Abstract
Tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL), also known as Apo-2 ligand (Apo2L), is a member of the TNF cytokine superfamily. TRAIL has been widely studied as a novel strategy for tumor elimination, as cancer cells overexpress TRAIL death receptors, inducing apoptosis and inhibiting blood vessel formation. However, cancer stem cells (CSCs), which are the main culprits responsible for therapy resistance and cancer remission, can easily develop evasion mechanisms for TRAIL apoptosis. By further modifying their properties, they take advantage of this molecule to improve survival and angiogenesis. The molecular mechanisms that CSCs use for TRAIL resistance and angiogenesis development are not well elucidated. Recent research has shown that proteins and transcription factors from the cell cycle, survival, and invasion pathways are involved. This review summarizes the main mechanism of cell adaption by TRAIL to promote response angiogenic or pro-angiogenic intermediates that facilitate TRAIL resistance regulation and cancer progression by CSCs and novel strategies to induce apoptosis.
Keywords: TRAIL, cancer stem cells, TRAIL resistance, angiogenesis
1. Introduction
Apoptosis, or programmed cell death, is a naturally occurring mechanism that eliminates damaged cells. Intracellular signals from mitochondria or by ligands that bind to receptors on the cell membrane, such as Fas, tumor necrosis factor (TNF)-α/TNF receptor 1, Apo-3 ligand/death receptor (DR) 3, and TNF-related apoptosis-inducing ligand (TRAIL), can initiate apoptosis [1,2]. Intrinsic and extrinsic pathways can activate apoptosis. The extrinsic pathway is induced by signals that activate cell surface death receptors, such as the binding of TNF-α to TNF-R1. Meanwhile, an example of an intrinsic pathway can be seen as induced by the B cell lymphoma 2 (Bcl-2)-regulated mitochondrial pathway, leading to a release of cytochrome c, which associates with apoptotic protease activating factor 1 (APAF-1) and pro-caspase-9, forming the apoptosome, leading to the activation of caspase-9 [3]. Thus, apoptosis plays an important role in physiological processes, including the development of cardiovascular and neurological diseases and malignancies [4].
TRAIL was discovered in the last decade of the 20th century [5]. It is a TNF-related type 2 transmembrane protein encoded by the NFSF10 gene located on human chromosome 3 at 3q26. In the organism, TRAIL is part of the mechanism by which the immune system reacts against malignant cells, inducing apoptosis with minimal cytotoxicity toward normal cells [6]. The TRAIL protein consists of 281 amino acids of 33 KDa and, in its fully glycosylated form, 41 KDa. However, TRAIL is cleaved at the 114 amino acid position by cysteine proteases to produce soluble TRAIL, a protein of 24 KDa called sTRAIL. For TRAIL to fully activate, an insertion of 12–16 amino acids in the receptor-binding site is required [7]. Physiologically, TRAIL is secreted by different tissue cells in the spleen, lung, prostate, placenta, kidney, cytotoxic T cells, and natural killer cells. Monocytes and dendritic cells can express TRAIL on their surface after stimulation with interferon-β (IFN-β), which boosts antitumoral activity. In addition, there is a trace of sTRAIL in blood plasma (approximately 100 pg/mL) [8].
TRAIL can bind to five different receptors. DR4 and DR5 are death receptors (TRAIL-R1 and TRAIL-R2). Decoy receptors (DcR1 or DcR2, also TRAIL-R3 and TRAIL-R4) are anti-apoptosis receptors. The first receptors are overexpressed in tumors, and the latter are expressed mainly in normal cells [9]. The difference between both receptor types is the lack of cytoplasmic domains required for apoptosis activation. Another receptor discovered to bind TRAIL is osteoprotegerin (OPG). OPG is a soluble receptor that inhibits TRAIL apoptosis [10]. DR5 has been reported to be more efficient in apoptosis induction. However, DR5 nuclear localization in tumor cells is a signal of resistance to TRAIL [11].
DR4 and DR5 are transmembrane proteins with several cysteine-rich domains (CRDs) in their extracellular region, a single transmembrane domain, and a death domain (DD) in their intracellular region. DDs are homotypic protein modules organized in six alpha-helices that act as binding sites for other proteins and communicate the apoptotic signal to the cell interior [7]. After TRAIL binding to DR4 and DR5 occurs, their trimerization initiates by the interaction of the DD and the Fas-associated death domain (FADD), inducing TRAIL receptors that expose the death effector domain (DED) and the formation of the death-inducing signaling complex (DISC) [3]. Next, the DISC recruits pro-caspase-8 and cleaves it. Cleaved caspase-8 decreases the membrane potential and converts Bid to truncated Bid (tBid). Then, tBid, p53, Noxa, Puma, and Bax form the pore-forming complex in the mitochondria outer membrane [12]. After pore formation, cytochrome C is released into the cytoplasm, interacting with dATP. Pro-caspase-9 is then recruited to Apaf-1 to form the Apaf-1/caspase-9 apoptosome [13]. Active caspases are proteolytic proteins that bench to cytosolic and nuclear targets; caspases cause cleavage of actin filaments of the cytoskeleton, the inhibitor of caspase-activated DNase (ICAD) that avoids activation of caspase-activated DNase (CAD) that destroys DNA [12].
This mechanism of cell death, which has been widely studied in the context of cancer and other diseases, is efficient. Many basic and clinical studies have demonstrated a relevant role in selectively inducing apoptosis, and in tumor cells, this has been demonstrated. Therefore, apoptosis continues to be a therapeutic target that needs to be studied.
2. Recombinant TRAIL
Recombinant versions of human APO2L/TRAIL have been developed and used in clinical trials due to their potential as antitumoral therapy. However, there has been some limitation in their use as an anticancer drug because of their short half-life in blood, fast elimination, and resistance by cancer cells [10]. Dulanermin is a recombinant non-tagged TRAIL used in clinical trials. However, this protein has not shown important therapeutical benefits due to poor efficiency binding to TRAIL receptors [14]; another form of Dulanermin, Apo2L.XL, presents higher pro-apoptotic activity by artificial cross-linking [7].
Tumoral cells can generate TRAIL resistance by downregulation of DR4 and DR5 and inhibition of the CD95/Fas domain [6]. Moreover, the signal received in TRAIL receptors can be switched to activate non-canonical signaling, inducing pro-inflammatory, pro-survival, and proliferation characteristics. This signal involves a complex integrated by receptor-interacting serine/threonine protein kinase 1 (RIPK19), tumor necrosis factor (TNF) receptor-associated factor 2 (TRAF2), and TNF receptor-associated death domain (TRADD), activating pro-tumor pathways, such as IkB/NF-kB, MAPK/ERK, STAT3, PI3K, Akt, JAK2, and Src [10].
The development of different recombinant TRAIL therapies has gained importance as a new strategy for reducing cancer progress. As mentioned before, TRAIL receptors have been discovered mainly in cancer cells; however, their overexpression has been reported in a particular population of cancer cells in tumors called cancer stem cells (CSCs).
3. Cancer Stem Cells and TRAIL
CSCs are a subpopulation of cells that represent a low percentage within the tumor niche. These cells have pluripotency, self-renewal, and tumorigenic properties, such as invasiveness, plasticity, and maintenance, and are the main cause of chemoresistance and cancer relapse. Several CSC markers have been identified, such as homing cell adhesion molecule (CD44) [15], aldehyde dehydrogenase (ALDH) [15], CD326 [16], and CD133 [17]. Although some of these markers are useful for identification and therapeutic targets, they are further found in normal stem cells and are not specific [16].
Epithelial–mesenchymal transition (EMT) is a process associated with the stemness of cancer cells, which is critical during cancer progression. This process of EMT implicates the conversion of epithelial cells into a mesenchymal phenotype with loss of cell–cell junctions, altering cell–ECM interactions and cytoskeletal organization [18]. EMT mediators can stimulate the increased malignancy associated with the CSC phenotype, such as migration and invasion by protein expression and activation of transcription factors. These factors include SNAI1 and SNAI2 (Snail and Slug), ZEB1 (dEF1/TCF8), and ZEB2 and Twist. Others are Prrx1, Sox4, Sox9, Klf4, and members of the AP-1 (Jun/Fos) family [19]. Pathways involved in EMT include transforming growth factor-beta (TGF-β), bone morphogenetic protein (BPM), receptor tyrosine kinase (RTK), Wnt/β-catenin, Notch, Hedgehog, signal transducer and activator of transcription 3 (STAT3), extracellular matrix (ECM), and hypoxia [20].
Genes of stem lineage Oct-4 and Nanog upregulate the process of EMT by binding to the promotors of Zeb1, Zeb2, Twist1, Prrx1, and miR-21. In addition, Sox2 increases slug expression, activating the STAT3/ hypoxia-inducible 1alpha (HIF-1α) signaling pathway, inducing EMT and promoting metastasis [20,21,22]. Altogether, these factors improve the protection of senescence and apoptosis and regulate cell progression and resistance to chemotherapy and radiotherapy, reducing E-cadherin expression, which drives to a mesenchymal state. In the tumor microenvironment, cancer cells secrete factors, such as TGF-β, hepatocyte growth factor (HGF), and platelet-derived growth factor (PDGF), activating changes in EMT [23]. Moreover, TGF-β is a major inducer of EMT since it can interact with other growth factors, such as epidermal growth factor (EGF), to influence the malignant transformation of CSCs and tumor-associated stromal fibrosis [23]. Once activated, EMT increases the expression of genes involved in stemness and stem cell markers. Additionally, in breast cancer, EMT increases stem cell phenotypes, such as CD44+/CD24- markers. EMT markers, such as E-cadherin, β-catenin, Snail, and Vimentin, correlate with CD133 expression, invasion, and metastasis of CSCs [20].
4. TRAIL Resistance Mechanism
EMT promotes TRAIL resistance and silencing of E-cadherin, which inhibits apoptosis due to the lack of efficient DISC assembly by ligated TRAIL receptors [10]. CD133 is a cell marker commonly expressed in CSCs, such as in colorectal cancer (CRC) and glioma [13]. Other CSC markers include CD44, nestin, and sox-2, usually co-expressing with CD133 [9,23]. CD133-positive cells present high ATP-binding cassette transporter (ABCG5) expression related to chemoresistance [12]. For this reason, these cells are novel targets for cancer therapy [12]. Embryonic pathways, such as Notch, Wnt, Hedgehog, and Hippo, are overactivated in CSCs to maintain their stem cell characteristics [24]. The Wnt signaling pathway participates in the chemoresistance of CD133-positive cells in CRC; thus, it is also considered a potential target [25]. Moreover, CD133 activates the PI3K pathway, and this, Akt, whose activation leads to upregulation of anti-apoptosis factors, such as BCL-2, BCL-XL, and MCL-1, decreases the pro-apoptotic factors Bid, Bax, and Bim [12].
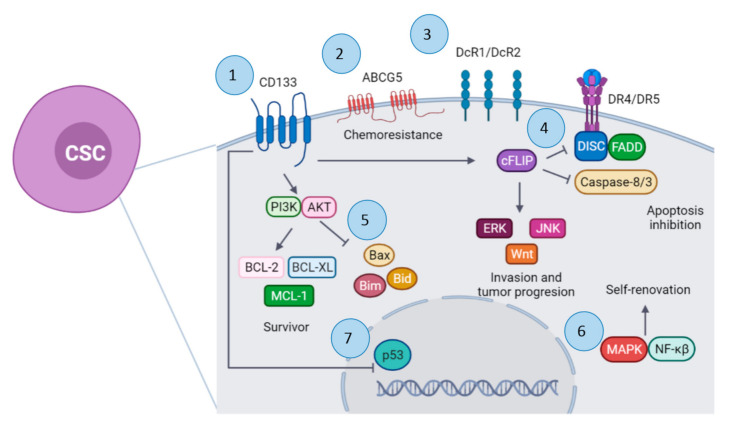
Although TRAIL is a promising anticancer therapy, which can induce apoptosis in tumoral cells instead of normal cells, some CSC tumoral cells develop resistance to TRAIL (Figure 1) [26]. However, TRAIL treatment resistance has been developed by a variety of cancers [27]. Another TRAIL resistance mechanism associated with downregulation of the dead receptors DR4 and DR5 is overexpression of the decoy receptors DcR1 and DcR2 and overexpression of apoptosis inhibitors, such as cFLIP. It is suggested that activation of NF-kB could upregulate DR5 expression [9]. In turn, activation of the NF-kB pathway by TRAIL is associated with improvement of tumor growth, clonal expansion, and CSC signaling [6]. TRAIL-R2 or DR5 promotes invasion and metastasis of KRAS-mutated cancers by activating Rac1/phosphatidylinositol-3-kinase (PI3K) signaling. This metastasis process is cell-autonomous and mediated by the membrane-proximal domain (MDP) of the receptor [28]. In addition, it is reported that TRAIL-R downregulation and apoptosis resistance are mediated by signals, such as Src, Talin, PI3K, and MAP. Phosphatase and tensin homolog (PTEN) protein negatively regulates the PI3K/AKT/mTOR pathway, working as a tumor suppressor gene, and EMT [29].
Figure 1.
Mechanism of apoptosis resistance by cancer stem cells (CSCs). 1. CD133 activates the PI3K/AKT pathway. 2. Overex-pression of ATP-binding cassette transporter (ABCG5). 3. Overexpression of decoy receptors (DcR1/DcR2) and down-regulation of DR4/DR5 receptors. 4. Overexpression of cFLIP protein. 5. Downregulation of pro-apoptotic factors. 6. Upregulation of MAPK and NF-kβ pathways. 7. Downregulation of p53. Created with BioRender.com (accessed on 25 May 2021).
Moreover, the molecule ONC201/TIC10 can induce apoptosis by the TRAIL pathway, showing great results in vitro and in vivo. It is currently being used in phase I/II clinical trials for advanced-stage cancer, such as breast cancer, colon cancer, and glioblastoma. The mechanism of ONC201/TIC10 is the inactivation in CSCs of Akt and ERK signaling, inducing Foxo3 nuclear translocation and transcription of TRAIL, independent of the p53 status. In addition, this leads to the expression of the TRAIL receptor DR5. This molecule improves the half-life, distribution, route of administration, and activity of recombinant TRAIL and TRAIL-agonist antibodies, the main problems in its clinical application [30].
CD133-positive cells can also develop TRAIL resistance by overexpression of FLICE-like inhibitory protein (FLIP), inhibiting the DISC ensemble and TRAIL apoptosis. Moreover, p53 protein expression has an inverse relationship with CD133 expression [12]. cFLIP overexpression is also associated with TRAIL resistance in cancer cells. cFLIP inhibits caspase-8 and caspase-3 activation [9]. The expression of FLIP, a caspase-8 inhibitor, is higher in CD133-positive cells than in CD133-negative cells. CD133 upregulates FLIP expression, and this protein inhibits autophagy and activates ERK, JNK, ERK, and Wnt pathways. FLIP also inhibits FADD [12,26]. According to some studies, suppression of cytoplasmic cFLIP and elevated nuclear cFLIP levels are associated with regulating the Wnt pathway, which impacts the maintenance of CSCs. Inhibition of cFLIP further reduces beta-catenin levels and inhibits Wnt target gene expression, whereas overexpression of nuclear cFLIP promotes Wnt target gene expression [31]. In addition, downregulating Wnt/β-catenin signaling impacts TRAIL sensitivity and reduces EMT [32,33]. TRAIL resistance is also associated with activation of self-renewing pathways by mitogen-activated protein kinases (MAPKs) and NF-kβ, both negatively regulated by PTEN. The high expression of PTEN correlates with a better TRAIL response in tumors and with the reverse process of EMT (mesenchymal–epithelial transition (MET)) [34].
Although there are CSCs resistant to TRAIL, some research groups have reported that CSCs are susceptible to TRAIL activity after stimulation with small-molecule compounds, such as CDDP, etoposide, PS-341 (bortezomib), tunicamycin, rottlerin, brandisianins, sodium butyrate, and inostamycin [35]. Other natural compounds, such as kurarinone, icaritin, and withanolide E, are reported to downregulate cFLIP expression and TRAIL-resistant cancer cell sensitization to TRAIL-induced apoptosis. Natural compounds, such as silibinin, gingerol, and indomethacin, are reported to possess both mechanisms of sensitizing TRAIL-resistant cancer cells. The most relevant results are summarized in Table 1. A TRAIL-sensitive phenotype can be observed in different types of cancers and under different conditions. TRAIL can induce contrasting effects in tumoral cells, mainly controlled by the TME. The combination of TRAIL with some compounds prevents CSC TRAIL resistance and induces its elimination as sulforaphane [6]. Additional treatment with cisplatin combined with recombinant TRAIL could restore the expression of death receptors and Fas domain activity [6]. Dickkopf-1 (DKK-1) diminishes the expression of CD133, and consequently, proliferation, migration, and invasion of cancer cells diminish [25]. Agonists of TRAIL receptors have not presented enough efficacy due to the complexity of TRAIL signaling [10].
Table 1.
Treatments that increase TRAIL sensitivity.
| Treatment | Cancer | Effect | Reference |
|---|---|---|---|
| Goniothalamin plus TRAIL | Colorectal cancer | Enhance cytotoxicity and apoptosis | [35] |
| Icaritin plus TRAIL | Glioblastoma | Enhance apoptosis by c-FLIP downregulation and inhibition of NF-κB activity | [36] |
| Micelle-in-liposomes with piperlongumine plus TRAIL | Prostate cancer | Increase sensitization to TRAIL apoptosis in cancer cells | [37] |
| Silibinin plus TRAIL | Glioma | Enhance apoptosis by upregulation of DR5 and downregulation of cFLIP and survival | [38] |
| SH122 plus TRAIL | Prostate cancer | Enhanced TRAIL-induced apoptosis via D5R and the mitochondrial pathway | [39] |
| MSC/dTRAIL-TK gene therapy | Renal cell carcinoma | Enhance sensitization to TRAIL and increase apoptosis | [40] |
| Duloxetine plus TRAIL | Lung cancer | Enhance apoptosis of tumor cells through inhibition of autophagy | [41] |
| 3-Methyladenine and chloroquine plus TRAIL | Malignant melanoma and osteosarcoma | Enhance pro-apoptotic mitochondrial pathway of tumor cells through inhibition of autophagy | [42] |
| Adenovirus-p53 plus TRAIL | Ovarian and nasopharyngeal squamous cancer | Overexpression of DR5 receptor in cancer cells to increase apoptosis by TRAIL | [43] |
| Adenovirus E1A plus adenovirus-hTRAIL | Hepatic cancer | Enhance apoptosis by upregulation of TRAIL receptors | [44] |
| MiR-760 plus TRAIL | Non-small-cell lung cancer | Enhance apoptosis by targeting FOXA1 | [45] |
5. Microenvironment and TRAIL Activity
The interaction of cells in the TME and CSCs can change the signaling mechanism of TRAIL in a tumor, leading to cell death or disease progression [46]. An antitumor TME is made by normal fibroblasts, dendritic cells (DC), natural killer (NK) cells, cytotoxic T cells, and M1 tumor-associated macrophages (TAMs) with the release of pro-inflammatory cytokines [10]. In contrast, a protumor TME includes M2 TAMs producing anti-inflammatory cytokines; myeloid-derived suppressor cells (MDSCs); regulatory T cells (Tregs) and B cells; cancer-associated fibroblasts (CAFs); and TIE2-expressing monocytes, mast cells, pericytes, and endothelial cells. In addition, neutrophils and T helper cells present both roles, pro- and anti-tumorigenic activity [47]. Different factors can regulate the production and secretion of TRAIL by several immune cells from the innate and adaptative immune systems. On the other hand, these similar factors can regulate the expression of membrane bound TRAIL and its receptors in the cellular microenvironment from components in TME, such as cells, cytokines, pH, oxygen levels, and matrix components [7]. For example, cytokines as IFNs can activate TRAIL transcription by the IRF1/STAT complex. TRAIL and TRAIL-R transcription is also mediated by stress-induced factors, such as nuclear factor of activated T cells (NFAT), Forkhead Box (FOX) proteins, NF-kB, C/EBP homologous protein, activator protein 1 (AP1), and p53 [10].
Physiologically, the TRAIL/TRAIL-R system regulates the homeostasis of adaptative immune cells by inducing apoptosis of aberrantly activated T cells. NK cells eliminate aberrant tumor cells by granule release (perforin/granzyme) in the innate immune system. This release is dependent on membrane receptor interactions involving FasL, TNFα, and TRAIL. TNFα increases TRAIL expression in mesenchymal stem cells (MSCs), inhibiting tumor growth by apoptosis induction of cancer cells [7]. In addition, DNA released from MSCs could act as damage-associated molecular patterns (DAMPs) that via TLR3-dependent NF-kB feed-forward loop further increase TRAIL expression on MSCs. Furthermore, TNFα-activated MSCs also produce IFNβ due to DNA/RNA released from apoptotic cells, thus enhancing TRAIL expression [10]. The activation of NK cells by IL12 generates IFNγ, which enhances TRAIL expression [48].
Monocytes can also express TRAIL and target TRAIL-R in tumoral cells. It is seen that IFNα increases the release of soluble TRAIL by monocytes and promotes apoptosis of tumoral cells [27,49]. Moreover, macrophages secrete matrix metallopeptidase 12 (MMP12), which can mimic TRAIL and induce apoptosis in tumor cells [50]. TRAIL also induces CD14 and CD11b expression in monocytes, promoting its M1 differentiation and its phagocytic capacity and antitumor activity [51]. In addition, by TRAIL stimulation, macrophages produce pro-inflammatory cytokines IL1β, IL6, and TNFα in an NF-kB-dependent way [10].
As a component of the ECM, elastin microfibril interface-located protein 2 (EMILIN2) can bind to TRAIL receptors DR4 and DR5, inducing clustering and co-localization on lipid rafts from cell membrane, and then induce activation of apoptosis [10]. Hypoxia factors, such as HIF-1α, are associated with PKCε down-modulation, which acts as a key molecular event that promotes apoptosis by TRAIL in hypoxic tumor cells. In addition, the expression of vascular cell adhesion molecule-1 (VCAM-1) by tumors has been proposed as an immune escape mechanism and improves metastasis. VCAM-1 and a4 integrin interaction promotes T cell migration away from the tumor, reducing CD8+ T cell infiltration [52]. Cytotoxic T cells (CTLs) are the main effectors of the adaptative immune system against tumor cells, expressing TRAIL and TRAIL-R. This TRAIL expression is stimulated by interaction with TRAIL receptors on tumoral cells [10]. In addition, IFNα stimulates CTLs to increase TRAIL expression. Dendritic cells (DCs) participate in innate and adaptative immunity, acting as a bridge between both responses [53]. DCs present antigens to T cells; however, cytotoxic DCs activated by IFNα or IFNγ present antitumor activity by the TRAIL system [54]. TRAIL reduces T regulatory cells (Tregs), while increasing the CD8+ CTLs population [10].
TRAIL shares homology with FasL, another member of the TNF family that can induce T cell apoptosis. In a pro-tumoral TME, TRAIL, soluble or membrane bound, can induce apoptosis in IL2-secreting T cells but not inactivated T cells [55]. Fas ligand (FasL/CD95L) expressed by tumors allows them to inhibit T cell recognition and elimination. FasL is associated with immune escape because it binds to Fas in the T cell membrane and induces apoptotic signals. In addition, galectin-1 participates in the immunosuppressive tumor microenvironment, improving FasL activity [52]. It seems that cancer cells can release microvesicles with FAS and TRAIL, which, instead, induce apoptosis of cancer cells and target and eliminate CTLs as an immune escape mechanism. In multiple myeloma cancer cells, TRAIL bound to membranes can eliminate osteoclasts and bone formation, consequently improving the distribution of cancer cells to other tissues and allow metastasis development [10]. In metastatic tumors, cells can evade immune surveillance by inducing cell death of tumor-infiltrating lymphocytes (TILs). CRC cells expressing TRAIL can induce apoptosis of CD8+ cells by this mechanism [56]. In lymphomas, cancer cells can develop TRAIL resistance by the expression of CD40, a co-stimulatory receptor for interaction with CD4+ T cells that protects apoptosis by TRAIL. CD40 upregulates NF-kB, cFLIP, and Bcl-XL [10,31].
In this microenvironment of resistant tumor cells, TRAIL can potentiate immune suppressive effects of Tregs. Tumor-infiltrating Tregs reduce antitumor immune responses by secretion of TGFβ, IL10, and IL35, inhibiting CTL, NK cell, and DC activity. IL35 can stimulate macrophages and neutrophil polarization to an M2 anti-inflammatory state that promotes tumor development. Another cytokine that suppresses TRAIL activity in cancer cells is IL8, by upregulation of cFLIP in a CXCR2- and NF-kB-dependent way [57]. In addition, cancer cells from primary tumors release IL4, increasing the expression of anti-apoptotic proteins, such as cFLIP, Bcl-XL, and Bcl-2 [58]. It is important to note that even when cancer cells are resistant to TRAIL, exposure activates the secretion of the immune-suppressive cytokines, IL8, CXCL1, CXCL5, and CCL2 in a FADD-dependent way [59].
CCL2 is important because it seems to modulate the immune environment to a pro-tumoral state when interacting with cells with CCR2 receptors. As mentioned before, the interaction of cancer cells with endogenous TRAIL induces FADD-dependent secretion of CCL2, which polarizes monocytes to the M2 macrophage phenotype [59]. In addition, TRAIL receptors and FADD can promote NF-kB activation and proliferation of tumor cells. Moreover, CCL2 supports tumor growth by acting as a chemoattractant for MDSCs and monocytes, promoting its MS differentiation by their CD206 expression [28]. The reduction in TRAIL expression is stimulated by IL6, IL1β, IL17, and G-CSF through STAT3-dependent downregulation and upregulation of MMP9. The result is immune suppression and a pro-angiogenic state [10].
6. TRAIL Activity in Angiogenesis
Angiogenesis allows the support of tissue growth and organ function under physiological and pathological conditions. During the pathological process, such as cancer, this mechanism helps the tumor feed, supply oxygen, and eliminate waste from the body [49]. The process of generating new blood vessels occurs through several different mechanisms: (1) from pre-existing vasculature; (2) inducing new blood vessel formation through a process involving formation and outgrowth of sprouts (tip cells), which eventually fuse with an existing vessel or newly formed sprout; (3) vasculogenesis (neo-vascularization from endothelial progenitor cells); (4) vascular mimicry, in which aggressively growing tumor cells can form vessel-like structures, which are formed without the contribution of endothelial cells, and that represents an alternate channel for tumor cells to source sufficient blood supply and nutrients; and (5) trans-differentiation of CSCs (neo-vascularization in tumors through differentiation of CSCs to endothelial cells) [60].
Normal stem cells and CSCs grow primarily in vascular niches due to a perivascular microenvironment [61]. Tumors can be vascularized through the cooperation of endothelial cells [62]. The involvement of CSC is key to promote angiogenesis in cancer and disease progression. Studies suggest that Notch signaling plays an essential role in angiogenesis through interactions with Notch ligands to cross-talk with other pathways, such as vascular endothelial growth factor (VEGF) signaling [63]. However, the vascular niche of cancer is rich in abnormal blood vessels. These abnormalities are induced by hypoxia, low pH, and high pressure of a hostile interstitial fluid. Hypoxia also activates NF-kB and promotes EMT [64].
Furthermore, hypoxia increases hypoxia-inducible 1alpha (HIF1α) in cancer cells [65]. Moreover, hypoxia increases nitric oxide (NO), which activates the Wnt/b-catenin signaling pathway, VEGF-A, and, ultimately, angiogenesis [66]. Angiogenesis is orchestrated within the tumor mass that harbors various host-derived cells, regulated by secreted regulators, such as VEGFR2, the expression of Tie-2 monocytes, fibroblasts, endothelial cells, and innate and adaptive immune cells that are central regulators of pro-angiogenic VEGF and angiopoietin signaling [67]. The role of CD133 in angiogenesis was recently reported since it is observed that it regulates the expression of the angiogenic protein vascular endothelial growth factor (VEGF) by activating the Wnt/b-catenin signaling pathway and promoting greater recruitment of endothelial progenitor cells (CPEs) in CSC-enriched tumors. This mechanism increases VEGF-A and interleukin 8 (IL8) expression. Both factors cause neovascularization and tumor growth [60].
TRAIL can modulate angiogenesis as endothelial cells from tumor vasculature also express TRAIL receptors; this indicates that endothelial cells are sensitive to TRAIL apoptosis [68]. However, TRAIL modulates multiple cellular functions in endothelial cells involving the ECM necessary for vascular remodeling. TRAIL regulates FGF-2 angiogenic function in human endothelial cells (HMEC-1); FGF2 is a growth factor that activates endothelial cell proliferation, migration, and tubule formation [69]. Mice lacking TRAIL have increased vascular leakage. In vitro, TRAIL at low concentrations (10 ng/mL) reduces angiotensin II-induced oxidative stress, leukocyte adhesion, and permeability as it prevents redistribution of VE-cadherin from the cell membrane [70]. The effects induced by TRAIL involve NOX4, which participates in the generation of oxygen species and catalyzing the transfer of electrons from NADPH to O2. Via NOX4, TRAIL promotes angiogenesis by modulation of H2O2 production, eNOS phosphorylation, and NO production [71]. Low production of H2O2 from NOX4 activates MAPK family members, the TGF-β1/SMAD2/3 pathway of PI3K/AKT signaling, and cell proliferation, migration, and angiogenesis [26]. Moreover, angiogenesis induced by TRAIL can improve perfusion in ischemic disease, as TRAIL receptors are expressed by vascular smooth muscle cells and cardiomyocytes from the cardiovascular system, contributing to the pathophysiology of cardiovascular diseases. In addition, TRAIL can induce apoptosis of vascular smooth muscle cells [72].
Conversely, TRAIL administration has anti-angiogenic action, inducing tumor starvation and downregulation of OPG receptors [10,64]. sTRAIL confirmed its anti-angiogenetic potential, even higher compared to recombinant human TRAIL (rhTRAIL). Therefore, sTRAIL seems to have a double effect in this model generating PDAC cell death and reducing angiogenesis. Thus, TRAIL could induce apoptosis in tumoral and endothelial cells, even when TRAIL resistance develops. In cancer, anti-angiogenic therapy has been used to sensibilize cells to TRAIL. However, there exist different resistance mechanisms to anti-angiogenic agents that could inhibit TRAIL activity [73].
7. Regulation Mechanism
MicroRNAs (miRNAs or miRs) are a set of 18–24-nucleotide-long strands that can silence or downregulate the expression of their targets by base-pairing with the respective miRNA response elements found in the 3´UTR of the mRNA. In this way, there is a destabilization of the target mRNA; therefore, the efficiency of processing is reduced, which leads to an overall protein decrease [74]. What is even more remarkable is that a single miR is known to have hundreds if not thousands of targets that may be involved in many cell regulatory processes, including differentiation and apoptosis [75,76]. Not surprisingly, miRs have been shown to have different expression patterns when comparing cancerous with normal tissue, and even within cancer, malignant states often vary in expression [77].
TRAIL is a member of the TNF family, which, when activated, can induce apoptosis in tumor cells with no cytotoxicity to normal cells [78]. Unfortunately, many human cancer cells are resistant to TRAIL-induced apoptosis; hence, pharmacological studies have had significant drawbacks. Nonetheless, there is a silver lining as researchers are currently unraveling the different miRs involved in TRAIL regulation and TRAIL-induced apoptosis, which could, in turn, become either targets of TRAIL resistance or direct targets that induce TRAIL-induced apoptosis [78,79]. Interestingly, TRAIL resistance seems to be enhanced by PTEN and TIMP3 downregulation. To achieve this, the cluster of miR-221/222 promotes the phosphorylation of Akt, enriching the population of CD44+ cells, which are known to enhance invasion and tumorgenicity [27,80,81]. In addition, miR-221 can also downregulate proapoptotic, Bcl-2-modifying factor (Bmf), and p53 upregulated modulator of apoptosis (PUMA) [82]. Moreover, miR-221 has been detected in several cancer pathologies and has been identified in high levels in peripheral blood, making it an excellent biomarker for early detection [83]. We should note that although the mechanisms are not yet fully determined, it has been shown that BMF and certain energy enzymes are involved in TRAIL-induced necrosis, most likely through the TNF-R1 via activation of RIPKs, which promote mitochondrial fragmentation through MLKL and PGAM5 [69,76]. Opposing this activity, the activation of miR-125b, miR-224, and miR-122 can target Mcl-1 and Bcl-w, both anti-apoptotic factors [27,84,85].
Another interesting regulator in TRAIL apoptosis is miR-25, as it has been implicated to block TRAIL death receptor (DR) 4, thereby blocking induced apoptosis. Additionally, predictive analysis has also confirmed Bim and Mcl-1 as targets for miR-25 [86,87]. In the case of DR4, bioinformatic analysis has determined direct targeting of the 3´UTR of DR4 by miR-25 [86]. Moreover, DR4 can also be repressed by Hedgehog signaling Gl3, thereby serving as an antagonist to TRAIL-induced apoptosis [88]. miR-25 is associated with the sensitivity of liver cancer stem cells to TRAIL-induced apoptosis. Studies have reported that the knockdown of miR-25 promotes TRAIL-induced apoptosis by inhibiting the PI3K/Akt/Bad signaling pathway through the miR-25/PTEN axis. The combination of anti-miR-25 and TRAIL may represent a novel strategy for treating LCSCs [89].
PTEN has a key function in the regulation of cell survival pathways, such as the aforementioned PI3K/AKT/mTOR and MAPK pathways; its inhibition by different mi-RNAs (miR-21, miR-221, miR-23b, miR-214) has been associated with resistance to chemotherapeutic agents, as well as proapoptotic mechanisms, such as those induced by TRAIL [90]. In addition, it inhibits metastasis development, invasion, and angiogenesis [29,91,92]. Meanwhile, miR-25-3p (part of the miR-25 cluster) has been shown to promote malignant phenotypes by also regulating the PTEN/Akt pathway and the promotion of the epithelial–mesenchymal transition similarly, as does miR-92a in non-small-cell lung cancer cells (NSCLC) and miR-129-5p in retinoblastomas by targeting PAX6 [93,94,95]. In addition, Wan et al. showed that miR-25-3p can induce Vimentin and Snail and suppress E-cadherin, which enhances invasiveness [86,96].
MiR-148a has an interesting effect on cancer, as it has been demonstrated to both reduce tumorigenesis and induce TRAIL apoptosis. Particularly, MMP15 and ROCK1, crucial players in invasion, have been shown as direct targets of miR-148a [97]. In addition, the NF-κB/p65 pathway, which leads to TRAIL resistance, has been previously shown to be under the control of miR-30c, miR-100, and miR-21 [97,98]. Partial elucidation of the mechanism of resistance by miR-21 involves downregulation of caspase-8, which blocks receptor-interacting protein-1 cleavage; meanwhile, miR-30 involves direct binding to the 3’UTR of metastasis-associated protein-1, promoting invasion [99]. Finally, miR-100 has been shown to target mTOR, a key regulator of motility by the PI3K/Akt pathway, which leads to the regulation of 4E-BP1 and p70S6K pathways. Interestingly, p70S6K is a cell cycle effector that directly regulates mRNA in cell cycle progression [100].
TRAIL-mediated apoptosis in prostate cancer seems to correlate directly with the expression of miR-135a-3p. Shin et al. investigated the role of Tanshinone I. Their research concluded that co-treatment directly with TRAIL upregulates DR5 and miR-135a-3p. Moreover, when using miR-135a-3p mimics, PARP cleavage further increases, leading to an increase in apoptotic key regulator Bcl2-associated X protein (Bax) [101]. Still under investigation, there are several miRs of the miR-519 and miR-520 families that have been predicted to also indirectly activate proapoptotic factors Bax and Bak or enhance caspase 8 and 3 activity by FADD activity; in addition, KEGG analysis also shows that most of the targets of these families are associated with the PI3K/Akt pathway, similarly to miR-100, and although many of the hypothesized genes continue to require validation, both the NF-κB-inducing kinase and RELA have been confirmed [102,103].
8. Mechanism against TRAIL Resistance
TRAIL presents a limitation in its use as antitumoral therapy, as many primary tumors develop resistance to monotherapy with recombinant TRAIL and TRAIL receptor agonists [104]. Thus, the need to combine strategies to increase TRAIL sensitization and prevent resistance is clear. Table 2 shows different approaches being carried out using TRAIL as a therapeutic target in clinical trials that combine drugs or other strategies.
Table 2.
Recombinant TRAIL use in clinical trials.
| Recombinant TRAIL | Disease | Phase | Clinical Trial |
|---|---|---|---|
| Recombinant human Apo-2 ligand for injection | Non-small-cell lung cancer (NSCLC) stage IV | 3 | NCT03083743 |
| Recombinant human TRAIL–trimer fusion protein (SCB-313) | Malignant pleural effusions | 1 | NCT038669697 |
| Peritoneal malignancies | 1 | NCT03443674 | |
| Peritoneal carcinomatosis | 1 | NCT04047771 | |
| rhApo2L/TRAIL (AMG 951) with chemotherapy bevacizumab | Non-small-cell lung cancer (NSCLC) | 2 | NCT00508625 |
| Dulanermin plus rituximab | Non-Hodgkin’s lymphoma | 1, 2 | NCT00400764 |
| Dulanermin plus Camptosar® /Erbitux® or FOLFIRI | Metastatic colorectal cancer | 1 | NCT00671372 |
| Dulanermin with FOLFOX and bevacizumab | Metastatic colorectal cancer | 1 | NCT00873756 |
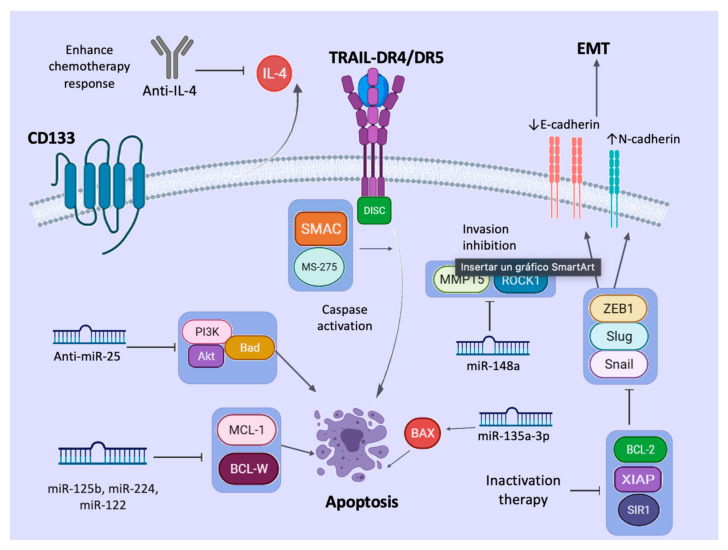
Targeting CSCs by TRAIL can be difficult as fast resistance development is reported. Todaro et al. presented that CD133+ CSCs from colon carcinomas can release IL4 to prevent apoptosis. However, they can be sensitized, as Loebinger et al. showed that MSC-expressing TRAIL can migrate to tumors and reduce tumor growth and metastasis of primary cancer. The combination of TRAIL plus chemotherapy with mitoxantrone increases the synergistic effect, improving apoptosis of putative CSCs. In CSCs that produce IL4, the administration of the IL4Rα antagonist of anti-IL4 neutralizing antibodies enhances the sensitivity of CD133+ cells to chemotherapy with oxaliplatin and 5-FU [105]. As another example, MSCs expressing TRAIL inhibit metastasis of the non-small-cell lung cancer (NSCLC)-derived H460 cell line combined with Claudin-7. This small molecule regulates mitogen-activated protein kinase/extracellular signal-regulated kinase (MEK/ERK) signaling pathways. Other studies have shown that targeting of the XIAP molecule increases CSC sensitivity to TRAIL in pancreatic cancer, reducing metastasis. CD133+ CSCs from brain overexpress BCL-2 after TRAIL induction, and its knockdown enhances CSC sensitivity to TRAIL. In nasopharyngeal carcinoma, the use of a second mitochondria-derived activator of caspases (SMAC) mimics the induced inhibitor of apoptosis (IAP) degradation and enhances TRAIL apoptosis. Moreover, the knockdown of Sirtuin 1 (SIR1) sensitizes CSCs from colon cancer to TRAIL cytotoxicity [106].
Some studies have shown that TRAIL-induced apoptosis is regulated by post-translational modifications of death receptors [45]. O-glycosylation of DR4 and DR5 is proven to control the sensitivity of many cancer cells to TRAIL [36]. Subsequently, Dufour et al. reported that N-glycosylated DR4 promotes TRAIL signaling [46]. We previously found that DR5 is activated by fucosylation for TRAIL-induced apoptosis using our TRAIL variants [47]. A relationship between HDAC inhibition and glycosylation patterns has been reported. This finding can be an explanation for the increased sensitivity of TRAIL receptors in the presence of HDAC inhibitors.
Epigenetic factors, such as drug resistance and immune evasion mechanisms, allow tumor progression. Histone deacetylases (HDACs) are important promoters of TRAIL resistance via TRAIL receptors. Since HDACs are associated with changes in glycosylation patterns, O-glycosylation, N-glycosylation, and fucosylation in DR4 and DR5 receptors are necessary to improve TRAIL signaling. Thus, HDAC inhibitors have been proposed as another strategy against cancer since they maintain glycosylation in TRAIL receptors [107]. In addition, HDAC inhibitors act in synergy with TRAIL by upregulating the mitochondrial pathway; downregulating NF-kβ and its gene products, such as cyclin D1, Bcl-2, Bcl-XL, VEGF, HIF-1a, IL6, IL8, MMP-2, and MMP-9; and upregulating the pro-apoptotic proteins Bax, Bak, and p21/CIP1 and TRAIL receptors DR4 and DR5 in cancer cells [108].
It has been reported that the HDAC inhibitor MS-275 can sensitize TRAIL-resistant breast cancer xenografts in nude mice through upregulation of DR4 and DR5 TRAIL receptors, inducing apoptosis, tumor cell growth inhibition, angiogenesis, and metastasis. All these mechanisms generate a reversion of EMT, upregulate E-cadherin, and downregulate N-cadherin and transcription factors, such as Snail, Slug, and ZEB1 [108]. Moreover, the compound suberoylanilide hydroxamic acid (SAHA), another HDAC inhibitor, significantly increases the expression of Caspase-3 and the expression in MDA-MB-231 but not in MCF-7 breast cancer cells [109]. Recently, hypersensitization of CSCs to TRAIL required TRAIL-R2 and increased microenvironmental stress by the endoplasmic reticulum stress inducer celecoxib [110]. Therefore, microenvironmental modification could be a strategy to improve TRAIL sensitivity of CSCs. In addition, more research on agents that can act on CSC spheroids and thus avoid tumor progression, metastasis, and angiogenesis is needed [111].Figure 2 summarizes the different approaches that could be used against TRAIL resistance in CSCs.
Figure 2.
Mechanisms again TRAIL resistance. Therapeutic agents against TRAIL resistance by CSCs have been discovered. The use of anti-IL4 antibodies enhances the chemotherapy response. HDAC inhibitors, such as MS-275 and second mitochon-dria-derived activator of caspases (SMAC), sensitize CSCs resistant to TRAIL and potentiate apoptosis. Inactivation of BCL-2, SIR1, and XIAP inhibits EMT. Some miRNAs and anti-miRNAs could be used as additional strategies against cancer. Anti-miR-25 inhibits PI3K/Akt activation; miR-125b, miR-224, and miR-122 inhibit anti-apoptotic proteins MCL-1 and BCL-W; miR-135a-3p activates pro-apoptotic proteins, such as BAX; and miR-148a inhibits proteins related to inva-sion of CSCs, such as MMP15 and ROCK1. Created with BioRender.com (accessed on 25 May 2021).
9. Conclusions
Cancer treatments have evolved; however, cancer cells have developed several resistance mechanisms. TRAIL research demonstrates that this protein can induce tumor cell apoptosis of a wide variety of cancers when used as a recombinant TRAIL or TRAIL receptor agonist. CSC populations inside tumors have developed ways to evade this mechanism and activate survival pathways, proliferation, and angiogenesis that allow tumor progression. Likewise, CSCs can modulate the microenvironment to improve immune cell and cytokine recruitment, hypoxia, and the action of microRNAs generated by those cells. Thus, a reaction strategy has been developed that uses the combination of drugs and chemotherapeutic agents to increase CSC sensitivity to TRAIL and thereby facilitate its elimination, which reduces metastasis.
Acknowledgments
Special thanks to personal of Support Publication Scientific, Facultad de Medicina, UANL your time and expertise in reviewing this manuscript.
Abbreviations
| ABCG5 | ATP-binding cassette transporter |
| APAF-1 | Apoptotic protease activating factor 1 |
| AP1 | Activator protein 1 |
| Apo2L | Apo-2 ligand |
| Bcl-2 | B-cell lymphoma 2 |
| BPM | Bone morphogenetic protein |
| CAD | Caspase-activated DNase |
| CAF | Cancer-associated fibroblasts |
| CRC | Colorectal cancer |
| CRD | Cysteine-rich domain |
| CSCs | Cancer stem cells |
| CTLs | Cytotoxic T cells |
| DAMPs | Damage-associated molecular patterns |
| DCs | Dendritic cells |
| DED | Death-inducing signaling complex |
| DCRs | Decoy receptors |
| DD | Death domain |
| DISC | Death-inducing signaling complex |
| DKK-1 | Dickkopf-1 |
| DR | Death receptor |
| EGF | Epidermal growth factor |
| ECM | Extracellular matrix |
| EMT | Epithelial–mesenchymal transition |
| EMILIN2 | Elastin microfibril interface-located protein 2 |
| FADD | Fas-associated death domain |
| FLIP | FLICE-like inhibitory protein |
| FOX | Forkhead Box |
| HGF | Hepatocyte growth factor |
| HIF-1α | Hypoxia-inducible 1alpha |
| ICAD | Inhibitor of caspase-activated DNase |
| IFN-β | Interferon-β |
| IL8 | Interleukin 8 |
| MAPK | mitogen-activated protein kinase |
| MDP | membrane-proximal domain |
| MDSC | myeloid-derived suppressor cells |
| MET | mesenchymal–epithelial transition |
| miRNAs or miRs | microRNAs |
| MMP12 | matrix metallopeptidase 12 |
| MSCs | Mesenchymal stem cells |
| NFAT | Nuclear factor of activated T cells |
| NK | Natural killer |
| NO | Nitric oxide |
| NSCLC | Non-small-cell lung cancer |
| OPG | Osteoprotegerin |
| PDGF | Platelet-derived growth factor |
| PI3K | Phosphatidylinositol-3-kinase |
| PTEN | Phosphatase and tensin homolog |
| rhTRAIL | Recombinant human TRAIL |
| sTRAIL | Soluble TRAIL |
| TAMs | Tumor-associated macrophages |
| TGF-β | Transforming growth factor-beta |
| Tregs | Regulatory T cells |
| TILs | Tumor-infiltrating lymphocytes |
| VEGF | Vascular endothelial growth factor |
| TNF | Tumor necrosis factor |
| TRAF2 | Tumor receptor-associated factor 2 |
| TRAIL | Tumor necrosis factor (TNF)-related apoptosis-inducing ligand |
| TNF-α | Tumor necrosis factor-alpha |
| VCAM-1 | Vascular cell adhesion molecule-1 |
| VEGF | Vascular endothelial growth factor |
Author Contributions
A.G.Q.-R. designed the images and wrote, analyzed, and corrected the manuscript. P.D.-G. made the literature analysis and wrote and discussed the revised manuscript of this review. J.F.I. and J.L.D.G. made the literature analysis, wrote part of the text. J.H.M.G. corrected and revised the manuscript. E.N.G.-T. supervised, directed, and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
All authors indicated no potential conflicts of interest in publishing this manuscript.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Johnstone R.W., Ruefli A.A., Lowe S.W. Apoptosis: A link between cancer genetics and chemotherapy. Cell. 2002;108:153–164. doi: 10.1016/S0092-8674(02)00625-6. [DOI] [PubMed] [Google Scholar]
- 2.Elmore S. Apoptosis: A review of programmed cell death. Toxicol. Pathol. 2007;35:495–516. doi: 10.1080/01926230701320337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong S.H.M., Kong W.Y., Fang C.-M., Loh H.-S., Chuah L.-H., Abdullah S., Ngai S.C. The TRAIL to cancer therapy: Hindrances and potential solutions. Crit. Rev. Oncol. 2019;143:81–94. doi: 10.1016/j.critrevonc.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Teringova E., Tousek P. Apoptosis in ischemic heart disease. J. Transl. Med. 2017;15:87. doi: 10.1186/s12967-017-1191-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holoch P.A., Griffith T.S. TNF-related apoptosis-inducing ligand (TRAIL): A new path to anti-cancer therapies. Eur. J. Pharmacol. 2009;625:63–72. doi: 10.1016/j.ejphar.2009.06.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Labsch S., Liu L., Bauer N., Zhang Y., Aleksandrowicz E., Gladkich J., Schönsiegel F., Herr I. Sulforaphane and TRAIL induce a synergistic elimination of advanced prostate cancer stem-like cells. Int. J. Oncol. 2014;44:1470–1480. doi: 10.3892/ijo.2014.2335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naval J., de Miguel D., Gallego-Lleyda A., Anel A., Martinez-Lostao L. Importance of TRAIL molecular anatomy in receptor oligomerization and signaling. Implications for cancer therapy. Cancers. 2019;11:444. doi: 10.3390/cancers11040444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Merino D., Lalaoui N., Morizot A., Solary E., Micheau O. TRAIL in cancer therapy: Present and future challenges. Expert Opin. Ther. Targets. 2007;11:1299–1314. doi: 10.1517/14728222.11.10.1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu J., Gao Q., Xie T., Liu Y., Luo L., Xu C., Shen L., Wan F., Lei T., Ye F. Synergistic effect of TRAIL and irradiation in elimination of glioblastoma stem-like cells. Clin. Exp. Med. 2018;18:399–411. doi: 10.1007/s10238-018-0504-7. [DOI] [PubMed] [Google Scholar]
- 10.De Looff M., de Jong S., Kruyt F.A.E. Multiple interactions between cancer cells and the tumor microenvironment modulate trail signaling: Implications for TRAIL receptor targeted therapy. Front. Immunol. 2019;10:1530. doi: 10.3389/fimmu.2019.01530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yuan X., Gajan A., Chu Q., Xiong H., Wu K., Wu G.S. Developing TRAIL/TRAIL death receptor-based cancer therapies. Cancer Metastasis Rev. 2018;37:733–748. doi: 10.1007/s10555-018-9728-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Behrooz A.B., Syahir A., Ahmad S. CD133: Beyond a cancer stem cell biomarker. J. Drug Target. 2019;27:257–269. doi: 10.1080/1061186X.2018.1479756. [DOI] [PubMed] [Google Scholar]
- 13.Zhang R., Xu J., Zhao J., Bai J. Knockdown of miR-27a sensitizes colorectal cancer stem cells to TRAIL by promoting the formation of Apaf-1-caspase-9 complex. Oncotarget. 2017;8:45213–45223. doi: 10.18632/oncotarget.16779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Miguel D., Lemke J., Anel A., Walczak H., Martinez-Lostao L. Onto better TRAILs for cancer treatment. Cell Death Differ. 2016;23:733–747. doi: 10.1038/cdd.2015.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sahlberg S.H., Spiegelberg D., Glimelius B., Stenerlöw B., Nestor M. Evaluation of cancer stem cell markers CD133, CD44, CD24: Association with AKT isoforms and radiation resistance in colon cancer cells. PLoS ONE. 2014;9:e94621. doi: 10.1371/journal.pone.0094621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim W.-T., Ryu A.C.J. Cancer stem cell surface markers on normal stem cells. BMB Rep. 2017;50:285–298. doi: 10.5483/BMBRep.2017.50.6.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh M., Yelle N., Venugopal C., Singh S.K. EMT: Mechanisms and therapeutic implications. Pharmacol. Ther. 2018;182:80–94. doi: 10.1016/j.pharmthera.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 18.Kim T., Veronese A., Pichiorri F., Lee T.J., Jeon Y.-J., Volinia S., Pineau P., Marchio A., Palatini J., Suh S.-S., et al. p53 regulates epithelial–mesenchymal transition through microRNAs targeting ZEB1 and ZEB. J. Exp. Med. 2011;208:875–883. doi: 10.1084/jem.20110235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Babaei G., Aziz S.G.-G., Jaghi N.Z.Z. EMT, cancer stem cells and autophagy; The three main axes of metastasis. Biomed. Pharmacother. 2021;133:110909. doi: 10.1016/j.biopha.2020.110909. [DOI] [PubMed] [Google Scholar]
- 20.Zhao X., Sun B., Sun D., Liu T., Che N., Gu Q., Dong X., Li R., Liu Y., Li J. Slug promotes hepatocellular cancer cell progression by increasing sox2 and nanog expression. Oncol. Rep. 2014;33:149–156. doi: 10.3892/or.2014.3562. [DOI] [PubMed] [Google Scholar]
- 21.Javaeed A., Ghauri S.K. Metastatic potential and prognostic significance of SOX2: A meta-analysis. World J. Clin. Oncol. 2019;10:234–246. doi: 10.5306/wjco.v10.i6.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou P., Li B., Liu F., Zhang M., Wang Q., Liu Y., Yao Y., Li D. The epithelial to mesenchymal transition (EMT) and cancer stem cells: Implication for treatment resistance in pancreatic cancer. Mol. Cancer. 2017;16:1–11. doi: 10.1186/s12943-017-0624-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stantic M., Zobalova R., Prokopova K., Neuzil J., Dong L.-F. Cancer cells with high expression of CD133 exert FLIP upregulation and resistance to TRAIL-induced apoptosis. BioFactors. 2008;34:231–235. doi: 10.1002/biof.5520340307. [DOI] [PubMed] [Google Scholar]
- 24.Clara J.A., Monge C., Yang Y., Takebe N. Targeting signalling pathways and the immune microenvironment of cancer stem cells—a clinical update. Nat. Rev. Clin. Oncol. 2020;17:204–232. doi: 10.1038/s41571-019-0293-2. [DOI] [PubMed] [Google Scholar]
- 25.Akbari M., Shanehbandi D., Asadi M., Shomali N., Faraji A., Khaze V., Pakdel A., Mokhtarzadeh A., Ebrahimi A.A., Shabani A., et al. Effects of CD133 silencing on survival and migration of HT-29 colorectal cancer cells. Iran. J. Immunol. 2019;16:246–257. doi: 10.22034/IJI.2019.80275. [DOI] [PubMed] [Google Scholar]
- 26.Garofalo M., di Leva G., Romano G., Nuovo G., Suh S.-S., Ngankeu A., Taccioli C., Pichiorri F., Alder H., Secchiero P., et al. miR-221&222 Regulate TRAIL resistance and enhance tumorigenicity through PTEN and TIMP3 downregulation. Cancer Cell. 2009;16:498–509. doi: 10.1016/j.ccr.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 27.Hartwig T., Montinaro A., von Karstedt S., Sevko A., Surinova S., Chakravarthy A., Taraborrelli L., Draber P., Lafont E., Vargas F.A., et al. The TRAIL-induced cancer secretome promotes a tumor-supportive immune microenvironment via CCR. Mol. Cell. 2017;65:730–742.e5. doi: 10.1016/j.molcel.2017.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang J., Chen D., Liang S., Wang J., Liu C., Nie C., Shan Z., Wang L., Fan Q., Wang F. miR-106b promotes cell invasion and metastasis via PTEN mediated EMT in ESCC. Oncol. Lett. 2018;15:4619–4626. doi: 10.3892/ol.2018.7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prabhu V.V., Allen J.E., Dicker D.T., El-Deiry W.S. Small molecule ONC201/TIC10 targets chemotherapy-resistant colorectal cancer stem-like cells in an Akt/Foxo3a/TRAILdependent manner. Cancer Res. 2015;75:1423–1432. doi: 10.1158/0008-5472.CAN-13-3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.French R., Hayward O., Jones S., Yang W., Clarkson R. Cytoplasmic levels of cFLIP determine a broad susceptibility of breast cancer stem/progenitor-like cells to TRAIL. Mol. Cancer. 2015;14:1–13. doi: 10.1186/s12943-015-0478-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jalving M., Heijink D.M., Koornstra J.J., Ek W.B.-V., Zwart N., Wesseling J., Sluiter W.J., de Vries E.G.E., Kleibeuker J.H., de Jong S. Regulation of TRAIL receptor expression by -catenin in colorectal tumours. Carcinogenesis. 2013;35:1092–1099. doi: 10.1093/carcin/bgt484. [DOI] [PubMed] [Google Scholar]
- 32.Coelho B.P., Fernandes C.F.D.L., Boccacino J.M., Souza M.C.D.S., Melo-Escobar M.I., Alves R.N., Prado M.B., Iglesia R.P., Cangiano G., Mazzaro G.L.R., et al. Multifaceted WNT signaling at the crossroads between epithelial-mesenchymal transition and autophagy in glioblastoma. Front. Oncol. 2020;10:597743. doi: 10.3389/fonc.2020.597743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu J., Zhou J.-Y., Wei W.-Z., Wu G.S. Activation of the akt survival pathway contributes to TRAIL resistance in cancer cells. PLoS ONE. 2010;5:e10226. doi: 10.1371/journal.pone.0010226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sophonnithiprasert T., Nilwarangkoon S., Nakamura Y., Watanapokasin R. Goniothalamin enhances TRAIL-induced apoptosis in colorectal cancer cells through DR5 upregulation and cFLIP downregulation. Int. J. Oncol. 2015;47:2188–2196. doi: 10.3892/ijo.2015.3204. [DOI] [PubMed] [Google Scholar]
- 35.Pretzsch E., Bösch F., Neumann J., Ganschow P., Bazhin A., Guba M., Werner J., Angele M. Mechanisms of metastasis in colorectal cancer and metastatic organotropism: Hematogenous versus peritoneal spread. J. Oncol. 2019;2019:7407190. doi: 10.1155/2019/7407190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hui L., Chen Y. Tumor microenvironment: Sanctuary of the devil. Cancer Lett. 2015;368:7–13. doi: 10.1016/j.canlet.2015.07.039. [DOI] [PubMed] [Google Scholar]
- 37.Zwirner N.W., Ziblat A. Regulation of NK cell activation and effector functions by the IL-12 family of cytokines: The case of IL-27. Front. Immunol. 2017;8:25. doi: 10.3389/fimmu.2017.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Griffith B.T.S., Wiley S.R., Kubin M.Z., Sedger L.M., Maliszewski C.R., Fanger N.A. Monocyte-mediated tumoricidal activity via the tumor necrosis factor-related cytokine, TRAIL. Cell. 1999;189:1343–1353. doi: 10.1084/jem.189.8.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tecchio C., Huber V., Scapini P., Calzetti F., Margotto D., Todeschini G., Pilla L., Martinelli G., Pizzolo G., Rivoltini L., et al. IFNα-stimulated neutrophils and monocytes release a soluble form of TNF-related apoptosis-inducing ligand (TRAIL/Apo-2 ligand) displaying apoptotic activity on leukemic cells. Blood. 2004;103:3837–3844. doi: 10.1182/blood-2003-08-2806. [DOI] [PubMed] [Google Scholar]
- 40.Kessenbrock K., Plaks V., Werb Z. Matrix metalloproteinases: Regulators of the tumor. Cell. 2010;141:52–67. doi: 10.1016/j.cell.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Secchiero P., Gonelli A., Mirandola P., Melloni E., Zamai L., Celeghini C., Milani D., Zauli G. Tumor necrosis factor-related apoptosis-inducing ligand induces monocytic maturation of leukemic and normal myeloid precursors through a caspase-dependent pathway. Blood. 2002;100:2421–2429. doi: 10.1182/blood-2002-01-0047. [DOI] [PubMed] [Google Scholar]
- 42.Wu A.A., Drake V., Huang A., Chiu S., Zheng L. Reprogramming the tumor microenvironment: Tumor-induced immunosuppressive factors paralyze T cells. OncoImmunology. 2015;4:e1016700. doi: 10.1080/2162402X.2015.1016700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Winde C.M., Munday C., Acton S.E. Molecular mechanisms of dendritic cell migration in immunity and cancer. Med. Microbiol. Immunol. 2020;209:515–529. doi: 10.1007/s00430-020-00680-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fanger N.A., Maliszewski C.R., Schooley K., Griffith T.S. Human dendritic cells mediate cellular apoptosis via tumor necrosis factor–related apoptosis-inducing ligand (trail) J. Exp. Med. 1999;190:1155–1164. doi: 10.1084/jem.190.8.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rossin A., Miloro G., Hueber A.-O. TRAIL and FasL functions in cancer and autoimmune diseases: Towards an increasing complexity. Cancers. 2019;11:639. doi: 10.3390/cancers11050639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vinay D.S., Ryan E.P., Pawelec G., Talib W.H., Stagg J., Elkord E., Lichtor T., Decker W.K., Whelan R.L., Kumara H.M.C.S., et al. Immune evasion in cancer: Mechanistic basis and therapeutic strategies. Semin. Cancer Biol. 2015;35:S185–S198. doi: 10.1016/j.semcancer.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 47.Facciabene A., Motz G.T., Coukos G. T-Regulatory Cells: Key players in tumor immune escape and angiogenesis: Figure. Cancer Res. 2012;72:2162–2171. doi: 10.1158/0008-5472.CAN-11-3687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hallett M.A., Venmar K.T., Fingleton B. Cytokine stimulation of epithelial cancer cells: The similar and divergent functions of IL-4 and IL-13. Cancer Res. 2012;72:6338–6343. doi: 10.1158/0008-5472.CAN-12-3544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jeong J.-H., Ojha U., Lee Y.M. Pathological angiogenesis and inflammation in tissues. Arch. Pharmacal. Res. 2021;44:1–15. doi: 10.1007/s12272-020-01287-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lugano R., Ramachandran M., Dimberg A. Tumor angiogenesis: Causes, consequences, challenges and opportunities. Cell. Mol. Life Sci. 2019;77:1745–1770. doi: 10.1007/s00018-019-03351-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Plaks V., Kong N., Werb Z. The cancer stem cell niche: How essential is the niche in regulating stemness of tumor cells? Cell Stem Cell. 2015;16:225–238. doi: 10.1016/j.stem.2015.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Annan D.A.-M., Kikuchi H., Maishi N., Hida Y., Hida K. Tumor endothelial cell—A biological tool for translational cancer research. Int. J. Mol. Sci. 2020;21:3238. doi: 10.3390/ijms21093238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhao Y., Bao Q., Renner A., Camaj P., Eichhorn M., Ischenko I., Angele M., Kleespies A., Jauch K.-W., Bruns C. Cancer stem cells and angiogenesis. Int. J. Dev. Biol. 2011;55:477–482. doi: 10.1387/ijdb.103225yz. [DOI] [PubMed] [Google Scholar]
- 54.Ping Y.-F., Zhang X., Bian X.-W. Cancer stem cells and their vascular niche: Do they benefit from each other? Cancer Lett. 2016;380:561–567. doi: 10.1016/j.canlet.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 55.Jun J.C., Rathore A., Younas H., Gilkes D., Polotsky V.Y. Hypoxia-inducible factors and cancer. Curr. Sleep Med. Rep. 2017;3:1–10. doi: 10.1007/s40675-017-0062-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vallée A., Guillevin R., Vallée J.-N. Vasculogenesis and angiogenesis initiation under normoxic conditions through Wnt/β-catenin pathway in gliomas. Rev. Neurosci. 2017;29:71–91. doi: 10.1515/revneuro-2017-0032. [DOI] [PubMed] [Google Scholar]
- 57.Rivera L.B., Bergers G. Myeloid cell-driven angiogenesis and immune regulation in tumors. Trends Immunol. 2015;36:240–249. doi: 10.1016/j.it.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen P.-L., Easton A.S. Evidence that tumor necrosis factor-related apoptosis inducing ligand (TRAIL) inhibits angiogenesis by inducing vascular endothelial cell apoptosis. Biochem. Biophys. Res. Commun. 2010;391:936–941. doi: 10.1016/j.bbrc.2009.11.168. [DOI] [PubMed] [Google Scholar]
- 59.Cartland S.P., Genner S.W., Zahoor A., Kavurma M.M. Comparative Evaluation of TRAIL, FGF-2 and VEGF-A-induced angiogenesis in vitro and in vivo. Int. J. Mol. Sci. 2016;17:2025. doi: 10.3390/ijms17122025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Patil M.S., Cartland S.P., Kavurma M.M. TRAIL signals, extracellular matrix and vessel remodelling. Vasc. Biol. 2020;2:R73–R84. doi: 10.1530/VB-20-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.di Bartolo B., Cartland S., Prado-Lourenco L., Griffith T.S., Gentile C., Ravindran J., Azahri N.S.M., Thai T., Yeung A.W.S., Thomas S.R., et al. Tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) promotes angiogenesis and ischemia-induced neovascularization via NADPH oxidase 4 (NOX4) and nitric oxide-dependent mechanisms. J. Am. Hear. Assoc. 2015;4:e002527. doi: 10.1161/JAHA.115.002527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Goncalves I., Singh P., Tengryd C., Cavalera M., Mattisson I.Y., Nitulescu M., Persson A.F., Volkov P., Engström G., Orho-Melander M., et al. sTRAIL-R2 (soluble TNF [tumor necrosis factor]-related apoptosis-inducing ligand receptor 2) a marker of plaque cell apoptosis and cardiovascular events. Stroke. 2019;50:1989–1996. doi: 10.1161/STROKEAHA.119.024379. [DOI] [PubMed] [Google Scholar]
- 63.Chen C., Li L., Zhou H.J., Min W. The role of NOX4 and TRX2 in angiogenesis and their potential cross-talk. Antioxidants. 2017;6:42. doi: 10.3390/antiox6020042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Islas J.F., Moreno-Cuevas J.E. A microRNA perspective on cardiovascular development and diseases: An update. Int. J. Mol. Sci. 2018;19:2075. doi: 10.3390/ijms19072075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Xu L., Leng H., Shi X., Ji J., Fu J. MiR-155 promotes cell proliferation and inhibits apoptosis by PTEN signaling pathway in the psoriasis. Biomed. Pharmacother. 2017;90:524–530. doi: 10.1016/j.biopha.2017.03.105. [DOI] [PubMed] [Google Scholar]
- 66.Hamada S., Masamune A., Miura S., Satoh K., Shimosegawa T. MiR-365 induces gemcitabine resistance in pancreatic cancer cells by targeting the adaptor protein SHC1 and pro-apoptotic regulator BAX. Cell. Signal. 2014;26:179–185. doi: 10.1016/j.cellsig.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 67.Lujambio A., Lowe S.W. The microcosmos of cancer. Nat. Cell Biol. 2012;482:347–355. doi: 10.1038/nature10888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lu T., Shao N., Ji C. Targeting microRNAs to modulate TRAIL-induced apoptosis of cancer cells. Cancer Gene Ther. 2012;20:33–37. doi: 10.1038/cgt.2012.81. [DOI] [PubMed] [Google Scholar]
- 69.Xiao F., Chen J., Lian C., Han P., Zhang C. Tumor necrosis factor-related apoptosis-inducing ligand induces cytotoxicity specific to osteosarcoma by microRNA response elements. Mol. Med. Rep. 2014;11:739–745. doi: 10.3892/mmr.2014.2710. [DOI] [PubMed] [Google Scholar]
- 70.Zhou R., Yuan P., Wang Y., Hunsberger J.G., Elkahloun A., Wei Y., Damschroder-Williams P., Du J., Chen G., Manji H.K. Evidence for selective microRNAs and their effectors as common long-term targets for the actions of mood stabilizers. Neuropsychopharmacology. 2008;34:1395–1405. doi: 10.1038/npp.2008.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li D., Ji L., Liu L., Liu Y., Hou H., Yu K., Sun Q., Zhao Z. Characterization of circulating microRNA expression in patients with a ventricular septal defect. PLoS ONE. 2014;9:e106318. doi: 10.1371/journal.pone.0106318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Villanova L., Careccia S., De Maria R., Fiori M.E. Micro-economics of apoptosis in cancer: ncRNAs modulation of BCL-2 family members. Int. J. Mol. Sci. 2018;19:958. doi: 10.3390/ijms19040958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Xie X., Huang Y., Chen L., Wang J. miR-221 regulates proliferation and apoptosis of ovarian cancer cells by targeting BMF. Oncol. Lett. 2018;16:6697–6704. doi: 10.3892/ol.2018.9446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Voigt S., Philipp S., Davarnia P., Winoto-Morbach S., Röder C., Arenz C., Trauzold A., Kabelitz D., Schütze S., Kalthoff H., et al. TRAIL-induced programmed necrosis as a novel approach to eliminate tumor cells. BMC Cancer. 2014;14:74. doi: 10.1186/1471-2407-14-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sun J., Lu H., Wang X., Jin H. MicroRNAs in hepatocellular carcinoma: Regulation, function, and clinical implications. Sci. World J. 2013;2013:1–14. doi: 10.1155/2013/924206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Razumilava N., Bronk S.F., Smoot R.L., Fingas C.D., Werneburg N.W., Roberts L., Mott J.L. miR-25 targets TNF-related apoptosis inducing ligand (TRAIL) death receptor-4 and promotes apoptosis resistance in cholangiocarcinoma. Hepatology. 2012;55:465–475. doi: 10.1002/hep.24698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zeng Z., Li Y., Pan Y., Lan X., Song F., Sun J., Zhou K., Liu X., Ren X., Wang F., et al. Cancer-derived exosomal miR-25-3p promotes pre-metastatic niche formation by inducing vascular permeability and angiogenesis. Nat. Commun. 2018;9:1–14. doi: 10.1038/s41467-018-07810-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kurita S., Mott J.L., Almada L.L., Bronk S.F., Werneburg N.W., Sun S.-Y., Roberts L.R., Fernandez-Zapico M.E., Gores G.J. GLI3-dependent repression of DR4 mediates hedgehog antagonism of TRAIL-induced apoptosis. Oncogene. 2010;29:4848–4858. doi: 10.1038/onc.2010.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Feng X., Jiang J., Shi S., Xie H., Zhou L., Zheng S. Knockdown of miR-25 increases the sensitivity of liver cancer stem cells to TRAIL-induced apoptosis via PTEN/PI3K/Akt/Bad signaling pathway. Int. J. Oncol. 2016;49:2600–2610. doi: 10.3892/ijo.2016.3751. [DOI] [PubMed] [Google Scholar]
- 80.Panner A., Crane C.A., Weng C., Feletti A., Parsa A.T., Pieper R.O. A novel PTEN-dependent link to ubiquitination controls FLIPS stability and TRAIL sensitivity in glioblastoma multiforme. Cancer Res. 2009;69:7911–7916. doi: 10.1158/0008-5472.CAN-09-1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.El Sharkawi F.Z., Ewais S.M., Fahmy R.H., Rashed L.A. PTEN and TRAIL genes loaded zein nanoparticles as potential therapy for hepatocellular carcinoma. J. Drug Target. 2017;25:513–522. doi: 10.1080/1061186X.2017.1289536. [DOI] [PubMed] [Google Scholar]
- 82.Wang H., Xu C., Kong X., Li X., Kong X., Wang Y., Ding X., Yang Q. Trail resistance induces epithelial-mesenchymal transition and enhances invasiveness by suppressing PTEN via miR-221 in breast cancer. PLoS ONE. 2014;9:e99067. doi: 10.1371/journal.pone.0099067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lu C., Shan Z., Hong J., Yang L. MicroRNA-92a promotes epithelial-mesenchymal transition through activation of PTEN/PI3K/AKT signaling pathway in non-small cell lung cancer metastasis. Int. J. Oncol. 2017;51:235–244. doi: 10.3892/ijo.2017.3999. [DOI] [PubMed] [Google Scholar]
- 84.Fu F., Jiang W., Zhou L., Chen Z. Circulating exosomal miR-17-5p and miR-92a-3p predict pathologic stage and grade of colorectal cancer. Transl. Oncol. 2018;11:221–232. doi: 10.1016/j.tranon.2017.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu Y., Liang G., Wang H., Liu Z. MicroRNA-129-5p suppresses proliferation, migration and invasion of retinoblastoma cells through PI3K/AKT signaling pathway by targeting PAX6. Pathol. Res. Pr. 2019;215:152641. doi: 10.1016/j.prp.2019.152641. [DOI] [PubMed] [Google Scholar]
- 86.Zi Y., Zhang Y., Wu Y., Zhang L., Yang R., Huang Y. Downregulation of microRNA-25-3p inhibits the proliferation and promotes the apoptosis of multiple myeloma cells via targeting the PTEN/PI3K/AKT signaling pathway. Int. J. Mol. Med. 2020;47:1. doi: 10.3892/ijmm.2020.4841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Joshi P., Jeon Y.-J., Laganà A., Middleton J., Secchiero P., Garofalo M., Croce C.M. MicroRNA-148a reduces tumorigenesis and increases TRAIL-induced apoptosis in NSCLC. Proc. Natl. Acad. Sci. USA. 2015;112:8650–8655. doi: 10.1073/pnas.1500886112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Farooqi A.A., Gadaleta C.D., Ranieri G., Fayyaz S., Marech I. New frontiers in promoting TRAIL-mediated cell death: Focus on natural sensitizers, miRNAs, and nanotechnological advancements. Cell Biophys. 2015;74:3–10. doi: 10.1007/s12013-015-0712-7. [DOI] [PubMed] [Google Scholar]
- 89.Xia Y., Chen Q., Zhong Z., Xu C., Wu C., Liu B., Chen Y. Down-regulation of MiR-30c promotes the invasion of non-small cell lung cancer by targeting MTA1. Cell. Physiol. Biochem. 2013;32:476–485. doi: 10.1159/000354452. [DOI] [PubMed] [Google Scholar]
- 90.Xu C., Zeng Q., Xu W., Jiao L., Chen Y., Zhang Z., Wu C., Jin T., Pan A., Wei R., et al. miRNA-100 inhibits human bladder urothelial carcinogenesis by directly targeting mTOR. Mol. Cancer Ther. 2013;12:207–219. doi: 10.1158/1535-7163.MCT-12-0273. [DOI] [PubMed] [Google Scholar]
- 91.Shin E.A., Sohn E.J., Won G., Choi J.-U., Jeong M., Kim B., Kim M.-J., Kim S.-H. Upregulation of microRNA135a-3p and death receptor 5 plays a critical role in Tanshinone I sensitized prostate cancer cells to TRAIL induced apoptosis. Oncotarget. 2014;5:5624–5636. doi: 10.18632/oncotarget.2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kim Y., Schwabe R., Qian T., Lemasters. J., Brenner D. TRAIL-mediated apoptosis requires NF-kappaB inhibition and the mitochondrial permeability transition in human hepatoma cells. Hepatology. 2002;36:1498–1508. doi: 10.1053/jhep.2002.36942. [DOI] [PubMed] [Google Scholar]
- 93.Nguyen P.N.N., Huang C.-J., Sugii S., Cheong S.K., Choo K.B. Selective activation of miRNAs of the primate-specific chromosome 19 miRNA cluster (C19MC) in cancer and stem cells and possible contribution to regulation of apoptosis. J. Biomed. Sci. 2017;24:1–14. doi: 10.1186/s12929-017-0326-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ralff M.D., El-Deiry W.S. TRAIL pathway targeting therapeutics. Expert Rev. Precis. Med. Drug Dev. 2018;3:197–204. doi: 10.1080/23808993.2018.1476062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Han L., Shi S., Gong T., Zhang Z., Sun X. Cancer stem cells: Therapeutic implications and perspectives in cancer therapy. Acta Pharm. Sin. B. 2013;3:65–75. doi: 10.1016/j.apsb.2013.02.006. [DOI] [Google Scholar]
- 96.Fakiruddin K.S., Ghazalli N., Lim M.N., Zakaria Z., Abdullah S. Mesenchymal stem cell expressing TRAIL as targeted therapy against sensitised tumour. Int. J. Mol. Sci. 2018;19:2188. doi: 10.3390/ijms19082188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang B., Liu B., Chen D., Setroikromo R., Haisma H.J., Quax W.J. Histone deacetylase inhibitors sensitize TRAIL-induced apoptosis in colon cancer cells. Cancers. 2019;11:645. doi: 10.3390/cancers11050645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Srivastava R.K., Kurzrock R., Shankar S. MS-275 Sensitizes TRAIL-resistant breast cancer cells, inhibits angiogenesis and metastasis, and reverses epithelial-mesenchymal transition in vivo. Mol. Cancer Ther. 2010;9:3254–3266. doi: 10.1158/1535-7163.MCT-10-0582. [DOI] [PubMed] [Google Scholar]
- 99.Zhou W., Feng X., Han H., Guo S., Wang G. Synergistic effects of combined treatment with histone deacetylase inhibitor suberoylanilide hydroxamic acid and TRAIL on human breast cancer cells. Sci. Rep. 2016;6:28004. doi: 10.1038/srep28004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Stöhr D., Schmid J.O., Beigl T.B., Mack A., Maichl D.S., Cao K., Budai B., Fullstone G., Kontermann R.E., Mürdter T.E., et al. Stress-induced TRAILR2 expression overcomes TRAIL resistance in cancer cell spheroids. Cell Death Differ. 2020;27:3037–3052. doi: 10.1038/s41418-020-0559-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Vinogradov S., Wei X. Cancer stem cells and drug resistance: The potential of nanomedicine. Nanomedicine. 2012;7:597–615. doi: 10.2217/nnm.12.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Han H., YunXu Z., Hou P., Jiang C., Liu L., Tang M., Yang X., Zhang Y., Liu Y. Icaritin sensitizes human glioblastoma cells to TRAIL-induced apoptosis. Cell Biophys. 2015;72:533–542. doi: 10.1007/s12013-014-0499-y. [DOI] [PubMed] [Google Scholar]
- 103.Zhang Z., Patel S.B., King M.R. Micelle-in-liposomes for sustained delivery of anticancer agents that promote potent TRAIL-induced cancer cell apoptosis. Molecules. 2020;26:157. doi: 10.3390/molecules26010157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Son Y.-G., Kim E.H., Kim J.Y., Kim S.U., Kwon T.K., Yoon A.-R., Yun C.-O., Choi K.S. Silibinin sensitizes human glioma cells to TRAIL-mediated apoptosis via DR5 up-regulation and down-regulation of c-FLIP and survivin. Cancer Res. 2007;67:8274–8284. doi: 10.1158/0008-5472.CAN-07-0407. [DOI] [PubMed] [Google Scholar]
- 105.Dai Y., Liu M., Tang W., Li Y., Lian J., Lawrence T.S., Xu L. A Smac-mimetic sensitizes prostate cancer cells to TRAIL-induced apoptosis via modulating both IAPs and NF-kappaB. BMC Cancer. 2009;9:392. doi: 10.1186/1471-2407-9-392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kim S.W., Kim S.J., Park S.H., Yang H.G., Kang M.C., Choi Y.W., Kim S.M., Jeun S.-S., Sung Y.C. Complete regression of metastatic renal cell carcinoma by multiple injections of engineered mesenchymal stem cells expressing dodecameric TRAIL and HSV-TK. Clin. Cancer Res. 2013;19:415–427. doi: 10.1158/1078-0432.CCR-12-1568. [DOI] [PubMed] [Google Scholar]
- 107.Zinnah K., Park S.-Y. Duloxetine enhances TRAIL-mediated apoptosis via AMPK-mediated inhibition of autophagy flux in lung cancer cells. Anticancer Res. 2019;39:6621–6633. doi: 10.21873/anticanres.13877. [DOI] [PubMed] [Google Scholar]
- 108.Onoe-Takahashi A., Suzuki-Karasaki M., Suzuki-Karasaki M., Ochiai T., Suzuki-Karasaki Y. Autophagy inhibitors regulate TRAIL sensitivity in human malignant cells by targeting the mitochondrial network and calcium dynamics. Int. J. Oncol. 2019;54:1734–1746. doi: 10.3892/ijo.2019.4760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kim K., Takimoto R., Dicker D., Chen Y., Gazitt Y., El-Deiry W. Enhanced TRAIL sensitivity by p53 overexpression in human cancer but not normal cell lines. Int. J. Oncol. 2001;18:241–247. doi: 10.3892/ijo.18.2.241. [DOI] [PubMed] [Google Scholar]
- 110.Hu B., Zhu H., Qiu S., Su Y., Ling W., Xiao W., Qi Y. Enhanced TRAIL sensitivity by E1A expression in human cancer and normal cell lines: Inhibition by adenovirus E1B19K and E3 proteins. Biochem. Biophys. Res. Commun. 2004;325:1153–1162. doi: 10.1016/j.bbrc.2004.10.154. [DOI] [PubMed] [Google Scholar]
- 111.Zhang X., Wang L., Liu Y., Huang W., Cheng D. MiR-760 enhances TRAIL sensitivity in non-small cell lung cancer via targeting the protein FOXA1. Biomed. Pharmacother. 2018;99:523–529. doi: 10.1016/j.biopha.2018.01.076. [DOI] [PubMed] [Google Scholar]