Abstract
Due to the immediate need for social distancing, as well as widespread disruption in clinical practices, brought on by the novel severe acute respiratory syndrome coronavirus 2 (COVID-19) pandemic, medical student education rapidly shifted to a virtual format, which resulted in a variety of innovative and remotely accessible practices to address new restrictions on face-to-face education. Educators approached curriculum design seeking to replicate as much of the in-person experience as possible, and were faced with overcoming the challenges of replacing the innately hands-on nature of surgery with virtual operative and skills experiences. Restrictions on in-person visiting electives expedited the role of virtual education as a notable opportunity for medical student education and recruitment, with a variety of approaches to engaging undergraduate medical learners, including the use of live-streaming operative cases, virtual didactic curricula, and a rise in podcasts; web-based conferences; and virtual journal clubs. In addition to education, virtual outreach to medical students has become an essential tool in trainee recruitment and selection, and ongoing application of novel educational platforms will allow for new opportunities in multi-institutional collaboration and exchange with a multitude of benefits to future vascular surgery trainees. Our aim was to outline the resources and practices used to virtually teach and recruit medical students and the benefits of virtual rotations to the program and students.
1. Introduction
Shortly after the first cases were noted in the United States in January 2020, the implications of the novel severe acute respiratory syndrome coronavirus 2 (COVID-19) to the health care system were profound. Medical education faced enormous challenges, but shifted rapidly to a virtual format, resulting in a variety of innovative and remotely accessible practices to address new restrictions on face-to-face medical student education [1], [2], [3].
With medical centers cessation of in-person clerkships and transitioning to remote learning, students were confronted with the inability to perform physical examinations, decreased in-person interaction with peers and educators, and curtailed ability to help in a time of great need [1]. However, despite many detractions to medical student education, many positive attributes have also been discovered, including use of remote learning to collaborate with other universities and hospitals and cost savings from reduced need for travel [2]. Our aim was to outline the resources and practices used to teach and recruit medical students virtually.
2. Development of virtual vascular surgery electives
The COVID-19 pandemic served as the impetus for the development of virtual vascular surgery rotations, focusing on decreasing patient and hands-on interaction, but ensuring a high-value and appropriate preparatory education for practice. The technologies for virtual surgical education and e-learning have been available and explored before the pandemic; however, enthusiasm for this modality has been aimed more at supplementing other educational opportunities than the primary form of teaching [4]. Medical students’ education was limited by the pandemic not only due to the need for social distancing and avoidance of group gatherings, but also by the repurposing and conservation of the physician workforce that would otherwise contribute to their education.
Fourth-year medical students were particularly affected, as that year has traditionally afforded students a different degree of freedom in their rotations, allowing for home and visiting electives to support their candidacy and exposure to their chosen field [5]. Visiting or “away” electives have been pursued historically by applicants in highly competitive specialties and have become almost universal in applicants to vascular surgery programs [6]. These educational opportunities that occur at institutions other than the student's home institution allow for more in-depth exploration of the specialty, exposure to different practice environments and case mixes, and often serve as a month-long audition, especially in programs for which the applicant has particular interest [7]. With concerns about the safety of travel as well as variable institution-based practices restricting visitors during a period of increasing prevalence and mortality from COVID-19, the Coalition for Physician Accountability formalized guidelines regarding visiting students, greatly discouraging, if not prohibiting, visiting electives except in certain unique circumstances [7], [8], [9], [10]. Virtual acting internships and electives emerged from several vascular surgery programs throughout the country seeking to accomplish many of the goals of previous, in-person opportunities.
Educators in vascular surgery faced the challenge head on with designing and implementing an educational program in a short period of time that focused on simulating the in-person environment as much as possible; it prioritized a virtual operative experience, providing live, interactive didactic material; skills assessments of participants; and professional development, while providing mentorship of students with faculty and residents [5]. Students applied to virtual electives in vascular surgery via the American Association of Medical Colleges Visiting Student Learning Opportunities Application Service or through institutional recruitment (Table 1 ). Course content varied by institution based on rotation goals and objectives, as well as length of rotation (Table 2 ). Courses had syllabi with clearly defined goals and objectives, as well as structured time for interactive activities. The available courses ranged from 1 to 4 weeks; students selected courses based on specific course content (Table 3 ), interest in the hosting program, and the length of the program. All courses followed a pass/fail grading format as guided by institutional practices and encouraged by Liaison Committee on Medical Education, which similarly determined whether the course was offered for credit; the latter was also affected by policies of the visiting students’ home institution [11].
Table 1.
Sites offering virtual vascular surgery rotations and recruitment
| University of South Florida Morsani (USF) |
| Medical University of South Carolina (MUSC) |
| Yale School of Medicine |
| Stanford |
| University of California Davis (UC Davis) |
| University of Michigan (U Michigan) |
| University of California San Diego (UCSD) |
| Louisiana State University (LSU) |
| University of Pittsburgh |
| Mount Sinai |
| University of Alabama (UAB) |
Table 2.
Characteristics of virtual acting internships.
| Institution | Length, wk | Rotations offered, n | Mode of assessment | Grading | Credit | Cost, $ |
|---|---|---|---|---|---|---|
| LSU | 4 | 2 | Skills assessment | Pass/fail | Yes | 0 |
| UC Davis | 2 | 1 | Skills assessment | Pass/fail | Yes | 0 |
| Stanford | 1 | 3 | NA | NA | No | 0 |
| USF | 4 | 4 | Skills assessment Student presentation Operative notes/postoperative orders |
Pass/fail | Yes | 0 |
| Yale | 2 | 1 | 11NA11 | Pass/fail | Yes | 0 |
| U Mich | 4 | 3 | Student presentation | Pass/fail | Yes | 0 |
| MUSC | 2 | 8 | Skills assessment | Pass/fail | Yes | 0 |
Abbreviations: LSU, Louisiana State University; MUSC, Medical University of South Carolina; NA, not available; UC, University of California; U Mich, University of Michigan; USF, University of South Florida Morsani.
Table 3.
Content of virtual acting internships.
| Institution | Virtual skills | Livestream OR | Didactic content | Virtual patient care |
|---|---|---|---|---|
| LSU | Yes | No | Daily | Virtual rounds |
| UC Davis | Yes | No | Daily | Virtual rounds |
| Stanford | No | No | Daily | NA |
| USF | Yes | No | Daily | NA |
| Yale | No | Yes | Daily | Virtual patient interaction |
| U Mich | No | No | 2–3 times/wk | Virtual rounds Virtual patient interaction |
| MUSC | Yes | Yes | 1–2 times/wk | Virtual rounds Virtual patient interaction |
Abbreviations: LSU, Louisiana State University; MUSC, Medical University of South Carolina; OR, operating room; UC, University of California; U Mich, University of Michigan; USF, University of South Florida Morsani.
Organization of virtual education was facilitated by selection of the communication platform. The most commonly used programs were Microsoft Teams, Zoom (Zoom Video Communications, San Jose, CA), or WebEx (Cisco Webex, Milpitas, CA), with additional utilization of cloud-based storage as a repository for course syllabi, recorded material, and supplemental educational resources. Selection of the communication platform was based on cost, availability, ease of use, and ability to achieve interactivity. Drawbacks to all modalities included reliability of security due to Health Insurance Portability and Accountability Act (HIPAA) considerations, fidelity of internet connectivity, and quality of image sharing [12]. Additional modalities of communication during virtual education included use of social media (Facebook, Instagram, and Twitter), standard e-mail exchange, and, in some instances, app-based or short-message service (text) messaging.
3. Operative curriculum: livestream operating room
The design of an operative curriculum in a virtual format was a particular challenge, given the hands-on nature of vascular surgery. For fourth-year students, in particular, elective rotations afford an additional opportunity to showcase technical skills, as well as continue to hone them in preparation for their intern year. Institutions turned to a variety of options to make up for lost time in the operating room, including the use of high-quality prerecorded videos available on YouTube (YouTube, San Bruno, CA) or other institution-sponsored websites. Other programs coordinated live-streaming videos of vascular surgical cases with opportunity for real-time teaching and exchange with students [7,12].
The use of a livestream operating room (LOR) is not a novel concept. It has been used historically, for example, as part of technical skills courses and scientific meetings. Recently, groups have described the use of LOR in both plastic surgery and neurosurgery as a means to educate medical students and residents [4,7,9,13]. These experiences used a HIPAA-compliant conferencing platform with a combination of OR light-mounted cameras, microscopes, and portable cameras on head mounts [6,7].
Colleagues at Yale Vascular Surgery used a magnified camera, with a built-in microphone (SurgiTel, Ann Arbor, MI) (Fig. 1 ). The camera provided a similar magnification as a 2.5 × loupe vision with high visual and audio clarity. This system was used in concert with a HIPAA-compliant Zoom platform. This allowed learners to see and hear the surgeon and team. Also, a large television was in the operating room, allowing the surgeon to see and interact with the learners when appropriate. Other video modalities that have been described include the use of head-mounted GoPro cameras (GoPro, Inc., San Mateo, CA) coupled with Bluetooth audio [14], [15], [16].
Fig. 1.
SurgiTel high-definition camera.
Learners found the LOR to be enriching to their learning experience. In addition, learners felt that “being” in the OR allowed a real-time surgical experience that cannot be garnered from videos or other content available. Similarly, it allowed faculty an opportunity to both evaluate and become acquainted with the learners.
Institution of LOR does require a significant amount of technical resources, with both equipment and dedicated technicians to help with the setup. Permission from patients is also critical beyond what is outlined in the consent. Finally, faculty buy-in for the experience is of paramount importance to ensure an optimal learning experience in the LOR.
4. Virtual skills teaching and assessment
At the University of South Florida, a virtual skills course was created to facilitate hands-on education during the COVID-19 pandemic and supplement the virtual operative experience. The need for social distancing limited student education, especially in surgery and surgical subspecialties. As a solution, we created a 4-week, technical skills course that would focus on building their technical repertoire.
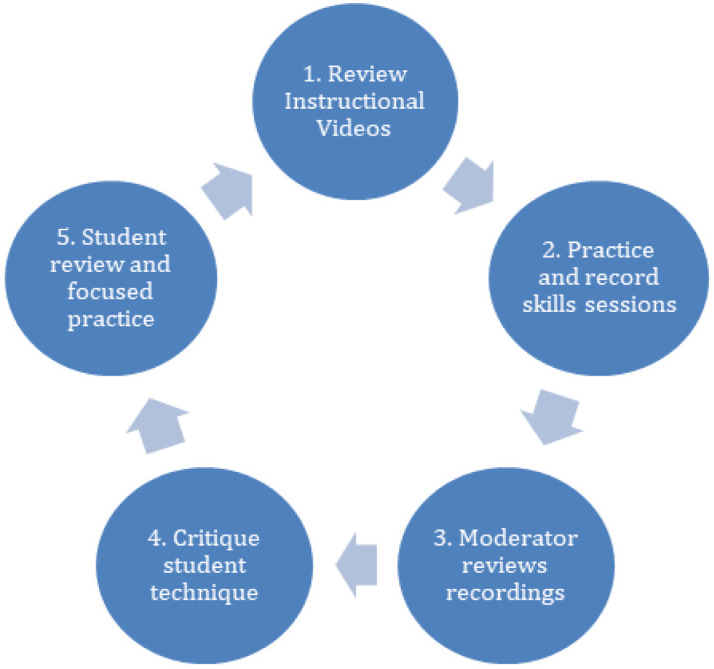
The course revolved around teaching specific technical skills. Students were asked to review instructional skills-based videos (YouTube Channel: The Clean Scalpel) before virtual meetings. After the first introductory session, each student would have to send skills-content (video recordings) to the moderator. The moderator would review the video and give constructive criticism along with specific objectives to be accomplished for their next task. At the time of subsequent sessions, questions about the skill would be answered and then the remainder of the class was devoted to reviewing student-derived skills content (Fig. 2 ). This was a formative opportunity for the students to compare their own technical skills with a particular task with their peers. It also provided a forum where the students could discuss the difficulties they were facing. This rapport helped facilitate resolutions that may not have come easily. In our experience, it drove students to a higher level of mastery and collegiality.
Fig. 2.
Feedback loop for virtual surgical technique.
Clear and specific articulation of goals was paramount to having students progress through the session. One of our early goals was to ensure the students could perform two-handed and one-handed surgical knots. The student would have to achieve 20 knots per minute with two-handed knots before moving on to one-handed knots—with a benchmark goal of 30 knots per minute. Other technical benchmarks are presented in Table 4 .
Table 4.
Skills and assessment targets.
| Skill | Target |
|---|---|
| Two-handed knots | 20 knots/min |
| One-handed knots | 30 knots/min |
| Handling needle | Using the driver in palm/fingers in loop |
| Forehand consistency | Loading/taking bites |
| Needle reloading | Accuracy |
| Tissue handling | Lack of trauma or tearing |
| Needle manipulation | Consistency |
| Backhand consistency | Loading/taking bites |
This skills course was an opportunity to provide students the much-needed technical training that they were seeking. It also allowed for students to have face time with faculty and has been a valuable recruitment tool. The students’ individual progress at their own pace and the course provided good insight into the student's level of maturity for adult learning. As such, it has been a good tool to help differentiate applicants in an otherwise very competitive applicant pool.
5. Application of surgical video libraries
Many programs used prerecorded, edited surgical videos available on YouTube or institutional websites. The course directors selected their representative videos based on validity and educational value and presented students with a prescribed list of case videos, avoiding lower-quality, albeit popular, videos that less informed learners might select [17]. Many of the programs selected course videos from the Houston Methodist DeBakey CV Education YouTube channel, which has more than 40,000 subscribers and offers a repository of high-quality videos on a breadth of vascular surgical procedures. Students were expected to prepare for these virtual cases as they would in-person operations and reviewed videos during their “virtual OR” period during their electives. A key component of the virtual OR experience was reinforcing students’ understanding of key operative steps; this was done through supplemental didactic sessions or case review conferences [15]. At the University of South Florida, for example, after each index vascular case, students submitted an operative dictation to reinforce comprehensive understanding of the operation (as often the videos would communicate the key steps of an operation but not at the level of granularity a student would experience in a live operating room).
6. Remote mentoring
The opportunity for virtual mentorship in the context of virtual education was a huge draw to the experience for students and sought to mirror the practices experienced during in-person electives. Rotations included sessions with current trainees, as well as a diversity of faculty members, including vascular division and educational leadership. In some instances, students were assigned to designated faculty mentors or resident mentors, with whom they were encouraged to “meet” during the course of their rotations. Many resident trainees took additional initiative in reaching out to medical students, often offering to read over personal statements, to hold individual meetings in order to answer questions regarding residency and interview processes, and to discuss possible research projects in which the students could participate. Faculty found that the dedicated time with students, even in a virtual format, afforded a degree of interaction in excess of what they ordinarily experience during in-person electives. Similarly, students found both faculty and residents to be very accessible and exceeded their expectations for the virtual elective (unpublished results). In numerous instances, participating students asked for letters of recommendation from their virtual electives; the prevalence and impact of these letters is a subject for future research.
7. Virtual education as a recruitment tool
Although medical students did benefit academically and technically from didactic and skills sessions in the virtual rotation, they were also given multiple opportunities to learn more about the program itself from virtual “meet and greet” events at a variety of institutions, as well as a Vascular Surgery Residency Fair sponsored by the Vascular and Endovascular Surgery Society (Table 5 ). This benefited the residency program, as it allowed further opportunity to engage the medical students outside of their rotation for recruitment purposes. The “meet and greet” event hosted once per rotation was a virtual opportunity in which students and residents were able to discuss questions about the residency, applications to programs, faculty, and research.
Table 5.
Recruitment tools used during the pandemic.
| Recruitment sources | Description |
|---|---|
| Virtual “meet and greet” | Single center or multicenter |
| Society sponsored fairs | Multicenter with catchment of more medical students |
| Social media | Site and user-specific modalities (ie, Twitter, Facebook, and Instagram) |
The residency fair event, held in September 2020, involved multiple residency programs linked via a Zoom meeting. Students were able to exit and enter rooms where faculty and residents from different programs were available to answer questions and provide information about their residency. This meeting was not limited to students in any one virtual elective at that point in time, but instead, included any medical students that could potentially have an interest in vascular surgery. This also allowed programs the opportunity to meet potential applicants before their interview session to assist with the recruitment process. A total of 45 integrated vascular surgery residency programs participated in the event, with 168 students (68.8% in their final year of medical school) participating [9].
Social media, including Instagram (Instagram, Menlo Park, CA) and Twitter (Twitter, San Francisco, CA) was also a useful communication tool during the pandemic for students to see in snapshots the daily lives of trainees and faculty at different programs. Many trainees posted images of pets, weddings, children, hospital locations, and daily activities at work in efforts to further medical student interest and attract applicants, seeking to humanize an otherwise virtual process.
8. Benefits and future of virtual education and recruitment
8.1. Decreased cost
Traditionally, travel, housing, and transportation are all added costs and factors that students have had to navigate in order to participate in an in-person environment. In a 2015 survey of medical students, the average cost of an away rotation was $958, with overall costs for highly competitive specialties expecting more away rotations being in excess of $3,500 [10,18]. Virtual electives remove those factors, making them more accessible to more students who potentially cannot afford the experience [10].
8.2. Flexibility
Students were able to participate in several rotations at the same time in the virtual environment. During hours when they may not be actively participating in the virtual rotation, many would be rotating on other electives at the same time. This afforded them the chance to experience multiple rotations rather than a select few and experience more programs before applying for interviews.
8.3. Increased student catchment
Vascular surgery does not have a strong presence at every institution across the country, and many programs do not have an integrated vascular residency. Students often apply for acting internships at other institutions to get a significant vascular surgery rotation. For this reason, virtual rotations have taken a very positive role. Students without integrated residencies for vascular or with a weaker vascular presence at their home institutions can experience vascular surgery at high-volume tertiary referral centers in a virtual environment. This in turn allows for rotations to have more student capacity, increasing their rotating student volume.
8.4. More single-site exposure
Unlike in-person rotations where students are potentially relegated to one site, virtual rotation students were given the unique opportunity to meet the entire body of faculty and trainees through various didactic and skills sessions offered throughout the course. In addition, resident meetings were offered in which all trainees were present and answering questions for the students.
8.5. Earlier recruitment in medical school
Although programs can get a mix of students in virtual rotations who may or may not have chosen vascular surgery as a career, it allows them the opportunity to expand interest in the vascular surgery field as a whole and educate a wider variety of medical students on the field itself. The virtual rotation is available to all medical students and can help promote involvement and recruitment of underrepresented minorities at a fraction of the cost of a traditional rotation. Virtual rotations are more accessible for students as a whole.
8.6. Favorable student experience
Overall, students participating in virtual electives have offered favorable reviews of the experience, often indicating that their expectations were exceeded. Although the obvious limitations of lack of hands-on experience and absence of real-time patient care persist, this was countered by an increase in access to faculty and residents, as well as more in-depth exploration of topics aimed at preparation for intern year, such as postoperative orders, dictations, and admitting and discharging patients that are historically part of “on the job training” and represent the value of acting internships.
8.7. Increased collaboration between programs
The benefits of the virtual rotation to medical students cannot be overstated, but it is not only the medical students that gain from the virtual format; vascular surgery programs benefit as well. It has allowed programs to interact with other programs across the nation through participation in journal clubs, lectures, and case presentations. This has increased program cohesiveness and opened networking opportunities for residents and faculty outside of standard conferences, with the goal of optimizing student engagement and recruitment, and representing the strengths of vascular surgery as a field.
9. Future of virtual rotations and recruitment
Although a remote or virtual experience is unlikely to replace an in-person experience when COVID-19 restrictions are lifted, they will likely maintain a role in medical student education. The future role of virtual rotations and recruitment will be relegated to benefits that they offer. Virtual rotations can continue for early exposure in the nonclinical years in medical school, for students that would like a high-volume, short-term experience into vascular surgery, or for students who are economically or regionally disadvantaged and cannot afford a traditional in-person rotation. It will also provide opportunities to students that may have otherwise not been able to travel or not see locations due to scheduling conflicts. As regards virtual recruitment, this will be dependent on the feedback from this previous match and its applicants.
10. Conclusions
Virtual acting internships have impacted medical student education during the COVID-19 pandemic. Previously, medical students would travel to rotate on electives located in various cities, but the pandemic restricted travel and fostered the use of virtual education. Virtual rotations positively changed the typical internship by allowing for a cost-effective means of experiencing a variety of programs, including in the program-specific curriculum design that reflects the educational culture and priorities of institutions. It remains to be seen whether enthusiasm for this education and recruitment modality will persist once COVID-19 vaccination is more widespread and travel restrictions are lifted. Although a virtual rotation will never be able to fully replace the utility of in-person operative and hands-on experiences, it has allowed for education to continue in an otherwise highly restrictive time due to viral outbreak, and offers new opportunities for education, outreach, and recruitment. The benefits of virtual rotations to both students and programs have created a new means of recruitment and education that will hopefully persist in the years to come.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
REFERENCES
- 1.Ahmed H, Allaf M, Elghazaly H. COVID-19 and medical education [published correction appears in Lancet Infect Dis. 2020 May;20(5):e79] Lancet Infect Dis. 2020;20:777–778. doi: 10.1016/S1473-3099(20)30226-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wijesooriya NR, Mishra V, Brand PLP, et al. COVID-19 and telehealth, education, and research adaptations. Paediatr Respir Rev. 2020;35:38–42. doi: 10.1016/j.prrv.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dedeilia A, Sotiropoulos MG, Hanrahan JG, et al. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In Vivo. 2020;34(suppl):1603–1611. doi: 10.21873/invivo.11950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akers A, Blough C, Iyer MS. COVID-19 implications on clinical clerkships and the residency application process for medical students. Cureus. 2020;12:e7800. doi: 10.7759/cureus.7800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Winterton M, Ahn J, Bernstein J. The prevalence and cost of medical student visiting rotations. BMC Med Educ. 2016;16:291. doi: 10.1186/s12909-016-0805-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilcha RJ. Effectiveness of virtual medical teaching during the COVID-19 crisis: systematic review. JMIR Med Educ. 2020;6(2):e20963. doi: 10.2196/20963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boyd CJ, Inglesby DC, Corey B, et al. Impact of COVID-19 on away rotations in surgical fields. J Surg Res. 2020;255:96–98. doi: 10.1016/j.jss.2020.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Medical student away rotations for remainder of 2020-21 and 21-22 academic year. Accessed March 3, 2021. Available at: https://www.aamc.org/what-we-do/mission-areas/medical-education/away-rotations-interviews-2020-21-residency-cycle.
- 9.Chung CY, Chandra V, Rectenwald J, et al. Abstract presented at: Association for Surgical Education Annual Meeting. 2020. The more, the merrier: virtual residency fair benefits both students and residency programs. April 29–May 1. [Google Scholar]
- 10.Asaad M, Glassman GE, Allam O. Virtual rotations during COVID-19: an opportunity for enhancing diversity. J Surg Res. 2021;260:516–519. doi: 10.1016/j.jss.2020.11.071. [DOI] [PubMed] [Google Scholar]
- 11.Althwanay A, Ahsan F, Oliveri F, et al. Medical education, pre- and post-pandemic era: a review article. Cureus. 2020;12(10):e10775. doi: 10.7759/cureus.10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.LCME UPdate on medical students, patients, and COVID-19: approaches to the clinical curriculum. Accessed March 4, 2021. Available at: https://lcme.org/wp-content/uploads/filebase/March-20-2020-LCME-Approaches-to-Clinical-Curriculum.pdf.
- 13.Chick RC, Clifton GT, Peace KM, et al. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020;77:729–732. doi: 10.1016/j.jsurg.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yuen JC, Gonzalez SR, Osborn T, et al. Untethered and HIPAA-compliant interactive livestreaming of surgery to residents and medical students. Plast Reconstr Surg Glob Open. 2020;8(10):e3165. doi: 10.1097/GOX.0000000000003165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chae JK, Haghdel A, Guadix SW, et al. COVID-19 impact on the medical student path to neurosurgery. Neurosurgery. 2020;87(2):E232–E233. doi: 10.1093/neuros/nyaa187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McKinley SK, Hashiomoto DA, Mansur A, et al. Feasibility and perceived usefulness of using head-mounted cameras for resident video portfolios. Surg Res. 2019;239:233–241. doi: 10.1016/j.jss.2019.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jack MM, Gattozzi DA, Camarata PJ, et al. Live-streaming surgery for medical student education—educational solutions in neurosurgery during the COVID-19 pandemic. J Surg Res. 2020;28:99–103. doi: 10.1016/j.jsurg.2020.07.005. [DOI] [PubMed] [Google Scholar]
- 18.Drolet BC, Brower JP, Lifchez SD, et al. Away rotations and matching in integrated plastic surgery residency: applicant and program director perspectives. Plast Reconstr Surg. 2016;137:1337–1343. doi: 10.1097/PRS.0000000000002029. [DOI] [PubMed] [Google Scholar]