Abstract
Severe cases of coronavirus disease 2019 (COVID-19) managed in the intensive care unit are prone to complications, including secondary infections with opportunistic fungal pathogens. Systemic fungal co-infections in hospitalized COVID-19 patients may exacerbate COVID-19 disease severity, hamper treatment effectiveness and increase mortality. Here, we reiterate the role of fungal co-infections in exacerbating COVID-19 disease severity as well as highlight emerging trends related to fungal disease burden in COVID-19 patients. Furthermore, we provide perspectives on the risk factors for fungal co-infections in hospitalized COVID-19 patients and highlight the potential role of prolonged immunomodulatory treatments in driving fungal co-infections, including COVID-19-associated pulmonary aspergillosis (CAPA), COVID-19-associated candidiasis (CAC) and mucormycosis. We reiterate the need for early diagnosis of suspected COVID-19-associated systemic mycoses in the hospital setting.
Keywords: COVID-19, fungal co-infections, corticosteroid treatment, COVID-19-associated candidiasis, COVID-19-associated pulmonary aspergillosis, mucormycosis
1. Introduction
The current COVID-19 disease has infected over 180 million people worldwide, with associated deaths in upwards of 3.9 million [1]. The disease is characterized by a variety of symptoms, of which breathing difficulties are typical of severe cases [2]. Such severe cases require urgent intervention in hospitals, including oxygenation and mechanical ventilation. For such patients, a variety of other complications may arise, including hospital-acquired secondary infections with opportunistic pathogens, including molds and yeast infections. In the current severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) pandemic, fungal co-infections among COVID-19 patients in intensive care units (ICUs) has been reported [3,4,5,6,7]. White et al. [7] reported an incidence of 14.1% and 12.6% for aspergillosis and yeast infections, respectively, amongst critically ill COVID-19 patients across multiple centers in Wales. Bartoletti et al. [6] reported a higher incidence of 27.7% for invasive pulmonary aspergillosis (IPA) (or COVID-19-associated pulmonary aspergillosis, CAPA) amongst COVID-19 patients (of a 108 patient cohort) requiring invasive mechanical ventilation between late February and April 2020 in Italy. Based on analysis of clinical data from several countries, Salmanton-Garcia et al. [5] found that the aggregate incidence of CAPA was between 1% and 39.1% amongst COVID-19 patients in ICUs. Apart from CAPA, the incidence of candidemia has also been reported among hospitalized COVID-19 patients, with up to 12% (106/889) reported for one health center [8] and between 1.54% and 7.54% for a hospital in Rio de Janeiro, Brazil [9]. Indeed, the observations of fungal co-infections, especially IPA, are not entirely unexpected in the current SARS-CoV-2 outbreak, given that similar observations were made during previous outbreaks of other coronaviruses such as the severe acute respiratory syndrome-coronavirus (SARS-CoV) and the middle east respiratory syndrome coronavirus (MERS-CoV) [10,11,12].
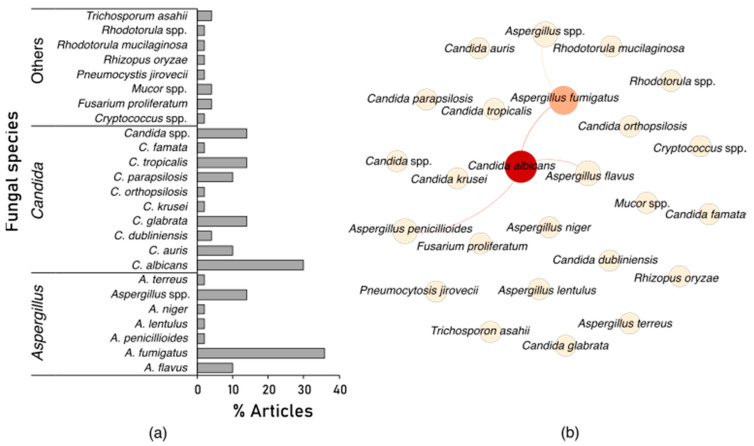
In order to elucidate the diversity and co-occurrence of fungal co-infections in COVID-19 patients, we summarized several randomly selected reports on fungal co-infections in COVID-19 patients (Figure 1). These reports span all but one of the inhabited continents, Africa, where to the best of our knowledge, little or no reports of fungal co-infections in critically ill COVID-19 patients currently exists. Based on our non-exhaustive summary of literature reports, at least 20 different fungal species have been reported in hospitalized COVID-19 patients. The majority of fungal co-infections are due to Aspergillus fumigatus (most common etiological agent of CAPA), followed by Candida albicans (common etiological agent of candidiasis or candidemia) (Figure 1a). Furthermore, we observed significant co-occurrences of Candida albicans and other fungal pathogens such as Aspergillus fumigatus, A. flavus and A. penicillioides amongst the reports (Figure 1b).
Figure 1.
Distribution (a) and co-occurrence (b) of fungal species across randomly selected 50 case studies, prospective and retrospective published reports on fungal co-infections in hospitalized COVID-19 patients [5,7,9,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56] (also see Supplementary Table S1). Searches were done on PubMed (Medline) and Google Scholar using query terms such as “Co-infections”, “coinfections”, “fungi” or “Fungal infections” in combination with either “COVID-19” or “SARS-CoV-2”. Most (>50%) of the selected articles included cases from the onset of the COVID-19 pandemic in several countries (December 2019–April 2020). In the co-occurrence network, nodes are colored based on betweenness centrality (species with high co-occurrence), while edges (connecting lines) indicate significant (p < 0.05) co-occurrence between species. The network was constructed using the visNetwork package of R (https://cran.r-project.org/web/packages/visNetwork/index.html, accessed on 21 May 2021) and further annotated in Gephi (https://gephi.org/, accessed on 21 May 2021).
In this review, we reiterate the role of fungal co-infections in exacerbating COVID-19 disease severity as well as highlight emerging trends related to fungal disease burden and multidrug resistance in COVID-19 patients. In particular, we provide up to date perspective on the risk factors for systemic mycoses in hospitalized patients with a specific focus on the potential role of immunomodulatory and/or immunosuppressive drugs in driving the observed high prevalence of fungal co-infections in COVID-19 patients in the ICU.
2. Fungal Co-Infections in COVID-19 Disease: Disease Severity, the Emergence of Multidrug Resistance and Mucormycosis
2.1. Contribution to COVID-19 Disease Severity and Mortality
Prospective and retrospective data of COVID-19 patients admitted to intensive care units (ICU), especially for a prolonged duration, show that these patients are susceptible to invasive microbial co-infections during hospitalization and that these may lead to more severe outcomes [3,7,16,31]. A prospective cohort study of 135 adults, performed across multiple centers in Wales, showed a significantly higher (up to 25%) mortality rate in COVID-19 patients with fungal infections compared to patients without fungal infections [7]. In particular, a multicenter study of 108 COVID-19 patients admitted to the ICUs in Italy showed a significantly higher 30-day mortality rate for patients with probable COVID-19-associated pulmonary aspergillosis (CAPA) or putative invasive pulmonary aspergillosis, compared to patients without suspected aspergillosis [6]. Similarly, Meijer et al. [38] reported mortality between 40% and 50% in patients with CAPA across the first wave (March–April 2020) and second wave (mid-September to mid-December 2020) of the COVID-19 pandemic in Brazil.
With respect to COVID-19-associated candidiasis (CAC), although the incidence rates may be slightly lower than that of CAPA, the mortality rate of COVID-19 patients with candidemia do not appear to differ markedly. Reports from Italy indicate that up to 57.1% and 50% mortality was reported in COVID-19 patients with candidemia [57] and Candida auris candidemia [27], respectively. Elsewhere, the mortality rate of COVID-19 patients with candidemia exceeded those of counterparts without candidemia in Iran (100% vs. 22.7%) [31]. Altogether, these observations highlight and re-emphasize the propensity of fungal co-infections to exacerbate disease severity and, consequently, increase the mortality of critically ill patients admitted to the ICUs.
2.2. Emergence of Multidrug-Resistant Fungi
Another concerning development is the report of the incidence of multidrug-resistant Aspergillus fumigatus [56] and Candida auris [26,27,58], as well as pan-echinocandin resistant C. glabrata amongst COVID-19 patients [59]. C. auris is a multidrug-resistant fungal pathogen that causes life-threatening systemic infections and could have a 30-day mortality rate of up to 35% [60,61,62] and a report from India stated a case-fatality rate of 60% amongst COVID-19 patients with candidemia due to multidrug-resistant C. auris infection [26]. Managing candidemia outbreaks due to C. auris poses a great challenge due to its resistance to multiple drugs and persistence in the human body and environment [63,64]. Suarez-de-la-Rica et al. [65] observed that co-infections by antimicrobial-resistant pathogens might be consequential for COVID-19 prognosis. In their study, the hazard ratio for death within 90 days in critically ill COVID-19 patients was significantly increased by antimicrobial-resistant pathogens. Hence, given that antifungal resistance undermines treatment efforts and can escalate treatment costs, such reports of multidrug resistance to antifungals, including echinocandins, are worrying. Furthermore, these reports highlight the need to appreciate the global burden of fungal co-infections in the current COVID-19 pandemic and the importance of prompt diagnosis and treatment of fungal pathogens in hospitalized COVID-19 patients.
2.3. Incidence of Mucormycosis
Recent reports emanating from India indicate the incidence of mucormycosis mostly among COVID-19 survivors (although cases in currently hospitalized COVID-19 patients have also been observed) [66,67,68,69]. Mucormycosis is a rare infection caused by filamentous fungi (molds) of the order Mucorales and can be fatal if the fungus penetrates the central nervous system [70,71]. According to one study, Rhizopus arrhizus is currently the most common etiological agent of COVID-19-associated mucormycosis (CAM) in India, with Rhizopus microsporus, Rhizopus homothallicus, Mucor irregularis, Saksenaea erythrospora and Apophysomyces variabilis also implicated in some cases in India and elsewhere [72,73,74]. Mucormycosis infections are common in diabetic or immunocompromised patients, including persons receiving immunosuppressive therapy [71,75]. A recent systematic review of mucormycosis cases in India and worldwide reported that corticosteroid use was recorded in 76.3% of cases and that 30.7% of mucormycosis cases were fatal [76]. Thus far, it is unclear whether the incidence of CAM is worldwide, and research is needed in this regard. Altogether, the foregoing reports and several other studies suggest that the heightened incidence of mucormycosis in India are related to certain risk factors, including poorly managed diabetes and the prolonged usage of high dosage steroids in treating COVID-19 [69,77,78].
3. Overview of Risk Factors for Opportunistic Fungal Infections in Critically Ill COVID-19 Patients
Overall, risk factors driving the high incidence of aspergillosis and candidemia in COVID-19 patients are related to invasive procedures (e.g., intubation) predisposing lung tissues to fungal colonization and proliferation [79,80,81], history of chronic pulmonary disease [7], prolonged corticosteroid treatments [7,82], immunological disposition of patients and antimicrobial therapy [59,64]. In one study comparing co-infections in critically ill patients with and without COVID-19, it was observed that the need for invasive assisted respiration was the most decisive factor for co-infections with antifungal-resistant pathogens in patients with severe COVID-19 [79]. In the following subsections, we provide an overview of risk factors associated with CAPA and CAC—the two most commonly reported fungal co-infections in hospitalized COVID-19 patients.
3.1. Risk Factors for CAPA
Given the high incidence of CAPA and the distinct clinical features of CAPA compared to influenza-associated pulmonary aspergillosis, it has been necessary to establish appropriate case definitions for CAPA in order to facilitate uniformity of reporting across medical practices. To this end, a number of case definitions or guidelines have been proposed for characterizing possible, putative, probable and proven CAPA cases [7,83,84] (case definitions for CAPA is not within the purview of this review). CAPA is essentially defined as pulmonary or tracheobronchial infection with Aspergillus spp. in COVID-19 patients. In one proposed case definition by Koehler et al. [83], a proven case of CAPA may be established by direct microscopic and/or histopathological evidence of fungal features that are typical of Aspergillus spp. Such evidence includes an observation of invasive growth into tissues with concomitant tissue damage, recovery of Aspergillus spp. by culture, detection of Aspergillus by microscopy in histology studies or by polymerase chain reaction from materials obtained by sterile aspiration or biopsies from a pulmonary site indicating an infectious disease.
Several factors predispose hospitalized COVID-19 patients to CAPA. SARS-CoV-2 insults in the lungs elicit the release of danger-associated molecular patterns (DAMPs) in severe COVID-19 [80]. Essentially, DAMPs are host-derived molecules that regulate the activation of pathogen recognition receptors and modulate the host’s organ response to injury [85]. The release of DAMPs is accompanied by inflammation and extensive damage of lung epithelial tissues, which are enabling risk factors for invasive pulmonary aspergillosis [80]. Other pathophysiological factors identified for IPA and potentially CAPA, include an impaired local immune response and a dysfunctional defective mucociliary activity [12,50]. In severe COVID-19 disease, extensive inflammation and injury to the lungs lead to acute respiratory syndrome (ARDS). ARDS is characterized by difficulty in breathing; hence, assisted ventilation is required for such patients. However, mechanical ventilation and the duration of ventilation is a known risk factor for invasive aspergillosis and CAPA in the ICU [50,86,87].
In addition, pharmaceutical treatments for malignancy and the use of corticosteroids (discussed in a later section) and antibiotics may be risk factors for CAPA [7,88]. For example, in a multicenter study across Wales [7], a significant association was observed between COVID-19 patients with IPA and patients treated for or diagnosed with solid malignancy. Further, in a multilocation retrospective cohort conducted in France, Dellière et al. [88] reported that treatment with azithromycin for up to 3 days significantly correlated with the incidence of probable invasive pulmonary aspergillosis in COVID-19 patients. Such observation was attributed to the immunomodulatory properties of azithromycin that may weaken the host’s immune response and subsequent susceptibility to aspergillosis [88,89].
3.2. Risk Factors for CAC
COVID-19-associated candidiasis (CAC) refers to the detection of one or more Candida spp. in the bloodstream or body tissues of COVID-19 patients. As earlier indicated, Candida albicans and other non-albicans Candida species have been reported among hospitalized COVID-19 patients [9,29,57,81]. Some of the risk factors identified for CAC include prolonged hospital stays, mechanical ventilation, central venous catheters, surgical procedure, and the use of broad-spectrum antibiotics [9,29]. For example, Nucci et al. [9] observed that COVID-19 patients with candidemia were more likely to be under mechanical ventilation than non-COVID-19 patients. Similarly, Mastrangelo et al. [57] reported that COVID-19 patients with candidemia were more likely to be in the ICU and receiving immunosuppressive agents than patients in the ICU for reasons other than COVID-19. In another report, the development of pan-echinocandin resistant C. glabarata co-infections in a hospitalized 53-year-old COVID-19 patient potentially rendered antifungal treatment ineffective and probably aggravated the progression of the disease [59]. According to the authors, the case report demonstrated the need for active monitoring for antifungal resistance development in order to inform the dynamic use of effective antifungal agents during patient management in the intensive care unit.
4. Immunosuppressants as Risk Factors for Fungal Infections in Critically Ill COVID-19 Patients
Most of the current treatment options for managing patients with severe COVID-19 are immunomodulators [90]. The anti-inflammatory properties of these immunomodulators are important to counteract the heightened and unregulated release of pro-inflammatory cytokines (also known as ‘cytokine storm’) in the lungs during SARS-CoV-2 infection [91,92]. Thus, immunosuppressants such as dexamethasone, methylprednisolone, prednisone, hydrocortisone and tocilizumab constitute the most common treatment options for managing severe COVID-19 cases in the ICU [90]. From a COVID-19 treatment standpoint, immunostimulants are required during the early stages of the disease, whereas immunosuppressants may be more beneficial to dampen the cytokine storm in the later stages of the disease [93]. For example, dexamethasone treatment decreased the 28-day mortality in COVID-19 patients on invasive respiratory support or receiving oxygen alone but was not particularly beneficial for COVID-19 patients with less severe disease, suggesting that hyper inflammation mediates the advanced stage of the disease and therefore can be alleviated by immunosuppressants [93,94].
Unfortunately, the immunosuppressants hamper both the individual’s innate and adaptive immune responses through sophisticated quantitative and qualitative mechanisms of immune deregulation [88,95,96,97,98], thereby increasing patients’ susceptibility to invasive fungal diseases. In particular, steroidal immunosuppressants such as corticosteroids predominantly affect the protective immunity process qualitatively through functional impairment of several effector immune cells, such as monocytes, polymorphonuclear leukocytes, T lymphocytes and macrophages [96] and is a significant acquired immunological risk factor for pulmonary aspergillosis [99,100]. Thus, corticosteroids such as dexamethasone and methylprednisolone, used for managing critically ill COVID-19 patients, have contraindications, including fostering secondary microbial infections in patients [99,101].
In the present COVID-19 pandemic, questions are being asked regarding the possible relationship between immunosuppressant or corticosteroid use and the incidence of fungal infections in critically ill COVID-19 patients (Table 1). A prospective study conducted across multiple COVID-19 intensive care units in Wales showed that the use of high-dose systemic corticosteroids significantly increased the odds of COVID-19 patients developing aspergillosis [7]. Similarly, in Brazil, Riche et al. [82] observed a 10-fold increase in candidemia amongst a cohort of critically ill COVID-19 patients receiving high doses of corticosteroids such as prednisone, hydrocortisone, methylprednisolone and dexamethasone, while a retrospective study conducted in Chicago and involving 111 COVID-19 patients receiving tocilizumab (a monoclonal antibody that inhibits binding of IL-6 to the membrane and soluble receptors [102]) was significantly linked with the risk of developing fungal pneumonia and sinusitis [103]. However, in a retrospective study involving 4313 COVID-19 patients in New York, corticosteroid use was not associated with increased bacteremia or fungaemia compared to non-corticosteroid users when administered within the first seven days of admission [104]. In this study, the early administration of low dose corticosteroids is advocated. It must, however, be noted that in many of the other reports, mention is made of high doses of corticosteroids often administered for prolonged periods [30], which may explain the high incidence of systemic fungal infections and ultimately negate the lifesaving benefits of these drugs.
Table 1.
Summary of literature on potential links between immunosuppressants and fungal co-infections in severely ill COVID-19 patients.
| Study Type | City, Country | Cohort Size | Immunosuppressants Therapy for COVID-19 | Associated Fungal Infection/Species | Observation with Regards to Corticosteroid Use | Comorbidities and Other Risk Factors | Reference |
|---|---|---|---|---|---|---|---|
| Case series | Salvador, Brazil | 2 | Unspecified | Candida auris | Prolonged corticosteroid therapy (34 days) | Deep-seated venous thrombosis (Patient 1); Chronic renal insufficiency and dialysis, diabetes mellitus, and hypertension (Patient 2) | de Almeida [30] |
| Case series | Nuevo Leon, Mexico | 12 | Hydrocortisone, methylprednisolone, dexamethasone | C. auris | Corticosteroid treatments preceded the onset of C. auris infection. Association not particularly investigated | Obesity, asthma, high blood pressure, diabetes, coronary artery disease; valvular heart disease | Villanueva-Lozano et al. [25] |
| Case series (retrospective) | Porto Alegre, Brazil | 11 | Prednisone, hydrocortisone, methylprednisolone, dexamethasone | Candidemia (Candida spp.) | All cases of candidemia (a 10-fold increase in frequency) in COVID-19 patients occurred after the use of high-doses of corticosteroids |
Diabetes, HIV-positive, central venous catheters. Additional risk factors for candidemia were virtually absent | Riche et al. [82] |
| Prospective study | Madrid, Spain | 8 | Not specified | Aspergillosis (A. fumigatus) | Aspergillosis affected mostly (75%) non-immunocompromised COVID-19 patients receiving corticosteroids |
Obesity, HTA, COPD, CKD, diabetes mellitus; Mostly (75%) non-immunocompromised patients | Machado et al. [105] |
| Prospective cohort | Milan, Italy | 21 | Prednisone, immunomodulators (tocilizumab, mavrilimumab, anakinra, reparixin, and sarilumab) and immunosuppressants (tacrolimus, cyclophosphamide and mycophenolate) | Candidemia (Candida albicans, Candida spp.) | A higher proportion of candidemia present in COVID-19 patients in the ICU and on immunosuppressive agents | Diabetes, broad-spectrum antibiotics, HIV, etc. | Mastrangelo et al. [57] |
| Prospective | Milan, Italy | 43 | Tocilizumab | Candidemia (C. albicans, C. tropicalis, C. parapsilosis) | 6.9% prevalence of candidemia observed | Previous hospitalisation in ICU; central venous catheter | Antinori et al. [34] |
| Case series | Puducherry, India | 10 | Dexamethasone | Orbital mucormycosis (Mucor spp. and Rhizopus spp.) | Five patients developed diabetic ketoacidosis after the initiation of corticosteroid therapy for COVID-19 disease | Diabetes mellitus | Sarkar et al. [72] |
| Case study | Udine, Italy | 1 | Dexamethasone, tocilizumab | Pulmonary aspergillosis (A. fumigatus) | A. fumigatus was isolated 22 days after tocilizumab administration | HBV-related liver cirrhosis, arterial hypertension and mild obesity | Deana et al. [106] |
| Case study | Brazil | 23 | Methylprednisolone, prednisone | Candidemia (C. parapsilosis, C. tropicalis) and Trichosporon asahii fungemia | Fungemia was observed in all patients with a history of prolonged corticosteroid therapy | CVC, exposure to broad-spectrum antibiotics, prior echinocandin therapy, obesity, diabetes | de Almeida Jr [46] |
| Case series | Paris, France | 145 | Tocilizumab, sarilumab, hydrocortisone succinate | IPMI (A. fumigatus; Fusarium proliferatum) | Corticosteroid therapies were related to an increased risk for developing IPMI (odds ratio, 8.55; IQR, 6.8–10.3; p = 0.01) | HTA, overweight/obesity, diabetes mellitus, COPD. Solid organ transplantation was related to an increased risk for IPMI |
Fekkar et al. [107] |
| Prospective | Wales, UK | 135 | Prednisolone, methylprednisolone, hydrocortisone, dexamethasone, fludrocortisone | Aspergillosis, yeast infections (mainly Candida, one case of Rhodotorula fungaemia) | High-dose corticosteroid use increased the likelihood of aspergillosis | Previous chronic respiratory disease also linked to aspergillosis. Associations between comorbidities /underlying conditions and yeast infections were not significant | White et al. [7] |
| Retrospective | New York, USA | 4313 | Methylprednisolone, prednisone, dexamethasone, hydrocortisone | Not reported | Corticosteroid use was not associated with increased bacteraemia or fungaemia compared to non-corticosteroid users when administered within the first 7 days | Hypertension, diabetes, CKD, asthma, COPD | Ho et al. [104] |
| Retrospective cohort study | Paris, France | 21 | Dexamethasone | Aspergillosis (Aspergillus spp.) | Although not statistically significant, a trend was observed between high-dose (≥100 mg) dexamethasone and incidence of IPA | Medical history did not significantly affect IPA | Dellière et al. [88] |
| Retrospective | India | 6 | Prednisolone, dexamethasone, or methylprednisolone | Rhino-orbital mucormycosis (Mucor spp.) | Five patients developed mucormycosis after treatment with corticosteroids. Mean duration between diagnosis of COVID-19 and development of symptoms of mucor was 15.6 ± 9.6 (3–42) days | Type 2 diabetes | Sen et al. [68] |
| Retrospective | Chicago, USA | 111 | Tocilizumab | Fungal pneumonia and sinusitis | Administration of tocilizumab was associated with a higher risk of fungal (p = 0.112) infections | Diabetes mellitus, HTA, obesity COPD, cardiovascular disease | Kimmig et al. [103] |
| Case control study | Barcelona, Spain | 71 cases, 142 controls | Tocilizumab, baricitinib, anakinra, dexamethasone, prednisone, hydroxycortisone | Candida spp., Aspergillus spp., Fusarium spp. | Immunomodifiers did not influence occurrence of nosocomial infections in COVID-19 patients | Chronic liver disease, obesity, smoking, invasive mechanical ventilation, hydroxychloroquine | Meira et al. [108] |
CKD, Chronic kidney disease; COPD, Chronic obstructive pulmonary disease; CVC, central venous catheter; HTA, Hypertension; HBV, Hepatitis B virus; HBD, High blood pressure, ICU, Intensive care unit; IPA, Invasive pulmonary aspergillosis; IPMI, Invasive pulmonary mold infections.
It should also be noted that the correlation between corticosteroid use and incidence of fungal infections in hospitalized COVID-19 patients may be masked by other co-founding risk factors for fungal infections, such as the patient’s history of pulmonary disease, comorbidities and mechanical ventilation [7,109]. For example, in the multicenter study by White et al. [7], apart from corticosteroid use, a history of chronic respiratory disease significantly increased the likelihood of aspergillosis. Importantly, with the exception of the study by Ho et al. [104], most of the currently reported investigations on the potential role between immunosuppressants and fungal infections are from a small cohort of patients. Such a small study size lacks sufficient statistical power and may consequently lead to false conclusions. Indeed, thorough metanalyses of additional retrospective and randomized control studies will help elucidate the role of immunosuppressants in predisposing COVID-19 patients to fungal co-infections.
5. Conclusions
Fungal co-infections are reported in severely ill COVID-19 patients admitted to the ICU, with a higher rate of incidence for aspergillosis followed by candidemia, as observed from our literature analysis. Risk factors for such fungal co-infections in the ICU are related to host factors, medical procedures and therapeutics such as corticosteroids, which are designed to alleviate the COVID-19 disease condition. Thus, the links between fungal infections and higher mortality rates in COVID-19 patients and between treatment options and fungal infections provide a conundrum that challenges current medical practices to develop innovative strategies for limiting secondary nosocomial fungal infections in the hospital setting. However, in the interim, prompt diagnosis of fungal co-infections and antifungal administration may help improve prognosis in hospitalized COVID-19 patients.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jof7070545/s1, Table S1: Bibliographic and geographical information of studies analyzed in Figure 1.
Author Contributions
Conceptualization, C.H.P. and O.G.; methodology, C.H.P.; formal analysis, O.T.E.; investigation, O.T.E., O.G. and C.H.P.; resources, C.H.P.; data curation, O.T.E.; writing—original draft preparation, O.T.E.; writing—review and editing, C.H.P. and O.G.; supervision, C.H.P.; funding acquisition, C.H.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Research Foundation (NRF) of South Africa, grant number 115566. C.H.P. holds an NRF SARChI Research Chair in Pathogenic Yeasts.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Supporting data for Figure 1 is in the supplementary information.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Worldometers COVID Live Update. [(accessed on 23 June 2021)]; Available online: https://www.worldometers.info/coronavirus/
- 2.WHO Coronavirus Disease (COVID-19) [(accessed on 21 May 2021)]; Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 3.Ezeokoli O.T., Pohl C.H. Opportunistic pathogenic fungal co-infections are prevalent in critically ill COVID-19 patients: Are they risk factors for disease severity? S. Afr. Med. J. 2020;110:1081–1085. doi: 10.7196/SAMJ.2020.v110i11.15248. [DOI] [PubMed] [Google Scholar]
- 4.Song G., Liang G., Liu W. Fungal Co-infections Associated with Global COVID-19 Pandemic: A Clinical and Diagnostic Perspective from China. Mycopathologia. 2020;185:599–606. doi: 10.1007/s11046-020-00462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salmanton-García J., Sprute R., Stemler J., Bartoletti M., Dupont D., Valerio M., Garcia-Vidal C., Falces-Romero I., Machado M., de la Villa S., et al. COVID-19-associated pulmonary aspergillosis, March–August 2020. Emerg. Infect. Dis. 2021;27:1077–1086. doi: 10.3201/eid2704.204895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bartoletti M., Pascale R., Cricca M., Rinaldi M., Maccaro A., Bussini L., Fornaro G., Tonetti T., Pizzilli G., Francalanci E., et al. Epidemiology of Invasive Pulmonary Aspergillosis Among Intubated Patients With COVID-19: A Prospective Study. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White P.L., Dhillon R., Cordey A., Hughes H., Faggian F., Soni S., Pandey M., Whitaker H., May A., Morgan M., et al. A National Strategy to Diagnose Coronavirus Disease 2019-Associated Invasive Fungal Disease in the Intensive Care Unit. Clin. Infect. Dis. 2020:1–11. doi: 10.1093/cid/ciaa1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katz J. Prevalence of candidiasis and oral candidiasis in COVID-19 patients: A cross-sectional pilot study from the patients’ registry in a large health center. Quintessence Int. 2021 doi: 10.3290/j.qi.b1491959. [DOI] [PubMed] [Google Scholar]
- 9.Nucci M., Barreiros G., Guimarães L.F., Deriquehem V.A.S., Castiñeiras A.C., Nouér S.A. Increased incidence of candidemia in a tertiary care hospital with the COVID-19 pandemic. Mycoses. 2021;64:152–156. doi: 10.1111/myc.13225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmadi A., Ardehali S.H., Beigmohammadi M.T., Hajiabdolbaghi M., Hashemian S.M.R., Kouchek M., Majidpour A., Mokhtari M., Moghaddam O.M., Najafi A. Invasive candidiasis in intensive care unit; consensus statement from an Iranian panel of experts, July 2013. JRSM Open. 2014;5:1–10. doi: 10.1177/2042533313517689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hwang D.M., Chamberlain D.W., Poutanen S.M., Low D.E., Asa S.L., Butany J. Pulmonary pathology of severe acute respiratory syndrome in Toronto. Mod. Pathol. 2005;18:1–10. doi: 10.1038/modpathol.3800247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schauwvlieghe A.F.A.D., Rijnders B.J.A., Philips N., Verwijs R., Vanderbeke L., Van Tienen C., Lagrou K., Verweij P.E., Van de Veerdonk F.L., Gommers D., et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: A retrospective cohort study. Lancet Respir. Med. 2018;6:782–792. doi: 10.1016/S2213-2600(18)30274-1. [DOI] [PubMed] [Google Scholar]
- 13.Prattes J., Valentin T., Hoenigl M., Talakic E., Reisinger A.C., Eller P. Invasive pulmonary aspergillosis complicating COVID-19 in the ICU—A case report. Med. Mycol. Case Rep. 2021;31:2–5. doi: 10.1016/j.mmcr.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Menon A.A., Berg D.D., Brea E.J., Deutsch A.J., Kidia K.K., Thurber E.G., Polsky S.B., Yeh T., Duskin J.A., Holliday A.M., et al. A case of COVID-19 and Pneumocystis jirovecii coinfection. Am. J. Respir. Crit. Care Med. 2020;202:136–138. doi: 10.1164/rccm.202003-0766LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salehi M., Ahmadikia K., Mahmoudi S., Kalantari S., Jamalimoghadam Siahkali S., Izadi A., Kord M., Dehghan Manshadi S.A., Seifi A., Ghiasvand F. Oropharyngeal candidiasis in hospitalized COVID-19 Patients from Iran: Species identification and antifungal susceptibility pattern. Mycoses. 2020 doi: 10.1111/myc.13137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu X., Ge Y., Wu T., Zhao K., Chen Y., Wu B., Zhu F., Zhu B., Cui L. Co-infection with respiratory pathogens among COVID-2019 cases. Virus Res. 2020;285 doi: 10.1016/j.virusres.2020.198005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He Y., Li W., Wang Z., Chen H., Tian L., Liu D. Nosocomial infection among patients with COVID-19: A retrospective data analysis of 918 cases from a single center in Wuhan, China. Infect. Control Hosp. Epidemiol. 2020;41:982–983. doi: 10.1017/ice.2020.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hughes S., Troise O., Donaldson H., Mughal N., Moore L.S.P. Bacterial and fungal coinfection among hospitalized patients with COVID-19: A retrospective cohort study in a UK secondary-care setting. Clin. Microbiol. Infect. 2020;26:1395–1399. doi: 10.1016/j.cmi.2020.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poignon C., Blaize M., Vezinet C., Lampros A., Monsel A., Fekkar A. Invasive pulmonary fusariosis in an immunocompetent critically ill patient with severe COVID-19. Clin. Microbiol. Infect. 2020;26:1582–1584. doi: 10.1016/j.cmi.2020.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmadikia K., Hashemi S.J., Khodavaisy S., Getso M.I., Alijani N., Badali H., Mirhendi H., Salehi M., Tabari A., Mohammadi Ardehali M., et al. The double-edged sword of systemic corticosteroid therapy in viral pneumonia: A case report and comparative review of influenza-associated mucormycosis versus COVID-19 associated mucormycosis. Mycoses. 2021 doi: 10.1111/myc.13256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Signorini L., Moioli G., Calza S., Van Hauwermeiren E., Lorenzotti S., Del Fabro G., Renisi G., Lanza P., Saccani B., Zambolin G., et al. Epidemiological and Clinical Characterization of Superinfections in Critically Ill Coronavirus Disease 2019 Patients. Crit. Care Explor. 2021;3:e0430. doi: 10.1097/CCE.0000000000000430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gerver S.M., Guy R., Wilson K., Thelwall S., Nsonwu O., Rooney G., Brown C.S., Muller-Pebody B., Hope R., Hall FFPH V. National surveillance of bacterial and fungal co- and secondary infection in COVID-19 patients in England—Lessons from the first wave. Clin. Microbiol. Infect. 2021 doi: 10.1016/j.cmi.2021.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Du Y., Tu L., Zhu P., Mu M., Wang R., Yang P., Wang X., Hu C., Ping R., Hu P., et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan: A retrospective observational study. Am. J. Respir. Crit. Care Med. 2020;201:1372–1379. doi: 10.1164/rccm.202003-0543OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Villanueva-Lozano H., Treviño-Rangel R.d.J., González G.M., Ramírez-Elizondo M.T., Lara-Medrano R., Aleman-Bocanegra M.C., Guajardo-Lara C.E., Gaona-Chávez N., Castilleja-Leal F., Torre-Amione G., et al. Outbreak of Candida auris infection in a COVID-19 hospital in Mexico. Clin. Microbiol. Infect. 2021;27:813. doi: 10.1016/j.cmi.2020.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chowdhary A., Tarai B., Singh A., Sharma A. Multidrug-Resistant Candida auris Infections in Critically Ill Coronavirus Disease Patients, India, April–July 2020. Emerg. Infect. Dis. 2020;26:2694–2696. doi: 10.3201/eid2611.203504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Magnasco L., Mikulska M., Giacobbe D.R., Taramasso L., Vena A., Dentone C., Dettori S., Tutino S., Labate L., Di Pilato V., et al. Spread of carbapenem-resistant gram-negatives and Candida auris during the COVID-19 pandemic in critically ill patients: One step back in antimicrobial stewardship? Microorganisms. 2021;9:95. doi: 10.3390/microorganisms9010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rodriguez J.Y., Le Pape P., Lopez O., Esquea K., Labiosa A.L., Alvarez-Moreno C. Candida auris: A Latent Threat to Critically Ill Patients With Coronavirus Disease 2019. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Al-Hatmi A.M.S.M., Mohsin J., Al-Huraizi A., Khamis F. COVID-19 associated invasive candidiasis. J. Infect. 2021;82:e45–e46. doi: 10.1016/j.jinf.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Almeida J.N., Francisco E.C., Hagen F., Brandão I.B., Pereira F.M., Presta Dias P.H., de Miranda Costa M.M., de Souza Jordão R.T., de Groot T., Colombo A.L. Emergence of Candida auris in brazil in a covid-19 intensive care unit. J. Fungi. 2021;7:220. doi: 10.3390/jof7030220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arastehfar A., Shaban T., Zarrinfar H., Roudbary M., Ghazanfari M., Hedayati M.-T., Sedaghat A., Ilkit M., Najafzadeh M.J., Perlin D.S. Candidemia among Iranian Patients with Severe COVID-19 Admitted to ICUs. J. Fungi. 2021;7:280. doi: 10.3390/jof7040280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meijer E.F.J., Dofferhoand A.S.M., Meis J.F., Hoiting O., Buil J.B. Azole-resistant COVID-19-associated pulmonary aspergillosis in an immunocompetent host: A case report. J. Fungi. 2020;6:79. doi: 10.3390/jof6020079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blaize M., Mayaux J., Nabet C., Nabet C., Lampros A., Marcelin A.G., Marcelin A.G., Thellier M., Thellier M., Piarroux R., et al. Fatal Invasive Aspergillosis and Coronavirus Disease in an Immunocompetent Patient. Emerg. Infect. Dis. 2020;26:1636–1637. doi: 10.3201/eid2607.201603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Antinori S., Bonazzetti C., Gubertini G., Capetti A., Pagani C., Morena V., Rimoldi S., Galimberti L., Sarzi-Puttini P., Ridolfo A.L. Tocilizumab for cytokine storm syndrome in COVID-19 pneumonia: An increased risk for candidemia? Autoimmun. Rev. 2020;19:102564. doi: 10.1016/j.autrev.2020.102564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lahmer T., Kriescher S., Herner A., Rothe K., Spinner C.D., Schneider J., Mayer U., Neuenhahn M., Hoffmann D., Geisler F., et al. Invasive pulmonary aspergillosis in critically ill patients with severe COVID-19 pneumonia: Results from the prospective AspCOVID-19 study. PLoS ONE. 2021;16:e0238825. doi: 10.1371/journal.pone.0238825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Benedetti M.F., Alava K.H., Sagardia J., Cadena R.C., Laplume D., Capece P., Posse G., Nusblat A.D., Cuestas M.L. COVID-19 associated pulmonary aspergillosis in ICU patients: Report of five cases from Argentina. Med. Mycol. Case Rep. 2021;31:24–28. doi: 10.1016/j.mmcr.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alobaid K., Yousuf B., Al-Qattan E., Muqeem Z., Al-Subaie N. Pulmonary aspergillosis in two COVID-19 patients from Kuwait. Access Microbiol. 2021;3 doi: 10.1099/acmi.0.000201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meijer E.F.J., Dofferhoff A.S.M., Hoiting O., Meis J.F. COVID-19–associated pulmonary aspergillosis: A prospective single-center dual case series. Mycoses. 2021;64:457–464. doi: 10.1111/myc.13254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Savi D., Valente G., Iacovelli A., Olmati F., Bezzi M., Palange P. Uncommon presentation of allergic bronchopulmonary aspergillosis during the COVID-19 lockdown: A case report. BMC Pulm. Med. 2020;20:325. doi: 10.1186/s12890-020-01373-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cataldo M.A., Tetaj N., Selleri M., Marchioni L., Capone A., Caraffa E., Caro A.D., Petrosillo N. Incidence of bacterial and fungal bloodstream infections in COVID-19 patients in intensive care: An alarming “collateral effect”. J. Glob. Antimicrob. Resist. 2020;23:290–291. doi: 10.1016/j.jgar.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Didbaridze T., Ratiani L., Labadze N., Maziashvili T., Didbaridze N., Gogokhia N. Prevalence and Prognosis of Candidiasis among Covid-19 Patients: Data from ICU Department. Int. J. Progress. Sci. Technol. 2021;26:36–39. [Google Scholar]
- 42.Alataby H., Atemnkeng F., Bains S.S., Kenne F.M., Diaz K., Nfonoyim J. A COVID-19 Case Complicated by Candida dubliniensis and Klebsiella pneumoniae-Carbapenem-Resistant Enterobacteriaceae. J. Med. Cases. 2020;11:403–406. doi: 10.14740/jmc3588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sari A.P., Darnindro N., Yohanes A., Mokoagow M.I. Role of tocilizumab for concomitant systemic fungal infection in severe COVID-19 patient: Case report. Medicine. 2021;100:e25173. doi: 10.1097/MD.0000000000025173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lescure F.X., Bouadma L., Nguyen D., Parisey M., Wicky P.H., Behillil S., Gaymard A., Bouscambert-Duchamp M., Donati F., Le Hingrat Q., et al. Clinical and virological data of the first cases of COVID-19 in Europe: A case series. Lancet Infect. Dis. 2020;20:697–706. doi: 10.1016/S1473-3099(20)30200-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burgos Santamaría A., Lema T.M., Pizarro C.A.G. Invasive pulmonary aspergillosis in COVID-19. A case series at Gregorio Maranon University General Hospital. Rev. Chil. Anest. 2021 doi: 10.25237/revchilanestv50-03-01. [DOI] [Google Scholar]
- 46.De Almeida J.N., Moreno L., Francisco E.C., Marques G.N., Mendes A.V., Barberino M.G., Colombo A.L. Trichosporon asahii superinfections in critically ill COVID-19 patients overexposed to antimicrobials and corticosteroids. Mycoses. 2021 doi: 10.1111/myc.13333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Patti R.K., Dalsania N.R., Somal N., Sinha A., Mehta S., Ghitan M., Seneviratne C., Kupfer Y. Subacute Aspergillosis “Fungal Balls” Complicating COVID-19. J. Investig. Med. High Impact Case Rep. 2020;8 doi: 10.1177/2324709620966475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vélez Pintado M., Camiro-Zúñiga A., Aguilar Soto M., Cuenca D., Mercado M., Crabtree-Ramirez B. COVID-19-associated invasive pulmonary aspergillosis in a tertiary care center in Mexico City. Med. Mycol. 2021:1–6. doi: 10.1093/mmy/myab009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dupont D., Menotti J., Turc J., Miossec C., Wallet F., Richard J.C., Argaud L., Paulus S., Wallon M., Ader F., et al. Pulmonary aspergillosis in critically ill patients with Coronavirus Disease 2019 (Covid-19) Med. Mycol. 2021;59:110–114. doi: 10.1093/mmy/myaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rutsaert L., Steinfort N., Van Hunsel T., Bomans P., Naesens R., Mertes H., Dits H., Van Regenmortel N. COVID-19-associated invasive pulmonary aspergillosis. Ann. Intensive Care. 2020;10:71. doi: 10.1186/s13613-020-00686-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Albasata H., Alamri M.M., Almuhaidb S.A., Aljebreen A.M., Almaghrabia R.S. Case Report: Diagnostic challenge of COVID-19 associated pulmonary aspergillosis (CAPA) F1000Research. 2021;10:59. doi: 10.12688/f1000research.28424.2. [DOI] [Google Scholar]
- 52.Alanio A., Dellière S., Fodil S., Bretagne S., Mégarbane B. Prevalence of putative invasive pulmonary aspergillosis in critically ill patients with COVID-19. Lancet Respir. Med. 2020;8:e48–e49. doi: 10.1016/S2213-2600(20)30237-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Van Arkel A.L.E., Rijpstra T.A., Belderbos H.N.A., van Wijngaarden P., Verweij P.E., Bentvelsen R.G. COVID-19-associated pulmonary aspergillosis. Am. J. Respir. Crit. Care Med. 2020;202:132–135. doi: 10.1164/rccm.202004-1038LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sharma A., Hofmeyr A., Bansal A., Thakkar D., Lam L., Harrington Z., Bhonagiri D. COVID-19 associated pulmonary aspergillosis (CAPA): An Australian case report. Med. Mycol. Case Rep. 2021;31:6–10. doi: 10.1016/j.mmcr.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Santana M.F., Pivoto G., Alexandre M.A.A., Baía-Da-silva D.C., Borba M.G.d.S., Val F.A., Brito-Sousa J.D., Melo G.C., Monteiro W.M., Souza J.V.B., et al. Confirmed invasive pulmonary aspergillosis and COVID-19: The value of postmortem findings to support antemortem management. Rev. Soc. Bras. Med. Trop. 2020;53:1–4. doi: 10.1590/0037-8682-0401-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mohamed A., Hassan T., Trzos-Grzybowska M., Thomas J., Quinn A., O’Sullivan M., Griffin A., Rogers T.R., Talento A.F. Multi-triazole-resistant Aspergillus fumigatus and SARS-CoV-2 co-infection: A lethal combination. Med. Mycol. Case Rep. 2021;31:11–14. doi: 10.1016/j.mmcr.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mastrangelo A., Germinario B.N., Ferrante M., Frangi C., Li Voti R., Muccini C., Ripa M., Canetti D., Castiglioni B., Oltolini C., et al. Candidemia in Coronavirus Disease 2019 (COVID-19) Patients: Incidence and Characteristics in a Prospective Cohort Compared With Historical Non–COVID-19 Controls. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kuehn B.M. Drug-Resistant Yeast Infections Spread in COVID-19 Unit. JAMA. 2021;325:714. doi: 10.1001/jama.2021.1031. [DOI] [PubMed] [Google Scholar]
- 59.Posteraro B., Torelli R., Vella A., Leone P.M., De Angelis G., De Carolis E., Ventura G., Sanguinetti M., Fantoni M. Pan-echinocandin-resistant Candida glabrata bloodstream infection complicating COVID-19: A fatal case report. J. Fungi. 2020;6:163. doi: 10.3390/jof6030163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Konopka J.B., Casadevall A., Taylor J.W., Heitman J., Cowen L. One Health: Fungal Pathogens of Humans, Animals, and Plants. American Society for Microbiology; Washington, DC, USA: 2019. [PubMed] [Google Scholar]
- 61.Fisher M.C., Hawkins N.J., Sanglard D., Gurr S.J. Worldwide emergence of resistance to antifungal drugs challenges human health and food security. Science. 2018;360:739–742. doi: 10.1126/science.aap7999. [DOI] [PubMed] [Google Scholar]
- 62.Morales-López S.E., Parra-Giraldo C.M., Ceballos-Garzón A., Martínez H.P., Rodríguez G.J., Álvarez-Moreno C.A., Rodríguez J.Y. Invasive infections with multidrug-resistant yeast Candida auris, Colombia. Emerg. Infect. Dis. 2017;23:162–164. doi: 10.3201/eid2301.161497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Forsberg K., Woodworth K., Walters M., Berkow E.L., Jackson B., Chiller T., Vallabhaneni S. Candida auris: The recent emergence of a multidrug-resistant fungal pathogen. Med. Mycol. 2019;57:1–12. doi: 10.1093/mmy/myy054. [DOI] [PubMed] [Google Scholar]
- 64.Ademe M., Girma F. Candida auris: From multidrug resistance to pan-resistant strains. Infect. Drug Resist. 2020;13:1287–1294. doi: 10.2147/IDR.S249864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Suarez-de-la-Rica A., Serrano P., de-la-Oliva R., Sánchez-Díaz P., Molinero P., Falces-Romero I., Ferrando C., Rello J., Maseda E. Secondary infections in mechanically ventilated patients with COVID-19: An overlooked matter? Rev. Esp. Quimioter. 2021 doi: 10.37201/req/031.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Biswas S. Mucormycosis: The “Black Fungus” Maiming Covid Patients in India. [(accessed on 9 May 2021)]; Available online: https://www.bbc.com/news/world-asia-india-57027829.
- 67.At Least 8 Covid Survivours Die of Black Fungus “Mucormycosis” in Maharashtra. [(accessed on 9 May 2021)]; Available online: https://theprint.in/health/at-least-8-covid-survivors-die-of-black-fungus-mucormycosis-in-maharashtra/654924/
- 68.Sen M., Lahane S., Lahane T.P., Parekh R., Honavar S.G. Mucor in a Viral Land: A Tale of Two Pathogens. Indian J. Ophthalmol. 2021;69:244–252. doi: 10.4103/ijo.IJO_3774_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sharma S., Grover M., Bhargava S., Samdani S., Kataria T. Post coronavirus disease mucormycosis: A deadly addition to the pandemic spectrum. J. Laryngol. Otol. 2021;135:442–447. doi: 10.1017/S0022215121000992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chikley A., Ben-Ami R., Kontoyiannis D.P. Mucormycosis of the central nervous system. J. Fungi. 2019;5:59. doi: 10.3390/jof5030059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dusart A., Duprez T., Van Snick S., Godfraind C., Sindic C. Fatal rhinocerebral mucormycosis with intracavernous carotid aneurysm and thrombosis: A late complication of transsphenoidal surgery? Acta Neurol. Belg. 2013;113:179–184. doi: 10.1007/s13760-012-0151-9. [DOI] [PubMed] [Google Scholar]
- 72.Sarkar S., Gokhale T., Choudhury S., Deb A. COVID-19 and orbital mucormycosis. Indian J. Ophthalmol. 2021;69:1002–1004. doi: 10.4103/ijo.IJO_3763_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Prakash H., Chakrabarti A. Epidemiology of mucormycosis in India. Microorganisms. 2021;9:523. doi: 10.3390/microorganisms9030523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zurl C., Hoenigl M., Schulz E., Hatzl S., Gorkiewicz G., Krause R., Eller P., Prattes J. Autopsy proven pulmonary mucormycosis due to Rhizopus microsporus in a critically Ill COVID-19 patient with underlying hematological malignancy. J. Fungi. 2021;7:88. doi: 10.3390/jof7020088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.CDC (Centers for Disease Control and Prevention) Mucormycosis. [(accessed on 11 May 2021)]; Available online: https://www.cdc.gov/fungal/diseases/mucormycosis/index.html.
- 76.Singh A.K., Singh R., Joshi S.R., Misra A. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab. Syndr. Clin. Res. Rev. 2021 doi: 10.1016/j.dsx.2021.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mulakavalupil B., Vaity C., Joshi S., Misra A., Pandit R.A. Absence of Case of Mucormycosis (March 2020–May 2021) under strict protocol driven management care in a COVID-19 specific tertiary care intensive care unit. Diabetes Metab. Syndr. Clin. Res. Rev. 2021 doi: 10.1016/j.dsx.2021.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Garg D., Muthu V., Sehgal I.S., Ramachandran R., Kaur H., Bhalla A., Puri G.D., Chakrabarti A., Agarwal R. Coronavirus Disease (Covid-19) Associated Mucormycosis (CAM): Case Report and Systematic Review of Literature. Mycopathologia. 2021;186:289–298. doi: 10.1007/s11046-021-00528-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cultrera R., Barozzi A., Libanore M., Marangoni E., Pora R., Quarta B., Spadaro S., Ragazzi R., Marra A., Segala D., et al. Co-infections in critically ill patients with or without covid-19: A comparison of clinical microbial culture findings. Int. J. Environ. Res. Public Health. 2021;18:4358. doi: 10.3390/ijerph18084358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Arastehfar A., Carvalho A., van de Veerdonk F.L., Jenks J.D., Koehler P., Krause R., Cornely O.A., Perlin D.S., Lass-Flörl C., Hoenigl M. COVID-19 associated pulmonary aspergillosis (CAPA)—From immunology to treatment. J. Fungi. 2020;6:91. doi: 10.3390/jof6020091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Arastehfar A., Carvalho A., Hong Nguyen M., Hedayati M.T., Netea M.G., Perlin D.S., Hoenigl M. Covid-19-associated candidiasis (Cac): An underestimated complication in the absence of immunological predispositions? J. Fungi. 2020;6:211. doi: 10.3390/jof6040211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Riche C.V.W., Cassol R., Pasqualotto A.C. Is the frequency of candidemia increasing in covid-19 patients receiving corticosteroids? J. Fungi. 2020;6:286. doi: 10.3390/jof6040286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Koehler P., Bassetti M., Chakrabarti A., Chen S.C.A., Colombo A.L., Hoenigl M., Klimko N., Lass-Flörl C., Oladele R.O., Vinh D.C., et al. Defining and managing COVID-19-associated pulmonary aspergillosis: The 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect. Dis. 2021;3099 doi: 10.1016/S1473-3099(20)30847-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Verweij P.E., Rijnders B.J.A., Brüggemann R.J.M., Azoulay E., Bassetti M., Blot S., Calandra T., Clancy C.J., Cornely O.A., Chiller T., et al. Review of influenza-associated pulmonary aspergillosis in ICU patients and proposal for a case definition: An expert opinion. Intensive Care Med. 2020;46:1524–1535. doi: 10.1007/s00134-020-06091-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tolle L.B., Standiford T.J. Danger-associated molecular patterns (DAMPs) in acute lung injury. J. Pathol. 2013;229:145–156. doi: 10.1002/path.4124. [DOI] [PubMed] [Google Scholar]
- 86.Singh G., Pitoyo C.W., Aditianingsih D., Rumende C.M. Risk factors for early invasive fungal disease in critically ill patients. Indian J. Crit. Care Med. 2016;20:633–639. doi: 10.4103/0972-5229.194007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chakraborti A., Jaiswal A., Verma P., Singhal R. A prospective study of fungal colonization and invasive fungal disease in long-term mechanically ventilated patients in a respiratory intensive care unit. Indian J. Crit. Care Med. 2018;22:597–601. doi: 10.4103/ijccm.IJCCM_181_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dellière S., Dudoignon E., Fodil S., Voicu S., Collet M., Oillic P.A., Salmona M., Dépret F., Ghelfenstein-Ferreira T., Plaud B., et al. Risk factors associated with COVID-19-associated pulmonary aspergillosis in ICU patients: A French multicentric retrospective cohort. Clin. Microbiol. Infect. 2021;27 doi: 10.1016/j.cmi.2020.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Venditto V.J., Haydar D., Abdel-Latif A., Gensel J.C., Anstead M.I., Pitts M.G., Creameans J., Kopper T.J., Peng C., Feola D.J. Immunomodulatory Effects of Azithromycin Revisited: Potential Applications to COVID-19. Front. Immunol. 2021;12:574425. doi: 10.3389/fimmu.2021.574425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.NIH (National Institute of Health) COVID-19 Treatment Guidelines. [(accessed on 11 May 2021)]; Available online: https://www.covid19treatmentguidelines.nih.gov/whats-new/
- 91.Ye Q., Wang B., Mao J. The pathogenesis and treatment of the “Cytokine Storm” in COVID-19. J. Infect. 2020;80:607–613. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hu B., Huang S., Yin L. The cytokine storm and COVID-19. J. Med. Virol. 2021;93:250–256. doi: 10.1002/jmv.26232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fajgenbaum D.C., June C.H. Cytokine Storm. N. Engl. J. Med. 2020;383:2255–2273. doi: 10.1056/NEJMra2026131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.The RECOVERY Collaborative Group Dexamethasone in Hospitalized Patients with Covid-19. N. Engl. J. Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lewis R.E., Kontoyiannis D.P. Invasive aspergillosis in glucocorticoid-treated patients. Med. Mycol. 2009;47:271–281. doi: 10.1080/13693780802227159. [DOI] [PubMed] [Google Scholar]
- 96.Lionakis M.S., Kontoyiannis D.P. Glucocorticoids and invasive fungal infections. Lancet. 2003;362:1828–1838. doi: 10.1016/S0140-6736(03)14904-5. [DOI] [PubMed] [Google Scholar]
- 97.Coutinho A.E., Chapman K.E. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol. Cell. Endocrinol. 2011;335:2–13. doi: 10.1016/j.mce.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Oppong E., Cato A.C.B. Effects of glucocorticoids in the immune system. Adv. Exp. Med. Biol. 2015;872:217–233. doi: 10.1007/978-1-4939-2895-8_9. [DOI] [PubMed] [Google Scholar]
- 99.Armstrong-James D., Youngs J., Bicanic T., Abdolrasouli A., Denning D.W., Johnson E., Mehra V., Pagliuca T., Patel B., Rhodes J., et al. Confronting and mitigating the risk of COVID-19 associated pulmonary aspergillosis. Eur. Respir. J. 2020;56 doi: 10.1183/13993003.02554-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Donnelly J.P., Chen S.C., Kauffman C.A., Steinbach W.J., Baddley J.W., Verweij P.E., Clancy C.J., Wingard J.R., Lockhart S.R., Groll A.H., et al. Revision and update of the consensus definitions of invasive fungal disease from the European organization for research and treatment of cancer and the mycoses study group education and research consortium. Clin. Infect. Dis. 2020;71:1367–1376. doi: 10.1093/cid/ciz1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nasir N., Rehman F., Omair S.F. Risk factors for bacterial infections in patients with moderate to severe COVID-19: A case-control study. J. Med. Virol. 2021 doi: 10.1002/jmv.27000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Gupta S., Wang W., Hayek S.S., Chan L., Mathews K.S., Melamed M.L., Brenner S.K., Leonberg-Yoo A., Schenck E.J., Radbel J., et al. Association between Early Treatment with Tocilizumab and Mortality among Critically Ill Patients with COVID-19. JAMA Intern. Med. 2021;181:41–51. doi: 10.1001/jamainternmed.2020.6252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kimmig L.M., Wu D., Gold M., Pettit N.N., Pitrak D., Mueller J., Husain A.N., Mutlu E.A., Mutlu G.M. IL-6 Inhibition in Critically Ill COVID-19 Patients Is Associated with Increased Secondary Infections. Front. Med. 2020;7 doi: 10.3389/fmed.2020.583897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ho K.S., Narasimhan B., Difabrizio L., Rogers L., Bose S., Li L., Chen R., Sheehan J., El-Halabi M.A., Sarosky K., et al. Impact of corticosteroids in hospitalised COVID-19 patients. BMJ Open Respir. Res. 2021;8:1–8. doi: 10.1136/bmjresp-2020-000766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Machado M., Valerio M., Álvarez-Uría A., Olmedo M., Veintimilla C., Padilla B., De la Villa S., Guinea J., Escribano P., Ruiz-Serrano M.J., et al. Invasive pulmonary aspergillosis in the COVID-19 era: An expected new entity. Mycoses. 2021;64:132–143. doi: 10.1111/myc.13213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Deana C., Vetrugno L., Bassi F., De Monte A. Tocilizumab administration in COVID-19 patients: Water on the fire or gasoline? Med. Mycol. Case Rep. 2021;31:32–34. doi: 10.1016/j.mmcr.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Fekkar A., Lampros A., Mayaux J., Poignon C., Demeret S., Constantin J.-M., Marcelin A.-G.E., Monsel A., Luyt C.-E., Blaize M. Occurrence of Invasive Pulmonary Fungal Infections in Patients with Severe COVID-19 Admitted to the ICU. Am. J. Respir. Crit. Care Med. 2021;203:307–317. doi: 10.1164/rccm.202009-3400OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Meira F., Moreno-García E., Linares L., Macaya I., Tomé A., Hernández-Meneses M., Albiach L., Morata L., Letona L., Bodro M., et al. Impact of Inflammatory Response Modifiers on the Incidence of Hospital-Acquired Infections in Patients with COVID-19. Infect. Dis. Ther. 2021 doi: 10.1007/s40121-021-00477-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Antinori S., Milazzo L., Sollima S., Galli M., Corbellino M. Candidemia and invasive candidiasis in adults: A narrative review. Eur. J. Intern. Med. 2016;34:21–28. doi: 10.1016/j.ejim.2016.06.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Supporting data for Figure 1 is in the supplementary information.