyclic fluctuations of blood pressure associated with an adrenal pheochromocytoma. Hypertension. 1984;6:281–284. [PubMed] [Google Scholar]
- 7.Wenting G.J., Man in 't Veld A.J., Boomsma F. Cyclic blood pressure changes in a patient with a phaeochromocytoma: role of a central oscillator? J Hypertens Suppl. 1985;3:S347–S349. [PubMed] [Google Scholar]
- 8.Otsuka M., Kohno K., Itoh A. Periodic fluctuation of blood pressure and transient left ventricular apical ballooning in pheochromocytoma. Heart. 2006;92:1837. doi: 10.1136/hrt.2006.088385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Streeten D.H., Anderson G.H., Jr. Mechanisms of orthostatic hypotension and tachycardia in patients with pheochromocytoma. Am J Hypertens. 1996;9:760–769. doi: 10.1016/0895-7061(96)00057-x. [DOI] [PubMed] [Google Scholar]