Abstract
Obstruction of the inferior vena cava (IVC) following surgical repair of an atrial septal defect (ASD) is a rare complication. We present the case of a patient who developed IVC obstruction following surgical repair of a large secundum ASD. The diagnostic and management approaches used to care for this patient are discussed. (Level of Difficulty: Intermediate.)
Key Words: ASD repair, eustachian valve, secundum ASD
Abbreviations and Acronyms: ASD, atrial septal defect; CMR, cardiac magnetic resonance; CT, computed tomography; CTA, computed tomography angiography; EV, eustachian valve; IVC, inferior vena cava; RA, right atrium; TEE, transesophageal echocardiogram; TTE, transthoracic echocardiogram
Graphical abstract
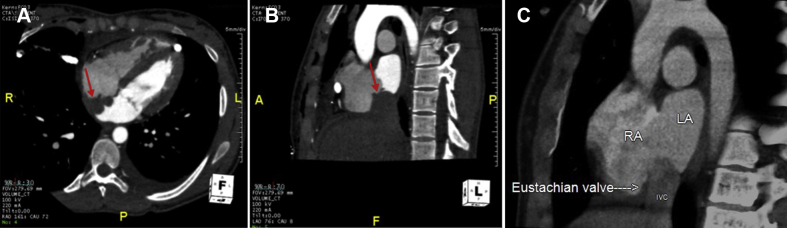
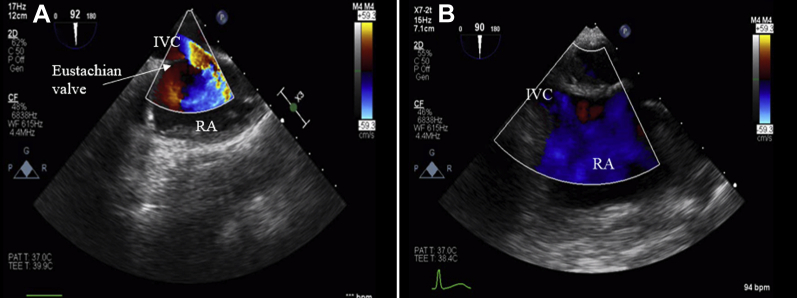
A 19-year-old female was admitted to the hospital for elective surgical repair of a large secundum atrial septal defect (ASD). She underwent minimally invasive bovine pericardial patch closure of the secundum ASD through a right thoracotomy incision. Intraoperative transesophageal echocardiogram (TEE) images acquired after completion of ASD repair showed intact ASD repair and a high-velocity jet of uncertain significance entering the right atrium that was eliminated by clamping the inferior vena cava (IVC) (Figure 1, Video 1). Post-operatively, there was a moderate left-sided pleural effusion which was drained by thoracentesis. Her vital signs were within normal limits. Physical examination was significant for a thoracotomy incision that was healing well and mild bilateral lower extremity edema. A transthoracic echocardiogram (TTE) obtained 2 days post-operatively again demonstrated the high-velocity jet entering the right atrium (Figure 2), as well as a nonobstructive echodensity in the IVC just proximal to the right atrial junction. Further imaging was performed.
Learning Objectives
-
•
To emphasize the importance of identifying a prominent eustachian valve on pre-operative imaging prior to surgical repair of ASD.
-
•
To highlight the echocardiographic and radiographic manifestations of post-operative IVC obstruction following ASD repair.
-
•
To describe the appropriate diagnostic and management approach for a patient with post-operative IVC obstruction and thrombosis following ASD repair.
Figure 1.
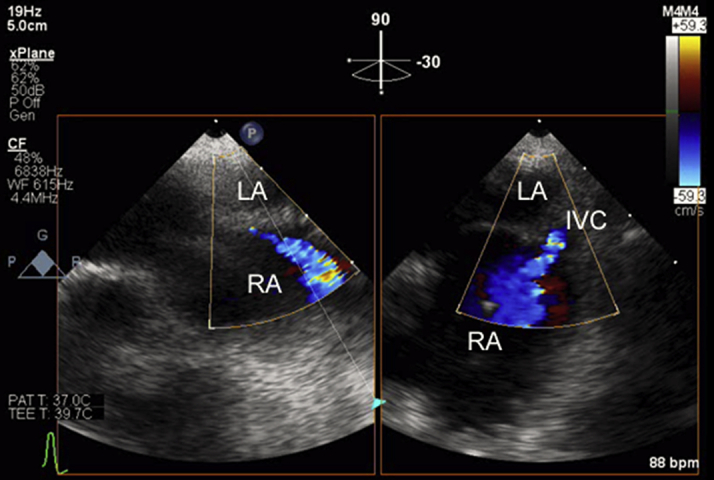
Intraoperative Transesophageal Echocardiogram in Mid Esophageal Position, Biplane Image Shows Turbulent Flow Originating From the Inferior Vena Cava
Figure 2.
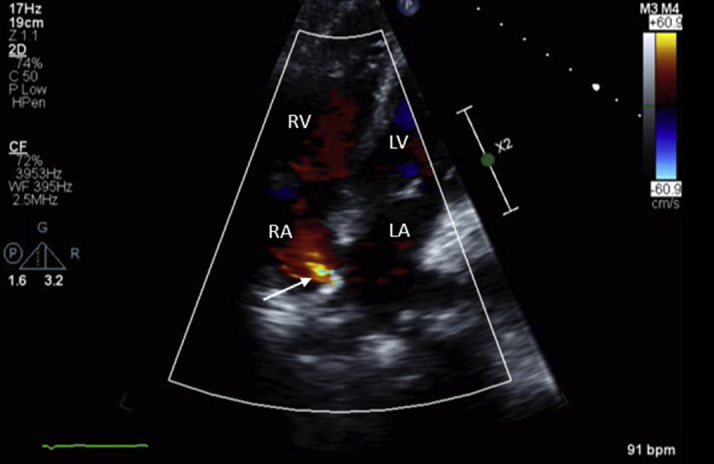
Post-Operative Transthoracic Echocardiogram Apical 4-Chamber View Shows High-Velocity Jet in the Right Atrium
Arrow indicates the high velocity jet entering the right atrium on this still frame.
Medical History
The patient initially presented to the cardiology clinic for evaluation of syncope, which was believed to be vasovagal in origin. However, she was noted to have fixed splitting of the second heart sound on physical examination. Electrocardiography showed first-degree atrioventricular block and incomplete right bundle branch block. A TTE showed a secundum ASD with significant left-to-right shunting and moderate right atrial and right ventricular dilation. Cardiac magnetic resonance (CMR) imaging confirmed a large secundum ASD measuring 2.4 × 2.3 cm with left-to-right shunting and pulmonary/systemic flow ratio (Qp:Qs) of 2.3. The CMR also showed moderate-to-severely dilated right ventricle without hypertrophy and unobstructed right ventricular outflow tract, main pulmonary artery, and branch pulmonary arteries. Normal pulmonary and systematic venous connections were noted. Due to evidence of right heart enlargement, she was referred for ASD closure. Computed tomography (CT) angiography of the heart was performed, which confirmed the CMR findings and demonstrated deficient rims for percutaneous device closure, and therefore, surgical ASD closure was planned.
Differential Diagnosis
Differential diagnosis of a high-velocity jet entering the right atrium included residual ASD, anomalous pulmonary venous connection, IVC obstruction, ventricular septal defect, Gerbode defect, coronary artery fistula, and severe tricuspid regurgitation.
Investigations
A CT angiogram of the heart was obtained which showed a lack of admixture of unenhanced blood from the IVC with contrast-enhanced blood in the right atrium, worrisome for IVC obstruction (Figures 3A and 3B). The os of the IVC was bounded superiorly by the ASD patch and inferiorly by the eustachian valve (EV). For comparison, a preoperative CT scan highlighting the EV is shown (Figure 3C). An abdominal ultrasonogram was performed, which showed an IVC thrombus measuring 5 cm. This was confirmed by CT venogram, which revealed extensive nonocclusive thrombus extending from the IVC to the right external iliac vein (Figure 4A).
Figure 3.
Axial Oblique and Sagittal Oblique CTA Images
(A) Axial oblique and (B) sagittal oblique CTA images shows lack of admixture of unenhanced blood from the IVC with the contrast in the right atrium (arrows), suggestive of iatrogenic IVC obstruction. (C) Preoperative CT imaging highlighting the location of the prominent EV. CTA = computed tomography angiography; EV = eustachian valve; IVC = inferior vena cava.
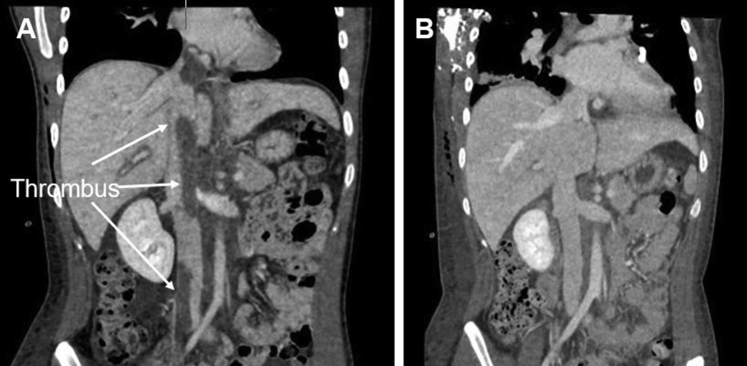
Figure 4.
Coronal Oblique Reconstructions of CT Venogram
Coronal oblique reconstructions of CT venogram showing (A) extensive thrombus in the IVC before and (B) resolution of thrombus after pharmacomechanical thrombectomy and EV excision. Abbreviations as in Figure 3.
Management
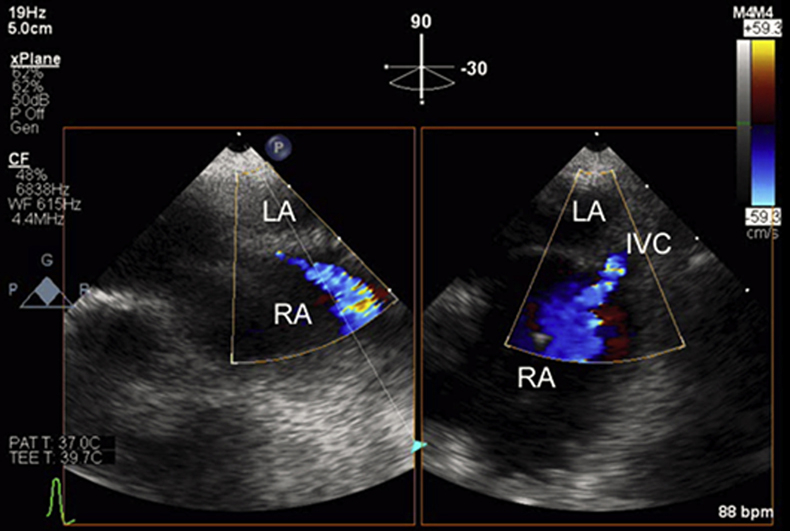
The patient was started on systemic anticoagulation with heparin infusion. Interventional radiology performed pharmacomechanical thrombectomy of the iliocaval thrombus as well as balloon angioplasty of the cavoatrial junction, resulting in a significantly reduced clot burden and improved antegrade flow into the right atrium. Repeat TTE showed residual high-velocity flow in the posterolateral region of the right atrium, indicating persistent IVC stenosis. Therefore, the patient was returned to the operating room for reoperative right thoracotomy and excision of the EV through the initial thoracotomy incision. Intraoperative TEE showed a narrow high-velocity jet directed from the IVC to the RA (Figure 5A). After EV excision, TEE showed restoration of laminar flow from the IVC into the RA (Figure 5B, Video 2); a post-operative CT venogram showed no residual IVC thrombus (Figure 4B) but small residual nonocclusive thrombi in the right common iliac vein and right external iliac vein. The patient was discharged home on warfarin therapy
Figure 5.
TEE Images in Midesophageal Bicaval View
(A) TEE images in midesophageal bicaval view show a narrow high-velocity jet from the IVC to the right atrium before excision of the EV. (B) After EV excision, laminar flow between the IVC and RA was restored. Abbreviations as in Figure 3.
Discussion
ASD is a common congenital heart abnormality, accounting for approximately 25% to 30% of congenital heart defects that are diagnosed in adulthood (1). The ASD is associated with other congenital defects concomitantly in approximately 30% of cases, including but not limited to total anomalous pulmonary venous connection, cleft mitral valve, persistent left superior vena cava, and valvular pulmonic stenosis. Transcatheter or surgical closure of the secundum ASD is indicated if there is impaired functional capacity, right-sided chamber enlargement, a Qp:Qs ratio ≥1.5:1, and absence of cyanosis and severe pulmonary hypertension (2). Surgical repair of the ASD is a safe and effective operation associated with <1% mortality (3,4) and rates of post-operative complications of 6% to 18% (4). Long-term follow-up of these patients results in excellent survival and functional capacity (5). Complications include bleeding, episodes of arrhythmia, pericardial effusion, pneumothorax, surgical wound complications, and pulmonary edema (6,7). In the present patient, the abnormal high-velocity flow entering the right atrium, shown on echocardiography but not present on pre-operative imaging, was a clue to an anatomical complication of the surgical repair. Imaging with CT angiography confirmed IVC obstruction and provided accurate diagnostic information about the cause of the IVC obstruction.
In the developing fetus, the EV is situated at the cavoatrial junction and directs blood flow toward the foramen ovale. The EV persists into adulthood but has no function after birth. In adults, the EV can range from being a prominent structure in the right atrium to being completely absent (8). When it is a prominent structure, the EV can be mistaken for the interatrial septum (9), which can cause inadvertent surgical or percutaneous closure of the EV to interatrial septum (10). Reports of this complication are rare but do exist in the medical literature. A 20-year-old woman who underwent primary suturing of the ASD was found to have restriction of the right atrial inflow on TEE due to iatrogenic suturing of the EV to the interatrial septum (10). Similarly, a 5-month-old boy with vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal anomalies, and limb abnormalities (VACTERL) syndrome underwent surgery for ASD closure but subsequently developed hepatomegaly, ascites, and prominent superficial veins on the chest and abdomen; and on echocardiography, it was noted that the EV had been sutured to the interatrial septum (11).
In the present patient, suturing the free end of the EV to the interatrial septum caused restricted flow between the IVC and the right atrium, ultimately leading to thrombosis along the iliocaval venous system. This patient required 2 additional procedures (thrombectomy with balloon dilation of cavoatrial junction and surgical excision of the EV) to restore laminar flow between the IVC and RA.
Follow-up
The patient recovered well from the hospitalization and is doing well. She underwent an extensive thrombophilia workup, and there was no evidence of inheritable or acquired thrombophilia. At least 3 months of anticoagulation therapy was planned.
Conclusions
This case highlights the utility of multimodality cardiac imaging using echocardiography and CT for accurate diagnosis of post-operative anatomical complications of ASD repair. Obstruction of the IVC should be suspected if there is presence of a high-velocity jet in the right atrium following ASD repair. Furthermore, this case illustrates the importance of identifying a prominent EV on pre-operative imaging prior to surgical ASD repair. Given its anatomical location, a prominent EV can be mistaken for the interatrial septum, which can result in inadvertent suturing of the EV and subsequent obstruction of IVC flow. Expeditious diagnostic workup and intervention resulted in good clinical outcome for this patient.
Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Intraoperative TEE in mid-esophageal position shows surgical ASD closure and abnormally high velocity right atrial inflow.
Intraoperative TEE in mid-esophageal position, bicaval view shows laminar IVC inflow after obstruction is relieved.
References
- 1.Lindsey J.B., Hillis L.D. Clinical update: atrial septal defect in adults. Lancet. 2007;369:1244–1246. doi: 10.1016/S0140-6736(07)60576-5. [DOI] [PubMed] [Google Scholar]
- 2.Stout K.K., Daniels C.J., Aboulhosn J.A. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73:1494–1563. doi: 10.1016/j.jacc.2018.08.1028. [DOI] [PubMed] [Google Scholar]
- 3.Ryan W.H., Cheirif J., Dewey T.M., Prince S.L., Mack M.J. Safety and efficacy of minimally invasive atrial septal defect closure. Ann Thorac Surg. 2003;75:1532–1534. doi: 10.1016/s0003-4975(02)04720-3. [DOI] [PubMed] [Google Scholar]
- 4.Chu M.W.A., Losenno K.L., Fox S.A. Clinical outcomes of minimally invasive endoscopic and conventional sternotomy approaches for atrial septal defect repair. Can J Surg. 2014;57:E75. doi: 10.1503/cjs.012813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liava’a M., Kalfa D. Surgical closure of atrial septal defects. J Thorac Dis. 2018;10(Suppl 24):S2931–S2939. doi: 10.21037/jtd.2018.07.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Du Z.D., Hijazi Z.M., Kleinman C.S., Silverman N.H., Larntz K., Amplatzer Investigators Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults: results of a multicenter nonrandomized trial. J Am Coll Cardiol. 2002;39:1836–1844. doi: 10.1016/s0735-1097(02)01862-4. [DOI] [PubMed] [Google Scholar]
- 7.Geva T., Martins J.D., Wald R.M. Atrial septal defects. Lancet. 2014;383:1921–1932. doi: 10.1016/S0140-6736(13)62145-5. [DOI] [PubMed] [Google Scholar]
- 8.Yavuz T., Nazli C., Kinay O., Kutsal A. Giant eustachian valve with echocardiographic appearance of divided right atrium. Texas Heart Inst J. 2002;29:336–338. [PMC free article] [PubMed] [Google Scholar]
- 9.Akkad I., Wartak S., Moskovits M. Pseudo atrial septum defect from a Eustachian valve on transesophageal echocardiogram. J Echocardiogr. 2017;15:41–42. doi: 10.1007/s12574-016-0303-7. [DOI] [PubMed] [Google Scholar]
- 10.Akpinar I., Guray Y., Demirkan B. Rare postsurgical complication of atrial septal defect closure: Right inflow obstruction due to inadvertent suturing of eustachian valve to interatrial septum. Can J Cardiol. 2011;27 doi: 10.1016/j.cjca.2011.08.116. 868.e9–868. [DOI] [PubMed] [Google Scholar]
- 11.Becker A., Buss M., Sebening W., Meisner H., Döhlemann C. Acute inferior cardiac inflow obstruction resulting from inadvertent surgical closure of a prominent eustachian valve mistaken for an atrial septal defect. Pediatr Cardiol. 1999;20:155–157. doi: 10.1007/s002469900427. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Intraoperative TEE in mid-esophageal position shows surgical ASD closure and abnormally high velocity right atrial inflow.
Intraoperative TEE in mid-esophageal position, bicaval view shows laminar IVC inflow after obstruction is relieved.