Abstract
Purpose
To describe the management of arterial partial pressure of carbon dioxide (PaCO2) in severe traumatic brain-injured (TBI) patients, and the optimal target of PaCO2 in patients with high intracranial pressure (ICP).
Methods
Secondary analysis of CENTER-TBI, a multicentre, prospective, observational, cohort study. The primary aim was to describe current practice in PaCO2 management during the first week of intensive care unit (ICU) after TBI, focusing on the lowest PaCO2 values. We also assessed PaCO2 management in patients with and without ICP monitoring (ICPm), and with and without intracranial hypertension. We evaluated the effect of profound hyperventilation (defined as PaCO2 < 30 mmHg) on long-term outcome.
Results
We included 1100 patients, with a total of 11,791 measurements of PaCO2 (5931 lowest and 5860 highest daily values). The mean (± SD) PaCO2 was 38.9 (± 5.2) mmHg, and the mean minimum PaCO2 was 35.2 (± 5.3) mmHg. Mean daily minimum PaCO2 values were significantly lower in the ICPm group (34.5 vs 36.7 mmHg, p < 0.001). Daily PaCO2 nadir was lower in patients with intracranial hypertension (33.8 vs 35.7 mmHg, p < 0.001). Considerable heterogeneity was observed between centers. Management in a centre using profound hyperventilation (HV) more frequently was not associated with increased 6 months mortality (OR = 1.06, 95% CI = 0.77–1.45, p value = 0.7166), or unfavourable neurological outcome (OR 1.12, 95% CI = 0.90–1.38, p value = 0.3138).
Conclusions
Ventilation is manipulated differently among centers and in response to intracranial dynamics. PaCO2 tends to be lower in patients with ICP monitoring, especially if ICP is increased. Being in a centre which more frequently uses profound hyperventilation does not affect patient outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00134-021-06470-7.
Keywords: Carbon dioxide, Hyperventilation, Traumatic brain injury, Intracranial pressure, Outcome
Take-home message
| The manipulation of arterial carbon dioxide levels (PaCO2) is easy, and hyperventilation (HV) has been a common ICP-lowering strategy for over half a century. However, hyperventilation-induced vasoconstriction is a double-edged sword. It reduces cerebral blood volume and intracranial volume, and therefore, lowers ICP |
| We observed huge variability among centers in PaCO2 values and use of HV. Although causal inferences cannot be drawn from these observational data, our results suggest that, in patients with severe intracranial hypertension, HV is not associated with worse long-term clinical outcome |
Introduction
Changes in the arterial partial pressure of carbon dioxide (PaCO2), by modifying the extravascular pH, modulate cerebrovascular tone, and hence cerebral blood flow (CBF) and cerebral blood volume (CBV) [1, 2]. Hypercapnia results in perivascular acidosis, which causes cerebral vasodilation, and consequently, an increase in intracranial volume. In patients with poor intracranial compliance, this could raise intracranial pressure (ICP). On the other hand, hyperventilation (HV) induced alkalosis reduces vascular calibre, and hence CBV, and can represent an effective measure to control intracranial hypertension, when ICP remains elevated despite first-line therapies [3–6]. However, hypocapnic cerebral vasoconstriction can also reduce CBF [7], thus posing the risk of secondary ischaemic insults [8]. In a survey across European trauma centers, the most frequently reported PaCO2 target was 36–40 mmHg in the absence of intracranial hypertension, which was reduced to 30–35 mmHg when ICP was > 20 mmHg [9]. The most recent evidence-based guidelines on TBI management provide no definitive recommendations regarding target PaCO2 levels due to the low quality of evidence available on this issue [10, 11].
Consequently, although many patients with severe TBI undergo several days of mechanical ventilation, there is little evidence-based guidance on PaCO2 targets, and clinical practice remains highly variable. A recent consensus on mechanical ventilation in patients with acute brain injury suggested aiming for a physiologic range of PaCO2 between 35 and 45 mmHg [12], and to only use hyperventilation (with an undefined PaCO2 target) as a short-term therapeutic option in patients with evidence of brain herniation. However, the document was unable to provide a recommendation on the use of hyperventilation in patients who showed significant ICP elevation, but no evidence of herniation. A management algorithm for patients with intracranial hypertension, based on expert consensus, suggested the use of HV (PaCO2 32–35 mmHg) for controlling ICP only as a second-tier treatment, did not support lower PaCO2 levels and recommended against routine hyperventilation to PaCO2 below 30 mmHg [13].
The objectives of this study were to assess, in a real-world context, PaCO2 management and the lowest target of PaCO2 in a large cohort of mechanically ventilated TBI patients and practice variability between centres to evaluate the association between the use of profound HV and 6-month clinical outcomes.
Methods
Study design and patients
The Collaborative European NeuroTrauma Effectiveness in Research in Traumatic Brain Injury (CENTER-TBI study, registered at clinicaltrials.gov NCT02210221) is a longitudinal, prospective collection of data from TBI patients across 65 centers in Europe. The study was conducted between December 19th, 2014, and December 17th, 2017 and details regarding the design and the results of the screening and enrolment process have been previously described [14–16].
The CENTER-TBI study was approved by the Medical Ethics Committees in all participating centers, and informed consent was obtained according to local regulations (https://www.center-tbi.eu/project/ethical-approval). This project on PaCO2 management was preregistered on the CENTER-TBI proposal platform and approved by the CENTER-TBI proposal review committee before starting the analysis (ESM Document 1). This report complies with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines (ESM Table S1).
We included all patients in the CENTER-TBI Core study who had a TBI necessitating ICU admission, required tracheal intubation and mechanical ventilation, had at least two PaCO2 measurements in the first 7 days and had been admitted to a study centre that enrolled at least ten patients.
Data collection and definitions
Detailed information on data collection is available on the study website (https://www.center-tbi.eu/data/dictionary). For the first week in ICU, the daily lowest and highest PaCO2 values from arterial blood gases and, if an ICP device was inserted, the hourly ICP measures were used for analysis.
HV was defined as moderate for PaCO2 ranging between 30 and 35 mmHg and profound for PaCO2 < 30 mmHg [10, 13]. Therapy intensity level (TIL) was calculated according to the most recent TIL scale [17]. Patients with invasive ICP monitoring during the first week of ICU stay were classified as ICPm, while those who did not receive ICP monitoring during ICU stay as no-ICPm. Intracranial hypertension was defined as ICP > 20 mmHg.
Objectives
The aims of this study are:
to describe the PaCO2 values in the first week from ICU admission in mechanically ventilated TBI patients, and to evaluate practice variability across centers, particularly focusing on the lowest targets of PaCO2;
to assess at a center level the PaCO2 management in patients with/without ICP monitoring and with/without intracranial hypertension;
to evaluate the association between patient outcomes and center propensity to use profound HV.
Outcomes
Mortality and functional outcome (measured as the Extended Glasgow Outcome Score, GOSE) were assessed at 6 months. All responses were obtained by study personnel from patients or from a proxy (where impaired cognitive capacity prevented patient interview), during a face-to-face visit, by telephone interview, or by postal questionnaire around 6 months after injury [18]. All evaluators had received training in the use of the GOSE. An unfavourable outcome was defined as GOSE ≤ 4, which includes both poor functional outcome and mortality.
Statistical methods
Patient characteristics were described by means (± standard deviation, SD), medians (I–III quartiles, Q1–Q3) and counts or proportions, as appropriate. The comparison of baseline features according to ICP monitoring was performed using Mann–Whitney U test, t test and Chi-square test as appropriate. We used the median odds ratio (MOR) to estimate the between-centre heterogeneity in targeting a PaCO2 of 35–45 mmHg. MOR was obtained from a longitudinal logistic mixed-effect model on daily lowest PaCO2 adjusted for the IMPACT core covariates [19], ICP monitoring, and daily evidence of elevated ICP (at least one ICP > 20 mmHg during the day); and with a hierarchical random intercept effect’s structure (i.e., patients within centers). The same model architecture was used to quantify between-centres heterogeneity in the use of profound HV.
We resorted to an instrumental variable approach to evaluate the association between HV and 6-month outcomes, trying to minimize the potential measured and unmeasured confounding acting in this complex observational study [20]. This was done by considering the propensity of centres to apply profound HV, measured as the proportion of daily lowest PaCO2 < 30 mmHg, as an instrument in the logistic regression model with a random intercept for centers. This model was adjusted for some subject-specific covariates that included IMPACT core covariates at baseline, ICP monitoring and dose of intracranial hypertension, calculated as the area under the ICP profile above 20 mmHg, named AUC ICP > 20[21]. The assumptions underlying the IV approach were assessed (ESM-Statistical methods).
Tests were performed with a two-sided significance level of 5%. All analyses were conducted using R statistical software (version 4.03).
Results
Of the 4509 patients included in the CENTER-TBI dataset, 2138 patients with TBI from 51 centers in Europe were admitted to ICU. Among these, 1176 required mechanical ventilation and had at least two PaCO2 measurements within the first 7 days from ICU admission. Excluding the centres that enrolled less than ten patients, 1100 patients from 36 centers were available for the analysis (ESM Fig. 1). During the first week of ICU admission, a total of 11,791 measurements of PaCO2 were available (5931 lowest and 5860 highest daily values).
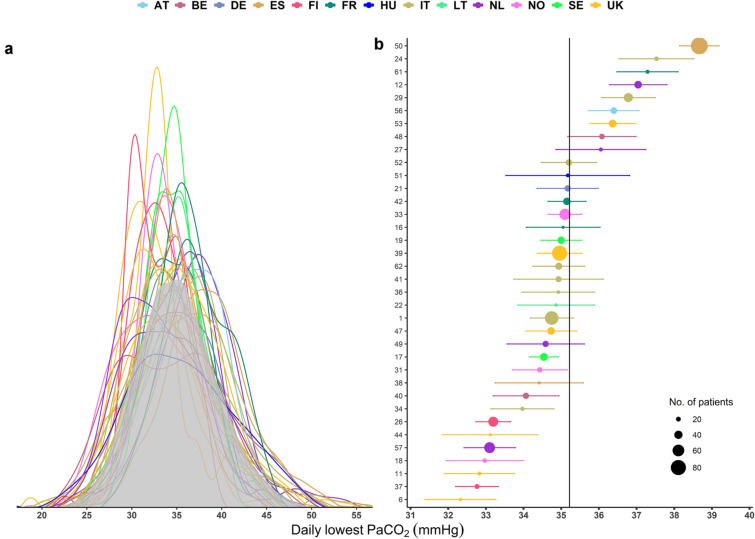
Fig. 1.
(a) Distributions of the daily lowest PaCO2 recorded in the first 7 days of ICU in each participating centre (coloured by country) and overall (grey area). These distributions were estimated by a Gaussian kernel density. (b) Centre-specific mean values (coloured by country) of daily lowest PaCO2 with the corresponding 95% confidence intervals. The solid vertical line represents the overall mean of daily lowest PaCO2 values, and the size of the dots is proportional to the number of patients in the centre. PaCO2 the partial pressure of carbon dioxide, AT Austria, BE Belgium, DE Germany, ES Spain, FI Finland, FR France, HU Hungary, IT Italy, LT Lithuania, NL Netherlands, NO Norway, SE Serbia, UK United Kingdom
Patient characteristics
Patient characteristics at hospital admission in the overall population and stratified according to the presence (n = 751) or not (n = 349) of ICP monitoring, are summarized in Table 1. The median age was 48 years (Q1–Q3 = 29–64), and most patients were male (74%). 64.7% of patients presented with a severe TBI (Glasgow Coma Scale, GCS ≤ 8) and 12.5% of cases were complicated by thoracic trauma. In 727 (97%) ICPm patients, ICP was inserted by the second day of ICU admission.
Table 1.
Baseline demographic and clinical characteristics, including trauma characteristics, clinical presentation, and neuroimaging features at ICU admission in the overall population and stratified according to the presence or not of ICP monitoring
| Characteristic | Overall (n = 1100) | no-ICPm (n = 349) | ICPm (n = 751) | P value | |
|---|---|---|---|---|---|
| Age (years), median (Q1–Q3) | 48 (29–64) | 53 (31–69) | 46 (28–61) | < 0.001 | |
| Sex, n (%) | Female | 284 (25.8) | 89 (25.5) | 195 (26) | 0.929 |
| Thoracic trauma, n (%) | Yes | 138 (12.5) | 42(12) | 96 (12.8) | 0.802 |
| ISS, median (Q1–Q3) | 34 (25–48) | 34 (25–43) | 34 (25–48) | 0.011 | |
| Hypotension, n (%) | Yes | 178 (17.4) | 60 (17.7) | 118 (17.3) | 0.936 |
| Not available | 78 | 10 | 68 | ||
| Hypoxia, n (%) | Yes | 182 (17.9) | 53 (15.6) | 129 (19) | 0.217 |
| Not available | 82 | 10 | 72 | ||
| Severity TBI, n (%) | GCS ≤ 8 | 367 (35.3) | 147 (44.3) | 220 (31) | < 0.001 |
| GCS > 8 | 674 (64.7) | 185 (55.7) | 489 (69) | ||
| Not available | 59 | 17 | 42 | ||
| Pupillary reactivity, n (%) | Both reactive | 799 (75.8) | 280 (82.8) | 519 (72.5) | 0.001 |
| One reactive | 89 (8.4) | 22 (6.5) | 67 (9.4) | ||
| Both unreactive | 166 (15.7) | 36 (10.7) | 130 (18.2) | ||
| Not available | 47 | 11 | 35 | ||
| GCS motor, n (%) | None | 460 (42.7) | 129 (37.7) | 331 (45) | < 0.001 |
| Extension | 51 (4.7) | 9 (2.6) | 42 (5.7) | ||
| Abnormal flexion | 60 (5.6) | 10 (2.9) | 50 (6.8) | ||
| Normal flexion | 89 (8.3) | 30 (8.8) | 59 (8) | ||
| Localizes/obeys | 418 (38.8) | 164 (48) | 254 (34.5) | ||
| Not available | 22 | 7 | 15 | ||
| Marshall CT classification, n (%) | 1 | 63 (6.5) | 48 (15.6) | 15 (2.3) | 0.0005 |
| 2 | 416 (42.9) | 167 (54.2) | 249 (37.7) | ||
| 3 | 98 (10.1) | 17 (5.5) | 81 (12.3) | ||
| 4 | 19 (2) | 3 (1) | 16 (2.4) | ||
| 5 | 6 (0.6) | 2 (0.6) | 4 (0.6) | ||
| 6 | 367 (37.9) | 71 (23.1) | 296 (44.8) | ||
| Not available | 131 | 41 | 90 | ||
| Overall PaCO2 (mmHg), mean (SD) | 39.10 (6) | 39.93 (6.8) | 38.72 (5.6) | 0.002 | |
| Lowest PaCO2 (mmHg), mean (SD) | 34.66 (5.98) | 35.92 (6.67) | 34.09 (5.56) | < 0.001 | |
| Highest PaCO2 (mmHg), mean (SD) | 43.68 (8.1) | 44.07 (8.6) | 43,5 (7.86) | 0.287 |
Hypotension was defined as a documented systolic blood pressure < 90 mmHg; hypoxia was defined as a documented partial pressure of oxygen (PaO2) < 8 kPa (60 mmHg), oxygen saturation (SaO2) < 90%, or both; PaCO2 data refer to values at ICU admission
PaCO2 the partial pressure of carbon dioxide, SD standard deviation, Q1–Q3 I and III quartiles, ISS injury severity score, TBI traumatic brain injury, GCS Glasgow Coma Scale, ICPm intracranial pressure monitored, ICU intensive care unit
In the overall population, the mean PaCO2 at ICU admission was 39.1 (± 6) mmHg, and the no-ICPm group had higher PaCO2 mean values compared to the ICPm patients (39.9 ± 6.8 vs 38.7 ± 5.6 mmHg, p < 0.002).
Lowest PaCO2 targets according to centers
Daily minimum PaCO2 distribution during the first week for the whole population, and separated by the centre, are presented in Fig. 1a. The overall mean lowest PaCO2 was 35.2 ± 5.4 mmHg with substantial heterogeneity between centres, whose means ranged from 32.3 (± 3.7) to 38.7 mmHg (± 5.9). This result seems to be related more to different management strategies at the centre level, rather than reflecting national policies (Fig. 1b). For example, among the UK centers (in yellow), two centers had a mean PaCO2 value of 32.3 and 36.4 mmHg.
Only 144 (13%) patients had all PaCO2 measurements between 35 and 45 mmHg, while 588 (53%) patients had at least half of the total PaCO2 measurements in this range. Using MOR to quantify between-centre differences in targeting the suggested PaCO2 range of 35–45 mmHg, we found that, after correction for patient and trauma characteristics, there was a 1.72-fold difference in the odds of having a PaCO2 range of 35–45 mmHg between centres with the highest and lowest rates. After excluding 390 patients with intracranial hypertension, the percentage of patients with all and at least half of the total PaCO2 measurements between 35 and 45 mmHg raised to 19% (111/593) and 64% (380/593), while MOR decreased to 1.4.
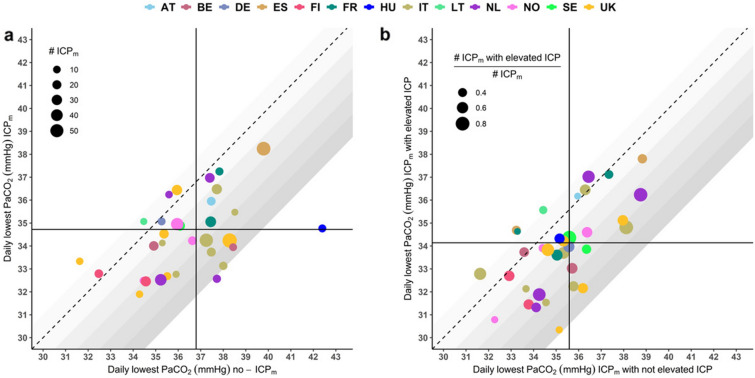
Lowest PaCO2 targets in the presence or not of ICP monitoring
Mean minimum PaCO2 values were significantly lower in ICPm patients compared to no-ICPm (34.7 ± 4.9 mmHg vs 36.8 ± 5.7 mmHg, p < 0.001). Large variability was observed among centers in the management of PaCO2 targets in both subgroups (Fig. 2 and ESM Fig. 2). Some centres showed no differences in target PaCO2 when ICPm was used (i.e. data points near the line of identity in Fig. 2a), but most hospitals tended to adopt lower PaCO2 targets when ICP was monitored (i.e. data points that deviate substantially from the line of identity in Fig. 2a). For example, three centers showed a reduction greater than 4 mmHg in the mean daily lowest PaCO2 when ICP monitoring was available (from 38–38.4 mmHg to 33.1–34.2 mmHg).
Fig. 2.
(a): Scatterplot of the mean daily lowest PaCO2 values in no-ICPm vs ICPm patients in each participating centre (coloured by country). The dashed line represents the line of identity, and a data point on or close to the line indicates that PaCO2 targets in that centre were not affected by the presence of ICP monitoring. The gradient of grey zones on either side of the grey area indicates increasing deviations from this line of identity between values in no-ICPm vs ICPm patients. Each gradation in shade representing one unit change (mmHg). The size of the dots is proportional to the number of ICPm patients at a centre. The outlier centre from Hungary included only two no-ICPm patients, out of a total of 12 patients, with only two measurements each before ending ventilation. (b) Mean of the daily lowest PaCO2 values in ICPm patients with no episodes of elevated ICP (ICP ≤ 20 mmHg) vs ICPm patients with at least one episode of elevated ICP (> 20 mmHg) in each participating centre (coloured by country). The dashed line represents the line of identity, and the size of the dot is proportional to the number of ICPm patients with elevated ICP. PaCO2 the partial pressure of carbon dioxide, AT Austria, BE Belgium, DE Germany, ES Spain, FI Finland, FR France, HU Hungary, IT Italy, LT Lithuania, NL Netherlands, NO Norway, SE Serbia, UK United Kingdom
Lowest PaCO2 in the presence of intracranial hypertension
In the subgroup of patients with ICP monitoring, we also explored the attitude of centres in response to episodes of intracranial hypertension (n = 3646). Some centres showed no differences in target PaCO2 when ICP was elevated (i.e. data points near the line of identity in Fig. 2b), but most hospitals tended to adopt lower PaCO2 targets when ICP was monitored (i.e. data points that deviate substantially from the line of identity in Fig. 2b). The mean minimum PaCO2 was significantly lower in 398 patients with at least one episode of intracranial hypertension compared to the 240 who did not experience increased ICP (34.1 vs 35.6 mmHg, p < 0.001). Within the group of patients with ICP monitoring in place, significant inter-centre differences were observed in the mean lowest PaCO2, both in the absence and presence of intracranial hypertension (ESM Fig. 3).
Profound hyperventilation
An episode of profound HV (PaCO2 < 30 mmHg) was recorded on 727 occasions during the first week of ICU admission in 397 (36%) patients (57% had one, 22% two and 10% three occurrences). Results from the longitudinal mixed-effects model show notable heterogeneity between centres on the use of HV, even after adjusting for patient and trauma characteristics, with a MOR of 2.04 (Fig. 3, ESM Table 1). We found a significant positive association between the occurrence of increased ICP and the use of HV. Among ICPm patients, even after correction for covariates, the odds of HV in a day with elevated ICP was nearly three times that in a day with controlled ICP (OR = 4.34 95% CI = 4.25-4.44, p value < 0.0001 vs OR = 1.47 95% CI = 0.97-2.22, p value = 0.03167). Finally, HV was less applied from day 1 to 7 (OR of HV per day = 0.83; 95% CI = 0.82–0.84, p value < 0.0001).
Fig. 3.
Caterpillar plot of between-centre variation in using profound HV. The figure shows the predicted random intercepts for each centre, on the log-odds scale, along with their 95% prediction intervals. Higher values indicate a higher propensity to use profound HV. A longitudinal random effect logistic model was used to correct for random variation and adjusted for the core IMPACT covariates and elevated ICP. The MOR summarises the between-centre variation: a MOR = 1 indicates no variation, while the larger the MOR is, the larger the variation present. The median odds ratio (MOR = 2.04) refers to the odds of using profound HV between two randomly selected centres for patients with the same covariates and (comparable) random effects
Neuromonitoring
Indirect CBF monitoring, using jugular bulb venous oxygen saturation or brain tissue oxygenation, was not used frequently. No differences were found in their use in patients receiving profoundly HV (jugular bulb venous oxygen saturation, SjvO2: 2.4% vs profound HV 3.5%, p value = 0.380; brain tissue oxygenation, PbtO2: 14.2% vs profound HV 13.9%, p value = 0.937). However, the use of profound HV was associated with significantly higher use of more aggressive treatment, expressed as mean TIL (9.7 vs 6.3 p value < 0.001). In particular, patients who received profound hyperventilation were more likely to have decompressive surgery (8.6 vs 4.8, p value < 0.001) and hyperosmolar therapy (low dose 12.7 vs 5.5, p value < 0.001; high dose 16.8 vs 5.7, p value < 0.001).
6 months mortality and neurological outcome
Overall, of the 1100 patient cohort, 165 died before ICU discharge (15%). Of the 970 patients for whom 6-month outcomes were available, 246 (25.4%) died, and 529 (54.5%) experienced unfavourable functional outcomes (GOSE ≤ 4). The 6 months mortality rate was 29% in patients who had at least one episode of profound HV and 23% in those who did not (p value = 0.045), while the rates of unfavourable GOSE were 64% vs 49% in the two groups, respectively (p value < 0.001). The percentage of patients who received profound HV in the first seven days from admission ranged from 1 to 30% between hospitals. In the IV analysis, the propensity to apply profound HV (defined by the use of PaCO2 < 30 mmHg) did not significantly increase mortality or unfavourable functional outcome, after adjusting for the dose of intracranial hypertension. Patients in hospitals that used 10% more profound HV had 1.06 higher odds of mortality compared to hospitals where profound HV was applied less often (95% CI = 0.77–1.45, p value = 0.7166) and the OR for the same comparison was 1.12 (95% CI = 0.90–1.38, p value = 0.3138) for an unfavourable functional outcome (Table 2).
Table 2.
Results of the logistic mixed-effect model on 6-month outcomes by the instrumental variable approach with complete data (n = 919)
| Outcome | 6-month GOSE | 6-month mortality |
|---|---|---|
| OR (95% CI) p value | OR (95% CI) p value | |
| Centre HV tendency (per 10% change)* | 1.12 (0.9–1.38) 0.3138 | 1.06 (0.77–1.45) 0.7166 |
| Age | 1.04 (1.03–1.05) < 0.0001 | 1.05 (1.04–1.06) < 0.0001 |
| GCS Motor Score | ||
| None | 2.08 (1.46–2.95) < 0.0001 | 2.28 (1.44–3.62) 0.0004 |
| Extension | 5.47 (2.39–12.51) < 0.0001 | 1.82 (0.74–4.48) 0.1886 |
| Abnormal flexion | 3.29 (1.63–6.65) 0.0009 | 1.69 (0.65–4.37) 0.2794 |
| Normal flexion | 1.45 (0.82–2.56) 0.1980 | 1.2 (0.55–2.64) 0.6421 |
| Localizes/obeys | 1 | 1 |
| Pupilar reactivity | ||
| Both reacting | 1 | 1 |
| One reacting | 1.98 (1.14–3.43) 0.0146 | 2.18 (1.16–4.11) 0.0154 |
| Both unreacting | 3.29 (2.05–5.27) < 0.0001 | 6.04 (3.69–9.87) < 0.0001 |
| ICP monitoring | ||
| No | 1 | 1 |
| Yes | 1.79 (1.27–2.51) 0.0008 | 1.00 (0.65–1.54) 0.9948 |
| AUC ICP > 20 (per one SD change)° | 3.72 (1.94–7.15) < 0.0001 | 5.15 (2.86–9.25) < 0.0001 |
OR Odds ratio, CI confidence intervals, SD standard deviation
*Centre HV propensity is calculated as the percentage of daily lowest PaCO2 < 30 mmHg out of all available measures
°Standardized AUC ICP > 20 is the dose of intracranial hypertension calculated as the area under the ICP profile above 20 mmHg
Discussion
The current literature is inconclusive regarding the optimal ventilatory strategy to adopt in patients with TBI and, though there is increasing caution surrounding the use of HV, the translation of expert consensus recommendations into clinical practice remains uncertain. This study examined the PaCO2 management during mechanical ventilation at a centre level in prospectively collected observational data from a large multicentre cohort of TBI patients, focusing on the use of HV.
Our main findings are:
there is substantial practice variation among countries and centers regarding PaCO2 levels and the lowest PaCO2 adopted in TBI patients;
patients who received ICP monitoring were managed at lower PaCO2 compared to patients in whom such monitoring was not used;
patients who did receive ICP monitoring and experienced episodes of increased ICP were managed at lower PaCO2 levels than those who did not have ICP elevations; profound HV was commonly used in such patients;
we observed no association between the risk of mortality or unfavourable functional outcome and more frequent use of profound hyperventilation (PaCO2 < 30 mmHg).
Appropriate management of PaCO2 is a critical requirement in mechanically ventilated patients with TBI, since carbon dioxide is one of the major determinants of cerebral vascular physiology, and therefore cerebral blood flow and volume. The effect of the interplay between carbon dioxide and perfusion pressure on the cerebral circulation results in a sophisticated modulation of cerebrovascular resistance and tone, with hypercapnia causing cerebral vasodilation, and hypocapnia, vasoconstriction.
The only randomized controlled trial [22] addressing the benefit of prophylactic hyperventilation was conducted thirty years ago, and randomised TBI patients into three categories: control (n = 41), hyperventilation (n = 36), and HV + tromethamine (an H+ acceptor used to treat metabolic acidosis; n = 36). This setting is different from the current context, as the putatively normoventilated controls had PaCO2 values in the hypocapnic range (35 mmHg), and the HV utilized was profound (PaCO2 25 mmHg). These discordances with current practice, the limited number of patients, and the low incidence of episodes of intracranial hypertension make the results difficult to interpret.
A recent consensus still recommends targeting a normal range of PaCO2 values in the absence of increased ICP [12]. However, in the case of increased ICP, no agreement was achieved regarding the role of HV, providing evidence of the current uncertainty in this area [12]. Although induced hypocapnia is considered an efficient second line measure to reduce ICP, clinicians remain worried about potential cerebral ischemic complications of hyperventilation [8, 23]. Coles et al. used positron emission tomography in a cohort of 30 patients to show that the acute application of HV resulted in a reduction of cerebral blood flow and an increase in oxygen extraction fraction and the ischemic brain volume [23]. These results have left an indelible imprint on the way HV is perceived by intensivists, but they do not represent a randomized trial. Other authors suggest that mild HV may reduce ICP without leading to pathological changes of brain metabolism and oxygenation measured through cerebral microdialysis and PbtO2 [24] or energy failure. Moreover, Diringer et al. demonstrated that HV reduces global cerebral blood flow while increased oxygen extraction fraction leaving cerebral metabolic rate for oxygen unchanged, concluding that it is unlikely that HV causes neurological injury [25, 26].
Although some concerns still exist, PaCO2 reduction is still widely used in the clinical setting for ICP control. The most common PaCO2 target declared by clinicians in the absence of intracranial hypertension (35–40 mmHg) is higher than in the case of raised ICP (30–35 mmHg) [9]. Similarly, in a retrospective study of 151 patients with TBI, the PaCO2 target adopted in clinically stable ICP was 36 ± 5.7 mmHg, whereas in the case of increased ICP it was 34 ± 5.4 mmHg [27]. Besides, a recent consensus on ICP treatment suggested considering HV to PaCO2 of 30–32 mmHg when ICP is elevated in patients not responding to Tier 1 and 2 treatment [13].
Our data document a divergence between suggestions from literature and practice: nearly half of the daily lowest PaCO2 measurements in the first week were < 35 mmHg. Moreover, in presence of ICP monitoring, clinicians use a lower target of PaCO2. However, we also saw wide variability in PaCO2 levels between centres, both in terms of the overall values, and the lowest levels of PaCO2 observed. These differences were seen not just across the whole study cohort, but also in subgroups of patients with and without ICP monitoring, and those with and without episodes of intracranial hypertension in the first week. HV in presence of high ICP was frequently used, particularly in the first few days after admission, and was often combined with other ICP-lowering therapies such as osmotic agents and decompressive craniectomy. Interestingly, centres that used HV more frequently were not more likely to routinely apply more advanced neuromonitoring techniques for early detection of impaired cerebral blood flow and cerebral oxygen availability.
There is no strong evidence regarding the possible benefits or harms of profound HV on patient outcomes. However, a single retrospective analysis of 251 brain-injured patients [28] reported that, when compared to controls, patients who underwent prolonged HV (PaCO2: 25–30 mmHg; mean duration = 10, min–max = 5–41 h) experienced lower mortality (9.8 vs. 32.8%) but a higher rate of poor functional outcome.
We found that being treated in a centre where profound hypocapnia is more frequently used compared to centers where it is rarely used was not significantly associated with a higher rate of mortality or poor functional outcome.
In summary, our results suggest that moderate HV is widely used in severely brain-injured patients, especially when ICP is monitored, and in case of elevated ICP.
Limitations
Although our results may provide useful context with an important clinical message for physicians, we believe they should be interpreted with caution for several reasons. First, 6 months GOSE and mortality are influenced by several other factors, such as systemic and ICU complications, as well as post-ICU events. Therefore, based on observational data, it is speculative to draw a direct causal relationship between PaCO2 and outcome: further randomized controlled studies are needed to assess the effect of PaCO2 more precisely and in particular HV, on the outcome. Second, this is an analysis of data from a large study, which primarily addressed the epidemiology, clinical care and outcome of TBI. However, as respiratory management was not a primary focus of the study, more specific data on ventilatory management of these patients are missing, and hence unavailable to strengthen our analysis. Data on the incidence and timing of pulmonary complications such as acute respiratory distress respiratory syndrome and ventilator-associated pneumonia, the use of ventilatory strategies used to manipulate PaCO2, and the ventilator settings used in our study population are unavailable. Third, the outcome was evaluated at 6 months, which can be considered as an early measurement of outcome after TBI, and further long-term evaluations would have been desirable. Fourth, we did not specifically take into consideration the temperature management of the patients, which can importantly affect PaCO2 values. However, the measurements of PaCO2 are automatically corrected for temperature from the arterial blood gases machines, and we aimed to assess the targets of PaCO2 achieved, regardless of the effects of different factors on its final value.
Finally, in our dataset only the daily lowest and highest PaCO2 values were collected, thus missing possible changes in PaCO2 and pulmonary function parameters that may occur suddenly and repeatedly during the day. However, our analysis includes data on daily PaCO2, thus providing a longitudinal view of PaCO2 management over time.
Conclusions
In a large cohort of mechanically ventilated TBI patients, we found substantial between-centre variations in PaCO2, but with a large proportion of patients being managed at PaCO2 levels below those suggested by expert consensus statements. On average, patients who had ICP monitors in place had significantly lower PaCO2 levels than those that did not, and amongst ICP monitored patients, PaCO2 levels were lower in patients who had episodes of intracranial hypertension—suggesting that HV is still used for ICP management. Profound hyperventilation (PaCO2 < 30 mmHg) was not uncommon. However, a centre that had a greater propensity to use profound HV did not worsen 6-month mortality or functional outcome. Notwithstanding this, we believe that the available evidence still makes the case for caution in the use of HV, with careful consideration of risks and benefits on a case-by-case basis. Our data provide no basis for dismissing continuing concerns regarding prophylactic or profound hyperventilation. We need randomized controlled trials and high-level evidence guidelines to support rational choices regarding optimal ventilation management and PaCO2 targets in patients with TBI.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge the CENTER-TBI ICU Participants and Investigators listed here as non-authors contributors: Cecilia Åkerlund1, Krisztina Amrein2, Nada Andelic3, Lasse Andreassen4, Audny Anke5, Anna Antoni6, Gérard Audibert7, Philippe Azouvi8, Maria Luisa Azzolini9, Ronald Bartels10, Pál Barzó11, Romuald Beauvais12, Ronny Beer13, Bo-Michael Bellander14, Antonio Belli15, Habib Benali16, Maurizio Berardino17, Luigi Beretta9, Morten Blaabjerg18, Peter Bragge19, Alexandra Brazinova20, Vibeke Brinck21, Joanne Brooker22, Camilla Brorsson23, Andras Buki24, Monika Bullinger25, Manuel Cabeleira26, Alessio Caccioppola27, Emiliana Calappi 27, Maria Rosa Calvi9, Peter Cameron28, Guillermo Carbayo Lozano29, Marco Carbonara27, Simona Cavallo17, Giorgio Chevallard30, Arturo Chieregato30, Giuseppe Citerio31, 32, Hans Clusmann33, Mark Coburn34, Jonathan Coles35, Jamie D. Cooper36, Marta Correia37, Amra Čović 38, Nicola Curry39, Endre Czeiter24, Marek Czosnyka26, Claire Dahyot-Fizelier40, Paul Dark41, Helen Dawes42, Véronique De Keyser43, Vincent Degos16, Francesco Della Corte44, Hugo den Boogert10, Bart Depreitere45, Đula Đilvesi 46, Abhishek Dixit47, Emma Donoghue22, Jens Dreier48, Guy-Loup Dulière49, Ari Ercole47, Patrick Esser42, Erzsébet Ezer50, Martin Fabricius51, Valery L. Feigin52, Kelly Foks53, Shirin Frisvold54, Alex Furmanov55, Pablo Gagliardo56, Damien Galanaud16, Dashiell Gantner28, Guoyi Gao57, Pradeep George58, Alexandre Ghuysen59, Lelde Giga60, Ben Glocker61, Jagoš Golubovic46, Pedro A. Gomez 62, Johannes Gratz63, Benjamin Gravesteijn64, Francesca Grossi44, Russell L. Gruen65, Deepak Gupta66, Juanita A. Haagsma64, Iain Haitsma67, Raimund Helbok13, Eirik Helseth68, Lindsay Horton 69, Jilske Huijben64, Peter J. Hutchinson70, Bram Jacobs71, Stefan Jankowski72, Mike Jarrett21, Ji-yao Jiang58, Faye Johnson73, Kelly Jones52, Mladen Karan46, Angelos G. Kolias70, Erwin Kompanje74, Daniel Kondziella51, Evgenios Kornaropoulos47, Lars-Owe Koskinen75, Noémi Kovács76, Ana Kowark77, Alfonso Lagares62, Linda Lanyon58, Steven Laureys78, Fiona Lecky79, 80, Didier Ledoux78, Rolf Lefering81, Valerie Legrand82, Aurelie Lejeune83, Leon Levi84, Roger Lightfoot85, Hester Lingsma64, Andrew I.R. Maas43, Ana M. Castaño-León62, Marc Maegele86, Marek Majdan20, Alex Manara87, Geoffrey Manley88, Costanza Martino89, Hugues Maréchal49, Julia Mattern90, Catherine McMahon91, Béla Melegh92, David Menon47, Tomas Menovsky43, Ana Mikolic64, Benoit Misset78, Visakh Muraleedharan58, Lynnette Murray28, Ancuta Negru93, David Nelson1, Virginia Newcombe47, Daan Nieboer64, József Nyirádi2, Otesile Olubukola79, Matej Oresic94, Fabrizio Ortolano27, Aarno Palotie95, 96, 97, Paul M. Parizel98, Jean-François Payen99, Natascha Perera12, Vincent Perlbarg16, Paolo Persona100, Wilco Peul101, Anna Piippo-Karjalainen102, Matti Pirinen95, Dana Pisica64, Horia Ples93, Suzanne Polinder64, Inigo Pomposo29, Jussi P. Posti 103, Louis Puybasset104, Andreea Radoi 105, Arminas Ragauskas106, Rahul Raj102, Malinka Rambadagalla107, Isabel Retel Helmrich64, Jonathan Rhodes108, Sylvia Richardson109, Sophie Richter47, Samuli Ripatti95, Saulius Rocka106, Cecilie Roe110, Olav Roise111,112, Jonathan Rosand113, Jeffrey V. Rosenfeld114, Christina Rosenlund115, Guy Rosenthal55, Rolf Rossaint77, Sandra Rossi100, Daniel Rueckert61 Martin Rusnák116, Juan Sahuquillo105, Oliver Sakowitz90, 117, Renan Sanchez-Porras117, Janos Sandor118, Nadine Schäfer81, Silke Schmidt119, Herbert Schoechl120, Guus Schoonman121, Rico Frederik Schou122, Elisabeth Schwendenwein6, Charlie Sewalt64, Toril Skandsen123, 124 , Peter Smielewski26, Abayomi Sorinola125, Emmanuel Stamatakis47, Simon Stanworth39, Robert Stevens126, William Stewart127, Ewout W. Steyerberg64, 128, Nino Stocchetti129, Nina Sundström130, Riikka Takala131, Viktória Tamás125, Tomas Tamosuitis132, Mark Steven Taylor20, Braden Te Ao52, Olli Tenovuo103, Alice Theadom52, Matt Thomas87, Dick Tibboel133, Marjolein Timmers74, Christos Tolias134, Tony Trapani28, Cristina Maria Tudora93, Andreas Unterberg90, Peter Vajkoczy 135, Shirley Vallance28, Egils Valeinis60, Zoltán Vámos50, Mathieu van der Jagt136, Gregory Van der Steen43, Joukje van der Naalt71, Jeroen T.J.M. van Dijck 101, Thomas A. van Essen101, Wim Van Hecke137, Caroline van Heugten138, Dominique Van Praag139, Ernest van Veen64, Thijs Vande Vyvere137, Roel P. J. van Wijk101, Alessia Vargiolu32, Emmanuel Vega83, Kimberley Velt64, Jan Verheyden137, Paul M. Vespa140, Anne Vik123, 141, Rimantas Vilcinis132, Victor Volovici67, Nicole von Steinbüchel38, Daphne Voormolen64, Petar Vulekovic46, Kevin K.W. Wang142, Eveline Wiegers64, Guy Williams47, Lindsay Wilson69, Stefan Winzeck47, Stefan Wolf143, Zhihui Yang113, Peter Ylén144, Alexander Younsi90, Frederick A. Zeiler47,145, Veronika Zelinkova20, Agate Ziverte60, Tommaso Zoerle27
1Department of Physiology and Pharmacology, Section of Perioperative Medicine and Intensive Care, Karolinska Institutet, Stockholm, Sweden
2János Szentágothai Research Centre, University of Pécs, Pécs, Hungary
3Division of Surgery and Clinical Neuroscience, Department of Physical Medicine and Rehabilitation, Oslo University Hospital and University of Oslo, Oslo, Norway
4Department of Neurosurgery, University Hospital Northern Norway, Tromso, Norway
5Department of Physical Medicine and Rehabilitation, University Hospital Northern Norway, Tromso, Norway
6Trauma Surgery, Medical University Vienna, Vienna, Austria
7Department of Anesthesiology & Intensive Care, University Hospital Nancy, Nancy, France
8Raymond Poincare hospital, Assistance Publique – Hopitaux de Paris, Paris, France
9Department of Anesthesiology & Intensive Care, S Raffaele University Hospital, Milan, Italy
10Department of Neurosurgery, Radboud University Medical Center, Nijmegen, The Netherlands
11Department of Neurosurgery, University of Szeged, Szeged, Hungary
12International Projects Management, ARTTIC, Munchen, Germany
13Department of Neurology, Neurological Intensive Care Unit, Medical University of Innsbruck, Innsbruck, Austria
14Department of Neurosurgery & Anesthesia & intensive care medicine, Karolinska University Hospital, Stockholm, Sweden
15NIHR Surgical Reconstruction and Microbiology Research Centre, Birmingham, UK
16Anesthesie-Réanimation, Assistance Publique – Hopitaux de Paris, Paris, France
17Department of Anesthesia & ICU, AOU Città della Salute e della Scienza di Torino—Orthopedic and Trauma Center, Torino, Italy
18Department of Neurology, Odense University Hospital, Odense, Denmark
19BehaviourWorks Australia, Monash Sustainability Institute, Monash University, Victoria, Australia
20Department of Public Health, Faculty of Health Sciences and Social Work, Trnava University, Trnava, Slovakia
21Quesgen Systems Inc., Burlingame, California, USA
22Australian & New Zealand Intensive Care Research Centre, Department of Epidemiology and Preventive Medicine, School of Public Health and Preventive Medicine, Monash University, Melbourne, Australia
23Department of Surgery and Perioperative Science, Umeå University, Umeå, Sweden
24Department of Neurosurgery, Medical School, University of Pécs, Hungary and Neurotrauma Research Group, János Szentágothai Research Centre, University of Pécs, Hungary
25Department of Medical Psychology, Universitätsklinikum Hamburg-Eppendorf, Hamburg, Germany
26Brain Physics Lab, Division of Neurosurgery, Dept of Clinical Neurosciences, University of Cambridge, Addenbrooke’s Hospital, Cambridge, UK
27Neuro ICU, Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milan, Italy
28ANZIC Research Centre, Monash University, Department of Epidemiology and Preventive Medicine, Melbourne, Victoria, Australia
29Department of Neurosurgery, Hospital of Cruces, Bilbao, Spain
30NeuroIntensive Care, Niguarda Hospital, Milan, Italy
31School of Medicine and Surgery, Università Milano Bicocca, Milano, Italy
32NeuroIntensive Care, ASST di Monza, Monza, Italy
33Department of Neurosurgery, Medical Faculty RWTH Aachen University, Aachen, Germany
34Department of Anesthesiology and Intensive Care Medicine, University Hospital Bonn, Bonn, Germany
35Department of Anesthesia & Neurointensive Care, Cambridge University Hospital NHS Foundation Trust, Cambridge, UK
36School of Public Health & PM, Monash University and The Alfred Hospital, Melbourne, Victoria, Australia
37Radiology/MRI department, MRC Cognition and Brain Sciences Unit, Cambridge, UK
38Institute of Medical Psychology and Medical Sociology, Universitätsmedizin Göttingen, Göttingen, Germany
39Oxford University Hospitals NHS Trust, Oxford, UK
40Intensive Care Unit, CHU Poitiers, Potiers, France
41University of Manchester NIHR Biomedical Research Centre, Critical Care Directorate, Salford Royal Hospital NHS Foundation Trust, Salford, UK
42Movement Science Group, Faculty of Health and Life Sciences, Oxford Brookes University, Oxford, UK
43Department of Neurosurgery, Antwerp University Hospital and University of Antwerp, Edegem, Belgium
44Department of Anesthesia & Intensive Care, Maggiore Della Carità Hospital, Novara, Italy
45Department of Neurosurgery, University Hospitals Leuven, Leuven, Belgium
46Department of Neurosurgery, Clinical centre of Vojvodina, Faculty of Medicine, University of Novi Sad, Novi Sad, Serbia
47Division of Anaesthesia, University of Cambridge, Addenbrooke’s Hospital, Cambridge, UK
48Center for Stroke Research Berlin, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Berlin, Germany
49Intensive Care Unit, CHR Citadelle, Liège, Belgium
50Department of Anaesthesiology and Intensive Therapy, University of Pécs, Pécs, Hungary
51Departments of Neurology, Clinical Neurophysiology and Neuroanesthesiology, Region Hovedstaden Rigshospitalet, Copenhagen, Denmark
52National Institute for Stroke and Applied Neurosciences, Faculty of Health and Environmental Studies, Auckland University of Technology, Auckland, New Zealand
53Department of Neurology, Erasmus MC, Rotterdam, the Netherlands
54Department of Anesthesiology and Intensive care, University Hospital Northern Norway, Tromso, Norway
55Department of Neurosurgery, Hadassah-hebrew University Medical center, Jerusalem, Israel
56Fundación Instituto Valenciano de Neurorrehabilitación (FIVAN), Valencia, Spain
57Department of Neurosurgery, Shanghai Renji hospital, Shanghai Jiaotong University/school of medicine, Shanghai, China
58Karolinska Institutet, INCF International Neuroinformatics Coordinating Facility, Stockholm, Sweden
59Emergency Department, CHU, Liège, Belgium
60Neurosurgery clinic, Pauls Stradins Clinical University Hospital, Riga, Latvia
61Department of Computing, Imperial College London, London, UK
62Department of Neurosurgery, Hospital Universitario 12 de Octubre, Madrid, Spain
63Department of Anesthesia, Critical Care and Pain Medicine, Medical University of Vienna, Austria
64Department of Public Health, Erasmus Medical Center-University Medical Center, Rotterdam, The Netherlands
65College of Health and Medicine, Australian National University, Canberra, Australia
66Department of Neurosurgery, Neurosciences Centre & JPN Apex trauma centre, All India Institute of Medical Sciences, New Delhi-110029, India
67Department of Neurosurgery, Erasmus MC, Rotterdam, the Netherlands
68Department of Neurosurgery, Oslo University Hospital, Oslo, Norway
69Division of Psychology, University of Stirling, Stirling, UK
70Division of Neurosurgery, Department of Clinical Neurosciences, Addenbrooke’s Hospital & University of Cambridge, Cambridge, UK
71Department of Neurology, University of Groningen, University Medical Center Groningen, Groningen, Netherlands
72Neurointensive Care , Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK
73Salford Royal Hospital NHS Foundation Trust Acute Research Delivery Team, Salford, UK
74Department of Intensive Care and Department of Ethics and Philosophy of Medicine, Erasmus Medical Center, Rotterdam, The Netherlands
75Department of Clinical Neuroscience, Neurosurgery, Umeå University, Umeå, Sweden
76Hungarian Brain Research Program—Grant No. KTIA_13_NAP-A-II/8, University of Pécs, Pécs, Hungary
77Department of Anaesthesiology, University Hospital of Aachen, Aachen, Germany
78Cyclotron Research Center , University of Liège, Liège, Belgium
79Centre for Urgent and Emergency Care Research (CURE), Health Services Research Section, School of Health and Related Research (ScHARR), University of Sheffield, Sheffield, UK
80Emergency Department, Salford Royal Hospital, Salford UK
81Institute of Research in Operative Medicine (IFOM), Witten/Herdecke University, Cologne, Germany
82VP Global Project Management CNS, ICON, Paris, France
83Department of Anesthesiology-Intensive Care, Lille University Hospital, Lille, France
84Department of Neurosurgery, Rambam Medical Center, Haifa, Israel
85Department of Anesthesiology & Intensive Care, University Hospitals Southhampton NHS Trust, Southhampton, UK
86Cologne-Merheim Medical Center (CMMC), Department of Traumatology, Orthopedic Surgery and Sportmedicine, Witten/Herdecke University, Cologne, Germany
87Intensive Care Unit, Southmead Hospital, Bristol, Bristol, UK
88Department of Neurological Surgery, University of California, San Francisco, California, USA
89Department of Anesthesia & Intensive Care,M. Bufalini Hospital, Cesena, Italy
90Department of Neurosurgery, University Hospital Heidelberg, Heidelberg, Germany
91Department of Neurosurgery, The Walton centre NHS Foundation Trust, Liverpool, UK
92Department of Medical Genetics, University of Pécs, Pécs, Hungary
93Department of Neurosurgery, Emergency County Hospital Timisoara , Timisoara, Romania
94School of Medical Sciences, Örebro University, Örebro, Sweden
95Institute for Molecular Medicine Finland, University of Helsinki, Helsinki, Finland
96Analytic and Translational Genetics Unit, Department of Medicine; Psychiatric & Neurodevelopmental Genetics Unit, Department of Psychiatry; Department of Neurology, Massachusetts General Hospital, Boston, MA, USA
97Program in Medical and Population Genetics; The Stanley Center for Psychiatric Research, The Broad Institute of MIT and Harvard, Cambridge, MA, USA
98Department of Radiology, University of Antwerp, Edegem, Belgium
99Department of Anesthesiology & Intensive Care, University Hospital of Grenoble, Grenoble, France
100Department of Anesthesia & Intensive Care, Azienda Ospedaliera Università di Padova, Padova, Italy
101Dept. of Neurosurgery, Leiden University Medical Center, Leiden, The Netherlands and Dept. of Neurosurgery, Medical Center Haaglanden, The Hague, The Netherlands
102Department of Neurosurgery, Helsinki University Central Hospital
103Division of Clinical Neurosciences, Department of Neurosurgery and Turku Brain Injury Centre, Turku University Hospital and University of Turku, Turku, Finland
104Department of Anesthesiology and Critical Care, Pitié -Salpêtrière Teaching Hospital, Assistance Publique, Hôpitaux de Paris and University Pierre et Marie Curie, Paris, France
105Neurotraumatology and Neurosurgery Research Unit (UNINN), Vall d'Hebron Research Institute, Barcelona, Spain
106Department of Neurosurgery, Kaunas University of technology and Vilnius University, Vilnius, Lithuania
107Department of Neurosurgery, Rezekne Hospital, Latvia
108Department of Anaesthesia, Critical Care & Pain Medicine NHS Lothian & University of Edinburg, Edinburgh, UK
109Director, MRC Biostatistics Unit, Cambridge Institute of Public Health, Cambridge, UK
110Department of Physical Medicine and Rehabilitation, Oslo University Hospital/University of Oslo, Oslo, Norway
111Division of Orthopedics, Oslo University Hospital, Oslo, Norway
112Institue of Clinical Medicine, Faculty of Medicine, University of Oslo, Oslo, Norway
113Broad Institute, Cambridge MA Harvard Medical School, Boston MA, Massachusetts General Hospital, Boston MA, USA
114National Trauma Research Institute, The Alfred Hospital, Monash University, Melbourne, Victoria, Australia
115Department of Neurosurgery, Odense University Hospital, Odense, Denmark
116International Neurotrauma Research Organisation, Vienna, Austria
117Klinik für Neurochirurgie, Klinikum Ludwigsburg, Ludwigsburg, Germany
118Division of Biostatistics and Epidemiology, Department of Preventive Medicine, University of Debrecen, Debrecen, Hungary
119Department Health and Prevention, University Greifswald, Greifswald, Germany
120Department of Anaesthesiology and Intensive Care, AUVA Trauma Hospital, Salzburg, Austria
121Department of Neurology, Elisabeth-TweeSteden Ziekenhuis, Tilburg, the Netherlands
122Department of Neuroanesthesia and Neurointensive Care, Odense University Hospital, Odense, Denmark
123Department of Neuromedicine and Movement Science, Norwegian University of Science and Technology, NTNU, Trondheim, Norway
124Department of Physical Medicine and Rehabilitation, St.Olavs Hospital, Trondheim University Hospital, Trondheim, Norway
125Department of Neurosurgery, University of Pécs, Pécs, Hungary
126Division of Neuroscience Critical Care, John Hopkins University School of Medicine, Baltimore, USA
127Department of Neuropathology, Queen Elizabeth University Hospital and University of Glasgow, Glasgow, UK
128Dept. of Department of Biomedical Data Sciences, Leiden University Medical Center, Leiden, The Netherlands
129Department of Pathophysiology and Transplantation, Milan University, and Neuroscience ICU, Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milano, Italy
130Department of Radiation Sciences, Biomedical Engineering, Umeå University, Umeå, Sweden
131Perioperative Services, Intensive Care Medicine and Pain Management, Turku University Hospital and University of Turku, Turku, Finland
132Department of Neurosurgery, Kaunas University of Health Sciences, Kaunas, Lithuania
133Intensive Care and Department of Pediatric Surgery, Erasmus Medical Center, Sophia Children’s Hospital, Rotterdam, The Netherlands
134Department of Neurosurgery, Kings college London, London, UK
135Neurologie, Neurochirurgie und Psychiatrie, Charité – Universitätsmedizin Berlin, Berlin, Germany
136Department of Intensive Care Adults, Erasmus MC– University Medical Center Rotterdam, Rotterdam, the Netherlands
137icoMetrix NV, Leuven, Belgium
138Movement Science Group, Faculty of Health and Life Sciences, Oxford Brookes University, Oxford, UK
139Psychology Department, Antwerp University Hospital, Edegem, Belgium
140Director of Neurocritical Care, University of California, Los Angeles, USA
141Department of Neurosurgery, St.Olavs Hospital, Trondheim University Hospital, Trondheim, Norway
142Department of Emergency Medicine, University of Florida, Gainesville, Florida, USA
143Department of Neurosurgery, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Berlin, Germany
144VTT Technical Research Centre, Tampere, Finland
145Section of Neurosurgery, Department of Surgery, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada
Abbreviations
- AUC CO2i
Area below the value of 30 mmHg as a benchmark and the interpolation of the PaCO2 profile in time
- AUC ICP > 20
Area under ICP profile above 20 mmHg
- CBF
Cerebral blood flow
- CENTER-TBI
Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury
- CI
Confidence interval
- CO2
Carbon dioxide
- CT
Computed tomography
- ESM
Electronic supplementary material
- GCS
Glasgow coma scale
- GOSE
Glasgow outcome scale extended
- HP
Hypocapnia
- HR
Hazard rate
- HV
Hyperventilation
- ICP
Intracranial pressure
- ICPm
ICP monitored
- No-ICPm
No-ICP monitored
- ICU
Intensive care unit
- ISS
Injury severity score
- LOS
Length of stay
- MOR
Median odds ratio
- OR
Odds ratio
- PaCO2
Partial pressure of carbon dioxide
- PbtO2
Brain tissue oxygenation
- SaO2
Oxygen saturation
- SjvO2
Jugular bulb venous oxygen saturation
- SD
Standard deviation
- STROBE
Strengthening the Reporting of Observational Studies in Epidemiology
- TBI
Traumatic brain injury
- TIL
Therapy intensity level
Author contributions
GC conceived and supervised the project, participated in the data analysis, revised the first version of the manuscript the manuscript, and the supplementary tables. CR participated in the data analysis, drafted the manuscript, the supplementary tables and collected the COIs. SG, MP, and PR analysed the data, drafted the manuscript, and the supplementary material. LM, ER, DKM, and NS were an active part of the manuscript drafting and revision. GC, CR, SG, MP, PR have verified the underlying data. DKM was one of the two coordinators of the CENTER-TBI study, and GC and NS were Work Package leaders. GC, CR, SG and DKM discussed the findings with all the authors. All co-authors gave substantial feedback on the manuscript and approved the final version of it.
Funding
Open access funding provided by Università degli Studi di Milano - Bicocca within the CRUI-CARE Agreement. The Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI study, registered at clinicaltrials.gov NCT02210221) was funded by the FW7 program of the European Union (602150). Additional funding was obtained from the Hannelore Kohl Stiftung (Germany), from OneMind (USA) and Integra LifeSciences Corporation (USA). The funder had no role in the design of the study, the collection, analysis, and interpretation of data, or in writing the manuscript.
Declarations
Conflict of interest
GC reports grants, personal fees as Speakers’ Bureau Member and Advisory Board Member from Integra and Neuroptics. DKM reports grants from the European Union and UK National Institute for Health Research, during the conduct of the study; grants, personal fees, and non-financial support from GlaxoSmithKline; personal fees from Neurotrauma Sciences, Lantmaanen AB, Pressura, and Pfizer, outside of the submitted work. The other authors declare that they have no competing interests.
Ethics approval and consent to participate
The Medical Ethics Committees of all participating centers approved the CENTER-TBI study, and informed consent was obtained according to local regulations. (https://www.center-tbi.eu/project/ethical-approval).
Footnotes
CENTER-TBI ICU participants and investigators are listed as non-author contributors in the Acknowledgement section.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Giuseppe Citerio and Chiara Robba equally contributed as first authors to this work. Stefania Galimberti and David K. Menon equally contributed as last authors to this work.
References
- 1.Hoiland RL, Fisher JA, Ainslie PN (2019) Regulation of the Cerebral Circulation by Arterial Carbon Dioxide. In: Compr. Physiol. Wiley. 10.1002/cphy.c180021 [DOI] [PubMed]
- 2.Gouvea Bogossian E, Peluso L, Creteur J, Taccone FS (2021) Hyperventilation in Adult TBI Patients: How to Approach It? Neurol Front. 10.3389/fneur.2020.580859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lundberg N, Kjallquist A, Bien C (1949) Reduction of increased intracranial pressure by hyperventilation. A therapeutic aid in neurological surgery, Acta Psychiatr. Scand. Suppl. 34:1–64. http://www.ncbi.nlm.nih.gov/pubmed/14418913. [PubMed]
- 4.Godoy DA, Seifi A, Garza D, Lubillo-Montenegro S, Murillo-Cabezas F (2017) Hyperventilation Therapy for Control of Posttraumatic Intracranial Hypertension. Front Neurol. 10.3389/fneur.2017.00250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stocchetti N, Maas AIR, Chieregato A, van der Plas AA (2005) Hyperventilation in Head Injury. Chest 127:1812–1827. 10.1378/chest.127.5.1812 [DOI] [PubMed] [Google Scholar]
- 6.Stocchetti N, Carbonara M, Citerio G, Ercole A, Skrifvars MB, Smielewski P, Zoerle T, Menon DK (2017) Severe traumatic brain injury: targeted management in the intensive care unit. Lancet Neurol 16:452–464. 10.1016/S1474-4422(17)30118-7 [DOI] [PubMed] [Google Scholar]
- 7.Coles JP, Minhas PS, Fryer TD, Smielewski P, Aigbirihio F, Donovan T, Downey SPMJ, Williams G, Chatfield D, Matthews JC, Gupta AK, Carpenter TA, Clark JC, Pickard JD, Menon DK (2002) Effect of hyperventilation on cerebral blood flow in traumatic head injury: clinical relevance and monitoring correlates*. Crit Care Med 30:1950–1959. 10.1097/00003246-200209000-00002 [DOI] [PubMed] [Google Scholar]
- 8.Curley G, Kavanagh BP, Laffey JG (2010) Hypocapnia and the injured brain: More harm than benefit. Crit Care Med 38:1348–1359. 10.1097/CCM.0b013e3181d8cf2b [DOI] [PubMed] [Google Scholar]
- 9.Cnossen MC, Huijben JA, van der Jagt M, Volovici V, van Essen T, Polinder S, Nelson D, Ercole A, Stocchetti N, Citerio G, Peul WC, Maas AIR, Menon D, Steyerberg EW, Lingsma HF (2017) Variation in monitoring and treatment policies for intracranial hypertension in traumatic brain injury: a survey in 66 neurotrauma centers participating in the CENTER-TBI study. Crit Care 21:233. 10.1186/s13054-017-1816-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.N Carney, AM Totten, C OReilly, JS Ullman, GWJ Hawryluk, MJ Bell, SL Bratton, R Chesnut, OA Harris, N Kissoon, AM Rubiano, L Shutter, RC Tasker, MS Vavilala, J Wilberger, DW Wright, J Ghajar (2017) Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery. 10.1227/NEU.0000000000001432. [DOI] [PubMed]
- 11.Roberts I, Schierhout G (1997) Hyperventilation therapy for acute traumatic brain injury. Cochrane Database Syst Rev. 10.1002/14651858.CD000566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robba C, Poole D, McNett M, Asehnoune K, Bösel J, Bruder N, Chieregato A, Cinotti R, Duranteau J, Einav S, Ercole A, Ferguson N, Guerin C, Siempos II, Kurtz P, Juffermans NP, Mancebo J, Mascia L, McCredie V, Nin N, Oddo M, Pelosi P, Rabinstein AA, Neto AS, Seder DB, Skrifvars MB, Suarez JI, Taccone FS, van der Jagt M, Citerio G, Stevens RD (2020) Mechanical ventilation in patients with acute brain injury: recommendations of the European Society of Intensive Care Medicine consensus. Intensive Care Med. 10.1007/s00134-020-06283-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hawryluk GWJ, Aguilera S, Buki A, Bulger E, Citerio G, Cooper DJ, Arrastia RD, Diringer M, Figaji A, Gao G, Geocadin R, Ghajar J, Harris O, Hoffer A, Hutchinson P, Joseph M, Kitagawa R, Manley G, Mayer S, Menon DK, Meyfroidt G, Michael DB, Oddo M, Okonkwo D, Patel M, Robertson C, Rosenfeld JV, Rubiano AM, Sahuquillo J, Servadei F, Shutter L, Stein D, Stocchetti N, Taccone FS, Timmons S, Tsai E, Ullman JS, Vespa P, Videtta W, Wright DW, Zammit C, Chesnut RM (2019) A management algorithm for patients with intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med. 10.1007/s00134-019-05805-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maas AIR, Menon DK, Steyerberg EW, Citerio G, Lecky F, Manley GT, Hill S, Legrand V, Sorgner A (2015) Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI). Neurosurgery. 10.1227/NEU.0000000000000575 [DOI] [PubMed] [Google Scholar]
- 15.Steyerberg EW, Wiegers E, Sewalt C, et al (2019) Case-mix, care pathways, and outcomes in patients with traumatic brain injury in CENTER-TBI: a European prospective, multicentre, longitudinal, cohort study. Lancet Neurol. 10.1016/S1474-4422(19)30232-7 [DOI] [PubMed] [Google Scholar]
- 16.Huijben JA, Wiegers EJA, Lingsma HF, Citerio G, Maas AIR, Menon DK, Ercole A, Nelson D, van der Jagt M, Steyerberg EW, Helbok R, Lecky F, Peul W, Birg T, Zoerle T, Carbonara M, Stocchetti N (2020) Changing care pathways and between-center practice variations in intensive care for traumatic brain injury across Europe: a CENTER-TBI analysis. Intensive Care Med 46:995–1004. 10.1007/s00134-020-05965-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huijben JA, Dixit A, Stocchetti N, Maas AIR, Lingsma HF, van der Jagt M, Nelson D, Citerio G, Wilson L, Menon DK, Ercole A (2021) Use and impact of high intensity treatments in patients with traumatic brain injury across Europe: a CENTER-TBI analysis. Crit Care 25:78. 10.1186/s13054-020-03370-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson JTL, Pettigrew LEL, Teasdale GM (1998) Structured Interviews for the Glasgow Outcome Scale and the Extended Glasgow Outcome Scale: Guidelines for Their Use. J Neurotrauma. 10.1089/neu.1998.15.573 [DOI] [PubMed] [Google Scholar]
- 19.Maas AIR, Marmarou A, Murray GD, Teasdale SGM, Steyerberg EW (2007) Prognosis and Clinical Trial Design in Traumatic Brain Injury: The IMPACT Study. J Neurotrauma 24:232–238. 10.1089/neu.2006.0024 [DOI] [PubMed] [Google Scholar]
- 20.Cnossen M, van Essen TA, Ceyisakar IE, Polinder S, Andriessen T, van der Naalt J, Haitsma I, Horn J, Franschman G, Vos P, Peul W, Menon DK, Maas A, Steyerberg E, Lingsma H (2018) Adjusting for confounding by indication in observational studies: a case study in traumatic brain injury. Clin Epidemiol 10:841–852. 10.2147/CLEP.S154500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vik A, Nag T, Fredriksli OA, Skandsen T, Moen KG, Schirmer-Mikalsen K, Manley GT (2008) Relationship of “dose” of intracranial hypertension to outcome in severe traumatic brain injury. J Neurosurg 109:678–684. 10.3171/JNS/2008/109/10/0678 [DOI] [PubMed] [Google Scholar]
- 22.Muizelaar JP, Marmarou A, Ward JD, Kontos HA, Choi SC, Becker DP, Gruemer H, Young HF (1991) Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg. 10.3171/jns.1991.75.5.0731 [DOI] [PubMed] [Google Scholar]
- 23.Coles JP, Fryer TD, Coleman MR, Smielewski P, Gupta AK, Minhas PS, Aigbirhio F, Chatfield DA, Williams GB, Boniface S, Carpenter TA, Clark JC, Pickard JD, Menon DK (2007) Hyperventilation following head injury: Effect on ischemic burden and cerebral oxidative metabolism*. Crit Care Med. 10.1097/01.CCM.0000254066.37187.88 [DOI] [PubMed] [Google Scholar]
- 24.Brandi G, Stocchetti N, Pagnamenta A, Stretti F, Steiger P, Klinzing S (2019) Cerebral metabolism is not affected by moderate hyperventilation in patients with traumatic brain injury. Crit Care. 10.1186/s13054-018-2304-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diringer MN, Videen TO, Yundt K, Zazulia AR, Aiyagari V, Dacey RG, Grubb RL, Powers WJ (2002) Regional cerebrovascular and metabolic effects of hyperventilation after severe traumatic brain injury. J Neurosurg 96:103–108. 10.3171/jns.2002.96.1.0103 [DOI] [PubMed] [Google Scholar]
- 26.Diringer MN, Yundt K, Videen TO, Adams RE, Zazulia AR, Deibert E, Aiyagari V, Dacey RG, Grubb RL, Powers WJ (2000) No reduction in cerebral metabolism as a result of early moderate hyperventilation following severe traumatic brain injury. J Neurosurg 92:7–13. 10.3171/jns.2000.92.1.0007 [DOI] [PubMed] [Google Scholar]
- 27.Neumann J-O, Chambers IR, Citerio G, Enblad P, Gregson BA, Howells T, Mattern J, Nilsson P, Piper I, Ragauskas A, Sahuquillo J, Yau YH, Kiening K (2008) The use of hyperventilation therapy after traumatic brain injury in Europe: an analysis of the brain database. Intensive Care Med 34:1676. 10.1007/s00134-008-1123-7 [DOI] [PubMed] [Google Scholar]
- 28.Gordon E (1971) Controlled respiration in the management of patients with traumatic brain injuries. Acta Anaesthesiol Scand. 10.1111/j.1399-6576.1971.tb05461.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.