Abstract
Background
Total knee arthroplasty is known to successfully alleviate pain and improve function in endstage knee osteoarthritis. However, there is some controversy with regard to the influence of obesity on clinical benefits after TKA. The aim of this study was to investigate the impact of body mass index (BMI) on improvement in pain, function and general health status following total knee arthroplasty (TKA).
Methods
A single-centre retrospective analysis of primary TKAs performed between 2006 and 2016 was performed. Data were collected preoperatively and 12-month postoperatively using WOMAC score and EQ-5D. Longitudinal score change was compared across the BMI categories identified by the World Health Organization.
Results
Data from 1565 patients [mean age 69.1, 62.2% women] were accessed. Weight distribution was: 21.2% BMI < 25.0 kg/m2, 36.9% BMI 25.0–29.9 kg/m2, 27.0% BMI 30.0–34.9 kg/m2, 10.2% BMI 35.0–39.9 kg/m2, and 4.6% BMI ≥ 40.0 kg/m2. All outcome measures improved between preoperative and 12-month follow-up (p < 0.001). In pairwise comparisons against normal weight patients, patients with class I-II obesity showed larger improvement on the WOMAC function and total score. For WOMAC pain improvements were larger for all three obesity classes.
Conclusions
Post-operative improvement in joint-specific outcomes was larger in obese patients compared to normal weight patients. These findings suggest that obese patients may have the greatest benefits from TKA with regard to function and pain relief one year post-op. Well balanced treatment decisions should fully account for both: Higher benefits in terms of pain relief and function as well as increased potential risks and complications.
Trial registration
This trial has been registered with the ethics committee of Eastern Switzerland (EKOS; Project-ID: EKOS 2020–00,879)
Keywords: Total knee arthroplasty, Obesity, Patient-reported outcome, EQ-5D, WOMAC Score
Background
Osteoarthritis (OA) is a major global cause of disability, with the knee being the most frequently affected joint [1]. Total knee arthroplasty (TKA) is successful in alleviating the pain and disability associated with knee OA, and is one of the most commonly performed elective surgical procedures in orthopaedics [2]. The improvements in patient health status achieved by TKA have been reported comparable to coronary revascularisation and renal transplant procedures [3]. Due to its well documented success, the number of TKAs performed increases every year and operative rates are reported to have doubled in the last decade [4, 5].
There is an established association between the patients’ body mass index (BMI) and knee OA, possibly due to increased mechanical loading at the joint [6–8]. Increased BMI is suggested to be one of the main modifiable risk factors of knee OA, given that every kilogram of weight loss leads to a fourfold reduction in the load exerted on the knee with daily activities [7]. Preoperative weight loss was found to have considerable implications for patient burden and cost reduction. [9]. High BMI is also associated with a variety of metabolic disturbances such as coronary heart disease, hypertension and diabetes [7, 10] that could result in systemic risk factors for OA. Consequently, patients with increased BMI are more likely to require total knee arthroplasty (TKA) at younger age than patients with normal BMI [11]. Worldwide levels of obesity (BMI > 30 kg/m2 by WHO definition) are rising rapidly [12, 13]. A quarter of the population of developed countries are reported as being obese [14]. By 2030, the respective number of overweight (BMI > 25 kg/m2) and obese (BMI > 30 kg/m2) adults is projected to be 1.35 billion and 573 million individuals [12, 15]. Although increased BMI has been linked to the need for TKA, the impact of BMI on outcomes after TKA is less well established [2, 6, 8, 16–20]. Patients with an increased BMI have been reported higher in-hospital discharge rates [21] and are accepted to have higher risks of postoperative wound dehiscence [22], infection [16, 22, 23], complications, and revision [6, 20, 24, 25]. These risks are often compounded by the associated comorbidities [20] or other factors like socioeconomic status [26] frequently found in such patients. It is not clear though whether BMI is associated with worse patient reported outcomes following TKA, as both equivalent outcomes [27, 28] and lower absolute post-operative scores [17, 19, 29] have been proposed scaled by BMI class using various metrics.
The objective of this study was to investigate the impact of preoperative BMI on postoperative improvement in pain, function and general health status following total knee arthroplasty (TKA) from the patients’ perspective.
Methods
The study was performed at a large teaching hospital in Switzerland; a higher-income country with a largely white European population. Ethics approval was obtained from the local ethics committee (ethics committee of Eastern Switzerland EKOS; Project-ID: EKOS 2020–00,879). Data from the local knee arthroplasty register was accessed and all patients undergoing elective primary total knee arthroplasty between 2006 and 2016 were considered for inclusion. Simultaneous bilateral surgery or incomplete data sets were criteria for patient exclusion. No patients were precluded from surgery or restricted from study inclusion due to their BMI. On an individual basis, depending on symptom burden and mobility, morbidly obese patients were referred to weight loss programs prior to surgery. Surgery was performed by consultant orthopaedic surgeons and their supervised trainees. Surgery was performed in spinal or general anesthesia. Antibiotic prophylaxis using 3rd generation cephalosporin was administered in every case. A tourniquet was applied and inflated for insertion of the cemented implant. A medial parapatellar approach was routinely used, with a lateral parapatellar approach and osteotomy of the tibial tubercle in cases with severe valgus deformity. Cemented primary implants (LCS complete or Attune, DePuy-Synthes) were implanted in all cases. A tibia first, ligament balancing technique was employed, with and without computer-navigation (Brainlab, Munich). The cruciate ligaments were routinely sacrificed. No special considerations were made for patients based on their BMI during the routine postoperative standard rehab protocol, which was followed in every case. This allowed unrestricted weight bearing as tolerated on crutches and physiotherapy to improve range of motion and muscle activation without further limitations from day one. VTE prophylaxis was performed for 6 weeks following surgery. Outpatient follow-up visits were routinely performed 2 and 12 months postoperatively, and in 5-year intervals thereafter. Preoperative and 12-month postoperative data were retrieved. Patient reported outcome data were prospectively collected at the time of treatment. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC score) was employed for measuring pain, stiffness and function in the respective subscales, the EQ-5D for measuring general health status. The WOMAC score is a widely used three-dimension self-administered patient-reported outcome instrument consisting of 24 questions that are linearly transformed to a 0–100 scale with higher scores indicating more severe impairment. The score has been extensively tested for validity, reliability, feasibility and responsiveness [30, 31]. The EQ-5D [32] is a generic self-report questionnaire. It consists of five questions measuring the patient’s health status and covers self-care, mobility, depression/anxiety, pain and usual activities. A health utility can be calculated from the five questions, with a score of 1 reflecting full health, 0 indicating a health state equaling death and negative values describing health states that patients consider worse than being dead. This widely used questionnaire has shown satisfying measurement characteristics in knee patients [33].
Statistical analysis
Sample characteristics are given as means, standard deviations or 95% confidence intervals, and ranges. Score change following surgery was compared across the BMI categories identified by the World Health Organization (WHO) [13]: normal weight (BMI < 25.00), overweight (BMI 25.00 to 29.99), class I obesity (BMI 30.00 to 34.99), class II obesity (BMI 35.00 to 39.99), and class III obesity (BMI ≥ 40.00).
To investigate the impact of BMI on postoperative improvement we used linear mixed models with the outcome parameters (WOMAC subscales, EQ-5D) as dependent variables, and the following independent variables: BMI group, time point (preoperative and 12-month follow-up), and the two-way interaction of group-by-time. In such a model, the interaction term indicates a difference in postoperative improvement between BMI groups. We ran pairwise post-hoc tests comparing postoperative improvement between the “normal weight” category and the four other BMI categories. The models also included a first-order autoregressive covariance matrix to account for correlations between repeated measurements. Results are presented as estimated marginal means with their 95% confidence intervals and p-values for the group effect, time effect, and the group-by-time interaction. P-values below 0.05 were considered to be statistically significant. All analyses were conducted in SPSS 24.0.
Results
Sample characteristics
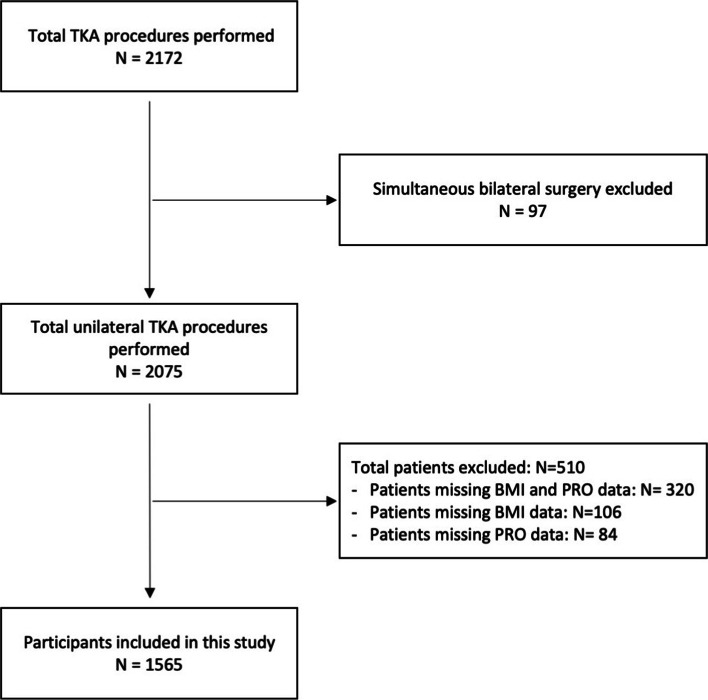
Between February 2006 and December 2016, a total of 2172 patients underwent primary TKA at our institution and were included in the local knee arthroplasty registry. 1565 patients were available for analysis (Fig. 1). There were no statistically significant differences between patients having or missing BMI or PROMs data, indicating that these missing values were random (data not shown).
Fig. 1.
Flowchart on study inclusion
In this sample, mean patient age was 69.1 years (range 24.8—92.3 years). 62.2% of patients were female, and the right side was affected in 817 cases (52.2%). Response rates for the WOMAC score and the EQ-5D at 12-month were 83.8% and 84.5%, respectively. We found 21.2% of patients (N = 332) to be normal weight (BMI < 25.0 kg/m2), 36.9% (N = 578) were overweight (BMI 25.0–29.9 kg/m2), 27.0% (N = 423) had class I obesity (BMI 30.0–34.9 kg/m2), 10.2% (N = 160) had class II obesity (BMI 35.0–39.9 kg/m2), and 4.6% (N = 72) had class III obesity (BMI ≥ 40.0 kg/m2) (Table 1).
Table 1.
Sociodemographic and clinical patient characteristics at pre-surgery (N = 1565)
| Mean (SD) | |||
|---|---|---|---|
| Age | 69.1 (10.1) | ||
| N | (%) | ||
| Sex | |||
| Women | 974 | (62.2%) | |
| Men | 591 | (37.8%) | |
| Education | |||
| Compulsory school | 479 | (31.2%) | |
| More than compulsory school (A-levels, apprenticeship, university) | 1058 | (68.8%) | |
| Missing | 28 | ||
| Employment status | |||
| Full-time or part-time | 293 | 18.9% | |
| Retired | 730 | 47.1% | |
| Homemaker | 448 | 28.9% | |
| Other | 51 | 5.1% | |
| Missing | 16 | ||
| Smoking | |||
| No | 1277 | (82.6%) | |
| Yes | 269 | (17.4%) | |
| Missing | 19 | ||
| Side of implant | |||
| Left | 748 | (47.8%) | |
| Right | 817 | (52.2%) | |
| BMI (%) | |||
| ≤ 24.99 | normal weight | 332 | (21.2%) |
| 25.00–29.99 | pre-obesity | 578 | (36.9%) |
| 30.00–34.99 | class I obesity | 423 | (27.0%) |
| 35.00–39.99 | class II obesity | 160 | (10.2%) |
| ≥ 40.00 | class III obesity | 72 | (4.6%) |
| Computer navigation | |||
| Yes | 931 | 61.0% | |
| Noa | 595 | 39.0% | |
| Missing | 39 | ||
aincluding N = 33 aborted navigations
BMI was associated with sex (p < 0.001), with a similar proportion of normal weight patients for both sexes (men 20.5% vs women 21.7%), a higher proportion of pre-obese men (men 43.3% vs women 33.1%), and more women in class I-III obesity (class I: 27.9% women vs 25.5% men, class II 12.2% women vs 6.9% men, class III: 5.1% women vs 3.7% men).
There was a statistically significant association of BMI class and age at the time of surgery (p < 0.001). Mean age was 70.5 years in normal weight patients and decreased monotonously to 65.3 years in class III obesity patients.
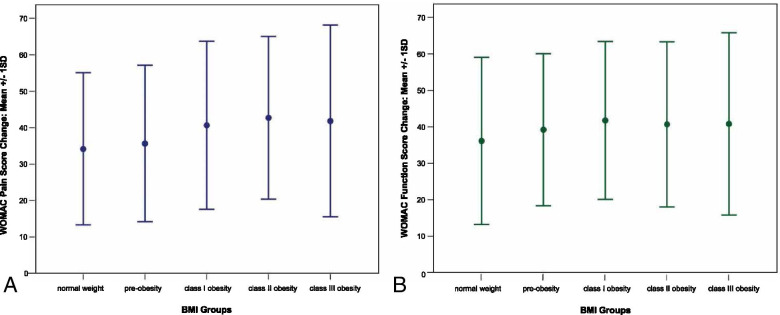
WOMAC pain
WOMAC pain scores differed significantly between BMI groups (p < 0.001) with better scores observed in lower BMI categories. Pain scores improved between preoperative assessments and 12-month follow-up (p < 0.001). Postoperative improvement was associated with BMI group (p < 0.001). In pairwise comparisons of BMI groups, we found improvements in class I, II and III obesity patients (-40.4, -44.2, and -42.3 points) to be statistically significantly (all p < 0.05) larger than in normal weight patients (-34.5 points). For further details please see Table 2 and Fig. 2a. All differences remained statistically significant when adjusting for sex and age.
Table 2.
WOMAC pain, function and total score for different BMI groups (pre-surgery: all scales N = 1565; 12-month: pain N = 1311, function N = 1308, total N = 1308)
| Pre-surgery | 12 months | Improvement | |
|---|---|---|---|
| BMI | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) |
| WOMAC pain | |||
| normal: < 25 | 45.2 (38.7–51.7) | 10.7 (2.9–18.5) | 34.5 (31.9–37.1) |
| pre-obesity: 25–30 | 45.9 (39.3–52.6) | 9.8 (3.7–16.0) | 36.1 (34.1–38.1) |
| class I obesity: 30–35 | 50.5 (43.7–57.2) | 10.1 (3.6–16.6) | 40.4 (38.0–42.7)* |
| class II obesity: 35–40 | 54.3 (41.8–66.8) | 10.2 (0.0–22.9) | 44.2 (40.3–48.0)* |
| class III obesity: ≥ 40 | 54.9 (39.1–70.7) | 12.6 (0.0–29.2) | 42.3 (36.7–48.0)* |
| Group | Time | Group-by-time interaction | |
| F = 6.1; p < 0.001 | F = 2458.4; p < 0.001 | F = 6.7; p < 0.001 | |
| WOMAC function | |||
| normal: < 25 | 52.6 (50.6–54.6) | 16.2 (14.0–18.4) | 36.4 (33.8–39.1) |
| pre-obesity: 25–30 | 54.5 (53.0–56.0) | 15.5 (13.9–17.1) | 39.0 (37.0–41.0) |
| class I obesity: 30–35 | 57.7 (56.0–59.5) | 16.2 (14.3–18.1) | 41.6 (39.2–43.9)* |
| class II obesity: 35–40 | 61.1 (58.2–63.9) | 18.7 (15.6–21.9) | 42.3 (38.5–46.2)* |
| class III obesity: ≥ 40 | 62.8 (58.6–67.1) | 22.4 (17.8–27.0) | 40.4 (34.8–46.1) |
| Group | Time | Group-by-time interaction | |
| F = 8.0; p < 0.001 | F = 2497.6; p < 0.001 | F = 2.7; p = 0.030 | |
| WOMAC total | |||
| normal: < 25 | 50.9 (49.0–52.8) | 15.1 (13.1–17.2) | 35.8 (33.3–38.3) |
| pre-obesity: 25–30 | 52.6 (51.1–54.0) | 14.5 (13.0–16.0) | 38.1 (36.2–39.9) |
| class I obesity: 30–35 | 56.0 (54.3–57.6) | 14.9 (13.1–16.7) | 41.0 (38.8–43.2)a |
| class II obesity: 35–40 | 59.1 (56.4–61.8) | 16.7 (13.7–19.6) | 42.4 (38.8–46.1)a |
| class III obesity: ≥ 40 | 60.8 (56.8–64.8) | 20.2 (15.8–24.5) | 40.6 (35.3–46.0) |
| Group | Time | Group-by-time interaction | |
| F = 7.4; p < 0.001 | F = 2739.4; p < 0.001 | F = 3.6; p = 0.006 | |
a statistically significant (p < 0.05) difference in change compared to “normal” weight patients
Fig. 2.
WOMAC pain (a) and function (b) score change between pre-surgery and 12-month follow-up across BMI groups
WOMAC function
WOMAC function scores differed significantly between BMI groups (p < 0.001), with lower BMI groups showing better function. Function significantly improved from pre-surgery to the 12-month follow-up (p < 0.001). Postoperative improvement was also associated with BMI group (p = 0.030). The pairwise comparisons of BMI groups, showed improvements in class I-II obesity patients (-41.6 and -42.3 points) to be statistically significantly (both p < 0.05) larger than in normal weight patients (-36.4 points). Further details are given in Table 2 and Fig. 2b. In sex-and age-adjusted analysis all differences remained statistically significant.
WOMAC total
For the WOMAC total score we found statistically significant differences between BMI groups overall (p < 0.001) with patients with lower BMI reporting better scores, and a general improvement between the preoperative time point and 12-month follow-up (p < 0.001).
For the WOMAC total score, postoperative improvement was associated with BMI group (p = 0.006). The pairwise comparisons of BMI groups showed statistically significantly (all p < 0.05) larger improvements in class I-II obesity patients (-41.0 and -42.4 points) compared to normal weight patients (-35.8 points). Details are given in Table 2. In sex-and age-adjusted analysis all differences remained statistically significant.
EQ-5D
The EQ-5D utility scores differed between BMI groups (p < 0.001), and improved in general from preoperatively to 12-month follow-up (p < 0.001). No statistically significant difference between BMI groups was observed regarding postoperative improvement (p = 0.066). Adjustment for sex and age resulted in the same statistical differences (Table 3).
Table 3.
EQ-5D utility values for different BMI groups (pre-surgery N = 1521, 12-month N = 1286)
| EQ-5D utility | Pre-surgery | 12 months | Improvement |
|---|---|---|---|
| BMI | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) |
| normal: < 25 | 0.66 (0.49–0.83) | 0.90 (0.31–1.00) | 0.24 (0.21–0.27) |
| pre-obesity: 25–30 | 0.66 (0.55–0.77) | 0.90 (0.79–1.00) | 0.24 (0.22–0.26) |
| class I obesity: 30–35 | 0.61 (0.45–0.77) | 0.89 (0.71–1.00) | 0.28 (0.25–0.31) |
| class II obesity: 35–40 | 0.58 (0.11–1.00) | 0.86 (0.12–1.00) | 0.28 (0.23–0.33) |
| class III obesity: ≥ 40 | 0.54 (-0.09–1.00) | 0.85 (-0.09–1.00) | 0.30 (0.24–0.37) |
| Group | Time | Group-by-time interaction | |
| F = 9.1; p < 0.001 | F = 785.9; p < 0.001 | F = 2.2; p = 0.066 |
No statistically significant (p < 0.05) differences in change between BMI groups
Discussion
This study highlights that the perceived benefit in terms of joint-specific patient-reported outcome following total knee arthroplasty is larger in obese patients compared to normal weight patients when analyzing post-operative improvement at 12-month follow-up. This association was found irrespective of a possible impact of sex and age.
The literature on the impact of BMI on pain and functional outcomes following TKA is somewhat conflicted. Multiple studies have shown that outcomes after TKA are worse in obese patients than in non-obese patients [10, 18, 34]. Amin et al. [34] reported inferior cross-sectional clinical outcome scores (Knee Society Score) and higher complication rates in morbidly obese patients at a mean follow-up of 38.5 months. They reported a significantly higher rate of radiolucent lines around the implants (notably around the tibial component) and inferior five-year implant survivorship for patients with BMI > 40 kg/m2 compared to patients with BMI < 30 kg/m2 in their prospective matched pair study. Lash et al. [35] found that patients with BMI > 35 kg/m2 had worse preoperative and post-operative functional scores (WOMAC, Oxford Knee Score, High-activity Arthroplasty Score) than patients with BMI < 30 kg/m2, but their benefit from surgery measured by the change in functional scores showed no difference. Similarly, Baker et al. [19] reported no differences in OKS improvement among patients with class I, II and III obesity.
In line with our results, Chen et al. [17] suggest greater improvement in the more obese patient groups, with the mean improvement in Oxford Knee Score (OKS) and Knee Society Knee Score (KSKS) at two years follow-up being significantly higher in the morbidly obese group than in the normal group. Greater obesity level was associated with more pain at baseline but greater postoperative pain relief in a study conducted by Li et al. [27]. In this study, the postoperative gain in Physical Component Summary (SF-36) did not differ by BMI level.
Similarly, a recent systematic review by Boyce et al. [6] found that all patients regardless of BMI experienced comparable improvements in knee function following TKA.
The more obese patients in our cohort generally reported a superior improvement in outcome scores. The context of this improvement is that they started with notably poorer preoperative scores. As such although the delta (improvement) was larger, the absolute post-operative score was not superior in the obese patients. When evaluating the clinical benefits of TKA it is crucial to focus on change rather than interpret post-operative data with cross-sectional analysis, as the latter may to a large degree simply reflect pre-operative differences between patients. Change in symptomatology is what is most noticeable to the patient and is the yardstick by which they interpret the benefit of surgery and patients with higher pre-operative symptom burden may have simply more to gain by surgery.
It is important to note that this study did not take into account the increased complication rate in obese patients associated with the intervention. Higher perioperative and postoperative complication risks are well accepted to be greater in obese patients [20, 25, 34, 36]. Complication rates climb further as BMI levels rise into morbidly and super-obese categories [6, 10, 37]. Increased risks include wound related problems like delayed wound healing, superficial wound infection and deep prosthetic joint infection [6, 22, 25, 34, 36, 38]. In addition, obese patients show higher rates of revision, aseptic loosening and radiographic signs of early loosening [6, 34, 38, 39] and more frequent osteolysis or wear [39]. Alongside reduced longevity of the implant, obesity is also associated with reduced life expectancy [40–42]. Patients with BMIs over 35 can expect a significantly reduced life expectancy compared to normal weight individuals. Large scale international study data suggests around 3–4 years are lost to individuals with class I obesity and 10 or more years to those in class III [43–45]. If hesitation to perform surgery in obese patients is due to concerns as to reduced implant longevity, this worry may be partially mitigated by a generally reduced life expectancy. In terms of health economy, even in “high risk” patients, TKA remains a cost-effective intervention [46].
From a clinical perspective, joint replacement surgery is an intervention for end-stage disease. Our findings also support a developmental relationship between OA and obesity, as highly obese patients underwent TKA at a younger age than the normal weight or pre-obese patient population. These considerations are in accordance with the findings of Changulani et al. [47] who stated that for both hip and knee replacement, the age at surgery fell significantly for patients with a BMI > 35 kg/m2. It is also likely that the management of increased complications in this population predispose obese patients rather toward a delay of arthroplasty, and it is likely they present even younger to orthopedics than the age at time of surgery suggests.
Strengths of this study include a large sample size which allowed for stratification and comparison of BMI subgroups as suggested by the WHO, the availability of data from a joint-specific questionnaire as well as a general health outcome measure which allowed to demonstrate the differential impact of BMI on outcome after TKA. A limitation is that we had a 28% loss to follow-up rate, 12.6% of patients had to be excluded due to missing PROM questionnaires and 10.9% of patients due to missing BMI values (Fig. 1). However, as collection of BMI values and PROM questionnaires in our series is largely unrelated to BMI category it is unlikely that this may have introduced relevant bias in this study. Another limitation is that the patients’ BMI was only recorded preoperatively and possible weight changes that may have taken place by the 12-month postoperative review were not accounted for. This is potentially important in the light that patients who underwent TKA and lost weight thereafter were reported to have better clinical outcome scores than patients who gained weight in the postoperative period [48]. However, recent literature indicates the patient’s bodyweight to be maintained after TKA [49–51], suggesting a minor possible impact of weight change on our results. The percentage of patients in obesity class II and III was relatively low, compared to reports in other countries with two-thirds of our patient cohort clustered in the overweight / pre-obese and class I obese categories. This however accurately reflects our wider country-specific weight distribution.
Conclusions
This study demonstrates larger post-operative improvement in joint-specific outcomes in obese patients compared to normal weight patients. Our findings suggest that obese patients may have the greatest benefits from TKA regarding increase of functional capacity and pain relief at one year follow-up. Well balanced treatment decisions in shared decision making should fully account for both: Higher benefits in terms of pain relief and function as well as increased potential risks and complications after TKA.
Acknowledgements
None
Abbreviations
- OA
Osteoarthritis
- TKA
Total knee arthroplasty
- BMI
Body Mass Index
- WHO
World Health Organisation
- WOMAC
Western Ontario and McMaster Universities Osteoarthritis Index
- EQ-5D
EuroQol 5D
- CR
Cruciate retaining
- PRO
Patient reported outcome
Authors’ contributions
KG and JMG were involved in conceptualization and design of the study. AL, DH, JR and KG were involved in analysis and interpretation of the data. AL and JMG were drafting the manuscript. All authors edited, read and approved the final manuscript.
Funding
No direct support for this project was received.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available as access to the relevant institutional database is restricted to the public, but data are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethics approval for this study was obtained from the Ethics Committee of Eastern Switzerland EKOS (Ethikkommission Ostschweiz; trial registration number 2020–00879 from 16.04.2020). All methods were carried out in accordance with relevant guidelines and regulations.
All patients provided informed consent to take part in the study.
Consent for publication
All patients provided informed consent to take part in the study.
Competing interests
DH reports research support from Stryker and to have held paid presentations for the same company. The other authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr Cartil. 2013;21(9):1145–53. [cited 2020 Apr 14] Available from: http://www.ncbi.nlm.nih.gov/pubmed/23973124 [DOI] [PMC free article] [PubMed]
- 2.Feng JE, Novikov D, Anoushiravani AA, Schwarzkopf R. Total knee arthroplasty: Improving outcomes with a multidisciplinary approach. J Multidisciplinary Healthcare. 2018;11:63–73. [DOI] [PMC free article] [PubMed]
- 3.Hamilton D, Henderson GR, Gaston P, MacDonald D, Howie C, Simpson AHRW. Comparative outcomes of total hip and knee arthroplasty: A prospective cohort study. Postgrad Med J. 2012;88(1045):627–31. [cited 2020 Aug 29] Available from: https://pubmed.ncbi.nlm.nih.gov/22822221/ [DOI] [PubMed]
- 4.National Joint Registry 15th Annual Report 2018 – HQIP. [cited 2020 Aug 29]. Available from: https://www.hqip.org.uk/resource/national-joint-registry-15th-annual-report-2018/#.X0o-aNMzbuw
- 5.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991–2010. JAMA - J Am Med Assoc. 2012;308(12):1227–36. [cited 2020 Aug 29] Available from: www.jama.com. [DOI] [PMC free article] [PubMed]
- 6.Boyce L, Prasad A, Barrett M, Dawson-Bowling S, Millington S, Hanna SA, et al. The outcomes of total knee arthroplasty in morbidly obese patients: a systematic review of the literature. Arch Orthopaedic Trauma Surg. 2019;139:553–60. [cited 2020 Apr 13] Available from: 10.1007/s00402-019-03127-5 [DOI] [PMC free article] [PubMed]
- 7.Bonasia DE, Palazzolo A, Cottino U, Saccia F, Mazzola C, Rosso F, et al. Modifiable and nonmodifiable predictive factors associated with the outcomes of total knee arthroplasty. Joints. 2019;7(1):13–18. doi: 10.1055/s-0039-1678563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu S, Chen JY, Lo NN, Chia SL, Tay DKJ, Pang HN, et al. The influence of obesity on functional outcome and quality of life after total knee arthroplasty. Bone Jt J. 2018;100B(5):579–583. doi: 10.1302/0301-620X.100B5.BJJ-2017-1263.R1. [DOI] [PubMed] [Google Scholar]
- 9.Keeney BJ, Austin DC, Jevsevar DS. Preoperative Weight Loss for Morbidly Obese Patients Undergoing Total Knee Arthroplasty: Determining the Necessary Amount. J Bone Jt Surg - Am Vol. 2019;101(16):1440–50. [cited 2021 Mar 31] Available from: https://pubmed.ncbi.nlm.nih.gov/31436651/ [DOI] [PubMed]
- 10.Martin JR, Jennings JM, Dennis DA. Morbid obesity and total knee arthroplasty: A growing problem. Vol. 25, Journal of the American Academy of Orthopaedic Surgeons. Lippincott Williams and Wilkins; 2017; 188–94. [cited 2020 Apr 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/28146438 [DOI] [PubMed]
- 11.Gandhi R, Wasserstein D, Razak F, Davey JR, Mahomed NN. BMI independently predicts younger age at hip and knee replacement. Obesity. 2010;18(12):2362–6. [cited 2020 Apr 10] Available from: http://www.ncbi.nlm.nih.gov/pubmed/20379147 [DOI] [PubMed]
- 12.Di Cesare M, Bentham J, Stevens GA, Zhou B, Danaei G, Lu Y, et al. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016 Apr 2;387(10026):1377–96. [DOI] [PMC free article] [PubMed]
- 13.Uccioli L, Monticone G, Russo F, Mormile F, Durola L, Mennuni G, et al. OBESITY: PREVENTING AND MANAGING THE GLOBAL EPIDEMIC. WHO Tech Rep Ser. 1994;37(10):1051–5. [cited 2020 Apr 7] Available from: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/
- 14.Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377(9765):557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Y, Chen X. How Much of Racial/Ethnic Disparities in Dietary Intakes, Exercise, and Weight Status Can Be Explained by Nutrition- and Health-Related Psychosocial Factors and Socioeconomic Status among US Adults? J Am Diet Assoc. 2011;111(12):1904–11. [cited 2020 Aug 29] Available from: https://pubmed.ncbi.nlm.nih.gov/22117667/ [DOI] [PMC free article] [PubMed]
- 16.Si H bo, Zeng Y, Shen B, Yang J, Zhou Z ke, Kang P de, et al. The influence of body mass index on the outcomes of primary total knee arthroplasty. Vol. 23, Knee Surgery, Sports Traumatology, Arthroscopy. Springer Verlag; 2015; 1824–32. [cited 2020 Apr 14] Available from: http://www.ncbi.nlm.nih.gov/pubmed/25217315 [DOI] [PubMed]
- 17.Chen JY, Lo NN, Chong HC, Bin Abd Razak HR, Pang HN, Tay DKJ, et al. The influence of body mass index on functional outcome and quality of life after total knee arthroplasty. Bone Jt J. 2016;98-B(6):780–5. [cited 2020 Apr 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/27235520 [DOI] [PubMed]
- 18.Abdel MP, Bonadurer GF, Jennings MT, Hanssen AD. Increased Aseptic Tibial Failures in Patients With a BMI ≥35 and Well-Aligned Total Knee Arthroplasties. J Arthroplasty. 2015;30(12):2181–4. [cited 2020 Apr 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/26220103 [DOI] [PubMed]
- 19.Baker P, Petheram T, Jameson S, Reed M, Gregg P, Deehan D. The association between body mass index and the outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2012;94(16):1501–8. [cited 2020 Apr 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/22992819 [DOI] [PubMed]
- 20.Kerkhoffs GMMJ, Servien E, Dunn W, Dahm D, Bramer JAM, Haverkamp D. The influence of obesity on the complication rate and outcome of total knee arthroplasty: A meta-analysis and systematic literature review. J Bone Jt Surg - Ser A. 2012;94(20):1839–44. [cited 2020 Apr 13] Available from: http://dx.doi.org/10.2106/JBJS.K.00820 [DOI] [PMC free article] [PubMed]
- 21.Rissman CM, Keeney BJ, Ercolano EM, Koenig KM. Predictors of Facility Discharge, Range of Motion, and Patient-Reported Physical Function Improvement After Primary Total Knee Arthroplasty: A Prospective Cohort Analysis. J Arthroplasty. 2016;31(1):36–41. [cited 2021 Mar 31] Available from: /pmc/articles/PMC4691374/ [DOI] [PMC free article] [PubMed]
- 22.D’Apuzzo MR, Novicoff WM, Browne JA. The John Insall Award: Morbid Obesity Independently Impacts Complications, Mortality, and Resource Use After TKA. Clin Orthop Relat Res. 2015;473(1):57–63. [cited 2021 Mar 31] Available from: https://pubmed.ncbi.nlm.nih.gov/24818736/ [DOI] [PMC free article] [PubMed]
- 23.Sun K, Li H. Body mass index as a predictor of outcome in total knee replace: A systemic review and meta-analysis. Knee. 2017;24(5):917–24. [cited 2020 Aug 29] Available from: https://pubmed.ncbi.nlm.nih.gov/28666646/ [DOI] [PubMed]
- 24.Adhikary SD, Liu WM, Memtsoudis SG, Davis CM, Liu J. Body Mass Index More Than 45 kg/m2 as a Cutoff Point Is Associated With Dramatically Increased Postoperative Complications in Total Knee Arthroplasty and Total Hip Arthroplasty. J Arthroplasty. 2016;31(4):749–53. [cited 2020 Apr 14] Available from: http://www.ncbi.nlm.nih.gov/pubmed/26652477 [DOI] [PubMed]
- 25.Bordini B, Stea S, Cremonini S, Viceconti M, De Palma R, Toni A. Relationship between obesity and early failure of total knee prostheses. BMC Musculoskelet Disord. 2009;10:29. doi: 10.1186/1471-2474-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keeney BJ, Koenig KM, Paddock NG, Moschetti WE, Sparks MB, Jevsevar DS. Do Aggregate Socioeconomic Status Factors Predict Outcomes for Total Knee Arthroplasty in a Rural Population? J Arthroplasty. 2017;32(12):3583–90. [cited 2021 Mar 31] Available from: /pmc/articles/PMC5693700/ [DOI] [PMC free article] [PubMed]
- 27.Li W, Ayers DC, Lewis CG, Bowen TR, Allison JJ, Franklin PD. Functional Gain and Pain Relief after Total Joint Replacement According to Obesity Status. J Bone Jt Surg - Am Vol. 2017;99(14):1183–9. [cited 2020 Aug 29] Available from: https://pubmed.ncbi.nlm.nih.gov/28719557/ [DOI] [PMC free article] [PubMed]
- 28.Collins JE, Donnell-Fink LA, Yang HY, Usiskin IM, Lape EC, Wright J, et al. Effect of Obesity on Pain and Functional Recovery Following Total Knee Arthroplasty. J Bone Joint Surg Am. 2017;99(21):1812–8. [cited 2020 Aug 29] Available from: https://pubmed.ncbi.nlm.nih.gov/29088035/ [DOI] [PMC free article] [PubMed]
- 29.Giesinger JM, Loth FL, MacDonald DJ, Giesinger K, Patton JT, Simpson AHRW, et al. Patient-reported outcome metrics following total knee arthroplasty are influenced differently by patients’ body mass index. Knee Surgery, Sport Traumatol Arthrosc. 2018;26(11):3257–64. [cited 2020 Apr 14] Available from: http://www.ncbi.nlm.nih.gov/pubmed/29417168 [DOI] [PMC free article] [PubMed]
- 30.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40. [cited 2018 Jul 16] Available from: http://www.ncbi.nlm.nih.gov/pubmed/3068365 [PubMed]
- 31.Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower ex. Arthritis Rheum. 2001;45(4):384–391. doi: 10.1002/1529-0131(200108)45:4<384::AID-ART352>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 32.The EuroQol Group. EuroQol - a new facility for the measurement of health-related quality of life. Health Policy (New York). 1990;16(3):199–208. [DOI] [PubMed]
- 33.Conner-Spady BL, Marshall DA, Bohm E, Dunbar MJ, Loucks L, Khudairy A Al, et al. Reliability and validity of the EQ-5D-5L compared to the EQ-5D-3L in patients with osteoarthritis referred for hip and knee replacement. Qual Life Res. 2015;24(7):1775–84. [cited 2020 Apr 7] Available from: http://www.ncbi.nlm.nih.gov/pubmed/25555837 [DOI] [PubMed]
- 34.Amin AK, Clayton RAE, Patton JT, Gaston M, Cook RE, Brenkel IJ. Total knee replacement in morbidly obese patients: Results of a prospective, matched study. J Bone Jt Surg - Ser B. 2006;88(10):1321–6. [cited 2020 Apr 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/17012421 [DOI] [PubMed]
- 35.Lash H, Hooper G, Hooper N, Frampton C. Should a Patients BMI Status be Used to Restrict Access to Total Hip and Knee Arthroplasty? Functional Outcomes of Arthroplasty Relative to BMI - Single Centre Retrospective Review. Open Orthop J. 2013;7(1):594–599. doi: 10.2174/1874325001307010594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dewan A, Bertolusso R, Karastinos A, Conditt M, Noble PC, Parsley BS. Implant Durability and Knee Function After Total Knee Arthroplasty in the Morbidly Obese Patient. J Arthroplasty. 2009;24(6 SUPPL.):89–94, 94.e1–3. [cited 2020 Apr 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/19576727 [DOI] [PubMed]
- 37.Werner BC, Evans CL, Carothers JT, Browne JA. Primary Total Knee Arthroplasty in Super-obese Patients: Dramatically Higher Postoperative Complication Rates Even Compared to Revision Surgery. J Arthroplasty. 2015;30(5):849–53. [cited 2020 Apr 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/25577726 [DOI] [PubMed]
- 38.Naziri Q, Issa K, Malkani AL, Bonutti PM, Harwin SF, Mont MA. Bariatric orthopaedics: Total knee arthroplasty in super-obese patients (BMI > 50 kg/m 2 ). Survivorship and complications. Clin Orthop Relat Res. 2013;471(11):3523–30. [DOI] [PMC free article] [PubMed]
- 39.Krushell RJ, Fingeroth RJ. Primary Total Knee Arthroplasty in Morbidly Obese Patients. A 5- to 14-Year Follow-up Study. J Arthroplasty. 2007;22(6 SUPPL.):77–80. [cited 2020 Apr 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/17823021 [DOI] [PubMed]
- 40.Jia H, Zack MM, Thompson WW. Population-based estimates of decreases in quality-adjusted life expectancy associated with unhealthy body mass index. Public Health Rep. 2016;131(1):177–84. [cited 2020 Jun 20] Available from: /pmc/articles/PMC4716486/?report=abstract [DOI] [PMC free article] [PubMed]
- 41.Lung T, Jan S, Tan EJ, Killedar A, Hayes A. Impact of overweight, obesity and severe obesity on life expectancy of Australian adults. Int J Obes. 2019;43(4):782–9. [cited 2020 Jun 20] Available from: https://pubmed.ncbi.nlm.nih.gov/30283076/ [DOI] [PubMed]
- 42.Finkelstein EA, Brown DS, Wrage LA, Allaire BT, Hoerger TJ. Individual and aggregate years-of-life-lost associated with overweight and obesity. Obesity (Silver Spring). 2010;18(2):333–9. [cited 2020 Jun 20] Available from: http://www.ncbi.nlm.nih.gov/pubmed/19680230 [DOI] [PubMed]
- 43.MacMahon S, Baigent C, Duffy S, Rodgers A, Tominaga S, Chambless L, et al. Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96. [cited 2020 Aug 29] Available from: http://www.ctsu. [DOI] [PMC free article] [PubMed]
- 44.Khan SS, Ning H, Wilkins JT, Allen N, Carnethon M, Berry JD, et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 2018;3(4):280–7. [cited 2020 Aug 29] Available from: /pmc/articles/PMC5875319/?report=abstract [DOI] [PMC free article] [PubMed]
- 45.Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6(12):944–53. [cited 2020 Aug 29] Available from: www.thelancet.com/diabetes-endocrinology [DOI] [PMC free article] [PubMed]
- 46.Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, et al. Cost-effectiveness of total knee arthroplasty in the United States: Patient risk and hospital volume. Arch Intern Med. 2009;169(12):1113–21. [cited 2020 Apr 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/19546411 [DOI] [PMC free article] [PubMed]
- 47.Changulani M, Kalairajah Y, Peel T, Field RE. The relationship between obesity and the age at which hip and knee replacement is undertaken. J Bone Jt Surg - Ser B. 2008;90(3):360–363. doi: 10.1302/0301-620X.90B3.19782. [DOI] [PubMed] [Google Scholar]
- 48.Ast MP, Abdel MP, Lee Y, Lyman S, Ruel A V., Westrich GH. Weight Changes After Total Hip or Knee Arthroplasty. J Bone Jt Surg. 2015;97(11):911–9. [cited 2021 Mar 31] Available from: https://journals.lww.com/00004623-201506030-00005 [DOI] [PubMed]
- 49.Razzaki T, Mak WK, Bin Abd Razak HR, Tan HCA. Patterns of Weight Change and Their Effects on Clinical Outcomes Following Total Knee Arthroplasty in an Asian Population. J Arthroplasty. 2020;35(2):375–9. [cited 2020 Apr 14] Available from: http://www.ncbi.nlm.nih.gov/pubmed/31563395 [DOI] [PubMed]
- 50.Schwartsmann CR, Borges AM, Freitas GLS de, Migon EZ, Oliveira GK de, Rodrigues MW. Do patients lose weight after total knee replacement? Rev Bras Ortop (English Ed. 2017;52(2):159–63. [cited 2020 Apr 14] Available from: http://www.ncbi.nlm.nih.gov/pubmed/28409132 [DOI] [PMC free article] [PubMed]
- 51.Kandil A, Novicoff WM, Browne JA. Obesity and total joint arthroplasty: Do patients lose weight following surgery? Phys Sportsmed. 2013;41(2):34–7. [cited 2020 Apr 14] Available from: http://www.ncbi.nlm.nih.gov/pubmed/23703515 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analysed during the current study are not publicly available as access to the relevant institutional database is restricted to the public, but data are available from the corresponding author on reasonable request.