Abstract
Hyaluronan (HA) is present in all connective tissues and organs, including the skin and joint fluid. However, few clinical trials have comprehensively evaluated the impacts of oral HA on skin conditions, including wrinkles and moisturization. In this study, we conducted a placebo-controlled, randomized, double-blind trial of daily HA (120 mg) intake for 12 weeks in 40 healthy Asian men and women (aged 35–64 years). Skin condition was determined by the evaluation of wrinkles, stratum corneum water content, the amount of transepidermal water loss, elasticity, and through image analysis. After 12 weeks, skin condition was significantly improved in terms of wrinkle assessment, stratum corneum water content, transepidermal water loss, and elasticity in the HA group compared to the placebo group. Regarding the percentage change from baseline, wrinkle assessment, stratum corneum water content, and skin elasticity were significantly improved in the HA group versus the placebo group after 8 and 12 weeks of ingestion. The present findings indicate that oral ingestion of HA may suppress wrinkles and improve skin condition.
Keywords: hyaluronic acid, dietary supplement, dry skin, wrinkles
1. Introduction
Hyaluronan (HA) is synthesized in all animals and some microorganisms. In vivo, it is present in all connective tissues and organs, including the skin, joint fluid, blood vessels, serum, the brain, cartilage, heart valves, and the umbilical cord. The skin is the largest organ of the body, accounting for 50% of the total body mass [1].
Under the impact of various factors (e.g., aging, ultraviolet light, and dryness, etc.), the content of HA in the skin becomes low and the water content of the horny layer is decreased, leading to the formation of wrinkles and skin aging [2,3]. A study reported that the amount of HA contained in the skin gradually decreases with aging. More specifically, the content of HA in the skin of individuals aged 75 years is less than a quarter of that measured in persons aged 19 years [4].
Surgical techniques (e.g., injection of HA fillers), topical agents, cosmetics, and health functional foods are currently utilized for the anti-aging treatment of the skin and improvement of dry skin. Surgical techniques offer immediate results; however, they are expensive and associated with a risk of pain and swelling [5]. Various laser and light treatments were also proposed to prevent and treat facial aging and dry skin, with variable results [6,7]. Topical drugs and cosmetic creams are relatively inexpensive treatment options. Nevertheless, they exert limited effects on the site of application and are occasionally linked to the occurrence of skin inflammation due to irritation caused by the preservatives and perfumes contained in the products [8]. Although health functional foods do not have an immediate effect, they are inexpensive; moreover, continuous intake of such foods can offer lasting benefits without unwanted side effects.
It was reported that food components (e.g., collagen peptide, placenta, and HA) function to maintain normal skin conditions, such as stratum corneum water content. However, evidence from randomized, placebo-controlled trials investigating anti-wrinkle therapy did not clearly demonstrate significant improvement in wrinkles by food materials other than HA [9,10,11]. Thus far, multiple skin-moisturizing or anti-wrinkle functions of oral HA ingestion have been reported. Sato et al. investigated 39 Japanese women (aged 37–59 years) with skin dryness, sagging, and wrinkles around the eyes who received HA (120 mg/day) for 6 weeks. After 3 weeks of treatment, the HA group had significantly improved corneal water content compared with the placebo group (p < 0.05) [12]. Oe et al. reported that the administration of HA (120 mg/day) for 12 weeks in 50 Japanese men and women (aged 22–59 years) with wrinkles around their eyes resulted in a significant reduction in wrinkle volume ratio after 8 weeks of consumption versus the placebo (p < 0.05) [13]. Nevertheless, thus far, no human study has comprehensively evaluated the impacts of HA ingestion on the skin, including skin hydration, skin barrier function, skin elasticity, skin structure, and facial photography. Therefore, we conducted a double-blind, randomized, placebo-controlled, parallel-group trial involving Asian men and women aged 35–64 years to evaluate the impacts of HA consumption on the skin, with a particular emphasis on multifaceted skin assessment.
2. Materials and Methods
2.1. Study Samples
The subjects received 120 mg/capsule/day of HA (Hyabest®(S)LF-P; Kewpie Corporation, Tokyo, Japan) or the placebo (dextrin; Matsutani Chemical Industry Co., Ltd., Hyogo, Japan), taken orally, for 12 consecutive weeks. The HA had 95% purity according to a high-performance liquid chromatography analysis.
2.2. Study Design and Ethical Aspects
The study followed a randomized, double-blind, and placebo-controlled design. It was conducted in compliance with the Good Clinical Practice guidelines and the applicable regulatory requirements [14]. Written informed consent was provided by all subjects. The study was registered with the UMIN Clinical Trials Registry (UMIN000043750). In addition, the study was approved by the institutional review board of Antai Medical Care Cooperation Antai Tian-Sheng Memorial Hospital (TSMHIRB 19-021-A) and was conducted in accordance with its rules and regulations. The study protocol conformed to the principles of the Declaration of Helsinki for the use of human subjects in experimental research. The present study was conducted from May to August 2019 in Taichung, Taiwan.
Prior to testing, the volunteers were examined by a cosmetic expert for any serious skin disease or damage, particularly on the cheeks and forearms. Before the study, every volunteer was provided with a volunteer protocol. This protocol, stating the terms and conditions of the testing, was individually signed by each volunteer.
2.3. Study Participants
In total, 41 subjects were enrolled into the trial; one subject withdrew from the study for personal reasons. All subjects were aged 35–64 years and met all inclusion criteria. The inclusion criteria were as follows:
-
(1)
Taiwanese male and female subjects aged 30–65 years;
-
(2)
Not currently taking any HA or any other health, nutritional, herbal supplement for skin;
-
(3)
Not currently under-going any medical treatment (including laser treatment, face-lift, or skin-peel);
-
(4)
Not using any topical application cream for skin treatment prescribed by doctors or dermatologists (commonly used facial cleanser, toner, and moisturizer were acceptable).
The subjects were randomly assigned to either the HA or placebo group. They were instructed to maintain their habitual patterns of physical activity throughout the entire study period. All measurements were carried out in a temperature- and relative humidity-controlled room (20 ± 2 °C and 50 ± 5%, respectively).
2.4. Study Schedule
The study was conducted over a period of 12 weeks. All parameters were assessed at four observation time points: weeks 0 (baseline), 4, 8, and 12.
2.5. Skin Hydration and Barrier Function
Skin hydration was evaluated using a capacitance method (Corneometer® CM 825, Courage+Khazaka Electronic, GmbH, Cologne, Germany). The barrier function was evaluated by measuring transepidermal water loss (TEWL) using the Tewameter® TM300 (Courage+Khazaka Electronic, GmbH). At each time point, measurements were performed at three sites on the face and two sites on the body (i.e., arm and waist). Three recordings were obtained for each of these different areas and the average was calculated.
2.6. Skin Elasticity
Skin elasticity was analyzed using the Cutometer® MPA580 (Courage+Khazaka Electronic, GmbH). Skin viscoelastic properties were evaluated by suction and measurements of the consequent skin deformation. This approach measures the elasticity of the upper skin layer using negative pressure, which mechanically deforms the skin. The measurements were performed on the forehead, arm, and waist. For the assessment of body skin elasticity, the Reviscometer® RVM 600 (Courage+Khazaka Electronic, GmbH) was used on the waist. The route resonance of an acoustic wave resonance running time was analyzed, and measurements were conducted at 0°, 90°, 180°, and 360° angles on the arm and waist.
2.7. Skin Structure
Ultrasound analysis was used to determine the thickness of the epidermis and dermis, as well as the collagen intensity score. The dermal thickness was measured using a DermaLab® (Cortex Technology, Hadsund, Denmark) ultrasound probe. Measurements were performed at the temple and waist. The skin surface analysis was carried out using the Visioscan VC98 (Courage+Khazaka Electronic, GmbH). A small area of the facial skin (at the crow feet region) was illuminated using non-harmful ultraviolet A light, and a high-resolution image was captured. The image was digitally analyzed using the surface evaluation of living skin method, which provides quantitative measurements of four parameters: roughness (SEr), scaling (SEsc), smoothness (SEsm), and wrinkling (SEw). This system also allows for the evaluation of five additional parameters, namely energy, entropy, homogeneity, variance, and contrast.
2.8. Facial Photography
Facial skin was digitally photographed, and the degree of wrinkling on the face was quantitatively analyzed using the VISIA® Evolution ver. 7.0.1 complexion analysis system (Canfield Scientific, Inc., Parsippany, NJ, USA).
2.9. Statistical Analysis
It was expected that an evaluable sample of 40 subjects would provide >80% power and an alpha of 0.05 to detect a difference between treatments in the primary outcome variable. The data were expressed as means ± standard deviation. Repeated measures analysis of variance and Dunnett’s test were used to compare the baseline value with that obtained at each measurement time point. After confirming the normal distribution of data using Levene’s test, the independent t-test was used to compare the placebo and HA groups. Statistical tests were performed with a significance level of 5%. SPSS statistics version 25.0 (IBM Corp., Armonk, NY, USA) software was used for the statistical calculations.
3. Results
Participants (n = 40) were randomized at week 0 and allocated to either the HA (n = 20) or placebo (n = 20) group. Overall, the baseline demographics and subject characteristics were in line with those of the targeted trial population. All subjects were aged 35–64 years. There was no significant difference between the HA and placebo groups at week 0 (Table 1).
Table 1.
Baseline characteristics of subjects.
| Placebo | HA | Total | ||||
|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | |
| Number | 5 | 15 | 6 | 14 | 11 | 29 |
| Age (years) mean ± SD |
44.2 ± 3.6 | 44.3 ± 6.5 | 40.5 ± 4.0 | 43.5 ± 6.8 | 43.0 ± 4.1 | 44.5 ± 6.6 |
| Number | 20 | 20 | 40 | |||
HA, hyaluronan; SD, standard deviation.
3.1. Skin Hydration
Skin moisture over the course of the study is shown in Table 2. The assessment showed that the HA group had significantly higher stratum corneum water content in the facial measurement sites (p = 0.02) as compared with the placebo group at 12 weeks after ingestion. The measurements performed on the arm and waist did not show significant differences between the HA and placebo groups. In terms of change from baseline after treatment, the HA group showed a significantly higher percentage change in stratum corneum water content compared with the placebo group at 8 weeks (p = 0.01) and 12 weeks (p = 0.0003) for the face, 12 weeks (p = 0.005) for the arms, and 12 weeks (p = 0.005) for the waist. The assessment showed that the HA group had significantly lower transdermal water transpiration in the face versus the placebo group after 12 weeks of treatment (p = 0.009). The measurements performed on the arm and waist did not show significant differences between the HA and placebo groups. Higher values of percutaneous water transpiration were associated with rougher and unhealthy skin.
Table 2.
Measurement of skin hydration using Corneometer® CM825 and transepidermal water loss (TEWL) using Tewameter® TM300.
| Evaluation Parameter | Group | Measurement Sites | Week 0 | Week 4 | Week 8 | Week 12 |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||
| Corneometer | HA | Face | 49.5 ± 8.53 | 51.5 ± 6.55 | 52.8 ± 7.18 ** | 54.9 ± 7.06 ***† |
| (AU) 1 | Placebo | Face | 49.1 ± 8.13 | 49.4 ± 8.79 | 48.9 ± 9.36 | 48.8 ± 8.99 |
| HA | Arm | 33.9 ± 8.41 | 36.8 ± 6.90 | 36.1 ± 6.38 | 38.6 ± 7.99 ** | |
| Placebo | Arm | 35.4 ± 4.91 | 36.4 ± 5.78 | 35.1 ± 4.99 | 35.6 ± 4.38 | |
| HA | Waist | 29.7 ± 7.85 | 31.9 ± 7.60 | 30.4 ± 7.20 | 32.5 ± 7.14 * | |
| Placebo | Waist | 29.7 ± 5.26 | 31.0 ± 6.57 | 29.9 ± 6.38 | 30.2 ± 5.87 | |
| Tewameter | HA | Face | 12.8 ± 2.39 | 12.1 ± 1.85 | 12.0 ± 2.65 | 10.8 ± 2.49 ***†† |
| (g/h/m2) 2 | Placebo | Face | 12.6 ± 3.23 | 12.9 ± 2.67 | 13.0 ± 3.45 | 13.3 ± 3.09 |
| HA | Arm | 5.79 ± 1.86 | 5.45 ± 1.89 | 5.39 ± 2.10 | 5.40 ± 2.07 | |
| Placebo | Arm | 5.89 ± 2.43 | 5.94 ±3.06 | 5.31 ± 2.10 | 5.57 ± 1.90 | |
| HA | Waist | 3.47 ± 2.18 | 4.27 ± 1.53 | 3.60 ± 1.88 | 4.30 ± 1.88 | |
| Placebo | Waist | 3.74 ± 2.03 | 3.41 ± 1.32 | 3.72 ± 2.68 | 3.83 ± 1.91 |
1 AU, arbitrary units. 2 g/h/m2: water lost per hour per square meter of skin. * p-values (Dunnett’s test), compared with week 0; * indicates p < 0.05, ** indicates p < 0.01, and *** indicates p < 0.001; † p-values (t-test), comparisons between values in the HA and placebo groups; † indicates p < 0.05, and †† indicates p < 0.01. HA, hyaluronan; SD, standard deviation.
3.2. Skin Elasticity
The changes in skin elasticity over time during the study are shown in Table 3 and Table 4. Assessment using Cutometer® MPA580 revealed significantly higher levels of R0, an index of skin acupuncture, in the forehead (p = 0.02), arms (p = 0.02), and waist (p = 0.005) after 12 weeks of ingestion in the HA group compared to the placebo group. The percentage change from the baseline for the waist was significantly higher in the HA group compared with the placebo group for R0 after 8 (p = 0.02) and 12 (p = 0.000006) weeks of ingestion. In the forehead (p = 0.002) and arm (p = 0.01), the HA group showed a significantly higher rate of change compared with the placebo group for R0. The HA group did not differ significantly from the placebo group for measurement of skin elasticity as assessed using the Reviscometer® RVM 600.
Table 3.
Measurement of skin elasticity using Cutometer® MPA580.
| Group | Measurement Sites | Evaluation Parameter | Week 0 | Week 4 | Week 8 | Week 12 |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||
| HA | Forehead | R0 | 0.09 ± 0.04 | 0.09 ± 0.04 | 0.10 ± 0.05 | 0.11 ± 0.05 **† |
| Placebo | 0.08 ± 0.03 | 0.08 ± 0.03 | 0.08 ± 0.02 | 0.08 ± 0.02 | ||
| HA | Forehead | R1 | 0.04 ± 0.02 | 0.04 ± 0.02 | 0.04 ± 0.01 | 0.04 ± 0.02 |
| Placebo | 0.04 ± 0.02 | 0.04 ± 0.01 | 0.04 ± 0.02 | 0.04 ± 0.01 | ||
| HA | Forehead | R2 | 0.62 ± 0.17 | 0.54 ± 0.14 * | 0.52 ± 0.18 ** | 0.59 ± 0.11 |
| Placebo | 0.61 ± 0.14 | 0.59 ± 0.17 | 0.55 ± 0.14 | 0.56 ± 0.15 | ||
| HA | Forehead | R7 | 0.44 ± 0.09 | 0.39 ± 0.09 | 0.37 ± 0.07 * | 0.41 ± 0.12 |
| Placebo | 0.43 ± 0.11 | 0.44 ± 0.16 | 0.42 ± 0.14 | 0.42 ± 0.11 | ||
| HA | Arm | R0 | 0.24 ± 0.04 | 0.24 ± 0.04 | 0.25 ± 0.05 | 0.26 ± 0.04 *† |
| Placebo | 0.23 ± 0.05 | 0.23 ± 0.06 | 0.23 ± 0.05 | 0.22 ± 0.04 | ||
| HA | Arm | R1 | 0.03 ± 0.01 | 0.03 ± 0.01 | 0.03 ± 0.01 | 0.03 ± 0.01 |
| Placebo | 0.04 ± 0.01 | 0.03 ± 0.01 | 0.03 ± 0.01 | 0.04 ± 0.01 | ||
| HA | Arm | R2 | 0.85 ± 0.05 | 0.86 ± 0.04 | 0.86 ± 0.04 | 0.88 ± 0.05 |
| Placebo | 0.84 ± 0.05 | 0.87 ± 0.05 | 0.86 ± 0.04 | 0.85 ± 0.05 | ||
| HA | Arm | R7 | 0.73±0.09 | 0.70 ± 0.05 | 0.72 ± 0.08 | 0.78 ± 0.06 |
| Placebo | 0.74 ± 0.07 | 0.72 ± 0.08 | 0.71 ± 0.08 | 0.75 ± 0.09 | ||
| HA | Waist | R0 | 0.32 ± 0.06 | 0.33 ± 0.07 | 0.34 ± 0.06 | 0.38 ± 0.08 ***†† |
| Placebo | 0.33 ± 0.05 | 0.31 ± 0.05 ** | 0.32 ± 0.05 | 0.32 ± 0.05 | ||
| HA | Waist | R1 | 0.04 ± 0.01 | 0.04 ± 0.01 | 0.03 ± 0.01 *** | 0.04 ± 0.01 |
| Placebo | 0.04 ± 0.01 | 0.04 ± 0.01 | 0.04 ± 0.01 | 0.04 ± 0.02 | ||
| HA | Waist | R2 | 0.87 ± 0.03 | 0.88 ± 0.04 | 0.90 ± 0.04 ** | 0.89 ± 0.04 * |
| Placebo | 0.87 ± 0.03 | 0.88 ± 0.03 | 0.89 ± 0.03 | 0.88 ± 0.04 | ||
| HA | Waist | R7 | 0.77 ± 0.05 | 0.73 ± 0.07 | 0.74 ± 0.06 | 0.78 ± 0.08 |
| Placebo | 0.79 ± 0.05 | 0.75 ± 0.06 | 0.73 ± 0.07 * | 0.77 ± 0.08 |
R0, skin distension: implication for the firmness of the skin; R1, resilient distension: the ability of the skin to return to its original state; and R2, gross elasticity. * p-values (Dunnett’s test), compared with week 0; * indicates p < 0.05, ** indicates p < 0.01, and *** indicates p < 0.001. † p-values (t-test), comparisons between values in the HA and placebo groups; † indicates p < 0.05, and †† indicates p < 0.01. HA, hyaluronan; SD, standard deviation.
Table 4.
Measurement of skin elasticity using Reviscometer® RVM 600.
| Group | Week 0 | Week 4 | Week 8 | Week 12 |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| HA | 269 ± 9.64 | 267 ± 9.85 | 269 ± 9.33 | 269 ± 11.6 |
| Placebo | 269 ± 12.19 | 269 ± 12.5 | 270 ± 11.7 | 269 ± 11.1 |
Resonance running times for angles 0°, 45°, 90°, and 135°. HA, hyaluronan; and SD, standard deviation.
3.3. Skin Structure
The changes in skin architecture over time during the study are shown in Table 5 and Table 6. The HA-treated group did not differ significantly from the placebo-treated group, as assessed using the DermaLab®. For thickness at the temple (p = 0.02) and waist (p = 0.03), the percentage change from baseline after treatment was significantly higher in the HA group than in the placebo group at 12 weeks. The assessment, using Visioscan® VC 98, showed that the HA group had significantly lower levels compared with the placebo group in volume (p = 0.048) and variance (p = 0.046) after 12 weeks of consumption. After 12 weeks of ingestion, the HA group had significantly higher values for SEsm compared with the placebo group (p = 0.02). The percentage change from the baseline was significantly lower in the HA group compared with the placebo group for the volume (p = 0.02), SEw (p = 0.005), SEr (p = 0.04), and variance (p = 0.01) after 12 weeks of ingestion. For SEsm, the HA group had a significantly higher rate of change compared with the placebo group after 12 weeks of ingestion (p = 0.005).
Table 5.
Measurement of skin structure using DermaLab®.
| Group | Measurement Sites | Evaluation Parameter | Week 0 | Week 4 | Week 8 | Week 12 |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||
| HA | Temple | Thickness | 1152 ± 195 | 1151 ± 205 | 1177 ± 204 | 1207 ± 217 * |
| Placebo | Temple | Thickness | 1152 ± 229 | 1152 ± 225 | 1151 ± 210 | 1150 ± 212 |
| HA | Waist | Thickness | 1537 ± 302 | 1544 ± 280 | 1566 ± 313 | 1614 ± 303 ** |
| Placebo | Waist | Thickness | 1513 ± 259 | 1501 ± 254 | 1509 ± 275 | 1517 ± 257 |
| HA | Temple | Intensity | 46.6 ± 9.96 | 47.9 ± 11.9 | 49.6 ± 13.6 | 52.0 ± 12.3 ** |
| Placebo | Temple | Intensity | 47.8 ± 11.9 | 47.0 ± 10.8 | 47.3 ± 11.4 | 48.7 ± 11.4 |
| HA | Waist | Intensity | 38.4 ± 13.4 | 37.6 ± 13.0 | 38.8 ± 13.8 | 41.8 ± 13.5 ** |
| Placebo | Waist | Intensity | 37.8 ± 12.8 | 39.8 ± 12.8 | 38.1 ± 12.6 | 39.3 ± 12.7 |
* p-values (Dunnett’s test) compared with week 0; * indicates p < 0.05, and ** indicates p < 0.01. HA, hyaluronan; and SD, standard deviation.
Table 6.
Measurement of skin micro-relief parameters using Primo and Visioscan® VC 98.
| Group | Evaluation Parameter | Week 0 | Week 4 | Week 8 | Week 12 |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| HA | Surface | 408 ± 54.0 | 429 ± 54.0 | 423 ± 58.5 | 432 ± 47.8 |
| Placebo | 422 ± 38.0 | 430 ± 43.4 | 421 ± 44.2 | 427 ± 45.2 | |
| HA | Volume | 69.2 ± 22.7 | 64.7 ± 26.5 | 59.6 ± 20.2 | 52.1 ± 9.29 **† |
| Placebo | 60.5 ± 19.0 | 61.1 ± 15.7 | 58.7 ± 13.2 | 59.8 ± 14.1 | |
| HA | SEw | 115 ± 23.1 | 110 ± 26.6 | 103 ± 33.9 | 97.8 ± 31.0 ** |
| Placebo | 115 ± 36.9 | 116 ± 34.7 | 113 ± 30.8 | 116 ± 28.7 | |
| HA | SEsc | 0.52 ± 0.13 | 0.49 ± 0.12 | 0.45 ± 0.09 | 0.43 ± 0.11 ** |
| Placebo | 0.47 ± 0.13 | 0.45 ± 0.13 | 0.44 ± 0.07 | 0.42 ± 0.11 | |
| HA | SEsm | 255 ± 48.9 | 254 ± 45.5 | 266 ± 48.2 | 287 ± 43.4 *† |
| Placebo | 252 ± 62.4 | 241 ± 64.5 | 252 ± 59.6 | 245 ± 60.7 | |
| HA | SEr | 3.63 ± 1.42 | 3.59 ± 1.43 | 3.51 ± 1.56 | 3.25 ± 1.39 |
| Placebo | 3.65 ± 1.44 | 3.62 ± 1.43 | 3.56 ± 1.40 | 3.66 ± 1.29 | |
| HA | NRJ | 0.03 ± 0.007 | 0.03 ± 0.008 | 0.03 ± 0.008 | 0.03 ± 0.007 |
| Placebo | 0.02 ± 0.005 | 0.02 ± 0.004 | 0.03 ± 0.005 | 0.03 ± 0.003 | |
| HA | ENT | 1.52 ± 0.04 | 1.52 ± 0.04 | 1.52 ± 0.04 | 1.52 ± 0.04 |
| Placebo | 1.51 ± 0.03 | 1.51 ± 0.02 | 1.51 ± 0.03 | 1.51 ± 0.02 | |
| HA | HOM | 1.40 ± 0.06 | 1.40 ± 0.08 | 1.42 ± 0.07 | 1.42 ± 0.08 |
| Placebo | 1.39 ± 0.05 | 1.40 ± 0.05 | 1.40 ± 0.05 | 1.40 ± 0.05 | |
| HA | CONT | 1.03 ± 0.28 | 1.00 ± 0.32 | 0.99 ± 0.30 | 0.95 ± 0.32 * |
| Placebo | 0.99 ± 0.24 | 0.90 ± 0.13 | 0.90 ± 0.20 * | 0.95 ± 0.17 | |
| HA | VAR | 3.83 ± 0.79 | 3.75 ± 0.80 | 3.59 ± 0.73 | 3.34 ± 0.63 **† |
| Placebo | 3.74 ± 0.47 | 3.67 ± 0.49 | 3.48 ± 0.51 * | 3.70 ± 0.46 |
SD, standard deviation; HA, hyaluronan; SEw, wrinkles: higher values indicated more wrinkles; SEsc, scaliness: lower values indicated less desquamation on the stratum corneum and less scaliness of the skin; SEsm, skin smoothness: lower values indicated smoother skin; SEr, skin roughness: lower values indicated rougher skin; NRJ, energy; ENT, entropy; HOM, homogeneity: higher in young, smooth skin; CONT, contrast; and VAR, variance: lower in young, smooth skin. * p-values (Dunnett’s test), compared with week 0; * indicates p < 0.05, and ** indicates p < 0.01. † p-values (t-test), comparisons between values in the HA and placebo groups; † indicates p < 0.05.
3.4. Facial Photography
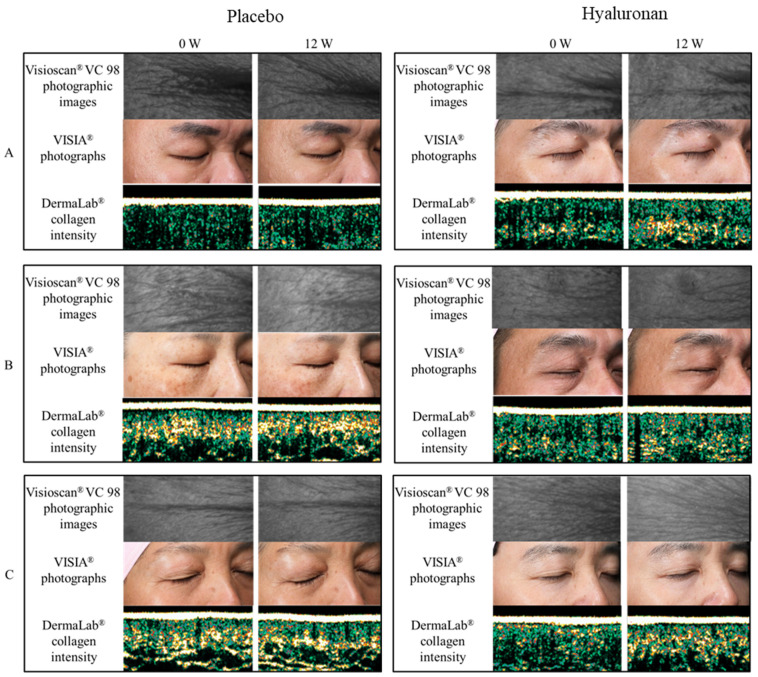
The time course of wrinkles, evaluated using VISIA®, during the study is shown in Table 7. There were no significant differences between the HA and placebo groups. Percentage change from baseline after ingestion of HA was significantly improved in the HA group compared with the placebo group at 8 weeks (p = 0.02) and 12 weeks (p = 0.01). Photographic images are shown in Figure 1.
Table 7.
Skin image by VISIA®.
| Group | Evaluation Parameter | Week 0 | Week 4 | Week 8 | Week 12 |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| HA | Wrinkle | 192 ± 38.0 | 187 ± 38.8 | 188 ± 38.7 | 184 ± 39.2 ** |
| Placebo | Wrinkle | 197 ± 42.6 | 202 ± 41.2 | 206 ± 37.4 | 204 ± 41.9 |
** indicates p < 0.01 (Dunnett’s test), compared with week 0. SD, standard deviation; and HA, hyaluronan.
Figure 1.
Photographic images of Visioscan® VC 98, VISIA® Photographs, and DermaLab® collagen intensity. Representative images of three subjects from each group are shown (A–C).
4. Discussion
This study revealed that oral ingestion of HA for 12 weeks significantly improved multiple parameters (e.g., skin moisturization and wrinkles) compared to the placebo. Moreover, there were no adverse events attributable to the consumption of HA. The epidermal turnover was 28 days [15]. Therefore, it was anticipated that the efficacy could be confirmed after 4 weeks of ingestion. However, significant differences were observed between the HA and placebo groups only after 8 weeks of ingestion. In addition to the stratum corneum, dermal fibroblasts also synthesize collagen fibers, elastin fibers, and HA. In vitro, HA stimulates the proliferation of dermal fibroblasts, and HA stimulates in fibroblasts [16,17]. Therefore, it was assumed that 8–12 weeks of ingestion (i.e., a longer period than the epidermal turnover) was required to obtain a statistically significant anti-senescence effect.
This study was conducted on Asian men and women. However, evidence shows that there are no major differences in skin function between sexes or races. Previous studies have reported that there are no significant differences between men and women in stratum corneum water content, TEWL, or skin elasticity, which are key indicators of skin condition [18,19,20,21,22]. Moreover, according to previous studies, there were no significant differences reported in stratum corneum water content between races [23,24,25,26]. Furthermore, investigations did not reveal significant differences in TEWL between black, white, and Hispanic subjects residing in Northern California, USA [27]. Reportedly, there is also no difference in TEWL between Japanese and German individuals [28]. Corneal lipid and ceramide levels were also reported to be similar in Thai and British individuals [29]. In addition, it was shown that the size of corneocytes does not differ greatly between races [30]. In a German study, ingestion of HA significantly improved stratum corneum moisture, elasticity, skin roughness, and wrinkle depth compared with the baseline [31]. Collectively, these studies demonstrate that there are no differences in the effects of HA consumption across races. Therefore, it is inferred that the results of the present study can also be extrapolated in men and women of other races.
Ingested HA is degraded to 4–6 sugars by the gut microbiota and absorbed into the body to reach the skin [32]. Enterobacteriaceae (e.g., Prevotella), which produce hyaluronidases, are widespread in the gut of Asians and Caucasians [33,34,35]. Since there is a constant number of bacteria with HA-degrading capacity in the gut microbiota regardless of race, there is also no major racial difference in the absorption of HA.
The epidermis is composed of the stratum corneum, the granular layer, the stratum spinosum, and the basal layer. HA, which is required in the epidermis, is synthesized in keratinocytes of the basal layer [36,37]. It binds to receptors (CD44) present on the surface of keratinocytes, and normalizes skin function by signaling [38]. It also possesses a high water retention capacity [39]. Furthermore, owing to its skin normalization function and high water retention capacity, it is thought that HA suppresses wrinkle formation in the epidermis. In addition, it is speculated that multiple factors associated with the in vivo functions of HA are involved in the suppression of wrinkle formation. These mechanisms may have led to the improved efficacy and skin condition against wrinkles demonstrated in this study. This study has potential limitations. It was a relatively small sample size study with some indicators, such as SEms, that were not consistent with trends in other indicator results. Further studies, including mechanisms and large-scale clinical studies, are desirable. Skin condition is associated with various components, including diet, sleep, exercise, aging, hormonal balance, ultraviolet radiation, and seasonal variation. It is desirable to review HA intake and lifestyle habits as a whole for maintaining healthy skin. In the future, further investigation on the synergistic anti-aging effect of HA intake and lifestyle habits is warranted.
5. Conclusions
This study demonstrated that oral ingestion of HA for 12 weeks may improve wrinkle control and skin condition in healthy Asian men and women aged 35–64 years. Thus, the consumption of HA may be used as a functional food that contributes to the maintenance of skin health.
Acknowledgments
We gratefully acknowledge the individuals who participated in the study.
Author Contributions
Conceptualization, M.-F.W.; methodology, software, validation, formal analysis, investigation, T.-F.H., Y.-H.H., and Z.-R.S.; resources, Y.M.; data curation, T.-F.H.; writing—original draft preparation, M.O. and R.M.; writing—review and editing, M.O.; visualization, T.-F.H. and M.O.; supervision, T.-F.H.; project administration, Y.M.; funding acquisition, Y.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Kewpie Corporation.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Antai Medical Care Cooperation Antai Tian-Sheng Memorial Hospital (protocol code TSMHIRB 19-021-A and date of approval 6 May 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions.
Conflicts of Interest
M.O., R.M., and Y.M. are employees of Kewpie Corporation. The remaining authors have no other conflict of interest to report in this work.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Laurent T.C., Fraser J.R. Hyaluronan. FASEB J. 1992;6:2397–2404. doi: 10.1096/fasebj.6.7.1563592. [DOI] [PubMed] [Google Scholar]
- 2.Fisher G.J., Wang Z.Q., Datta S.C., Varani J., Kang S., Voorhees J.J. Pathophysiology of premature skin aging induced by ultraviolet light. N. Engl. J. Med. 1997;337:1419–1428. doi: 10.1056/NEJM199711133372003. [DOI] [PubMed] [Google Scholar]
- 3.Dai G., Freudenberger T., Zipper P., Melchior A., Grether-Beck S., Rabausch B., de Groot J., Twarock S., Hanenberg H., Homey B., et al. Chronic ultraviolet B irradiation causes loss of hyaluronic acid from mouse dermis because of down-regulation of hyaluronic acid synthases. Am. J. Pathol. 2007;171:1451–1461. doi: 10.2353/ajpath.2007.070136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Longas M.O., Russell C.S., He X.Y. Evidence for structural changes in dermatan sulfate and hyaluronic acid with aging. Carbohydr Res. 1987;159:127–136. doi: 10.1016/S0008-6215(00)90010-7. [DOI] [PubMed] [Google Scholar]
- 5.Haneke E. Adverse effects of fillers and their histopathology. Facial Plast. Surg. 2014;30:599–614. doi: 10.1055/s-0034-1396755. [DOI] [PubMed] [Google Scholar]
- 6.Cannarozzo G., Fazia G., Bennardo L., Tamburi F., Amoruso G.F., Del Duca E., Nisticò S.P. A new 675 nm laser device in the treatment of facial aging: A prospective observational study. Photobiomodul. Photomed. Laser Surg. 2021;39:118–122. doi: 10.1089/photob.2020.4908. [DOI] [PubMed] [Google Scholar]
- 7.Nistico S.P., Silvestri M., Zingoni T., Tamburi F., Bennardo L., Cannarozzo G. Combination of fractional CO2 laser and rhodamine-intense pulsed light in facial rejuvenation: A randomized controlled trial. Photobiomodul. Photomed. Laser Surg. 2021;39:113–117. doi: 10.1089/photob.2020.4876. [DOI] [PubMed] [Google Scholar]
- 8.Draelos Z.D. Facial skin care products and cosmetics. Clin. Dermatol. 2014;32:809–812. doi: 10.1016/j.clindermatol.2014.02.020. [DOI] [PubMed] [Google Scholar]
- 9.Asserin J., Lati E., Shioya T., Prawitt J. The effect of oral collagen peptide supplementation on skin moisture and the dermal collagen network: Evidence from an ex vivo model and randomized, placebo-controlled clinical trials. J. Cosmet. Dermatol. 2015;14:291–301. doi: 10.1111/jocd.12174. [DOI] [PubMed] [Google Scholar]
- 10.Kim K., Sung J., Lee H., Ono T., Yonei Y. Effect of a dietary supplement containing porcine placenta extract on skin hydration-A placebo controlled, randomized, double blind, clinical study. Jpn. Pharmacol. Ther. 2018;46:1023–1034. [Google Scholar]
- 11.Sugihara F., Inoue N. Clinical effects of collagen hydrolysates ingestion on UV-induced pigmented spots of human skin: A preliminary study. Health Sci. 2012;28:153–156. [Google Scholar]
- 12.Sato T., Yoshida T., Kanemitsu T., Yoshida K., Hasegawa M., Urushibata O. Clinical effects of hyaluronic acid diet for moisture content of dry skin. Aesthetic Dermatol. 2007;17:33–39. (In Japanese) [Google Scholar]
- 13.Oe M., Sakai S., Yoshida H., Okado N., Kaneda H., Masuda Y., Urushibata O. Oral hyaluronan relieves wrinkles: A double-blinded, placebo-controlled study over a 12-week period. Clin. Cosmet. Investig. Dermatol. 2017;10:267–273. doi: 10.2147/CCID.S141845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use . ICH Harmonised Guideline: Integrated Addendum to ICH E6 (R1): Guideline for Good Clinical Practice E6 (R2) European Medicines Agency; London, UK: 2016. [Google Scholar]
- 15.Halprin K.M. Epidermal “turnover time”—A re-examination. Br. J. Dermatol. 1972;86:14–19. doi: 10.1111/j.1365-2133.1972.tb01886.x. [DOI] [PubMed] [Google Scholar]
- 16.Greco R.M., Iocono J.A., Ehrlich H.P. Hyaluronic acid stimulates human fibroblast proliferation within a collagen matrix. J. Cell. Physiol. 1998;177:465–473. doi: 10.1002/(SICI)1097-4652(199812)177:3<465::AID-JCP9>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 17.Lüke H.J., Prehm P. Synthesis and shedding of hyaluronan from plasma membranes of human fibroblasts and metastatic and non-metastatic melanoma cells. Biochem. J. 1999;343:71–75. doi: 10.1042/bj3430071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rogiers V., Derde M., Verleye G., Roseeuw D. Standardized conditions needed for skin surface hydration measurements. Cosmet. Toilet. 1990;105:73–82. [Google Scholar]
- 19.Jacobi U., Gautier J., Sterry W., Lademann J. Gender-related differences in the physiology of the stratum corneum. Dermatology. 2005;211:312–317. doi: 10.1159/000088499. [DOI] [PubMed] [Google Scholar]
- 20.Wilhelm K.P., Cua A.B., Maibach H.I. Skin aging. Effect on transepidermal water loss, stratum corneum hydration, skin surface pH, and casual sebum content. Arch. Dermatol. 1991;127:1806–1809. doi: 10.1001/archderm.1991.04520010052006. [DOI] [PubMed] [Google Scholar]
- 21.Close T., Ezure E., Yagi N., Kunizawa T., Hirao S. Amano. comparison of sagging at the cheek and lower eyelid between male and female faces. Ski. Res. Technol. 2011;17:510–515. doi: 10.1111/j.1600-0846.2011.00526.x. [DOI] [PubMed] [Google Scholar]
- 22.Ishikawa T., Ishikawa O., Miyachi Y. Measurement of skin elastic properties with a new suction device (I): Relationship to age, sex and the degree of obesity in normal individuals. J. Dermatol. 1995;22:713–717. doi: 10.1111/j.1346-8138.1995.tb03907.x. [DOI] [PubMed] [Google Scholar]
- 23.Berardesca E., Pirot F., Singh M. Differences in stratum corneum pH gradient when comparing white Caucasian and Black African American skin. Br. J. Dermatol. 1988;139:855–857. doi: 10.1046/j.1365-2133.1998.02513.x. [DOI] [PubMed] [Google Scholar]
- 24.Berardesca E., Maibach H.I. Sodium lauryl sulphate induced cutaneous irritation: Comparison of White and Hispanic subjects. Contact Derm. 1988;18:136–140. doi: 10.1111/j.1600-0536.1988.tb05512.x. [DOI] [PubMed] [Google Scholar]
- 25.Berardesca E., Maibach H.I. Racial differences in sodium lauryl sulphate induced cutaneous irritation: Black and white. Contact Derm. 1988;18:65–70. doi: 10.1111/j.1600-0536.1988.tb02741.x. [DOI] [PubMed] [Google Scholar]
- 26.Manuskiatti W., Schwindt D.A., Maibach H.I. Influence of age, anatomic site and race on skin roughness and scaliness. Dermatology. 1998;196:401–407. doi: 10.1159/000017932. [DOI] [PubMed] [Google Scholar]
- 27.Berardesca E., Rigal J., Leveque J.L. In vivo biophysical characterization of skin physiological differences in races. Dermatologica. 1991;182:89–93. doi: 10.1159/000247752. [DOI] [PubMed] [Google Scholar]
- 28.Aramaki J., Kawana S., Effendy I., Happle R., Loffler H. Differences of skin irritation between Japanese and European women. Br. J. Dermatol. 2002;146:1052–1056. doi: 10.1046/j.1365-2133.2002.04509.x. [DOI] [PubMed] [Google Scholar]
- 29.Meldrum H., Harding C.R., Rogers J.S. The characteristic decrease in scalp stratum corneum lipids in dandruff is reversed by the use of a Zince Pyrithione containing shampoo. IFSCC Mag. 2003;6:3–6. [Google Scholar]
- 30.Corcuff P., Lotte C., Rougier A., Maibach H.I. Racial differences in corneocytes. Acta Derm. Venereol. 1991;71:146–148. [PubMed] [Google Scholar]
- 31.Göllner I., Voss W., von Hehn U., Kammerer S. Ingestion of an oral hyaluronan solution improves skin hydration, wrinkle reduction, elasticity, and skin roughness: Results of a clinical study. J. Evid. Based Complement. Altern. Med. 2017;22:816–823. doi: 10.1177/2156587217743640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kimura M., Maeshima T., Kubota T., Kurihara H., Masuda Y., Nomura Y. Absorption of orally administered hyaluronan. J. Med. Food. 2016;19:1172–1179. doi: 10.1089/jmf.2016.3725. [DOI] [PubMed] [Google Scholar]
- 33.Karlsson F.H., Nookaew I., Nielsen J. Metagenomic data utilization and analysis (MEDUSA) and construction of a global gut microbial gene catalogue. PLoS Comput. Biol. 2014;10:e1003706. doi: 10.1371/journal.pcbi.1003706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kawai K., Kamochi R., Oiki S., Murata K., Hashimoto W. Probiotics in human gut microbiota can degrade host glycosaminoglycans. Sci. Rep. 2018;8:10674. doi: 10.1038/s41598-018-28886-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sato T., Kamaguchi A., Nakazawa F. Purification and characterization of hemolysin from Prevotella oris. J. Oral. Biosci. 2012;54:11–118. doi: 10.1016/j.job.2012.03.002. [DOI] [Google Scholar]
- 36.Tammi R., Ripellino J.A., Margolis R.U., Maibach H.I., Tammi M. Localization of epidermal hyaluronic acid using the hyaluronate binding region of cartilage proteoglycan as a specific probe. J. Investig. Dermatol. 1988;90:412–414. doi: 10.1111/1523-1747.ep12456530. [DOI] [PubMed] [Google Scholar]
- 37.Sakai S., Yasuda R., Sayo T., Ishikawa O., Inoue S. Hyaluronan exists in the normal stratum corneum. J. Investig. Dermatol. 2000;14:1184–1187. doi: 10.1046/j.1523-1747.2000.00992.x. [DOI] [PubMed] [Google Scholar]
- 38.Bourguignon L.Y. Matrix hyaluronan-activated CD44 signaling promotes keratinocyte activities and improves abnormal epidermal functions. Am. J. Pathol. 2014;184:1912–1919. doi: 10.1016/j.ajpath.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Comper W.D., Laurent T.C. Physiological function of connective tissue polysaccharides. Physiol. Rev. 1978;58:255–315. doi: 10.1152/physrev.1978.58.1.255. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions.