Abstract
This address was delivered by Samuel Dagogo-Jack, MD, President, Medicine & Science, of the American Diabetes Association (ADA), at the Association’s 75th Scientific Sessions in Boston, MA, on 7 June 2015. Dr. Dagogo-Jack is a professor of medicine and the director of the Division of Endocrinology, Diabetes and Metabolism and the director of the Clinical Research Center at The University of Tennessee Health Science Center, Memphis, TN, where he holds the A.C. Mullins Endowed Chair in Translational Research. He has been an ADA volunteer since 1991 and has served on several national committees and chaired the Association’s Research Grant Review Committee. At the local level, he has served on community leadership boards in St. Louis, MO, and Tennessee. A physician-scientist, Dr. Dagogo-Jack’s current research focuses on the interaction of genetic and environmental factors in the prediction and prevention of prediabetes, diabetes, and diabetes complications. He is the principal investigator of the Pathobiology of Prediabetes in a Biracial Cohort (POP-ABC) study and also directs The University of Tennessee site for the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) and the Diabetes Prevention Program (DPP)/DPP Outcomes Study (DPPOS). Dr. Dagogo-Jack earned his medical and research doctorate degrees from the University of Ibadan College of Medicine in Nigeria, holds a master’s of science from the University of Newcastle upon Tyne in England, and completed his postdoctoral fellowship training in metabolism at the Washington University School of Medicine in St. Louis in Missouri. A board-certified endocrinologist, Dr. Dagogo-Jack has been elected to the Association of American Physicians and is the 2015 recipient of the Banting Medal for Leadership from the ADA. The ADA and Diabetes Care thank Dr. Dagogo-Jack for his outstanding leadership and service to the Association.
Introduction
To begin with, I would like to congratulate all of us on our 75th birthday as an Association. During the Second World War, with the world facing an existential threat, a small band of intrepid physicians thought it fit to declare another kind of war, with these words:
The patient suffering from the syndrome of diabetes mellitus is the reason for the existence of this Association. His medical, social, and economic problems are our problems. Since the incidence of diabetes and the mortality from this disease are increasing in spite of modern developments in medicine and surgery, a concerted attack on diabetes is essential.
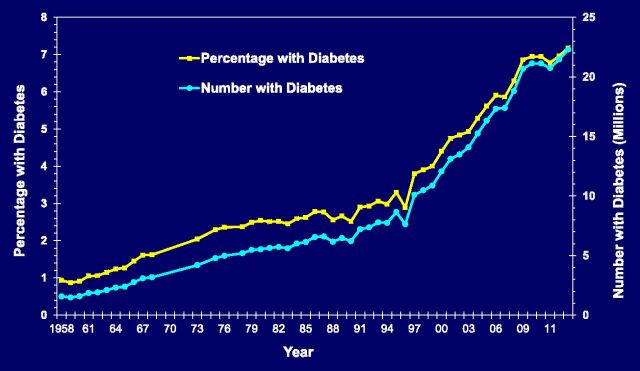
Approximately 750,000 Americans had been diagnosed with diabetes when Dr. Cecil Striker, the first American Diabetes Association (ADA) president, declared war on diabetes in 1941 (1). Today, with over 29 million Americans with diabetes and nearly 400 million similar individuals worldwide, the enormity of the diabetes problem has escalated exponentially (Fig. 1). Therefore, the war declared on diabetes by the first ADA president in 1941 must be prosecuted with renewed vigor. Our battle cry is “to prevent and cure diabetes and to improve the lives of all people affected by diabetes.” Our rallying vision is “Life free of diabetes and its burdens.” Our mission statement communicates three key goals: prevent, cure, improve. I would like to share my thoughts with you today on each of these critical pillars.
Figure 1.
Number and percentage of U.S. population with diagnosed diabetes, 1958–2013. Source: Centers for Disease Control and Prevention. Available from www.cdc.gov/diabetes/data/center/slides.html. Accessed 20 May 2015.
Improving the Lives of People With Diabetes
Each year nearly 2 million people are newly diagnosed with diabetes in America, and millions more around the world receive that diagnosis. Receiving a diagnosis of diabetes can trigger a range of emotions. Let me introduce you to Valerie, “America’s Supermom”! Valerie and her husband have six children, and then she decided to adopt and raise additional children, particularly children with troubled histories. In recognition of her work in opening her already crowded home to kids from all backgrounds, Valerie has been called America’s Supermom. Then Valerie was diagnosed with diabetes and this is how she expressed her feelings to her physician:
After taking care of myself, watching my diet and working out, how could I get the diagnosis of diabetes? Had I eaten the wrong things? No. Do I work out or exercise enough? Yes, I did. I just didn’t understand why or where I went wrong. So I just blamed myself. When I looked in the mirror I felt like a failure with this sudden life change, which seemed very drastic and it just felt like a death sentence to me. There needs to be more help for new patients and understanding this new, foreign lifestyle.
Supermom Valerie, the ADA hears you! You give voice to the nearly 2 million Americans and millions more around the world diagnosed with diabetes every year. At no time is the feeling of vulnerability, consternation, and helplessness greater than soon after receiving the diagnosis of diabetes. At no time is the need for support and information greater! The ADA “Living With Type 2 Diabetes” program provides critical information for newly diagnosed patients and valuable resources for self-management (2). We are also working on a parallel program for type 1 diabetes. In the past 4 years, “Living With Type 2 Diabetes” materials have been distributed to nearly 20,000 health care providers and have reached nearly 1.8 million patients, but that is far short of the 2 million new patients we need to reach each year. This valuable program is funded by the industry. With additional funding, we can extend coverage to every newly diagnosed American with diabetes.
To improve the lives of people with diabetes, the ADA sets standards of care for diabetes, delivers educational content to professionals and the lay public, and advocates for people with diabetes. Our Standards of Medical Care in Diabetes provides a blueprint for standardized management of diabetes. Our books and journals lead the field in the science and clinical practice of diabetes. With regard to textbooks, our Therapy for Diabetes Mellitus and Related Disorders (“Green Book”) has maintained its greenness but is now massively obese in its sixth edition, reflecting the explosion of knowledge that has taken place since the last edition. Our lay publications, including Diabetes Forecast and cookbooks, informational brochures, online resources, and our Call Center and social media presence all connect us to a vast global diabetes interest community.
Our advocacy efforts take us to many places from schools to the halls of Congress to sensitize elected officials to the enormity of the diabetes problem and to solicit increased public funding for diabetes research. We fight workplace discrimination, advocate for safety at schools for children with diabetes, and train police officers regarding the many facets of diabetes that can be misinterpreted during encounters with law enforcement. Sometimes, the opportunity to advocate for patients with diabetes may take nontraditional forms. In 2012, I received an e-mail from a woman called Shery, who lives in Tennessee, about her daughter. Shery wanted me to know that her daughter had been diagnosed with type 1 diabetes, which had “drastically changed” their lives. The daughter desires to become a doctor, but juggling diabetes with schoolwork was becoming quite a challenge. Sensing a family in need of encouragement, I wrote back to Shery the same day and reassured her that her daughter could indeed become a doctor if she so desired. I placed my services at the family’s disposal to help to guide and mentor them through the medical school preparation and application process. The daughter recently wrote to me that she is doing well in medical school and continues to volunteer for ADA’s Tour de Cure and Diabetes Camp for Children. She has enjoyed helping kids with diabetes in camp, an experience that has reinforced her commitment to pursuing a career in endocrinology!
Health surveys and reports consistently show marked ethnic disparities in the rates of diagnosed diabetes, as well as in diabetes complications. In the words of Dr. Martin Luther King Jr.: “Of all the forms of inequality, injustice in health care is the most shocking and inhumane.” Extensive genome-wide association studies have not provided a compelling explanation for the ethnic differences in type 2 diabetes prevalence (3). For example, the allelic frequencies of diabetes-related gene variants such as TCF7L2 are quite similar across major ethnic/racial groups (4). In the multiethnic Diabetes Prevention Program (DPP), individuals from different ethnic backgrounds progressed from impaired glucose tolerance to type 2 diabetes at similar rates (5). To determine whether ethnic disparities occur more proximally, in the Pathobiology of Prediabetes in a Biracial Cohort (POP-ABC) study, we evaluated the transition from normoglycemia to prediabetes in African American and Caucasian adults, all of whom have parents with type 2 diabetes. As was observed in the DPP, our results showed similar incidence of prediabetes in this biracial cohort (6). Thus, the factors that account for the marked ethnic disparities in the prevalence of diabetes remain to be fully elucidated.
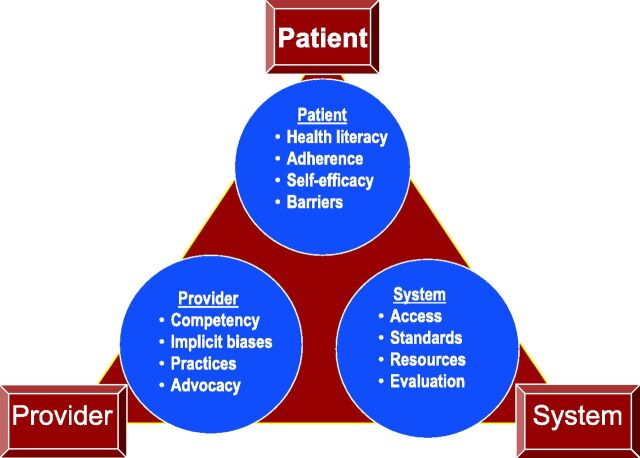
In contrast, marked ethnic disparities in the quality of diabetes control and the prevalence of diabetes complications have been noted, and have persisted, for more than 30 years (7,8). Yet, there is abundant evidence that optimized glycemic control prevents complications, regardless of race/ethnicity (9,10). For example, the national disparity in the rates of amputation (and other complications) by race/ethnicity is considerably attenuated among patients with diabetes enrolled in a health care system of uniform access and equal treatment (9). Health disparities are predicated upon a triangular interaction (Fig. 2) among the patient, the provider, and the health care system. Each one contributes significantly to the health and well-being of the patient. The ADA recognizes the need to reduce and eliminate disparities in diabetes. We have had in place for many years a high-risk health disparities initiative that reaches out to African Americans, Latinos, Native Americans, Asian Americans, Native Hawaiians, and Pacific Islanders. I am delighted to note that in 2014 our high-risk health disparity programs reached 4.5 million individuals in these communities!
Figure 2.
The health disparities triangle.
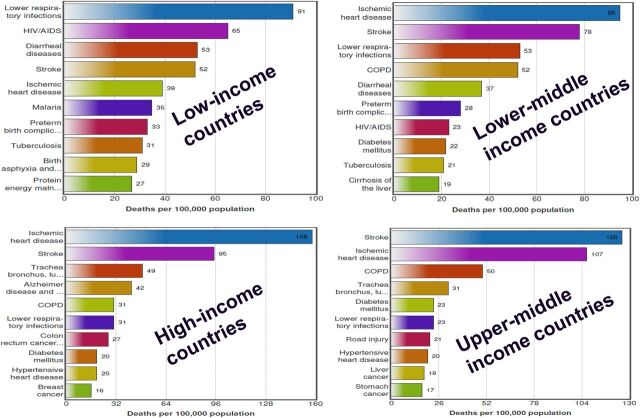
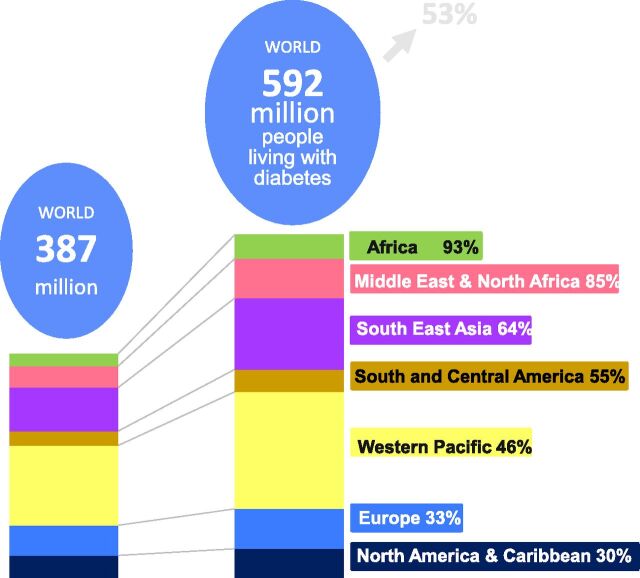
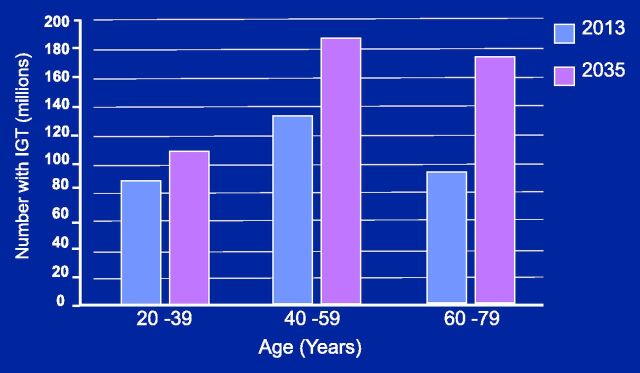
Preventing Diabetes
Preventing diabetes has become a global challenge. It has been projected that the number of people around the world diagnosed with diabetes will increase from 387 million (in 2014) to 592 million by the year 2035. Diabetes continues to be among the top 10 causes of death in most countries. Interestingly, that pattern is strongly linked to economic development: mortality from diabetes increases as countries transition from low-income through lower-middle and middle-income status (Fig. 3). This nefarious link between economic progress and death from diabetes is not inevitable. Leaders of countries in economic transition would be well advised to pay heed and institute timely preventive measures. Low- and middle-income countries are projected to experience the steepest increase in diabetes prevalence (Fig. 4). Yet, many of these countries lack the resources to deal effectively with the challenges of diabetes. Even among economically advantaged countries, it is concerning that nearly one-half of the patients with diabetes are not at an optimal level of control. This lack of adequate control drives the development of expensive complications. As we confront the global challenges of diabetes, we must also embrace the opportunity for primary prevention. Today, more than 300 million people around the world have prediabetes, and the number is projected to nearly double by the year 2035 (Fig. 5). The unequivocal demonstration that type 2 diabetes can be prevented presents a tremendous opportunity for stemming the global tide of diabetes (5,11).
Figure 3.
Top 10 causes of death in countries of the world grouped by income status. COPD, chronic obstructive pulmonary disease. Source: World Health Organization. Available from http://www.who.int/mediacentre/factsheets/fs310/en/index1.html. Accessed 20 May 2015.
Figure 4.
Projected increases in diabetes prevalence in different regions of the world. Source: International Diabetes Federation. IDF Diabetes Atlas. 6th ed. Brussels, Belgium, International Diabetes Federation, 2013, p. 12.
Figure 5.
Global burden of prediabetes, or the number of people with impaired glucose tolerance (IGT). Source: International Diabetes Federation. IDF Diabetes Atlas. 6th ed. Brussels, Belgium, International Diabetes Federation, 2013, p. 40.
Although local in its initial focus, it must be recognized that our Association has always had a global outlook from its earliest beginnings. For example, at the 1946 ADA Scientific Sessions held in Toronto, Canada, five Banting medals were awarded to recipients from five different countries (Dr. Bernardo Houssay of Argentina; Dr. Hans Hagedorn of Denmark; Dr. R.D. Lawrence of England; Dr. Eugene Opie, American pathologist; and Sidney Smith, president of the University of Toronto, Canada). In his 1946 Presidential Address, ADA President Dr. Joseph Barach noted that attendees had come “from many countries, bound together with a sole aim and common cause, to see that diabetes the world over is treated at the highest level of efficiency….” I am proud to observe that the ADA has maintained that early tradition of recognizing talent without national or geographical restrictions. At the 2015 Scientific Sessions held in Boston, attendees came from every inhabited continent of the globe, and our programming covered topics of global significance. Recognizing that health professionals in many countries are unable to attend our valuable scientific sessions, the ADA has developed a supplemental program. The “Best of ADA” program distills the material of the highest caliber from our Scientific Sessions for delivery to professionals around the world. The ADA will continue to embrace what has now become a global imperative. We will continue to partner with kindred organizations nationally and internationally that advocate for the rights, privileges, and well-being of individuals with diabetes wherever they may call home.
Finally, Curing Diabetes
We share the disappointment and impatience of those who take us to task for not yet having found the cure for diabetes. Understandably, parents of children with type 1 diabetes are particularly vocal in expressing that frustration. The war against diabetes has been a series of escalating battles. Viewed in that light, we can take comfort in the undisputed victories that have been recorded in many critical battles of the war. Before the 1920s and well into the century, there was tremendous ignorance surrounding diabetes. The battle against ignorance and misconceptions about diabetes is largely settled. A very critical battle—stop people from dying from diabetic ketoacidosis—was delivered by the discovery of insulin. Since then we have gone on to score victory after victory, discovering a plethora of oral agents and designer insulins and delivery systems, creating the modern diabetes team, and transferring self-management skills to patients with diabetes. Along the way, we have also deciphered a good deal regarding the pathophysiology of diabetes, mechanisms of glucose counterregulation and iatrogenic hypoglycemia, the role of autoimmunity in type 1 diabetes, and the complex genetic landscape of type 2 diabetes. We are also making significant progress in reducing diabetes complications. Indeed, Gregg and colleagues (12) reported that many of the complications of diabetes have declined significantly across U.S. demographic groups over the past 2 decades.
But we have several battles that are still in progress (Table 1). We need to unravel the biological and social determinants of human adherence, eliminate disparities, decrease excess cardiovascular burden, translate type 2 diabetes prevention globally, and accelerate knowledge to enable the prediction and prevention of type 1 diabetes. We must decode and interrupt the role of intrauterine factors in programming adult disorders. We need to develop technologies for the optimization of glycemic control and come up with common platforms to enable interoperability of blood glucose meters and test strips in order to minimize waste and frustration. There is an epic battle that is now raging in the field of diabetes—that of unlocking the mysteries of the β-cell. Insulin secretion by the β-cells in amounts commensurate with the body’s demand guarantees freedom from diabetes. It is known that the β-cells expand to increase their insulin output to meet demands in obese individuals as well as in pregnant women. What has gone awry with the natural processes for β-cell expansion in our patients with diabetes?
Table 1.
Areas of critical need for progress in diabetes research and practice
| • Unravel the biological and social determinants of human adherence |
| • Understand behavior and motivation for wellness |
| • Eliminate disparities in access, quality, and outcomes of diabetes care |
| • Reduce excess cardiovascular morbidity and mortality in diabetes |
| • Translate type 2 diabetes globally and discover novel approaches to prediction and prevention of type 1 diabetes |
| • Decode and interrupt the role of intrauterine factors in programming of adult cardiometabolic disorders |
| • Develop diabetes technologies for optimization of glycemic control and guidelines for their proper use |
| • Develop common platforms to enable interoperability of blood glucose meters and test strips |
| • Unlock the mystery of β-cell demise/dysfunction in diabetes and develop rescue/replacement strategies |
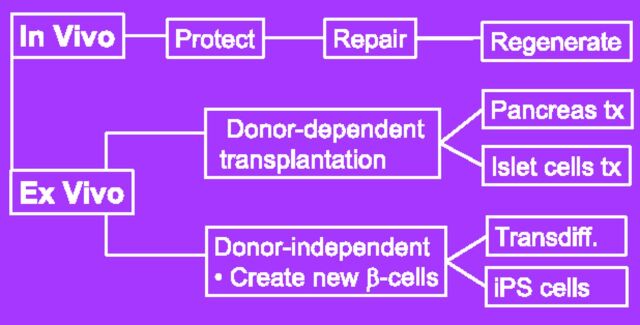
The epic battle of the β-cell is being fought on two fronts—in vivo and ex vivo. The in vivo tasks are to protect the β-cells from damage or to repair or regenerate damaged cells. The ex vivo approach has been based on transplantation of donor cells, an approach fraught with problems of supply and immunological rejection. The donor-independent approach involves the creation and proliferation of new β-cells, either through transdifferentiation of endoderm-derived cells (such as pancreatic exocrine cells and hepatocytes) or through induced pluripotent stem (iPS) cells (Fig. 6). In 1962, Dr. John Gurdon replaced the nucleus of a frog egg with the nucleus from an adult frog. The result was a tadpole generated from the frog egg bearing donor DNA from the adult frog. That was the first example of a cloned animal. Several decades later, in 2006, Dr. Shinya Yamanaka inserted four transcription factors into adult mouse skin cells, which then became reprogrammed to a more primitive form, akin to embryonic stem cells. The use of such iPS cells derived from adult cells obviates the moral and ethical arguments that plague the use of embryonic stem cells. Already, these technologies are being applied in numerous laboratories, including those of Dr. Douglas Melton and others, to address the β-cell problem in diabetes. Skin cells from patients with type 1 diabetes have been successfully reprogrammed to become iPS cells, which have then been differentiated to become pancreatic islet cells that produce insulin and glucagon (13). Recently, Dr. Raikwar and colleagues (14) transplanted human-derived iPS cells into diabetic mice and showed that the iPS cells secreted sufficient insulin to regulate blood glucose. We are still a long way from using these cells for human therapy, but, as the saying goes, a journey of a thousand miles begins with the first step, and we have taken those initial steps.
Figure 6.
Schema of in vivo and in vitro approaches to β-cell preservation or replacement. Transdiff., transdifferentiation; tx, transplantation.
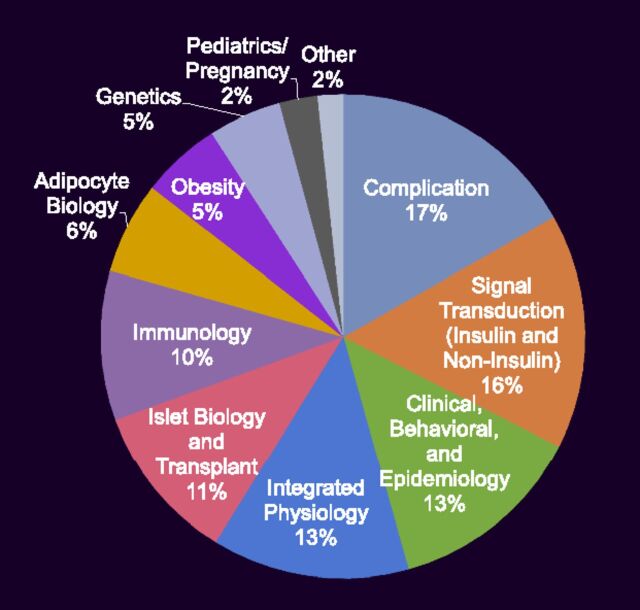
Research is the only credible path to winning the ongoing battles and finding a cure for diabetes. The ADA’s research program was initiated in 1952, and since then we have disbursed more than $700 million. Our funded research projects cover a broad range of topics in the basic, clinical, translational, and behavioral sciences (Fig. 7). We have followed the traditional approach in selecting applications to fund, but have recalled the words of the Nobel laureate, Max Born:
… there is no philosophical high road in science, with epistemological signposts. No, we are in a jungle and find our way by trial and error, building our road behind us as we proceed. (15)
Figure 7.
Approximate distribution of focus areas of research projects funded by grants from the ADA.
That is why, in 2013, the ADA launched a new funding mechanism to accelerate discovery: The Pathway to Stop Diabetes program guarantees significant support and invests in the success of the investigator rather than of a specific project. Pathway is funded by donations from individual and corporate donors. Research needs money, and we all can be fund-raisers for the ADA. Experience has shown that scientists can be effective fund-raisers. After all, we are the bridge between science and society. If we communicate clearly and passionately, we will strike a common chord with the inner philanthropist that resides in most people.
In conclusion, today, as in 1940, patients with diabetes remain the sole reason for the existence of this Association. Their medical, social, economic, and psychological problems are our problems. At no time in history have forces been better aligned for victory over diabetes as now. The global brainpower deployed in diabetes research, the amazing opportunity for global collaboration, and the speed with which research results can be shared (almost instantaneously), all bode well for victory. Indeed, we are nearing the crest of the Shakespearean wave of opportunity and discovery:
There is a tide in the affairs of men,
Which, taken at the flood, leads on to fortune;
Omitted, all the voyage of their life
Is bound in shallows and in miseries.
On such a full sea are we now afloat;
And we must take the current when it serves,
Or lose our ventures. (16)
With the enormous assets of our era, sooner than later, diabetes will succumb to the overwhelming force of science! This I believe with all my heart.
Article Information
Acknowledgments. The author acknowledges the early mentorship and support of his parents (Karibi and Biribota Dagogo-Jack), the abiding support of his wife (Dr. Agbani Dagogo-Jack) and children (Karibi, Ibiayi, Alali, and Sokiente), and the research and clinical mentorship of Professor Pat Kendall Taylor of the University of Newcastle and Drs. Philip E. Cryer and William H. Daughaday of Washington University School of Medicine in St. Louis. The author also gratefully acknowledges the support of Dr. Abbas E. Kitabchi, Dr. Solomon S. Solomon, and other colleagues at The University of Tennessee. The author thanks his current and former research volunteers, research fellows and associates, administrative staff, and the staff of the ADA Scientific and Medical Division, particularly Matt Petersen.
Duality of Interest. S.D.-J. has served as a consultant for Merck, Novo Nordisk, AstraZeneca, Boehringer Ingelheim, and Janssen and has served as an investigator on clinical trial contracts to The University of Tennessee from AstraZeneca, Novo Nordisk, and Boehringer Ingelheim. No other potential conflicts of interest relevant to this article were reported.
References
- 1.American Diabetes Association . The Journey & the Dream. A History of the American Diabetes Association. Alexandria, VA, American Diabetes Association, 1988, p. 10 [Google Scholar]
- 2.American Diabetes Association . Living With Diabetes, [Internet]. Available from http://www.diabetes.org/living-with-diabetes/. Accessed 15 May 2015
- 3.Dagogo-Jack S. Predicting diabetes: our relentless quest for genomic nuggets. Diabetes Care 2012;35:193–195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hivert MF, Jablonski KA, Perreault L, et al.; DIAGRAM Consortium; Diabetes Prevention Program Research Group . Updated genetic score based on 34 confirmed type 2 diabetes loci is associated with diabetes incidence and regression to normoglycemia in the Diabetes Prevention Program. Diabetes 2011;60:1340–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knowler WC, Barrett-Connor E, Fowler SE, et al.; Diabetes Prevention Program Research Group . Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dagogo-Jack S, Edeoga C, Ebenibo S, Nyenwe E, Wan J; Pathobiology of Prediabetes in a Biracial Cohort (POP-ABC) Research Group . Lack of racial disparity in incident prediabetes and glycemic progression among black and white offspring of parents with type 2 diabetes: the Pathobiology of Prediabetes in a Biracial Cohort (POP-ABC) study. J Clin Endocrinol Metab 2014;99:E1078–E1087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in Medicare managed care. JAMA 2002;287:1288–1294 [DOI] [PubMed] [Google Scholar]
- 8.Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988-1994 and 1999-2010. Ann Intern Med 2014;160:517–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV. Ethnic disparities in diabetic complications in an insured population. JAMA 2002;287:2519–2527 [DOI] [PubMed] [Google Scholar]
- 10.Bower JK, Brancati FL, Selvin E. No ethnic differences in the association of glycated hemoglobin with retinopathy: the National Health and Nutrition Examination Survey 2005-2008. Diabetes Care 2013;36:569–573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Echouffo-Tcheugui JB, Dagogo-Jack S. Preventing diabetes mellitus in developing countries. Nat Rev Endocrinol 2012;8:557–562 [DOI] [PubMed] [Google Scholar]
- 12.Gregg EW, Li Y, Wang J, et al. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med 2014;370:1514–1523 [DOI] [PubMed] [Google Scholar]
- 13.Maehr R, Chen S, Snitow M, et al. Generation of pluripotent stem cells from patients with type 1 diabetes. Proc Natl Acad Sci U S A 2009;106:15768–15773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raikwar SP, Kim E-M, Sivitz WI, Allamargot C, Thedens DR, Zavazava N. Human iPS cell-derived insulin producing cells form vascularized organoids under the kidney capsules of diabetic mice. PLoS One 2015;10:e0116582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Born M. Experiment and Theory in Physics. Cambridge University Press, 1943, p. 44 [Google Scholar]
- 16.Shakespeare W. Julius Caesar. In: The Complete Works of William Shakespeare, Wordsworth Editions, 1996, p. 604