Abstract
This report describes a young patient with paroxysmal atrial fibrillation (AF) with termination pause. Primary mediastinal large B-cell lymphoma with pericardial and right atrial involvement was diagnosed, and he was free of AF after chemotherapy. Therefore, for young patients with tachy-brady syndrome, thorough evaluation for other causes is recommended. (Level of Difficulty: Beginner.)
Key Words: atrial fibrillation, lymphoma, right atrium, transesophageal echocardiography
Abbreviations and Acronyms: AF, atrial fibrillation; RA, right atrium; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography
Graphical abstract

A 37-year-old man with paroxysmal atrial fibrillation (AF) taking flecainide, 100 mg twice daily for 1 year, complained of intermittent palpitation and dizziness for days and was admitted.
Learning Objectives
-
•
To exclude secondary causes of AF in young patients, including structural cardiac abnormalities.
-
•
To understand the limitations of TTE in assessing RA anatomy and to consider the additional value of TEE in examining cardiac structures.
-
•
To highlight the fact that treatment of secondary reversible causes (in this case, chemotherapy for mediastinal B-cell lymphoma) can eliminate AF and sinus dysfunction in some patients.
Medical history
The patient was healthy, without any underlying health conditions except for AF.
Differential diagnosis
Although thorough evaluation of neurogenic dizziness should always be considered, arrhythmia-related dizziness was the most likely diagnosis based on his medical history.
Investigations
His physical examination appeared normal, without superficial venous distension or facial or limb edema. A 24-h Holter monitor showed sinus rhythm, paroxysmal AF with termination pause of up to 7.6 s, and frequent junctional escape rhythm (Figure 1). Transthoracic echocardiography (TTE) examination was unremarkable. Antiarrhythmic agents were discontinued, and he decided to undergo catheter ablation for AF. However, preoperative transesophageal echocardiography (TEE) showed a soft tissue density in the right atrium (RA), with superior vena cava (SVC) encasement and no venous return obstruction (Figures 2A and 2B, Video 1). Therefore, catheter ablation was not done. Tissue biopsy results reported the presence of large neoplastic B-cells with enlarged nuclei. Positron emission tomography/computed tomography showed increased fluorodeoxyglucose uptake in the pericardium, surrounding the ascending aorta, SVC, main pulmonary artery, right pulmonary artery, and RA (Figure 3). Primary mediastinal large B-cell lymphoma was confirmed.
Figure 1.
24-h Holter Recording of the Patient
Intermittent junctional escape rhythm and atrial fibrillation with termination pause were found in the 24-h Holter recording.
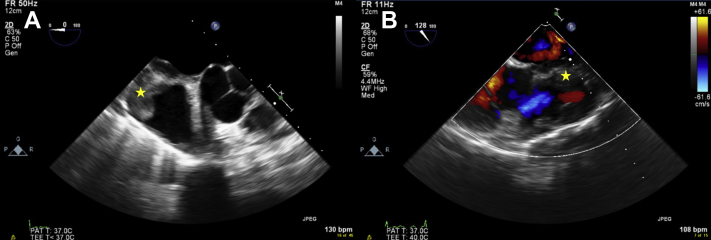
Figure 2.
Transesophageal Echocardiography Examination
TEE showed soft tissue density in the RA with encasement of SVC (A) and (B) (star) and RA inflow impairment before chemotherapy. RA = right atrium; SVC = superior vena cava; TEE = transesophageal echocardiography.
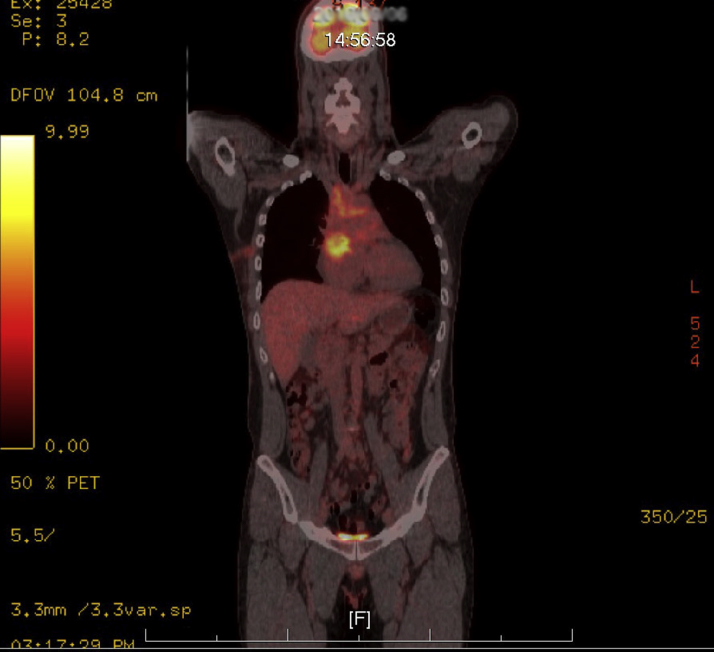
Figure 3.
PET/CT Examination
PET/CT showed fluorodeoxyglucose uptake in the anterior mediastinum with RA involvement. CT = computed tomography; PET = positron emission tomography; RA = right atrium.
Management
A total of 6 cycles of chemotherapy with dosage-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab) were prescribed. A 12-lead electrocardiogram (ECG) was performed before each cycle of chemotherapy, as well as continuous ECG monitoring during chemotherapy infusion. He returned to sinus rhythm 4 weeks after the first cycle of chemotherapy. He completed another 5 cycles of chemotherapy thereafter and remained in sinus rhythm in all follow-up ECGs. The event recorder showed sinus rhythm with occasional atrial premature complexes and TEE showed complete resolution of the RA mass (Figure 4).
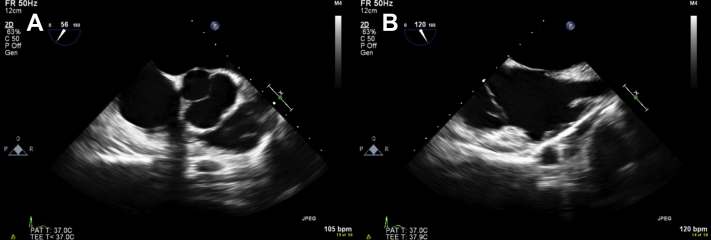
Figure 4.
TEE After 6 Cycles of Chemotherapy
The follow-up TEE (A and B) showed complete resolution of intracardiac mass. TEE = transesophageal echocardiography.
Discussion
TTE is the primary screening tool for anatomic and functional assessment without exposure to ionizing radiation. However, assessment of the RA is limited, with 2-dimensional TTE due to viewing dependency and geometric difficulties. Conventionally, the RA has been described in ultrasonography literature as the “neglected chamber” due to its geometry and posterior anatomical location in the heart (1). In addition, characterization of RA tissue using TTE can be limited. All these factors likely contribute to the missed diagnosis shown on TTE in this case.
Primary cardiac malignancy is rarely seen, whereas metastasis with cardiac involvement is sometimes reported. Previous medical literature has reported that primary cardiac lymphoma accounts for approximately 1% of primary cardiac tumors, and the incidence of secondary cardiac lymphoma can be up to 20% of cases (2). For cardiac involvement, the right side of the heart is more common than the left and is usually accompanied by SVC syndrome, pericardial invasion, lymphatic return obstruction, and pericardial effusion (3). Various arrhythmia episodes can occur in this scenario, including AF, atrioventricular block, and ventricular tachycardia (4).
Sick sinus syndrome is an uncommon complication of cardiac lymphoma and could be an initial symptom or a terminal manifestation (5). Clinical presentations include sinus arrest, tachy-brady syndrome, or AF with slow ventricular rate (6). Most cases have been of B-cell origin, whereas only 1 case was of T-cell origin (7), and pathology examination demonstrated typical infiltration of lymphoma cells in the sinus node region (5). In previous case reports, most patients were middle aged to elderly, with a median of >60 years of age. The patient in this case report was probably the youngest one ever reported.
Because of the variation of clinical presentations, delayed diagnosis is common, and some patients have been found to have cardiac lymphoma after pacemaker implantation (8). The response to chemotherapy also varies. Some patients, such as in this case, returned to normal sinus rhythm after chemotherapy, whereas others developed sick sinus syndrome during treatment (5,7). The prognosis relies on the lymphoma stage and cell types. Whether the presence of sick sinus syndrome implies poor prognosis remains uncertain.
Follow-up
The current patient remained in sinus rhythm and was free of AF without any use of antiarrhythmic agent thereafter.
Conclusions
As the incidence of AF has increased over the years, it is common to see young patients with paroxysmal AF. Nevertheless, a thorough evaluation for both genetic and cardiac structural abnormalities is important in these patients. As certain structural abnormalities could be missed by TTE alone, a high index of suspicion is required. The present report describes a rare case of paroxysmal AF with termination pause caused by primary mediastinal large B-cell lymphoma with cardiac involvement. Correct diagnosis and successful chemotherapy of cardiac lymphoma metastasis can eradicate primary disease and eliminate AF, raising awareness of precipitating factors in young population.
Author Disclosures
This research was supported by the Ministry of Science and Technology, Taiwan awards NSC-101-2314-B-195-020, NSC103-2314-B-010-005-MY3, 103-2314-B-195-001-MY3, 101-2314-B-195-020–MY1, MOST 103-2314-B-195-006-MY3, MOST 108-2314-B-075-022, and NSC102-2314-B-002-046-MY3 and MacKay Memorial Hospital awards 10271, 10248, 10220, 10253, 10375, 10358, and E-102003. The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgment
The authors thank the Research Foundation of Cardiovascular Medicine.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Transesophageal echocardiography showed a soft tissue density in the right atrium with superior vena cava encasement.
References
- 1.Rai A.B., Lima E., Munir F. Speckle tracking echocardiography of the right atrium: the neglected chamber. Clin Cardiol. 2015;38:692–697. doi: 10.1002/clc.22438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O'Mahony D., Peikarz R.L., Bandettini W.P., Arai A.E., Wilson W.H., Bates S.E. Cardiac involvement with lymphoma: a review of the literature. Clin Lymphoma Myeloma. 2008;8:249–252. doi: 10.3816/CLM.2008.n.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Besien K., Kelta M., Bahaguna P. Primary mediastinal B-cell lymphoma: a review of pathology and management. J Clin Oncol. 2001;19:1855–1864. doi: 10.1200/JCO.2001.19.6.1855. [DOI] [PubMed] [Google Scholar]
- 4.Linhart M., Lickfett L., Hammersting C., Tiemann K., Nickenig G., Lewalter T. Paroxysmal atrial flutter caused by cardiac lymphoma. Pacing Clin Electrophysiol. 2006;29:682–684. doi: 10.1111/j.1540-8159.2006.00419.x. [DOI] [PubMed] [Google Scholar]
- 5.Suzuki T., Ishibashi S., Qin X. Sick sinus syndrome in association with malignant lymphoma. Eur Heart J. 1996;17:968. doi: 10.1093/oxfordjournals.eurheartj.a014987. [DOI] [PubMed] [Google Scholar]
- 6.Kamimura M., Tanabe N., Hojo M., Horiuchi T., Kudo K., Saitoh K. Malignant lymphoma demonstrating sick sinus syndrome. Intern Med. 1998;37:463–466. doi: 10.2169/internalmedicine.37.463. [DOI] [PubMed] [Google Scholar]
- 7.Haq M., Patel A., Guglin M. Cardiac lymphoma: sinus pauses disappear after chemotherapy. Ann Hematol. 2014;93:891–892. doi: 10.1007/s00277-013-1894-y. [DOI] [PubMed] [Google Scholar]
- 8.Motto A., Ballo P., Zito D. Primary cardiac lymphoma presenting as sick sinus syndrome. J Clin Oncol. 2008;26:6003–6005. doi: 10.1200/JCO.2008.19.4803. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transesophageal echocardiography showed a soft tissue density in the right atrium with superior vena cava encasement.