Abstract
While in vitro and animal studies of osteoblastic and osteoclastic activity as well as bone resistance for copper are numerous, and the results encouraging in terms of regulation, human studies are scarce. The aim of this narrative review was to investigate the correlation of blood copper, daily copper intake, and copper supplementation with bone mineral density. This review included 10 eligible studies: five studies concerned copper blood levels, one study concerned daily copper intake, and four studies concerned copper supplementation. Blood copper levels did not show statistically significant differences in four of the studies analyzed, while only one study showed differences between osteoporotic and healthy women, although only with women between 45 and 59 years of age and not between 60 and 80 years of age. The dietary copper intake among women with or without osteoporosis did not show any differences. Only one study with a small sample of subjects carried out these assessments; therefore, it is a topic that the literature must deepen with further studies. The two studies that analyzed the integration of copper (2.5–3 mg/day) only showed good results in terms of slowing down bone mineral loss and reducing resorption markers, confirming the effectiveness of copper supplementation on bone metabolism.
Keywords: copper, bone health, humans, supplementation, bone mineral density
1. Introduction
In our organism there are between 50 and 120 mg of copper; almost two thirds of the body’s copper content is found in the muscles and skeleton, but the liver is also a key site for maintaining copper concentrations in plasma [1,2].
The quantity of copper absorption varies with dietary copper intake, ranging from over 50 percent at 1 mg/day to less than 20 percent at above 5 mg/day [3]. Part of the absorption occurs in the stomach where the acidic environment promotes the solubility of copper by dissociation from copper-containing macromolecules derived from food sources [4,5].
Turnover is faster and more copper is expelled into the gastrointestinal tract when there is more absorption. Excretion is probably the main point of regulation of the body’s total copper, and this efficient homeostatic regulation of absorption and retention helps to protect the body against copper toxicity and deficiency [3], while also considering that the excretory capacity of the kidney is limited [5]. The absorption of copper is inhibited by the presence of phytates, calcium, ascorbic acid, and other trace elements such as zinc, whose metabolism is linked to that of copper [6]. Indeed, it has been found that zinc supplementation in subjects with sickle cell anemia causes a deficiency of copper in the blood [7,8].
The RDA for adult women and men is 900 μg/day [9], and the foods with the highest content of copper are: bovine and ovine liver, dried fruit especially cashews, oysters, arigas, octopus, prawns, cod, mackerel, quail, and chicken and turkey leg [10].
A study carried out on healthy young people established that 0.38 mg of copper per day was not sufficient to maintain its balance in the body and that the minimum requirement should be between 0.4 and 0.8 mg/day [11].
The main function of copper is the constitution of enzymes that transfer electrons (oxidases) to achieve the reduction of molecular oxygen, and is therefore essential for energy metabolism at the cellular level [4,12,13]. Among these enzymes we find lysyl oxidase, which uses lysine and hydroxylysine (present in collagen and elastin) as substrates to produce the cross-links necessary for the development of connective tissues, including those of bones [9,14,15,16,17].
Various in vitro studies have ascertained the positive effect of copper on the cells that regulate bone metabolism; Li et al. showed that copper ion can inhibit osteoclastic resorption, [18] while other authors demonstrated that the positive effects of copper are dose-dependent. In particular, low concentrations (i.e., 0.1% w/w) of Cu improved the viability and growth of osteoblastic cells, while higher concentrations of Cu (i.e., 2.5% and 1% (w/w)) proved to be cytotoxic [19].
Furthermore, the presence of copper stimulates the differentiation of mesenchymal stem cells towards the osteogenic lineage [20].
Animal studies have shown that dietary copper deficiency can lead to a decrease in the copper present in our body and consequently to the reduction of the activity of some enzymes [5,21]. The physiological consequences of copper deficiency include connective tissue defects, which lead, among others, to skeletal problems [5].
A copper-deficient diet in chicks showed that this deficiency is able to block the formation of cross bonds in collagen and elastin from various tissues, with consequent bone fragility related to the nutritional deficiency of copper [22].
To evaluate bone strength in copper deficiency, a diet deficient in this mineral was administered to mice, which showed a reduction in mechanical strength. This situation was subsequently associated with defects in the bone collagen component [23].
A recent review summarized all these mechanisms of copper and its skeletal impact [24].
While in vitro and animal studies of osteoblastic and osteoclastic activity and bone resistance are numerous and the results encouraging in terms of regulation, human studies are scarce, and no reviews have been published on this topic. Therefore, the aim of this narrative review was to consider the correlation of blood copper, daily copper intake, and copper supplementation with bone mineral density.
2. Results
2.1. Blood Copper Concentrations in Relation to Bone Metabolism
This research was conducted with these keywords: “copper” AND “copper blood concentrations” AND “bone” AND “humans”. We analyzed a total of five studies: four cross-sectional studies and one case-control study.
The description of the studies are presented in Table 1.
Table 1.
Studies that considered blood copper levels.
| First Author, Year | Study Design | Institution and Country | Inclusion Criteria | Number of Subjects (M-F) Mean Age |
Micronutrient Serum Concentration Osteoporosis | Micronutrient Serum Concentration Osteopenia | Micronutrient Serum Concentration Normal | Primary Outcomes | Results |
|---|---|---|---|---|---|---|---|---|---|
| Okyay E, 2013 [25] | Cross-sectional study | Dokuz Eylul University School of Medicine, Izmir, Turkey | Postmenopausal women between age 45 and 80 | 728 F 56.52 ± 6.14 y |
Women at 45–59 years: (p value < 0.05) Cu (μg/mL):
|
Women at 45–59 years: (p value < 0.05) CU (μg/mL):
|
Relationship between serum main minerals and postmenopausal osteoporosis. | Low Cu serum levels were independent risk factors for development of OP especially in early menopausal period. | |
| Mutlu M, 2007 [26] | Cross-sectional study | Erciyes University, Kayseri, Turkey | Post-menopausal women | 120 F 40 OP 58 ± 8.40 y, osteopenic 57 ± 9 y and 40 healthy group 59 ± 6 y |
Cu (mg/L) 1.54 ± 0.12 |
Cu (mg/L) 1.59 ± 0.09 |
Cu (mg/L) 1.60 ± 0.08 |
Cu changes in osteoporotic, osteopenic, and normal postmenopausal women. | No statistically significant differences observed between the osteopenic, osteoporotic, and control groups with respect to copper levels. |
| Arikan DC 2011 [27] | Case–control study | Medical Faculty of Kahramanmaras Sutcu Imam (Kahramanmaras, Turkey) |
Natural menopause for more than 6 months | 107 F 35 healthy 48.17 ± 7.78 y, 37 osteopenic 55.32 ± 7.78 y and 35 OP 60.57 ± 8.65 y |
Cu (μg/dL) 138.76 ± 37.21 |
Cu (μg/dL) 137.58 ± 31.73 |
Cu (μg/dL) 140.92 ± 32.74 |
Serum Cu levels in postmenopausal women with osteoporosis, osteopenia, and in healthy controls, and the relationship between Cu and bone mineral density (BMD). |
Plasma levels of all parameters were similar across each group (p > 0.05). |
| Mahdavi-Roshan, 2015 [28] | Cross-sectional study | Rheumatology clinic in Tabriz, Islamic Republic of Iran | women > 50 years old postmenopausal, having no history of hormone replacement therapy | 51 F 57.97 ± 1.2 y |
Serum Cu (μg/dL): 27.29 ± 1.26 |
Serum Cu (μg/dL) 26.75 ± 1.35 |
Investigate and compare the mineral status between osteopenic and osteoporotic postmenopausal women. |
No statistically significant differences between the osteopenic and osteoporotic groups with respect to serum levels of Cu. |
|
| LIU SZ, 2009 [29] | Cross- sectional study | Xi’an urban area, China | 45 to 65-year-old females in natural and no hormone drug intake and osteoporosis treatment 6 months before investigation |
290 F 54.4 ± 5.5 y |
Cu serum (mg/L) 0.8873 ± 0.2930 |
Cu serum (mg/L) 0.8528 ± 0.2397 |
Cu serum (mg/L) 0.8498 ± 0.3106 |
Correlation between serum macroelement and trace element contents and BMD as well as the occurrence of osteoporosis. | There exist significant correlations between the contents of serum Cu, but no significant differences in this element content between the osteoporosis group, osteopenia group, and healthy group. |
2.2. Copper Intake in Relation to Bone Metabolism
This research was conducted with these keywords: “copper” AND “copper intake” AND “bone” AND “humans”. We analyzed a total of one cross-sectional study.
The description of the studies are presented in Table 2.
Table 2.
Studies that considered copper intake.
| First Author, Year | Study Design | Institution and Country | Inclusion Criteria | Number of Subjects (M-F) Mean Age |
Lowest Quintile Intake/RDA or EAR | % Subject in Lowest Quintile Intake/% Subject < RDA or EAR | Highest Quintile Intake | % Subject in Highest Quintile Intake | Primary Outcomes | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Mahdavi-Roshan, 2015 [28] | Cross-sectional study | Rheumatology clinic in Tabriz, Islamic Republic of Iran | Postmenopausal women > 50 years, having no history of hormone replacement therapy | 51 F 57.97 ± 1.2 y |
The mean dietary intake (and percent from RDA) of copper in post-menopausal women with low bone density was 1.07 ± 0.08 mg/day (120 ± 12.2% RDA) |
Investigate and compare the mineral status between osteopenic and osteoporotic postmenopausal women. | No statistically significant differences between the osteopenic and osteoporotic groups with respect to dietary intake copper. |
2.3. Copper Supplementation in Relation to Bone Metabolism
This research was conducted with these keywords: “copper” and “copper supplementation” and “bone” and “humans”. A total of four studies were analyzed: two double-blind placebo-controlled trial, one double-blind randomized trial, and one longitudinal study.
The description of the studies are presented in Table 3.
Table 3.
Studies that considered copper supplementation.
| First Author, Year | Study Design | Institution and Country | Inclusion Criteria | Intervention | Parallel Treatments | Number of Subjects (M-F) Mean Age |
Duration of the Intervention | Primary Outcomes | Results |
|---|---|---|---|---|---|---|---|---|---|
| Nielsen FH, 2011 [30] | double-blind, placebo-controlled design. | University of North Dakota | postmenopausal women aged 51–80 y, BMI ≤ 32 kg/m2, BMD not more than 2·5 standard deviations below that for young adults | 600 mg calcium (Ca) supplement plus a 2 mg Cu (copper gluconate) and 12 mg Zn (zinc gluconate) supplement. |
supplement containing 600 mg Ca plus a maize starch placebo | 649 F | 2 years | How Cu and Zn intakes would reduce the risk for bone loss. | Cu supplementation apparently did not have an impact on whole-body bone contents, BMD. |
| Strause L, 1994 [31] | double-blind, placebo-controlled trial. | San Diego greater Metropolitan area |
>50 y old and in good general health | (1) placebo Ca + active trace minerals, (2) active Ca + placebo trace minerals, (3) active Ca + active trace mineral: 1000 mg elemental calcium/d in the form of Ca citrate malate and active supplement contained 15.0 mg of Zn as sulfate salt, 2.5 mg of Cu, and 5.0 mg of manganese as gluconate salts. | placebo calcium + placebo trace minerals | 59 F 66 ± 7 y |
2 years | Impact of supplementary Ca with and without the addition of a combination trace elements on spinal bone loss. |
Supplementation with 1000 mg of Ca, 15 mg of Zn, 5 mg of manganese, and 2.5 mg of Cu maintained spinal bone density and differed significantly from a placebo group that lost bone density. |
| Eaton-Evans 2003 [32] | random and double-blind study | Royal Victoria Hospital, north Belfast | healthy women, aged 45–56 years | 3 mg Cu as amino acid chelate | placebo | 73 F Cu group: 49.97± 3.1 Placebo group: 50.8 ± 3.5 |
2 years | Effects of Cu supplementation over 2 years on vertebral trabecular bone mineral density (VTBMD). | Cu supplementation appeared to have reduced the loss of VTBMD in these middle-aged women over a 2-year period. |
| Baker A 1999 [33] | longitudinal intervention trial | Institute of Food Research, Norwich, UK | Subjects without any history of bone or articular disease, and with no intake of medicine that could affect bone or cartilage metabolism | Medium (1.6 mg/d), low (0.7 mg/d) and high (6.0 mg/d) intakes of Cu, in that order. A 7 d rotating low Cu menu was formulated and analysed for Cu content. This low Cu diet (0.7 mg/d) was fed throughout the three dietary periods and was supplemented to the appropriate level of Cu (as a CuSO4 solution dissolved in de-mineralised water taken with a meal) to achieve the medium (1.6 mg/d) and high (6.0 mg/d) Cu intakes. |
////////// | 11 M 30.9 y |
8-week dietary periods with a minimum of 4-week washout periods. | Effects of changing from a medium (1.6 mg Cu/d) to a low (0.7 mg Cu/d) or a high (6.0 mg/d) Cu intake on biochemical indices of bone turnover in healthy adult males. | Biomarkers of bone resorption were significantly increased when subjects were switched from the medium to the low Cu diet. |
3. Discussion
A total of five studies evaluated the blood levels of copper in osteoporotic, osteopenic, and healthy subjects. While there were no statistically significant differences in copper blood levels between the population groups investigated in four of the papers [26,27,28,29], outcomes were the opposite in Okyay’s 2013 study. A total of 728 menopausal, osteoporotic, or healthy women were enrolled and divided into age groups (45–59 years and 60–80 years); blood levels of copper and bone mineral density in different districts (lumbar L1–L4, neck of the femur, and whole femur) in these women were evaluated. The study results demonstrated a statistically significant difference in blood copper levels between osteoporotic and healthy women in all the districts analyzed, but only in the 45–59 age group [25].
A single 2015 study compared the dietary copper intake of postmenopausal women with osteopenia and osteoporosis, demonstrating the absence of a statistically significant difference between the two groups [28].
Regarding the studies that evaluated copper supplementation in relation to bone metabolism, the individual effects of copper were assessed in two studies [32,33], while two other papers evaluated the effects of a micronutrient association [30,31].
The Eaton-Evans study evaluated the effects of supplementation with 3 mg of copper versus placebo, in a group of healthy women, for a total of 2 years, subsequently coming to the conclusion that there seems to be a reduction in the loss of vertebral bone mineral density in the treated group [32].
A different type of study was instead designed by Baker et al. A total of 11 healthy men were identified and given several levels of copper intakes. The subjects all followed a 3-week diet that started with medium copper content (1.6 mg/d), followed by low copper content (0.7 mg/d), and lastly, with high copper content (6 mg/d). The basic power supply was always that which corresponded to the low copper intake, with different additions of copper sulfate to achieve the average intake or the high intake. Between the first and the second period, i.e., the transition from medium to low copper intake, an increase in some bone resorption markers was assessed, while these markers significantly decreased with the transition from the deficient to the rich copper diet [33].
The remaining two papers have conflicting conclusions. Nielsen’s 2011 study, which compared calcium supplementation versus calcium supplementation associated with copper and zinc in a group of postmenopausal women emphasized the effectiveness of the association of zinc but not copper [30]. However, in the study by Strause, healthy postmenopausal women were involved and divided into four groups (calcium supplement + micronutrient supplement, calcium supplement + micronutrient placebo, calcium placebo + micronutrient supplement, placebo of calcium + placebo of micronutrients), where the group that received both calcium and micronutrient supplements, including copper, maintained lumbar bone mineral density with a significant difference as compared to the group that received only placebo. The remaining two groups were at an intermediate level, demonstrating no significant differences with the treated group or with the placebo group [31].
4. Materials and Methods
This narrative review was performed following Egger et al. [34] with these steps:
Configuration of the working group: two operators, experts in clinical nutrition (one acting as a methodological operator and one participating as a clinical operator).
Formulation of the questions based on the considerations indicated in the abstract: the correlation of blood copper, daily copper intake, and copper supplementation with bone mineral density.
Recognition of the relevant studies. Research was carried out on PubMed (Public Medline run by the National Center of Biotechnology Information (NCBI) of the National Library of Medicine of Bethesda (USA)) as follows: (a) definition of the keywords (copper, humans, bone health, bone mineral density, supplementation), inserting the interest field of the documents to be searched, grouped in quotation marks (“…”), and used separately or in combination; (b) use of the Boolean variable (true or false) AND operator, that allows for the establishment of logical relations among concepts; (c) research modalities: advanced search; (d) limits: papers published in the last 20 years; humans; adults; languages: English; (e) manual search performed by the researchers experienced in clinical nutrition through the revision of articles, focusing on the effectiveness of copper supplementation (alone or with other micronutrients) on the growth and maintenance of bone in humans, in order to suggest a daily dosage for copper supplementation.
Published in journals qualified in the Index Medicus.
Analysis and presentation of the outcomes: paragraphs about effectiveness of copper supplementation alone or in combination with other nutrients were created, and the data extrapolated from the “revised studies” were collocated in tables; in particular, the author, year of publication, and the characteristics of the study were specified for each study.
An analysis of the reports in the form of a narrative review was carried out. At the beginning of each section, the type of studies chosen and the keywords considered are reported. Studies of any design which considered the effectiveness of copper supplementation (alone or with other micronutrients) on the growth and maintenance of bone in humans were evaluated.
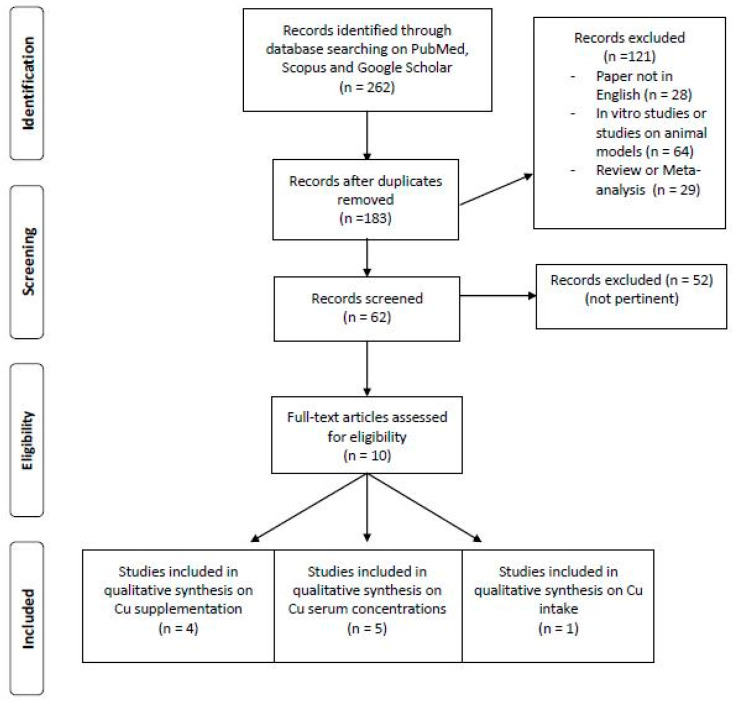
Figure 1 indicates the flow chart for the research of the literature.
Figure 1.
Flow chart for research of the literature.
5. Conclusions
While in vitro and animal studies of osteoblastic and osteoclastic activity and bone resistance are numerous and the results encouraging in terms of regulation, human studies are scarce.
Blood copper levels did not show statistically significant differences in four of the studies analyzed, while only one study showed differences between osteoporotic and healthy women, although only with women 45–59 years of age and not 60–80 years of age.
The dietary copper intake among women with or without osteoporosis did not show any differences. Only one study with a small sample of subjects carried out these assessments; therefore, it is a topic that the literature must deepen with further studies.
The two studies that analyzed the integration of copper (2.5–3 mg/day) only showed good results in terms of slowing down bone mineral loss and reducing resorption markers, thus confirming their effectiveness.
Author Contributions
Conceptualization, M.R.; methodology, M.R.; data curation, S.P.; writing—original draft preparation, M.R. and M.A.F.; writing—review and editing, V.I., C.G., A.T., and G.P. (Gabriella Peroni); visualization, A.R. and G.P. (Giovanna Petrangolini); supervision, G.I.; project administration, M.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available in this article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Olivares M., Uauy R. Limits of metabolic tolerance to copper and biological basis for present recommendations and regulations. Am. J. Clin. Nutr. 1996;63:846S–852S. doi: 10.1093/ajcn/63.5.846. [DOI] [PubMed] [Google Scholar]
- 2.Turnlund J.R., Keyes W.R., Peiffer G.L., Scott K.C. Copper absorption, excretion, and retention by young men consuming low dietary copper determined by using the stable isotope 65Cu. Am. J. Clin. Nutr. 1998;67:1219–1225. doi: 10.1093/ajcn/67.6.1219. [DOI] [PubMed] [Google Scholar]
- 3.Turnlund J.R. Human whole-body copper metabolism. Am. J. Clin. Nutr. 1998;67:960S–964S. doi: 10.1093/ajcn/67.5.960S. [DOI] [PubMed] [Google Scholar]
- 4.Harris D. Copper. In: O’Dell B., Sunde R., editors. Handbook of Nutritionally Essential Mineral Elements. Marcel Dekker; New York, NY, USA: 1997. pp. 231–273. [Google Scholar]
- 5.Turnlund J. Copper. In: Shike M., Ross A., editors. Modern Nutrition in Health and Disease. Williams & Wilkins; Baltimore, MD, USA: 1999. pp. 241–252. [Google Scholar]
- 6.Roggi C., Turconi G. Igiene Degli Alimenti e Della Nutrizione Umana-La Sicurezza Alimentare. EMSI; Rome, Italy: 2003. [Google Scholar]
- 7.Prasad A., Brewer G., Schoomaker E., Rabbani P. Hypocupremia induced by zinc therapy in adults. J. Am. Med. Assoc. 1978;240:2166–2168. doi: 10.1001/jama.1978.03290200044019. [DOI] [PubMed] [Google Scholar]
- 8.Simon S.R., Branda R.F., Tindle B.H., Burns S.L. Copper deficiency and sideroblastic anemia associated with zinc ingestion. Am. J. Hematol. 1988;28:181–183. doi: 10.1002/ajh.2830280310. [DOI] [PubMed] [Google Scholar]
- 9.Food and Nutrition Board Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium. National Academies Press; Washington, DC, USA: 2001. [PubMed] [Google Scholar]
- 10.Ieo BDA Banca Dati di Composizione degli Alimenti per studi Epidemiologici in Italia. [(accessed on 20 September 2007)]; Available online: http://www.bda-ieo.it.
- 11.Turnlund J.R., Scott K.C., Peiffer G.L., Jang A.M., Keyes W.R., Keen C.L., Sukanashi T.M. Copper status of young men consuming a low-copper diet. Am. J. Clin. Nutr. 1997;65:72–78. doi: 10.1093/ajcn/65.1.72. [DOI] [PubMed] [Google Scholar]
- 12.da Silva F., Williams R. Copper: Extracytoplasmic oxidases and matrix formation. In: da Silva F., Williams R., editors. The Biological Chemistry of the Elements: The Inorganic Chemistry of Life. Clarendon Press; Oxford, UK: 1991. pp. 388–399. [Google Scholar]
- 13.Kubiak K., Klimczak A., Dziki Ł., Modranka R., Malinowska K. Influence of copper (II) complex on the activity of selected oxidative enzymes. Pol. Merkur. Lekarski. 2010;28:22–25. [PubMed] [Google Scholar]
- 14.Dahl S., Rucker R., Niklason L. Effects of copper and cross-linking on the extracellular matrix of tissue-engineered arteries. Cell Transpl. 2005;14:861–868. doi: 10.3727/000000005783982936. [DOI] [PubMed] [Google Scholar]
- 15.John J. Nutrition and bone health. In: Mahan L., editor. Escott-Stump Krause’s Food, Nutrition & the Nutrition Care Process. Elsevier; Amsterdam, The Netherlands: 2012. [Google Scholar]
- 16.Rucker R.B., Murray J., Riggins R.S. Nutritional copper deficiency and penicillamine administration: Some effects on bone collagen and arterial elastin crosslinking. Adv. Exp. Med. Biol. 1977;86:619–648. doi: 10.1007/978-1-4757-9113-6_35. [DOI] [PubMed] [Google Scholar]
- 17.Rucker R., Kosonen T., Clegg M., Mitchell A., Rucker B., Uriu-Hare J., Keen C. Copper, lysyl oxidase, and extracellular matrix protein cross-linking. Am. J. Clin. Nutr. 1998;67:996S–1002S. doi: 10.1093/ajcn/67.5.996S. [DOI] [PubMed] [Google Scholar]
- 18.Li B., Yu S. In vitro study of the effects of copper ion on osteoclastic resorption in various dental mineralized tissues. Chin. J. Stomatol. 2007;42:110–113. [PubMed] [Google Scholar]
- 19.Milkovic L., Hoppe A., Detsch R., Boccaccini A.R., Zarkovic N. Effects of Cu-doped 45S5 bioactive glass on the lipid peroxidation- associated growth of human osteoblast-like cells in vitro. J. Biomed. Mater. Res. Part A. 2014;102:3556–3561. doi: 10.1002/jbm.a.35032. [DOI] [PubMed] [Google Scholar]
- 20.Ding H., Gao Y.-S., Wang Y., Hu C., Sun Y., Zhang C. Dimethyloxaloylglycine increases the bone healing capacity of adipose-derived stem cells by promoting osteogenic differentiation and angiogenic potential. Stem Cells Dev. 2014;23:990–1000. doi: 10.1089/scd.2013.0486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Milne D. Assessment of copper nutritional status. Clin. Chem. 1994;40:1479–1484. doi: 10.1093/clinchem/40.8.1479. [DOI] [PubMed] [Google Scholar]
- 22.Rucker R., Riggins R., Laughlin R., Chan M., Chen M., Tom K. Effects of nutritional copper deficiency on the biomechanical properties of bone and arterial elastin metabolism in the chick. J. Nutr. 1975;105:1062–1070. doi: 10.1093/jn/105.8.1062. [DOI] [PubMed] [Google Scholar]
- 23.Jonas J., Burns J., Abel E.W., Cresswell M.J., Strain J.J., Paterson C.R. Impaired mechanical strength of bone in experimental copper deficiency. Ann. Nutr. Metab. 1993;37:245–252. doi: 10.1159/000177774. [DOI] [PubMed] [Google Scholar]
- 24.Gaffney-Stomberg E. The Impact of Trace Minerals on Bone Metabolism. Biol. Trace Elem. Res. 2019;188:26–34. doi: 10.1007/s12011-018-1583-8. [DOI] [PubMed] [Google Scholar]
- 25.Okyay E., Ertugrul C., Acar B., Sisman A.R., Onvural B., Ozaksoy D. Comparative evaluation of serum levels of main minerals and postmenopausal osteoporosis. Maturitas. 2013;76:320–325. doi: 10.1016/j.maturitas.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 26.Mutlu M., Argun M., Kilic E., Saraymen R., Yazar S. Magnesium, zinc and copper status in osteoporotic, osteopenic and normal post-menopausal women. J. Int. Med. Res. 2007;35:692–695. doi: 10.1177/147323000703500514. [DOI] [PubMed] [Google Scholar]
- 27.Arikan D.C., Coskun A., Ozer A., Kilinc M., Atalay F., Arikan T. Plasma selenium, zinc, copper and lipid levels in postmenopausal Turkish women and their relation with osteoporosis. Biol. Trace Elem. Res. 2011;144:407–417. doi: 10.1007/s12011-011-9109-7. [DOI] [PubMed] [Google Scholar]
- 28.Mahdavi-Roshan M., Ebrahimi M., Ebrahimi A. Copper, magnesium, zinc and calcium status in osteopenic and osteoporotic post-menopausal women. Clin. Cases Miner. Bone Metab. 2015;12:18–21. doi: 10.11138/ccmbm/2015.12.1.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu S.Z., Yan H., Xu P., Li J.P., Zhuang G.H., Zhu B.F., Lu S.M. Correlation analysis between bone mineral density and serum element contents of postmenopausal women in Xi’an urban area. Biol. Trace Elem. Res. 2009;131:205–214. doi: 10.1007/s12011-009-8363-4. [DOI] [PubMed] [Google Scholar]
- 30.Nielsen F.H., Lukaski H.C., Johnson L.K., Roughead Z.K. Reported zinc, but not copper, intakes influence whole-body bone density, mineral content and T score responses to zinc and copper supplementation in healthy postmenopausal women. Br. J. Nutr. 2011;106:1872–1879. doi: 10.1017/S0007114511002352. [DOI] [PubMed] [Google Scholar]
- 31.Strause L., Saltman P., Smith K., Bracker M., Andon M. Spinal bone loss in postmenopausal women supplemented with calcium and trace minerals. J. Nutr. 1994;124:1060–1064. doi: 10.1093/jn/124.7.1060. [DOI] [PubMed] [Google Scholar]
- 32.Eaton-Evans J., Mcllrath E., Jackson W., McCartney H., Strain J. Copper supplementation and the maintenance of bone mineral density in middle-aged women. J. Trace Elem. Exp. Med. Off. Publ. Int. Soc. Trace Elem. Res. Hum. 2003;9:87–94. doi: 10.1002/(SICI)1520-670X(1996)9:3<87::AID-JTRA1>3.0.CO;2-E. [DOI] [Google Scholar]
- 33.Baker A., Harvey L., Majask-Newman G., Fairweather-Tait S., Flynn A., Cashman K. Effect of dietary copper intakes on biochemical markers of bone metabolism in healthy adult males. Eur. J. Clin. Nutr. 1999;53:408–412. doi: 10.1038/sj.ejcn.1600763. [DOI] [PubMed] [Google Scholar]
- 34.Egger M., Dickersin K., Smith G.D. Systematic Reviews in Health Care. BMJ Publishing Group; London, UK: 2008. Problems and Limitations in Conducting Systematic Reviews; pp. 43–68. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available in this article.