Abstract
Delivering healthcare to people living with Parkinson’s disease (PD) may be challenging in face of differentiated care needs during a PD journey and a growing complexity. In this regard, integrative care models may foster flexible solutions on patients’ care needs whereas Parkinson Nurses (PN) may be pivotal facilitators. However, at present hardly any training opportunities tailored to the care priorities of PD-patients are to be found for nurses. Following a conceptual approach, this article aims at setting a framework for training PN by reviewing existing literature on care priorities for PD. As a result, six prerequisites were formulated concerning a framework for training PN. The proposed training framework consist of three modules covering topics of PD: (i) comprehensive care, (ii) self-management support and (iii) health coaching. A fourth module on telemedicine may be added if applicable. The framework streamlines important theoretical concepts of professional PD management and may enable the development of novel, personalized care approaches.
Keywords: Parkinson’s disease, nursing training, integrated care, Parkinson nurse, personalized care, multidisciplinary care
1. Introduction
Parkinson’s disease (PD) is a progressive non-curable neurodegenerative disorder with an age of onset usually over 60 and presenting with complex motor and non-motor features such as cognitive impairment, mood and sleep disorders, autonomic dysfunction, and pain. In Europe, 1.2 million people are living with PD [1] with an increasing incidence in the elderly, so that the number of affected patients worldwide is expected to double by 2030 [2]. PD ranges among the top ten most resource intensive brain disorders in Europe [1] so that the need for PD services is expected to build up and consequently the burden on healthcare systems. This reality warrants the development and implementation of a care delivery model that conforms with society resources to guarantee its sustainability, while promoting better public policies, and reducing the overwhelming societal impact of PD [3]. The complexity of PD implies specific requirements for the design and delivery of care. Nevertheless, to date personalized care delivery models are rare [4]. While it has been shown that integrated and multidisciplinary care delivery models following a personalized care approach have positive implications for persons living with PD (PwPs), care partner and care providers, their implementation is difficult due to several reasons [3,4,5]. A key aspect for personalizing care services, is the availability of specialized staff [3]. Among these healthcare professionals, Parkinson Nurses (PN) can accomplish important tasks in the care process, such as providing mental health support, monitoring symptom progression and promoting patient navigation through the local healthcare system [3,6,7]. There has not been a consensus on defining the PN, but following Parkinsons UK, a PN can “…provide expert care because they only work with people with the condition.” They describe the major role of a PN in providing care as whilst “…helping people to manage their medication” [8], the provided care by a PN will result in less side effects. Generally, PN help patients to manage their illness through making, for example by giving information and support to people with Parkinson’s.
However, there are various definitions and descriptions not only of the role in the care team but there are also multiple approaches on the training of PNs as highlighted in Table 1.
Table 1.
Existing Training Opportunities for Parkinson Nurses in different Countries.
| Country | Role | Formal Education | Reference |
|---|---|---|---|
| United Kingdom | Being responsible for overall management within primary or secondary care teams Resource of Information and advice for PwPs Catalyst for improving public awareness |
Provided via national universities Prerequisite:
|
[8,9] |
| Germany | Providing information and advice to patients and care givers on medication, symptoms and treatment options | Provided via German Parkinson Society (DPG), German Parkinson Association, (dPV), Parkinson Competence Network (KNP), Association of Parkinson Nurses and Assistants (VPNA) Prerequisite:
|
[7,10] |
| United States 1 | Role of APN (generally)
|
Advanced Practice Nurse (APN) → post-graduate education in nursing Two Types of APN roles have been recognized in the United States.
Prerequisite:
|
[11,12] |
| Canada 1 | Role of APN (generally)
|
Two types of APN roles have been recognized in Canada.
NP → Registered nurses; completed NP education program; Bachelor- or Master’s degree CNP → Master or Doctoral degree in nursing Topics covered during education for APNs:
|
[13,14,15,16] |
1 In the United States and Canada, a variety of different forms of nurse education exist, and the nomenclature also holds a wide range of designations in both countries. The role and education of APNs (Advanced Practice Nurses) will be discussed here as an example. An explicit training as an advanced practice nurse for Parkinson’s disease is not currently available in the United States and Canada.
Even though specialized training for PN on the delivery of personalized care services has been recommended [17], no framework has been proposed yet and existing curricular do not explicitly in cooperate it. By reviewing the specific requirements for the design and delivery of care in PD, we aim to propose a training framework for PN to facilitate the personalization and integration of care delivery.
2. Materials and Methods
We adopted a conceptual research approach to synthesize different perspectives on the theme of PD care and role of nurses. [18]. We entertained various conceptual streams from health care design, care delivery and medical prerequisites of PD. We considered the following questions to be essential to PN training: What are the care priorities for people living with PD (PwPs)? What type of PD-specific skills should a PN be equipped with in order to meet these needs?
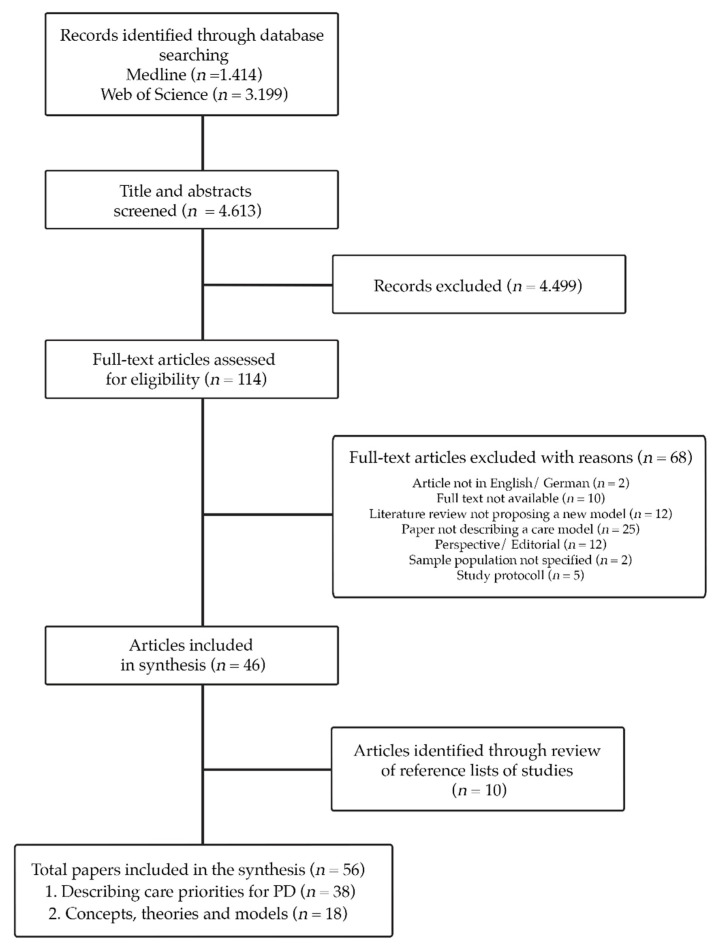
The conceptualization of a training framework, may thus be seen a synthesis from various theoretical concepts which address care priorities for PD. We followed the structure of a line of reasoning to model this novel concept [19]. In this approach different hypothesis are formulated which then are integrated into a proposed model [19]. Following Lynham’s Growth Cycle of Applied Theory-Building, the conceptualization of the training framework was informed by research, theory and practice [20]. A scoping literature review was conducted in order to identify relevant literature on care for PD. We chose The methodological approach of a scoping review, as it has been recommended to be particularly useful for categorizing the existing scientific literature in a defined research area in terms of its type, characteristics, and scope [21].The literature review was conducted in March 2020, (with an update in April 2021) by searching MEDLINE and Web of Knowledge (Figure 1), using the terms Parkinson’s disease, concept and care. The search was not restricted in terms of the publication year. Studies were included if they described or theorized care models or concepts, relevant to PD and were either published in English or German. If a paper referred to another theory which was not focusing on PD but still relevant for the research aim (developing a PN training framework), the paper and theory reported also included. Opinion papers, literature reviews not proposing a new care model or studies testing short term interventions (i.e., physical therapy) were excluded. Publications focusing on palliative care were excluded, because this was seen as a different topic, where PwPs and care partners develop unique needs and concepts become relevant, which distinguish from other PD care literature. The search strategies, as well as a detailed list of in- and exclusion criteria can be accessed in the Supplementary Material (Table S1).
Figure 1.
PRISMA flow diagram for the conducted scoping review.
As a first step, publications retrieved from the literature review were grouped into 3 categories: intervention, practical care concept or theoretical concepts. Next, practical care concepts, guidelines and interventions were reviewed to identify care priorities for PD. Consecutively, a code was invented, whenever a new guiding care principle was mentioned following the approach of an undirected content analysis [22]. Thirdly, the identified care priorities informed the formulation of two hypothesis regarding a PN training framework. Fourth, the content of theoretical concepts was analyzed according to the previously identified care priorities. Finally, the content was used to construct a line of reasoning and to propose a framework for training PN. The literature research and coding, following the guidelines of PRISMA-ScR [23], was independently performed by two researchers (M.vM; J.S.). Discrepancies in coding and grouping were solved via discussion with a third researcher (F.T.). The final framework was commented by a range of PD experts for the iCARE-PD consortium (http://icare-pd.ca/, 1 June 2021), including PN, neurologists and scientists.
3. Results
Fifty-six publications were included for final synthesis. (Figure 1).
The analysis included nine interventions implementing and evaluating a care model for PD, two guidelines for organizing PD care, 29 publications describing an implemented care model and 18 conceptual papers. Few publications described the same practical care model [24,25,26,27] whereas two reported the same care concept [28,29]. Consequently, 35 publications informed the definition of care priorities for PD care and 18 models informed the conceptualization of a PN training framework. Based on the implemented care models and recommendations, nine priorities for the organization and delivery of PD care were identified. The priorities and the frequency with which they were mentioned are summarized in Table 2.
Table 2.
Care Priorities for Parkinson’s Disease in Practical Care Concepts.
| Care Priority | Citation (Frequency) |
Reference |
|---|---|---|
| Multidisciplinary care | 24 | [19,24,25,26,27,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] |
| Patient-centeredness | 17 | [24,25,26,27,32,36,39,40,41,42,43,44,45,47,48,52,53,54,55,56] |
| Integrated care | 16 | [3,24,25,26,27,31,32,36,38,40,42,44,45,46,48,51,52,56,57] |
| Home-based care | 13 | [36,37,40,41,42,44,51,53,56,57,58,59,60] |
| Self-management | 11 | [24,25,26,27,36,39,40,44,45,55,57,61,62] |
| Community-centered care | 9 | [24,25,26,27,30,41,45,52,53,59,60,63] |
| Patient-/care partner education | 7 | [36,39,40,42,44,51,55] |
| Telemedicine | 7 | [30,42,44,56,57,58,59] |
| Professional education | 1 | [55] |
The conceptual models covered the same care priorities as the practical care concepts. In addition to these priorities, the priority personalized care was observable in the conceptual models. The priorities and the frequency with which they were mentioned are summarized in Table 3. A content summary of the included models can be found in the Supplementary Material (Table S2).
Table 3.
Care Priorities for Parkinson’s Disease in Conceptual Models.
| Care Priority | Citation (Frequency) | Reference |
|---|---|---|
| Patient-centeredness | 9 | [64,65,66,67,68,69,70,71,72] |
| Integrated care | 8 | [66,68,69,73,74,75,76,77] |
| Multidisciplinary care | 6 | [64,66,68,74,76,78] |
| Community-centered care | 6 | [67,68,69,71,77,78] |
| Home-based care | 5 | [28,29,65,68,73,79] |
| Personalized care | 4 | [70,75,78,80] |
| Self-management | 4 | [65,70,73,77] |
| Patient-/care partner education | 2 | [75,80] |
| Telemedicine | 1 | [28,29] |
| Professional education | 1 | [65] |
Based on the identified care priorities for PD patients and their conceptualization in various care models, we present two hypotheses on the training requirements for PN, followed by relevant question(s) related to each hypothesis and their implication to the development of a PN training framework.
Hypothesis 1 (H1).
Parkinson Nurses should be trained to deliver comprehensive care for people living with parkinson’s Disease and their care partner.
Given the heterogeneous and progressive nature of PD, treatments require a high degree of personalization, as this enables the adjustment of the multiple existing management options to the clinical presentation, the individual symptoms and their progression, and the care needs of PwPs [81]. Based on the analyzed concepts of PD care, two models described personalized care management as important aspect [70,75] whereas two other models included the provision of tailored information [69,80].
What is personalized care? Personalizing care means adapting the care process to the patients’ needs and preferences [78] (813) (p.813). Van Halteren et al. described five essential aspects of personalized care: providing information, proactively monitoring early detection signs and symptoms and the care process, coordinating care and navigating the patient in the healthcare system [78].
Implications for a PN curriculum: In reference to the conceptualization of a training framework, a PN ought to be competent to identify care needs and preferences for each individual. Additionally, they must be able to decide their implications for the care plan.
Personalizing care approaches means, that patients’ perspective plays a central role in decision-making processes and leads to another frequently mentioned care priority: patient-centered care. Two models incorporated patient-centeredness as a pivotal aspect for care delivery [66,70] and three models highlighted the patients perspective as central component [65,68,71].
What is patient-centered care? Implementing a patient-centered perspective means ‘[…] ensuring that patient values guide all clinical decisions.’ ([69], p. 360). Good communication is needed in order to identify these values [64,67]. PN must be able to meet patients and care partner with respect and empathy [64,67,69,72]. Providing emotional support and creating a trustful relationship has been mentioned as important element for implementing patient-centered care across all three identified concepts [67,69].
Implications for a PN curriculum: In reference to the conceptualization of a training framework, a PN ought to be trained in communicating with PwPs and care partner to enhance patient-centeredness.
What is integrated care? Integrated care is a form of multidisciplinary care. A multidisciplinary care approach can be described as an approach ‘[…] with contributions by experts from multiple complementary disciplines.’ [49] (p.167). Bringing together these professions is what Goodwin described as professional integration [74]. Other concepts referred to this by highlighting the importance of incorporating physicians’ perspectives in the care process; coordinating care across professions and implementing a clinical information system [64,68,77].
While there is a wide range of definitions, integrated care can be described as a care approach that aims ‘[…] bringing together key aspects in the design and delivery of care systems that are fragmented’ [74] (p 1) (p.1). Three conceptual models described components that an integrated care approach should consider [66,74,76]. The Rainbow defines four primary domains of integration: clinical, professional, organizational, and systems integration, whereby functional and normative enablers play a role [76]. The Development Model of Integrated Care (DMIC) presents a nine-cluster model for organizational development in four phases with an emphasis on actual co-operation and commitment [66]. The DMIC also focuses on conditions for achieving effective collaboration, such as patient engagement, clarity of roles and responsibilities within the care delivery team [66]. Goodwin’s work [74] distinguishes not only in the form in which integrated care should be designed (horizontal, vertical, sectoral, people-centered and whole-system), but also by how it is classified (by type, level, process, breadth and degree/intensity) [74].
An important aspect that was identifiable across the three integrated care concepts is care organization [66,74,76]. For PD, the inclusion of multiple healthcare professionals and the coordination of their care actions is of utmost importance [3]. Delivering integrated care has been described as central aspect for meeting PwPs complex care needs, reducing the burden of care partner and improving health care professional satisfaction [4].
Two of the conceptual models in integrated care services as important aspect for care delivery [73,75] and three models referred indirectly to the integration of care by mentioning a continuous collaboration of care providers, the organization of care and the selection of combined helping methods as important aspects of care organization [68,77].
Implications for a PN curriculum: PN fulfill important roles as clinical care integrators, navigators, support person and supervisor [4,75,82]. PNs, as part of the professional care team, should be able to design and implement a flexible routine network of service provider to support PwPs and their care partner in inpatient and outpatient settings.
What is home-based and community-centered care? Home-based care ‘[…] refers to clinical practices that provide physician- or nurse practitioner led, longitudinal interdisciplinary care […]’ at home ([79], p. 1). According to the Quality of Care Framework for Home-Based Medical Care [79], the essential elements are: assessment, care-coordination, patient and care partner education, provider competency, safety, provider competency and shared decision-making [79]. Additionally, factors such as patient and care partner experience, financial aspects and quality of life should be considered [79]. According to the model, patient-centered care can be promoted through the use of quality indicators that assess patients’ access to care services, as well as their satisfaction with the expertise of care providers [79]. From the reviewed conceptual models, two referred indirectly to the organization of home-based care by mentioning the support of autonomy as important aspect for organizing patient-centered care [55,56]. Three models highlighted the need to assess available community resources [58,68], one model referred to the importance of assessing the personal lifestyle [59], one model defined quality criteria for the implementation of home-based telemedicine [19,20] and five models mentioned the navigation of the patient towards these resources and the reduction of barriers as important aspect for the organization of care and the selection of combined support methods as important aspects of care organization [59,60,62,68,69].
Delivering community-centered care means bringing ‘[…] care directly to the patients in the local community setting […].’ ([30], p. 1). Consequently, knowledge about the community and available resources is required. Based on the literature review, no model exclusively focusing on community-centered care was identified, however several concepts included available community resources as important quality aspects of care [67,77] as further detailed above.
Delivering care at home and within the community is important for PwPs and their care partners in order to enable access to care [3,73,83]. Additionally, home-based care for PwPs is becoming increasingly important from a demographic (e.g., aging, immobile population) and social (e.g., patients having a pronounced desire to continue living in their own homes) point of view [68].
Implications for a PN curriculum: Based on the concepts of home-based and community-centered care, we propose that the quality of care provided by PN may be influenced by level of coordination skills of different stakeholders in the healthcare system and knowledge about local healthcare resources. Thus, PN should be trained to map available community resources and navigate PwPs towards them.
Hypothesis 2 (H2).
Parkinson Nurses should be trained to deliver self-management support to persons with Parkinson’s Disease and their care partner.
Self-management support (SMS) and patient-education are critical elements of effective PD management [4,84], and key component of integrated care. SMS is a top priority for PwPs when asked about their care requirements [85]. SMS and patient-education help to reduce disease progression, complications and costs [4,84,85].
What is patient and care partner education? Based on Graham’s concept, patient and care partner education are a form of knowledge translation [80]. The ability of lifelong learning is an important aspect of healthy aging and may be jeopardized by PD [70]. Implementing learning processes and empowering patients and care partner through education characterize integrated care concepts that were included in the analysis [66,69,75,77]. According to the Knowledge Translation Framework, patient education should be based on identified problems and adapted knowledge based on these problems. Patients and care partner should be motivated to use the delivered knowledge. Additionally, the identification of barriers and the use of knowledge should be evaluated continuously [80].
What is self-management support? Self-management support ‘[…] aims to empower patients with the skills and confidence necessary to manage their clinical disease.’ ([73], p. 25). Activities include patient education, monitoring changes in symptoms and abilities, goal setting, and problem-solving [73]. Based on Orem’s Self Deficit Theory, self-management support is needed, when the client’s self-care demand exceeds the available self-care agency [68]. From the literature review, four conceptual models were identified that included self-management support as important aspect of care [65,70,73,77]. The Glasgow model (or 5-A’s approach) describes five important actions that should be taken by the health-care professional when delivering SMS to the patient, namely: assessing, agreeing, advising, arranging and assisting. Another model, which is often referred to by SMS interventions for PwPs is the Chronic Care Model [77]. The model does not exclusively focus on SMS, but describes SMS as one of six dimensions, which should be addressed to improve care for patients with a chronic disease. According to the model, all dimensions affect each other, which is why all dimensions should be considered when aiming to improve care. The Chronic Disease Self-Management Model [77] is another model, which does not explicitly address PwPs but informed SMS approaches for PD [86]. Similar to the Glasgow model, it focuses on the relationship between the healthcare professional and the patient, however, a stronger focus is placed on the motivational aspect. According to the model, a good SMS-program pays attention to emotional and role management in addition to medical management and incorporates techniques to improve the patients’ confidence.
Implications for a PN curriculum: PN play an important role in delivering SMS to PwPs [4,87,88], as good SMS relies on support from educated health professionals [88]. PN have a have a close patient contact and thus, are ideal professionals for delivering SMS [88]. In order to advise and assist PwPs properly, an understanding of the disease and its complexity is required, making it an essential part of a PN training framework. Considering the Knowledge Translation Framework, we propose that a PN training should include aspects of motivational interviewing in order to facilitate knowledge use by PwPs and their care partners [89].
Finally, one of the identified theoretical concepts considered telemedicine [28,29]. Telemedical applications can improve PwPs access to care, enhance quality of life and reduce the burden of care partner [90]. However, their purpose can vary greatly [28], which is why we propose to add a fourth module to the PN training framework when applicable, specifically focusing on the available technology.
Proposing a Framework for Training Parkinson Nurses to Deliver a Personalized Care Approach
In the previous section, we have formulated two hypotheses: (1) PN should be trained to deliver comprehensive care for PwPs and their care partner and (2) PD Nurses should be trained to deliver self-management support to PwPs and their care partner. Based on the review of conceptual models, we identified the following requirements to a framework for training PN:
-
(1)
PN ought to be competent to identify needs and preferences. Additionally, they must be able to decide their implications for the care plan.
-
(2)
PN require training in communicating with PwPs and care partner.
-
(3)
PNs, as part of the professional care team, should be able to design and implement a flexible routine network of service providers to support PwPs and their care partner in inpatient and outpatient settings.
-
(4)
The quality of care provided by PN may be influenced by specific training in the coordination of different stakeholders in the health care system and knowledge about local healthcare resources. Thus, PN should be trained to map available community resources and navigate PwPs towards them.
-
(5)
In order to advise and assist PwPs properly, an understanding of the disease and its complexity is indispensable, making it an essential part of a PN training. Considering the Knowledge Translation Framework, we propose that a PN training should include aspects of motivational interviewing in order to facilitate knowledge use [89].
-
(6)
Education on telemedicine should be incorporated whenever possible and applicable.
-
(7)
Based on these requirements, we propose that PN should be trained in three central aspects in order to deliver a personalized care approach: i. understanding PD, ii. health coaching and iii. delivering comprehensive care. These aspects form the framework of the PN training displayed in Table 4.
Table 4.
Conceptual framework for training Parkinson-Nurses to deliver a personalized care approach.
| Module | Topic | Components | Goals |
|---|---|---|---|
| 1 | Understanding Parkinson’s disease |
|
Acquire fundamental knowledge about PD and management principles of motor and non-motor symptoms |
| 2 | Being a health coach |
|
Acquire skills and knowledge to assess patient-outcomes and identify personal care requirements |
| 3 | Aspects of care delivery for people living with Parkinson’s disease and care partner |
|
Acquire knowledge about available local care resources and methods to motivate patients and care partners to use them |
| 4 | Telemedicine |
|
Acquire knowledge about the technology |
Understanding the disease is a fundamental prerequisite for delivering care and, consequently, a foundational knowledge and skills for PN training [6,17,82]. PN must be able to adapt care delivery to the care requirements of PwPs and care partner, which change across the course of the disease. After completing the first module, PN are equipped with skills, that are important for integrating, personalizing and centering care around the patient. Besides a sound medical knowledge, PN must be able to understand and conduct clinical assessments [91]. These assessments may help the PN to evaluate patient needs as a starting point for discussion about care plans. Additionally, aspects of patient education and self-management support come into play when the PN discusses tests results or care plans with the patients. Consequently, we propose training on clinical assessments. And obtaining clinical conversation skills as central goal for the second training module: health coaching. Optimal care of PD should promote general health and wellbeing and care priorities should be defined together with PwPs and care partner [3]. Also, PwPs and care partner require a reference person that can be embodied by the PN through the empathic assessment of their care needs and the nurse’s role as a care coordinator [3]. After the completion of this second training module, PN will have acquired the skills to assess personal care requirements of PwPs. The understanding of PD and health coaching skills merge, in line with the care priorities of home-based and community centered care, into a third and last module: delivering comprehensive tailored care. PwPs and care partner have to be navigated throughout the local healthcare system; multiple professions have to be incorporated in the care process and PwPs and care partner need motivation to use these resources. Consequently, we propose that PN should be trained to identify relevant local resources for PwPs and care partner, understand their living situation and motivate them to utilize available resources. Finally, a fourth module regarding available technologies can be added if applicable. This module will be discussed in greater detail in the following section.
4. Discussion
This paper proposes a framework for a novel PN training in the context of integrated care. There is a scientific consensus that PNs will take a significant and prominent role in integrated, patient-centered home-/and community-based care in the future [92]. The PN is widely considered to be an important primary point of contact for PwPs and care partner alike. PNs are also recognized to be very helpful in the role of a multidisciplinary care team coordinator [93]. When PNs are available to provide home-based care, it has been shown that patients’ quality of life improves [54,94]. The importance of professional education can be identified in both theoretical and intervention-based models [55,65].
When it comes to educating PN, a variety of training pathways exist in the various countries. Also, the recognition of nurses as important care coordinators differs. As it has been stated elsewhere, funding mechanisms and the structure of healthcare systems play an important task for defining a nurse’s role [95]. This is also reflected in different education programs. Therefore, it is necessary to address country specific requirements when implementing the framework. Also, the structure of healthcare systems affects the availability of resources, which is why a sound understanding of the overall context is essential for implementing the framework presented here. We emphasize that module 3 of the framework should be adjusted to the country-specific context. Further research may aim to further defining this module and adapting it to a country-specific context. For countries with extensive training opportunities and high resources, such as the United States [95], we suggest, that single modules of the proposed training framework could be implemented in the basic training of nurses as prerequisite for a later specialization in the field. This would enable nurse students to better understand PD and prepare them to be empowered nursing advocates for PwPs in inpatient and outpatient settings. For countries, where the profession of PN is less well developed, such as Germany [7,95] the framework may be fully implemented and also be utilized to build an agenda for future research on how the role of PN can be strengthened.
When implementing the framework into pratice, one might face challenges and barriers. In some countries, the PN has been an integral part of the multidisciplinary care team for a long time [96], while in others PN are not present in every care team [7,17]. Also, it is necessary to clarify funding issues for implementing the framework and hire staff, such as experienced PN, to deliver the framework. Additionally the lack in certification of such training could be another barrier [7]. However, the framework introduced here may represent an crucial step towards a universal consensus on certification.
Concerning the fourth module, the framework is deliberately kept open. Telemedicine represents an increasingly studied and apparently beneficial instrument for the provision of medical care to the chronically ill [29,97,98]. However, telemedicine must always be evaluated in the context of its application, i.e., the technical prerequisites for widespread use must also be accessible to the individual patients [99]. Therefore, telemedicine is not yet part of this framework, but we strongly encourage its future integration. Due to the emerging possibility of remote patient monitoring (i.e., smart glasses, smart beds or wearables [83,100]), we emphasize future research on up-to-date tech-based home-based care solutions and the future role a PN may hold in this scenario of increasingly tech-based medical and social care delivery. This demand would also meet the need of care approaches to not only being responsive to specific care situations, but to incorporate proactive elements, such as the utilization of telemedicine [92,93].
For the future, the model being proposed here should configure a practical care concept that addresses effectively the identified care priorities for PD. One important aspect is the validation of the role of the PN and its training across cultures and societal contexts. Further research may focus on evaluating the implementation of the framework into a practical care concept and the development of a toolkit, which allows a flexible and streamlined adaptation of the training curriculum into different settings. Also, the model may be extended by reviewing care priorities for palliatve care.
5. Limitations
This review holds potential limitations. The quality of evidence, which was included in the review was not assessed, since the purpose was to review existing concepts as widely as possible. Further, the curriculum has not been implemented or evaluated in practice, which is why no claims about its feasibility can be made. Rather, it should be understood as stimulating and inspiring source of information for developing future PN curricula. Finally, the framework does not include country-specific differences of PN, which may affect its applicability.
6. Conclusions
A training framework for PN introduced here marks a pivotal contribution to increase the quality of care delivery for PwPs and their care partner following a care priority adapted approach. This framework is intended as an invitation to other researchers and practitioners to aid supporting the role of PNs and to move towards a standardized training. A shift towards a proactive role of a PN amongst healthcare providers is necessary and should be encouraged by legislation.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jpm11070623/s1, Table S1: Search Strategy and In- and Exclusion Criteria, Table S2: Overview of Theoretical Concepts.
Author Contributions
Conceptualization, M.v.M., J.S., F.T., D.C. and T.A.M.; methodology, M.v.M., J.S.; formal analysis, M.v.M. and J.S.; investigation, M.v.M. and J.S.; resources, M.v.M., J.S., F.T. and T.A.M.; writing—original draft preparation, M.v.M., J.S.; writing—review and editing, F.T., D.J.P. and T.A.M.; visualization, M.v.M.; supervision, T.A.M.; funding acquisition, T.A.M., D.C., D.J.P., A.A., M.F., J.J.F., D.G., E.R. contributed with professional expertise and provided critical revisions of the intellectual content. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Canadian Institutes of Health Research/EU Joint Programme—Neurodegenerative Disease Research, grant number 01789-000/HESOCARE-329-073.
Conflicts of Interest
M.v.M. declares no C.o.I. J.S. declares no C.o.I. F.T. declares no C.o.I. D.P. declares no C.o.I. A.A. has received compensation for consultancy and speaker related activities from UCB, Boehringer Ingelheim, General Electric, Britannia, AbbVie, Kyowa Kirin, Zambon, Bial, Neuroderm, Theravance Biopharma, Roche, Medscape; he receives research support from Bial, Lundbeck, Roche, Angelini Pharmaceuticals, Horizon 2020—Grant 825785, Horizon2020 Grant 101016902, Ministry of Education University and Research (MIUR) Grant ARS01_01081, Cariparo Foundation. He serves as consultant for Boehringer–Ingelheim for legal cases on pathological gambling. D.C. declares no C.o.I. M.F. declares no C.o.I. J.J.F. has held consultancy functions with GlaxoSmithKline, Novartis, TEVA, Lundbeck, Solvay, Abbott, Abbvie, BIAL, Merck-Serono, Merz, Ipsen, Biogen, NeuroDerm, Zambon, Sunovion, Affiris, ONO; has received lecture fees from Biogen, BIAL, Sunovion, ONO, Zambon, Abbvie; has received grants from GlaxoSmithKline, Grunenthal, MSD, Allergan, Novartis, Fundação MSD (Portugal), Medtronic and Teva; has been employed by Faculdade de Medicina de Lisboa and CNS—Campus Neurológico. D.G. received honorarium for speaking and consulting from Sunovion, Paladin Labs Inc, Clinical trials funding from Canadian Institutes of Health Research, Genzyme Corporation/Sanofi Canada, Eli Lilly and Company and grants from Canadian Institutes of Health Research, Parkinson Canada, Brain Canada, Ontario Brain Institute, PSI Foundation, Parkinson Research Consortium, EU Joint Programme—Neurodegenerative Disease Research, uOBMRI E. R. has been employed by First Faculty of Medicine, Charles University and General University Hospital in Prague, Czechia; received research funding form Czech Health Research Council and Michael J Fox Foundation; has no other relationships that present a potential conflict of interest. T.M. has received personal compensation for serving as a Consultant for CHDI, Sunovion, Valeo Pharma, Roche, Biogen and nQ, received personal compensation serving on a Speakers Bureau for Abbvie, Valeo Pharma, and has received research support from the Canadian Institutes of Health Research, EU Joint Programme—Neurodegenerative Disease Research, the Ontario Research Fund, Michael J Fox Foundation, Parkinson Canada, uOBMRI/Parkinson Research Consortium, Parkinson Canada, Brain Canada, Ontario Brain Institute, and PSI Foundation.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gustavsson A., Svensson M., Jacobi F., Allgulander C., Alonso J., Beghi E., Dodel R., Ekman M., Faravelli C., Fratiglioni L., et al. Cost of disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011;21:718–779. doi: 10.1016/j.euroneuro.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Dorsey E.R., Constantinescu R., Thompson J.P., Biglan K.M., Holloway R.G., Kieburtz K., Marshall F.J., Ravina B.M., Schifitto G., Siderowf A., et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007;68:384–386. doi: 10.1212/01.wnl.0000247740.47667.03. [DOI] [PubMed] [Google Scholar]
- 3.Radder D.L.M., de Vries N.M., Riksen N.P., Diamond S.J., Gross D., Gold D.R., Heesakkers J., Henderson E., Hommel A.L.A.J., Lennaerts H.H., et al. Multidisciplinary care for people with Parkinson’s disease: The new kids on the block! Expert Rev. Neurother. 2019;19:145–157. doi: 10.1080/14737175.2019.1561285. [DOI] [PubMed] [Google Scholar]
- 4.Rajan R., Brennan L., Bloem B.R., Dahodwala N., Gardner J., Goldman J.G., Grimes D.A., Iansek R., Kovács N., McGinley J., et al. Integrated Care in Parkinson’s Disease: A Systematic Review and Meta-Analysis. Mov. Disord. 2020;35:1509–1531. doi: 10.1002/mds.28097. [DOI] [PubMed] [Google Scholar]
- 5.Van der Marck M.A., Munneke M., Mulleners W., Hoogerwaard E.M., Borm G.F., Overeem S., Bloem B.R. Integrated multidisciplinary care in Parkinson’s disease: A non-randomised, controlled trial (IMPACT) Lancet Neurol. 2013;12:947–956. doi: 10.1016/S1474-4422(13)70196-0. [DOI] [PubMed] [Google Scholar]
- 6.MacMahon D.G. Parkinson’s disease nurse specialists: An important role in disease management. Neurology. 1999;52.7(Suppl. 3):S21–S25. [PubMed] [Google Scholar]
- 7.Prell T., Siebecker F., Lorrain M., Tönges L., Warnecke T., Klucken J., Wellach I., Buhmann C., Wolz M., Lorenzl S., et al. Specialized Staff for the Care of People with Parkinson’s Disease in Germany: An Overview. J. Clin. Med. 2020;9:2581. doi: 10.3390/jcm9082581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parkinson’s U.K. A Competency Frame-Work for Nurses Working in Parkinson’s Disease Management. 3rd ed. Parkinson’s U.K.; London, UK: 2016. [Google Scholar]
- 9.Morgan E., Moran M. The Parkinson’s disease nurse specialist. In: Palyfer J., Hindle J.V., Lees A., editors. Parkinson’s Disease in the Older Patient. 2nd ed. CRC Press; London, UK: 2008. pp. 314–323. [Google Scholar]
- 10.Mai T. Stand und Entwicklung der Rolle als Parkinson Nurse in Deutschland—Eine Online-Befragung. Pflege. 2018;31:181–189. doi: 10.1024/1012-5302/a000617. [DOI] [PubMed] [Google Scholar]
- 11.Schober M., Lehwaldt D., Rogers M., Steinke M., Turale S., Pulcini J., Roussel J., Stewart D. Guidelines on Advanced Practice Nursing. International Council of Nurses; Geneva, Switzerland: 2020. [Google Scholar]
- 12.Bryant-Lukosius D., Spichiger E., Martin J., Stoll H., Kellerhals S.D., Fliedner M., Roussel J., de Geest S. Framework for evaluating the impact of advanced practice nursing roles. J. Nurs. Scholarsh. 2016;48:201–209. doi: 10.1111/jnu.12199. [DOI] [PubMed] [Google Scholar]
- 13.DiCenso A., Martin-Misener R., Bryant-Lukosius D., Bourgeault I., Kilpatrick K., Donald F., Kaasalainen S., Harbman P., Carter N., Kioke S., et al. Advanced practice nursing in Canada: Overview of a decision support synthesis. Nurs. Leadersh. 2010;23:15–34. doi: 10.12927/cjnl.2010.22267. [DOI] [PubMed] [Google Scholar]
- 14.Carter F.D., Harbman P., Kilpatrick K., Martin-Misener R., Sherifali D., Tranmer J., Valaitis R. Report on Advanced Practice Nursing (APN) in Canada; Proceedings of the Global Summit; Ottawa, ON, Canada. 28–29 July 2014; [(accessed on 14 May 2021)]. Available online: https://fhs.mcmaster.ca/ccapnr/documents/CanadianReportGlobalAPNSummit2014June12FINAL.pdf. [Google Scholar]
- 15.Bryant-Lukosius D., Carter N., Kilpatrick K., Martin-Misener R., Donald F., Kaasalainen S., Harbman P., Bourgeault I., DiCenso A. The clinical nurse specialist role in Canada. Nurs. Leadersh. 2010;23:140–166. doi: 10.12927/cjnl.2010.22273. [DOI] [PubMed] [Google Scholar]
- 16.Canadian Nurses Association . Advanced Practice Nursing. A Pan-Canadian Framework. Canadian Nurses Association; Ottawa, ON, Canada: 2019. [Google Scholar]
- 17.Lennaerts H., Groot M., Rood B., Gilissen K., Tulp H., van Wensen E., Munneke M., van Laar T., Bloem B.R. A Guideline for Parkinson’s Disease Nurse Specialists, with Recommendations for Clinical Practice. J. Parkinsons. Dis. 2017;7:749–754. doi: 10.3233/JPD-171195. [DOI] [PubMed] [Google Scholar]
- 18.Fawcett S.E., Waller M.A., Miller J.W., Schwieterman M.A., Hazen B.T., Overstreet R.E. A Trail Guide to Publishing Success: Tips on Writing Influential Conceptual, Qualitative, and Survey Research. J. Bus Logist. 2014;35:1–16. doi: 10.1111/jbl.12039. [DOI] [Google Scholar]
- 19.Jaakkola E. Designing conceptual articles: Four approaches. AMS Rev. 2020;10:18–26. doi: 10.1007/s13162-020-00161-0. [DOI] [Google Scholar]
- 20.Lynham S.A. The General Method of Theory-Building Research in Applied Disciplines. Adv. Dev. Hum. Resour. 2002;4:221–241. doi: 10.1177/1523422302043002. [DOI] [Google Scholar]
- 21.Khalil H., Peters M., Godfrey C.M., McInerney P., Soares C.B., Parker D. An Evidence-Based Approach to Scoping Reviews. Worldviews Evid. Based Nurs. 2016;13:118–123. doi: 10.1111/wvn.12144. [DOI] [PubMed] [Google Scholar]
- 22.Hsieh H.-F., Shannon S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 23.Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D.J., Horsley T., Weeks L., et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 24.Bloem B.R., Rompen L., De Vries N.M., Klink A., Munneke M., Jeurissen P. ParkinsonNet: A Low-Cost Health Care Innovation with A Systems Approach from The Netherlands. Health Aff. 2017;36:1987–1996. doi: 10.1377/hlthaff.2017.0832. [DOI] [PubMed] [Google Scholar]
- 25.Nijkrake M.J., Keus S.H.J., Overeem S., Oostendorp R.A.B., Vlieland T.P.V., Mulleners W., Hoogerwaard E.M., Bloem B.R., Munneke M. The ParkinsonNet concept: Development, implementation and initial experience. Mov. Disord. 2010;25:823–829. doi: 10.1002/mds.22813. [DOI] [PubMed] [Google Scholar]
- 26.Tosserams A., de Vries N.M., Bloem B.R., Nonnekes J. Multidisciplinary Care to Optimize Functional Mobility in Parkinson Disease. Clin. Geriatr. Med. 2020;36:159–172. doi: 10.1016/j.cger.2019.09.008. [DOI] [PubMed] [Google Scholar]
- 27.Van der Eijk M., Bloem B.R., Nijhuis F.A.P., Koetsenruijter J., Vrijhoef H.J.M., Munneke M., Wensing M., Faber M.J. Multidisciplinary Collaboration in Professional Networks for PD A Mixed-Method Analysis. J. Parkinsons. Dis. 2015;5:937–945. doi: 10.3233/JPD-150673. [DOI] [PubMed] [Google Scholar]
- 28.Larson D.N., Schneider R.B., Simuni T. A New Era: The Growth of Video-Based Visits for Remote Management of Persons with Parkinson’s Disease. J. Parkinsons. Dis. 2021 doi: 10.3233/JPD-202381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dorsey E.R., Okun M.S., Bloem B.R. Care, Convenience, Comfort, Confidentiality, and Contagion: The 5 C’s that Will Shape the Future of Telemedicine. J. Parkinsons. Dis. 2020;10:893–897. doi: 10.3233/JPD-202109. [DOI] [PubMed] [Google Scholar]
- 30.Aye Y.M., Liew S., Neo S.X., Li W., Ng H.-L., Chua S.-T., Zhou W.-T., Au W.-L., Tan E.-K., Tay K.-Y., et al. Patient-Centric Care for Parkinson’s Disease: From Hospital to the Community. Front. Neurol. 2020;11:502. doi: 10.3389/fneur.2020.00502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen E.V., Hagestuen R., González-Ramos G., Cohen H.W., Bassich C., Book E., Bradley K.P., Carter J.H., Di Minno M., Gardner J., et al. Interprofessional education increases knowledge, promotes team building, and changes practice in the care of Parkinson’s disease. Parkinsonism Relat. Disord. 2016;22:21–27. doi: 10.1016/j.parkreldis.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 32.Eggers C., Dano R., Schill J., Fink G.R., Timmermann L., Voltz R., Golla H., Lorenzl S. Access to End-of Life Parkinson’s Disease Patients Through Patient-Centered Integrated Healthcare. Front. Neurol. 2018;9:627. doi: 10.3389/fneur.2018.00627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fleisher J.E., Klostermann E.C., Hess S.P., Lee J., Myrick E., Chodosh J. Interdisciplinary palliative care for people with advanced Parkinson’s disease: A view from the home. Ann. Palliat. Med. 2020;9:S80–S89. doi: 10.21037/apm.2019.09.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fründt O., Mainka T., Schönwald B., Müller B., Dicusar P., Gerloff C., Buhmann C. The Hamburg Parkinson day-clinic: A new treatment concept at the border of in- and outpatient care. J. Neural. Transm. 2018;125:1461–1472. doi: 10.1007/s00702-018-1918-9. [DOI] [PubMed] [Google Scholar]
- 35.Giladi N., Manor Y., Hilel A., Gurevich T. Interdisciplinary teamwork for the treatment of people with Parkinson’s disease and their families. Curr. Neurol. Neurosci. Rep. 2014;14:493. doi: 10.1007/s11910-014-0493-1. [DOI] [PubMed] [Google Scholar]
- 36.Grimes D., Fitzpatrick M., Gordon J., Miyasaki J., Fon E.A., Schlossmacher M., Suchowersky O., Rajput A., Lafontaine A.L., Mestre T., et al. Canadian guideline for Parkinson disease. CMAJ. 2019;191:E989–E1004. doi: 10.1503/cmaj.181504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hack N., Akbar U., Monari E.H., Eilers A., Thompson-Avila A., Hwynn N.H., Sriram A., Haq I., Hardwick A., Malaty I.A., et al. Person-Centered Care in the Home Setting for Parkinson’s Disease: Operation House Call Quality of Care Pilot Study. Parkinsons. Dis. 2015;2015:639494. doi: 10.1155/2015/639494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Iansek R. Interdisciplinary rehabilitation in Parkinson’s disease. Adv. Neurol. 1999;80:555–559. [PubMed] [Google Scholar]
- 39.Jones B., Hopkins G., Wherry S.-A., Lueck C.J., Das C.P., Dugdale P. Evaluation of a Regional Australian Nurse-Led Parkinson’s Service Using the Context, Input, Process, and Product Evaluation Model. Clin. Nurse Spec. 2016;30:264–270. doi: 10.1097/NUR.0000000000000232. [DOI] [PubMed] [Google Scholar]
- 40.Kessler D., Hatch S., Alexander L., Grimes D., Côté D., Liddy C., Mestre T. The Integrated Parkinson’s disease Care Network (IPCN): Qualitative evaluation of a new approach to care for Parkinson’s disease. Patient Educ. Couns. 2021;104:136–142. doi: 10.1016/j.pec.2020.07.002. [DOI] [PubMed] [Google Scholar]
- 41.Keus S.H.J., Nijkrake M.J., Borm G.F., Kwakkel G., Roos R.A.C., Berendse H.W., Adang E.M., Overeem S., Bloem B.R., Munneke M. The ParkinsonNet trial: Design and baseline characteristics. Mov. Disord. 2010;25:830–837. doi: 10.1002/mds.22815. [DOI] [PubMed] [Google Scholar]
- 42.Loewenbrück K.F., Stein D.B., Amelung V.E., Bitterlich R., Brumme M., Falkenburger B., Fehre A., Feige T., Frank A., Gißke C., et al. Parkinson Network Eastern Saxony (PANOS): Reaching Consensus for a Regional Intersectoral Integrated Care Concept for Patients with Parkinson’s Disease in the Region of Eastern Saxony, Germany. J. Clin. Med. 2020;9:2906. doi: 10.3390/jcm9092906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Monticone M., Ambrosini E., Laurini A., Rocca B., Foti C. In-patient multidisciplinary rehabilitation for Parkinson’s disease: A randomized controlled trial. Mov. Disord. 2015;30:1050–1058. doi: 10.1002/mds.26256. [DOI] [PubMed] [Google Scholar]
- 44.Radder D.L.M., Nonnekes J., van Nimwegen M., Eggers C., Abbruzzese G., Alves G., Browner N., Chaudhuri K.R., Ebersbach G., Ferreira J.J., et al. Recommendations for the Organization of Multidisciplinary Clinical Care Teams in Parkinson’s Disease. J. Parkinsons. Dis. 2020;10:1087–1098. doi: 10.3233/JPD-202078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rompen L., De Vries N.M., Munneke M., Neff C., Sachs T., Cedrone S., Cheves J., Bloem B.R. Introduction of Network-Based Healthcare at Kaiser Permanente. J. Parkinsons. Dis. 2020;10:207–212. doi: 10.3233/JPD-191620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shrubsole K. Implementation of an integrated multidisciplinary Movement Disorders Clinic: Applying a knowledge translation framework to improve multidisciplinary care. Disabil. Rehabil. 2019:1–13. doi: 10.1080/09638288.2019.1691666. [DOI] [PubMed] [Google Scholar]
- 47.Taylor J., Anderson W.S., Brandt J., Mari Z., Pontone G.M. Neuropsychiatric Complications of Parkinson Disease Treatments: Importance of Multidisciplinary Care. Am. J. Geriatr. Psychiatry. 2016;24:1171–1180. doi: 10.1016/j.jagp.2016.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tönges L., Ehret R., Lorrain M., Riederer P., Müngersdorf M. Epidemiology of Parkinson’s Disease and Current Concepts of Outpatient Care in Germany. Fortschr. Neurol. Psychiatr. 2017;85:329–335. doi: 10.1055/s-0043-103275. [DOI] [PubMed] [Google Scholar]
- 49.Van der Marck M.A., Bloem B.R. How to organize multispecialty care for patients with Parkinson’s disease. Parkinsonism Relat. Disord. 2014;20:S167–S173. doi: 10.1016/S1353-8020(13)70040-3. [DOI] [PubMed] [Google Scholar]
- 50.Vaughan C.P., Prizer L.P., Vandenberg A.E., Goldstein F.C., Trotti L.M., Hermida A.P., Factor S.A. A Comprehensive Approach to Care in Parkinson’s Disease Adds Quality to the Current Gold Standard. Mov. Disord. Clin. Pract. 2017;4:743–749. doi: 10.1002/mdc3.12508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vickers L.F., O’Neill C.M. An interdisciplinary home healthcare program for patients with Parkinson’s disease. Rehabil. Nurs. 1998;23:286–289. doi: 10.1002/j.2048-7940.1998.tb01806.x. [DOI] [PubMed] [Google Scholar]
- 52.Albanese A., Di Fonzo A., Fetoni V., Franzini A., Gennuso M., Molini G., Pacchetti C., Priori A., Riboldazzi G., Volonté M.A., et al. Design and Operation of the Lombardy Parkinson’s Disease Network. Front. Neurol. 2020;11:573. doi: 10.3389/fneur.2020.00573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Connor K.I., Cheng E.M., Barry F., Siebens H.C., Lee M.L., Ganz D.A., Mittman B.S., Connor M.K., Edwards L.K., McGowan M.G., et al. Randomized trial of care management to improve Parkinson disease care quality. Neurology. 2019;92:e1831–e1842. doi: 10.1212/WNL.0000000000007324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fleisher J., Barbosa W., Sweeney M.M., Oyler S.E., Lemen A.C., Fazl A., Ko M., Meisel T., Friede N., Dacpano G., et al. Interdisciplinary Home Visits for Individuals with Advanced Parkinson’s Disease and Related Disorders. J. Am. Geriatr. Soc. 2018;66:1226–1232. doi: 10.1111/jgs.15337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marr J.A., Reid B. Implementing managed care and case management: The neuroscience experience. J. Neurosci. Nurs. 1992;24:281–285. doi: 10.1097/01376517-199210000-00010. [DOI] [PubMed] [Google Scholar]
- 56.Pretzer-Aboff I., Prettyman A. Implementation of an Integrative Holistic Healthcare Model for People Living with Parkinson’s Disease. Gerontologist. 2015;55(Suppl. 1):S146–S153. doi: 10.1093/geront/gnv004. [DOI] [PubMed] [Google Scholar]
- 57.Mestre T.A., Kessler D., Côté D., Liddy C., Thavorn K., Taljaard M., Grimes D. Pilot Evaluation of a Pragmatic Network for Integrated Care and Self-Management in Parkinson’s Disease. Mov. Disord. 2021;36:398–406. doi: 10.1002/mds.28332. [DOI] [PubMed] [Google Scholar]
- 58.Achey M.A., Beck C.A., Beran D.B., Boyd C.M., Schmidt P.N., Willis A.W., Riggare S.S., Simone R.B., Biglan K.M., Dorsey E.R. Virtual house calls for Parkinson disease (Connect.Parkinson): Study protocol for a randomized, controlled trial. Trials. 2014;15:465. doi: 10.1186/1745-6215-15-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dorsey E.R., Achey M.A., Beck C.A., Beran D.B., Biglan K.M., Boyd C.M., Schmidt P.N., Simone R., Willis A.W., Galifianakis N.B., et al. National Randomized Controlled Trial of Virtual House Calls for People with Parkinson’s Disease: Interest and Barriers. Telemed. J. E Health. 2016;22:590–598. doi: 10.1089/tmj.2015.0191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jorm L.R., Walter S.R., Lujic S., Byles J.E., Kendig H.L. Home and community care services: A major opportunity for preventive health care. BMC Geriatr. 2010;10:26. doi: 10.1186/1471-2318-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hellqvist C., Dizdar N., Hagell P., Berterö C., Sund-Levander M. Improving self-management for persons with Parkinson’s disease through education focusing on management of daily life: Patients’ and relatives’ experience of the Swedish National Parkinson School. J. Clin. Nurs. 2018;27:3719–3728. doi: 10.1111/jocn.14522. [DOI] [PubMed] [Google Scholar]
- 62.Hellqvist C. Promoting Self-Care in Nursing Encounters with Persons Affected by Long-Term Conditions-A Proposed Model to Guide Clinical Care. Int. J. Environ. Res. Public Health. 2021;18:2223. doi: 10.3390/ijerph18052223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schröder S., Martus P., Odin P., Schaefer M. Impact of community pharmaceutical care on patient health and quality of drug treatment in Parkinson’s disease. Int. J. Clin. Pharm. 2012;34:746–756. doi: 10.1007/s11096-012-9672-9. [DOI] [PubMed] [Google Scholar]
- 64.Coulter A., Cleary P.D. Patients’ experiences with hospital care in five countries. Health Aff. 2001;20:244–252. doi: 10.1377/hlthaff.20.3.244. [DOI] [PubMed] [Google Scholar]
- 65.Sjödahl Hammarlund C., Westergren A., Åström I., Edberg A.-K., Hagell P. The Impact of Living with Parkinson’s Disease: Balancing within a Web of Needs and Demands. Parkinsons. Dis. 2018;2018:4598651. doi: 10.1155/2018/4598651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Minkman M.M.N. Developing integrated care. Towards a development model for integrated care. Int. J. Integr. Care. 2012;12:e197. doi: 10.5334/ijic.1060. [DOI] [Google Scholar]
- 67.Murray C.J.L., Evans D.B. Health Systems Performance Assessment: Debates, Methods and Empiricism. World Health Organization; Geneva, Switzerland: 2003. [Google Scholar]
- 68.Hartweg D. Dorothea Orem: Self-Care Deficit Theory: Notes on Nursing Theories Volume 4. SAGE Publications; Thousand Oaks, CA, USA: 1991. [Google Scholar]
- 69.Van der Eijk M., Faber M.J., Al Shamma S., Munneke M., Bloem B.R. Moving towards patient-centered healthcare for patients with Parkinson’s disease. Parkinsonism Relat. Disord. 2011;17:360–364. doi: 10.1016/j.parkreldis.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 70.Fereshtehnejad S.-M., Lökk J. Active aging for individuals with Parkinson’s disease: Definitions, literature review, and models. Parkinsons. Dis. 2014;2014:739718. doi: 10.1155/2014/739718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Glasgow R.E., Davis C.L., Funnell M.M., Beck A. Implementing Practical Interventions to Support Chronic Illness Self-Management. JT Comm. J. Qual. Saf. 2003;29:563–574. doi: 10.1016/S1549-3741(03)29067-5. [DOI] [PubMed] [Google Scholar]
- 72.Freeman G.K., Olesen F., Hjortdahl P. Continuity of care: An essential element of modern general practice? Fam. Pract. 2003;20:623–627. doi: 10.1093/fampra/cmg601. [DOI] [PubMed] [Google Scholar]
- 73.Fabbri M., Caldas A.C., Ramos J.B., Sanchez-Ferro Á., Antonini A., Růžička E., Lynch T., Rascol O., Grimes D., Eggers C., et al. Moving towards home-based community-centred integrated care in Parkinson’s disease. Parkinsonism Relat. Disord. 2020;78:21–26. doi: 10.1016/j.parkreldis.2020.07.001. [DOI] [PubMed] [Google Scholar]
- 74.Goodwin N. Understanding Integrated Care. Int. J. Integr. Care. 2016;16:6. doi: 10.5334/ijic.2530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tenison E., Smink A., Redwood S., Darweesh S., Cottle H., van Halteren A., van den Haak P., Hamlin R., Ypinga J., Bloem B.R., et al. Proactive and Integrated Management and Empowerment in Parkinson’s Disease: Designing a New Model of Care. Parkinsons. Dis. 2020;2020 doi: 10.1155/2020/8673087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Valentijn P.P., Schepman S.M., Opheij W., Bruijnzeels M.A. Understanding integrated care: A comprehensive conceptual framework based on the integrative functions of primary care. Int. J. Integr. Care. 2013;13:e010. doi: 10.5334/ijic.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wagner E.H., Austin B.T., Davis C., Hindmarsh M., Schaefer J., Bonomi A. Improving chronic illness care: Translating evidence into action. Health Aff. 2001;20:64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 78.Van Halteren A.D., Munneke M., Smit E., Thomas S., Bloem B.R., Darweesh S.K.L. Personalized Care Management for Persons with Parkinson’s Disease. J. Parkinsons. Dis. 2020;10:S11–S20. doi: 10.3233/JPD-202126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ritchie C.S., Leff B., Garrigues S.K., Perissinotto C., Sheehan O.C., Harrison K.L. A Quality of Care Framework for Home-Based Medical Care. J. Am. Med. Dir. Assoc. 2018;19:818–823. doi: 10.1016/j.jamda.2018.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Graham I.D., Logan J., Harrison M.B., Straus S.E., Tetroe J., Caswell W., Robinson N. Lost in knowledge translation: Time for a map? J. Contin. Educ. Health Prof. 2006;26:13–24. doi: 10.1002/chp.47. [DOI] [PubMed] [Google Scholar]
- 81.Titova N., Chaudhuri K.R. Personalized medicine in Parkinson’s disease: Time to be precise. Mov. Disord. 2017;32:1147–1154. doi: 10.1002/mds.27027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gopalakrishna A., Alexander S.A. Understanding Parkinson Disease: A Complex and Multifaceted Illness. J. Neurosci. Nurs. 2015;47:320–326. doi: 10.1097/JNN.0000000000000162. [DOI] [PubMed] [Google Scholar]
- 83.Ferreira J.J., Godinho C., Santos A.T., Domingos J., Abreu D., Lobo R., Gonçalves N., Barra M., Larsen F., Fagerbakke Ø., et al. Quantitative home-based assessment of Parkinson’s symptoms: The SENSE-PARK feasibility and usability study. BMC Neurol. 2015;15:89. doi: 10.1186/s12883-015-0343-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kessler D., Liddy C. Self-management support programs for persons with Parkinson’s disease: An integrative review. Patient Educ. Couns. 2017;100:1787–1795. doi: 10.1016/j.pec.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 85.Kessler D., Hauteclocque J., Grimes D., Mestre T., Côtéd D., Liddy C. Development of the Integrated Parkinson’s Care Network (IPCN): Using co-design to plan collaborative care for people with Parkinson’s disease. Qual. Life Res. 2019;28:1355–1364. doi: 10.1007/s11136-018-2092-0. [DOI] [PubMed] [Google Scholar]
- 86.Lawn S., Schoo A. Supporting self-management of chronic health conditions: Common approaches. Patient Educ. Couns. 2010;80:205–211. doi: 10.1016/j.pec.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 87.Tennigkeit J., Feige T., Haak M., Hellqvist C., Seven Ü.S., Kalbe E., Schwarz J., Warnecke T., Tönges L., Eggers C., et al. Structured Care and Self-Management Education for Persons with Parkinson’s Disease: Why the First Does Not Go without the Second-Systematic Review, Experiences and Implementation Concepts from Sweden and Germany. J. Clin. Med. 2020;9:2787. doi: 10.3390/jcm9092787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chenoweth L., Gallagher R., Sheriff J.N., Donoghue J., Stein-Parbury J. Factors supporting self-management in Parkinson’s disease: Implications for nursing practice. Int. J. Older People Nurs. 2008;3:187–193. doi: 10.1111/j.1748-3743.2008.00123.x. [DOI] [PubMed] [Google Scholar]
- 89.Rollnick S., Miller W.R. What is Motivational Interviewing? Behav. Cogn. Psychother. 1995;23:325–334. doi: 10.1017/S135246580001643X. [DOI] [PubMed] [Google Scholar]
- 90.Achey M., Aldred J.L., Aljehani N., Bloem B.R., Biglan K.M., Chan P., Cubo E., Dorsey E.R., Goetz C.G., Guttman M., et al. The past, present, and future of telemedicine for Parkinson’s disease. Mov. Disord. 2014;29:871–883. doi: 10.1002/mds.25903. [DOI] [PubMed] [Google Scholar]
- 91.Bhidayasiri R., Martinez-Martin P. Clinical Assessments in Parkinson’s Disease: Scales and Monitoring. Int. Rev. Neurobiol. 2017;132:129–182. doi: 10.1016/bs.irn.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 92.Bloem B.R., Henderson E.J., Dorsey E.R., Okun M.S., Okubadejo N., Chan P., Andrejack J., Darweesh S.K.L., Munneke M. Integrated and patient-centred management of Parkinson’s disease: A network model for reshaping chronic neurological care. Lancet Neurol. 2020;19:623–634. doi: 10.1016/S1474-4422(20)30064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bloem B.R., Okun M.S., Klein C. Parkinson’s disease. Lancet. 2021 doi: 10.1016/S0140-6736(21)00218-X. [DOI] [PubMed] [Google Scholar]
- 94.Beck C.A., Beran D.B., Biglan K.M., Boyd C.M., Dorsey E.R., Schmidt P.N., Simone R., Willis A.W., Galifianakis N.B., Katz M., et al. National randomized controlled trial of virtual house calls for Parkinson disease. Neurology. 2017;89:1152–1161. doi: 10.1212/WNL.0000000000004357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bianchi M., Bagnasco A., Bressan V., Barisone M., Timmins F., Rossi S., Pellegrini R., Aleo G., Sasso L. A review of the role of nurse leadership in promoting and sustaining evidence-based practice. J. Nurs. Manag. 2018;26:918–932. doi: 10.1111/jonm.12638. [DOI] [PubMed] [Google Scholar]
- 96.Reynolds H., Wilson-Barnett J., Richardson G. Evaluation of the role of the Parkinson’s disease nurse specialist. Int. J. Nurs. Stud. 2000;37:337–349. doi: 10.1016/S0020-7489(00)00013-4. [DOI] [PubMed] [Google Scholar]
- 97.Ben-Pazi H., Browne P., Chan P., Cubo E., Guttman M., Hassan A., Hatcher-Martin J., Mari Z., Moukheiber E., Okubadejo N.U., et al. The Promise of Telemedicine for Movement Disorders: An Interdisciplinary Approach. Curr. Neurol. Neurosci. Rep. 2018;18:26. doi: 10.1007/s11910-018-0834-6. [DOI] [PubMed] [Google Scholar]
- 98.Dorsey E.R., Venkataraman V., Grana M.J., Bull M.T., George B.P., Boyd C.M., Beck C.A., Rajan B., Seidmann A., Biglan K.M. Randomized controlled clinical trial of “virtual house calls” for Parkinson disease. JAMA Neurol. 2013;70:565–570. doi: 10.1001/jamaneurol.2013.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chirra M., Marsili L., Wattley L., Sokol L.L., Keeling E., Maule S., Sobrero G., Artusi C.A., Romagnolo A., Zibetti M., et al. Telemedicine in Neurological Disorders: Opportunities and Challenges. Telemed. J. E Health. 2019;25:541–550. doi: 10.1089/tmj.2018.0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Monje M.H.G., Foffani G., Obeso J., Sánchez-Ferro Á. New Sensor and Wearable Technologies to Aid in the Diagnosis and Treatment Monitoring of Parkinson’s Disease. Annu. Rev. Biomed. Eng. 2019;21:111–143. doi: 10.1146/annurev-bioeng-062117-121036. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.