Abstract
Objectives
This study aimed to examine discrepancies between self-report methods and methodological issues related to sexual risk taking. We examined sexual behaviour assessed via 3-month electronic recall and by daily electronic reporting among a large cohort of patients attending STI clinics.
Methods
STI clinic attenders (N= 628) aged 15 to 60 years reported on demographic information (at baseline), penile–vaginal sex acts, condom-unprotected penile–vaginal sex and STI history using 3-month recall and daily reports. Additionally, interviewer–participant match related to race and gender, as well as study site were considered as covariates.
Results
Concordance between recall and daily reports on penile–vaginal sex was moderately strong (Spearman’s r (rs)=0.62; p<0.001). Comparison for reports for condom-unprotected penile–vaginal sex resulted in a correlation coefficient of 0.61 (p<0.001), also indicating moderately strong agreement between the two methods. Two generalised logit models were conducted to explain lack of strong concordance in penile–vaginal sex acts and condom-unprotected penile–vaginal sex. The odds of a female reporting higher frequency of sex in daily reports compared with recall were more than two times that of a male. Every five person increase in the number of lifetime sexual partners was associated with five times the odds of a discrepancy in reporting methods. Age was also significantly associated with unequal daily versus recall sex frequency reporting.
Conclusions
Shifting focus to methodological considerations of technological reports can help ensure better investment of resources into sexual health research due to greater understanding of the methodological properties of data collection methods.
INTRODUCTION
Precise measurement in science is challenging, and measuring sexual behaviour poses a particularly complex set of issues. Such measurements are vital to public health efforts aimed at preventing the spread of HIV and other STIs.1,2 Unlike less private behaviours or those that can be inferred via blood, urine or exhalation tests, sexual behaviours are nearly always assessed by self-report.3–5 The most common methodological challenges in self-report involve the length of the reference interval (ie, recall period), frequency of the behaviour and method of measurement.6 Although shorter recall periods would seem to yield more accurate reports, one study found that 3-month retrospective reports could be as accurate as reports for a 1-month reference interval.7 On the other hand, shorter recall periods are not necessarily ideal for less frequent behaviour because measurement over a short interval may not generalise over weeks or months.6
A review article of sexual behaviour data collected via electronic daily diaries found a tendency for people to over-report behaviours when using retrospective methods compared with daily diary methods, an exception to this occurred for infrequent behaviours.8 Other research has documented that accuracy of the report decreases as frequency of the behaviour increases.9–11 An event occurring at a greater frequency may not be reported accurately due to digit preference (ie, a tendency to round numbers either up or down)9 and, possibly, the social context. The latter may lead to bias in self-reporting, depending on the extent to which social desirability or impression management concerns the participant.6
Socially desirable behaviours, such as condom use or STI testing, are more likely to be overreported, whereas behaviours that are socially unapproved, such as infidelity or positive STI status, are more likely to be under-reported.3–6,9 Social context and social desirability may be an especially important methodological concern in studying adolescent and young adult populations. For example, teens and young adults inaccurately recall condom use and provide socially desirable answers.12 Such bias may be reduced by using computer-based self-report rather than face-to-face interviewing.13,14
Given technological advances, improvements in data collection regarding sexual behaviours have been notable.6 Several studies have found that computer-based assessments lead to higher self-reporting of risky sexual behaviours versus assessments not conducted by computer.6,13–15 However, this is more plausibly due to the self-administration of the survey than to its computer-based nature.16,17
Although past research on this topic is diffuse, two basic questions have emerged. First, do people disclose more when their responses are made privately (as is true for computer-assisted methods)? Second, is memory error reduced by daily reporting versus less frequent recall? Numerous empirical investigations have amply addressed the first question11,14,18,19 to find that greater frequencies of sexual behaviours are reported when responses are not made to another person. Despite the benefits of data collection systems such as audio computer-assisted self-interview (A-CASI), accurate reporting of sexual behaviours may be distorted because of memory error.3,20 Daily electronic reporting may improve reliability by using shorter recall periods.4,21 In any case, a comparison of ‘like methods’ (eg, computer-based reporting for both the longer period and the daily period) is necessary to draw valid conclusions regarding memory error. Studies that compare two different recall periods without like methods (eg, one by personal interview and one by a computer-based method) are inherently confounded, although several of these have been published.22–26 Moreover, existing studies using like methods have been conducted with very small samples, college students or both.3–6,9,11,12 Thus, little is known about this measurement issue from studies involving large numbers of people with elevated risk of HIV/STIs. Additionally, little is known about the relationship between discrepancies in reporting and the impact of demographic and sexual behavioural variables (such as gender, age, sexual frequency) or demographic match with the researcher on accuracy of reports.
Accordingly, the purpose of the present study was to examine the discrepancies between self-reported sexual behaviours assessed via electronic recall using a 3-month period and daily electronic reporting, among a large cohort of patients attending clinics that diagnose HIV/STIs. More specifically, we sought to determine whether discrepancies in 3-month recall and daily reporting were related to the frequency of sexual activity, history of STI, gender, age and/or demographic match with the clinic researcher.
METHODS
Study design and participants
The data are from a study of condom effectiveness against non-viral STIs described elsewhere.27 Data collection began in December of 2007 and concluded in April of 2011. Briefly, 929 outpatients were recruited from five clinics that treat STIs in three US cities. Eligibility criteria included being age ≥15 at two adolescent medicine clinics and age ≥18 at three STI clinics, reporting penile–vaginal intercourse in the preceding 3 months, willingness to be tested for STIs and written informed consent (assent for patients age <18, with a waiver of parental consent).
At baseline and 3-month visits, participants completed an A-CASI to recall penile–vaginal events in the previous 3 months and were tested for STIs (see online supplemental file). Between visits, participants used a personal digital assistant (PDA) programmed with the configurable electronic real-time assessment system (CERTAS; Personal Improvement Computer Systems, Reston, Virginia, USA) to provide daily reports on each penile–vaginal event in the previous 24 hours. Participants were offered remuneration in gift cards based on the study activities completed (maximum amount was approximately US$2.50 per day of observation).
An auditory signal was emitted from the PDA once a day, prompting participants to indicate whether they had sex in the past 24 hours; participants were encouraged to enter a PDA report of penile–vaginal sexual encounter as soon after the act as possible. This daily ‘demand’ entry method precluded retrospective data entry into the PDAs. In addition, participants were asked to complete a report each time they had sex. To avoid counting the same event twice, participants were asked to indicate on the daily report if they had already reported the event. Of note, the technology used to capture the daily reports occasionally did not record the correct calendar date; about 3.6% of events described in the daily reports had unrecoverable calendar dates and were therefore excluded from analysis. All protocol were approved by the Institutional Review Board at University of Kentucky (Protocol #45927384).
Dataset construction
The original data set contained 17,156 daily sex event reports from 637 participants. Duplicate daily reports were removed (765 daily reports; 4.46% of total data) and data from seven subjects were removed because these participants did not report any sexual events during the study. Daily report data (6 daily reports; 0.03% of total data) from one participant was removed because sex frequency information was missing from the participant’s 3-month recall data. Erroneous data (eg, false reports) were also removed (1290 daily reports; one participant removed completely; 7.52% of total data). The final data set contained 15 095 daily sex event reports from 628 participants.
Data analysis
Descriptive statistics, including means with SDs for continuous variables and frequencies with percentages for categorical variables, were calculated for demographic, interviewer and sexual behaviour/history characteristics. These characteristics were stratified by both gender and age (divided into tertiles; ages 15–21, 22–36 and >37) and analysed using χ2 statistics for categorical variables and independent sample t-tests, one-way ANOVAs and paired-samples t-tests for continuous variables.
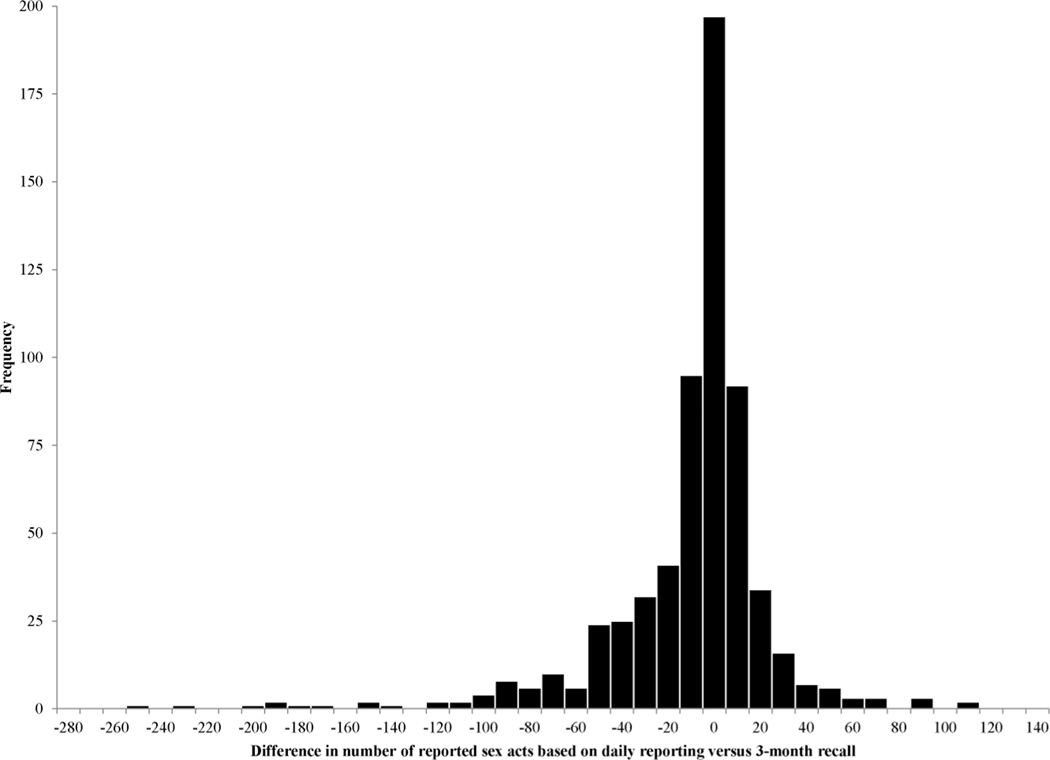
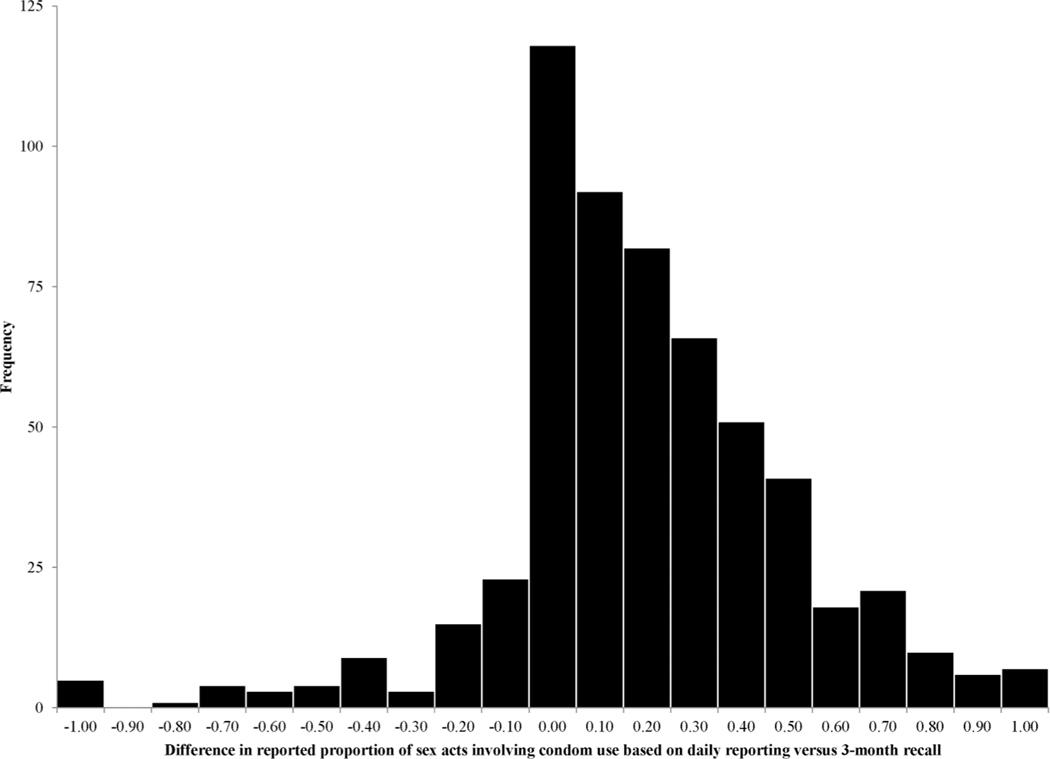
Daily versus recall differences in sex frequency (ie, number of penile–vaginal sex acts) and unprotected sex (ie, proportion of penile–vaginal sex acts in which a condom was not used from start to finish of sex) were used to assess concordance. The distributions of the raw differences were examined, with negative numbers indicating more frequent reporting via recall and positive numbers indicating more frequent reporting via daily report. In addition, correlation coefficients were calculated to compare daily and recall-based reporting of sex frequency and unprotected sex, respectively.
The variable representing difference in number of penile–vaginal sex acts had two modes, −1 and 0; therefore, a difference in the range of −1 to 1 was considered to indicate ‘consistent’ reporting of behaviour. For bivariate and multivariate modelling, the outcome variable was separated into three categories: (1) more sex acts reported in daily report than recall (ie, difference >1); (2) consistent number of sex acts reported in daily report as in recall (ie, −1≤ difference ≤1); and (3) more sex acts reported in recall than in daily report (ie, difference<−1).
On the variable representing difference in proportion of sex acts that were unprotected, nearly 13% of participants indicated the exact same proportion of unprotected sex in daily report as they did in recall; thus ‘consistent’ reporting of behaviour was defined as equal reporting in recall and daily report (ie, indicated by a value of 0 on the difference variable). For bivariate and multivariate modelling, the variable was separated into the following three nominal categories: (1) higher proportion of unprotected sex reported in daily than in recall (ie, difference >1); (2) equal proportion of unprotected sex reported in daily and recall (ie, difference=0); and (3) higher proportion of unprotected sex reported in recall than in daily (ie, difference <−1).
Covariates, selected a priori, were examined for their association with the outcome using a generalised logit model. Final multivariate models were derived using manual backward elimination. Analyses were performed using SAS V.9.4 (SAS Institute, Cary, North Carolina, USA) and SPSS V.22.0 (IBM, Armonk, New York, USA). A p value less than 0.05 denoted statistical significance.
RESULTS
The mean age was 30 years (SD=11.3; table 1), though males had a significantly higher mean age than females (p<0.001). The majority of the participants identified themselves as African American/black (61%). More than half had at least some college education or more (55%). The mean number of lifetime sexual partners was 28 (SD=36.3, median=15.0, IQR=28.0); males and those age 37 or older had significantly higher median number of sexual partners than their counterparts (p<0.001 for both). Nearly half of the participants self-reported a history of an STI (43%); females reported history of STI significantly more often than males (p=0.018). Twelve per cent of the cohort tested positive for chlamydia, gonorrhoea and/or trichomoniasis during participation in the study; females had significantly higher odds of testing positive than males (14.4% vs 8.0%; p=0.016).
Table 1.
Demographic, sexual behaviour and clinical characteristics of participants (n=628) and demographic characteristics of study interviewers
| Age group (years) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Overall N (%) | Female (n=364) N (%) | Male (n=264) N (%) | p Value | 15–21 (n=179) N (%) | 22–36 (n=283) N (%) | >37 (n=165) N (%) | p Value |
| Demographic factors | ||||||||
| Age—mean (SD) | 29.90 (11.27) | 28.49 (10.89) | 31.85 (11.52) | <0.001 | ||||
| Race* | ||||||||
| African American/black | 383 (60.99) | 215 (59.07) | 168 (63.64) | 0.049 | 94 (52.51) | 163 (57.60) | 126 (76.36) | <0.001 |
| Caucasian/white | 153 (24.36) | 85 (23.35) | 68 (25.76) | 42 (23.46) | 90 (31.80) | 21 (12.73) | ||
| Other/mixed | 92 (14.65) | 64 (17.58) | 28 (10.61) | 43 (24.02) | 30 (10.60) | 18 (10.91) | ||
| Hispanic | 54 (8.61) | 41 (11.29) | 13 (4.92) | 0.006 | 35 (19.55) | 15 (5.30) | 4 (2.42) | <0.001 |
| Income per month | ||||||||
| Less than $500 | 208 (39.92) | 118 (41.26) | 90 (38.30) | 0.050 | 73 (60.33) | 84 (31.94) | 51 (37.23) | <0.001 |
| Between $500 and $1000 | 154 (29.56) | 93 (32.52) | 61 (25.96) | 34 (28.10) | 73 (27.76) | 47 (34.31) | ||
| More than $1000 | 159 (30.52) | 75 (26.22) | 84 (35.74) | 14 (11.57) | 106 (40.30) | 39 (28.47) | ||
| Education | ||||||||
| Less than high school | 113 (18.02) | 76 (20.94) | 37 (14.02) | 0.061 | 51 (28.49) | 34 (12.01) | 28 (16.97) | <0.001 |
| High school graduate | 172 (27.43) | 92 (25.34) | 80 (30.30) | 47 (26.26) | 66 (23.32) | 59 (35.76) | ||
| Some college or more | 342 (54.55) | 195 (53.72) | 147 (55.68) | 81 (45.25) | 183 (64.66) | 78 (47.27) | ||
| Sexual behaviours | ||||||||
| Sexual partners, lifetime mean (SD) | 28.48 (36.34) | 22.52 (33.51) | 36.68 (38.49) | <0.001 | 10.31 (11.15) | 30.67 (37.60) | 44.42 (43.02) | <0.001 |
| Sexually transmitted infections | ||||||||
| History of STI† | 273 (43.47) | 173 (47.53) | 100 (37.88) | 0.018 | 57 (31.84) | 138 (48.76) | 78 (47.27) | <0.001 |
| Positive for STI‡, past 6 months | 73 (11.70) | 52 (14.36) | 21 (8.02) | 0.016 | 22 (12.43) | 35 (12.41) | 16 (9.76) | 0.661 |
Other includes: American Indian/Alaskan Native, Asian, mixed race and other race.
Herpes, genital warts, HPV, gonorrhoea, syphilis, chlamydia, trichomoniasis, hepatitis and/or other.
Positive for chlamydia, gonorrhoea and/or trichomoniasis as determined by laboratory results from samples taken at study visits 2 or 3.
HPV, human papillomavirus; STI, sexually transmitted infection.
Agreement between daily and recall reports of sex frequency was moderately strong (Spearman’s r (rs)=0.62; p<0.001), as well as the concordance for condom-unprotected penile–vaginal sex between the two reporting methods (rs=0.61; p<0.001) (see figures 1 and 2).
Figure 1.
Difference in number of reported sex acts based on daily reporting versus 3-month recall.
Figure 2.
Difference in reported proportion of sex acts involving condom use based on daily reporting versus 3-month recall.
The mean number of sexual events reported via recall was 38 (SD=42.7), while daily recall produced a mean of 24 sexual events (SD=27.9; p<0.001). According to daily report, the average proportion of sex acts that were unprotected was 0.31, which was significantly lower than that reported by recall (0.47, p<0.001).
Based on a generalised logit model, age, gender and number of lifetime sexual partners were each significantly associated with degree of consistency between the two reporting methods. More specifically, with every 5-year increase in age, subjects were 12% less likely (adjusted OR (AOR)=0.88; 95% CI (0.79 to 0.99)) to report higher sex frequency in recall as opposed to daily entries compared with equal reporting in the two methods. The odds of a female reporting higher frequency of sex in daily reports compared with recall were more than twice that of a male (higher frequency in daily reports than recall compared with equal frequency report in both methods: AOR=2.37, 95% CI (1.34 to 4.20); higher frequency in daily reports than recall compared with higher frequency in recall than daily reports: AOR=2.13, 95% CI (1.39 to 3.25)). Every five person increase in the number of reported lifetime sexual partners was associated with subjects being 6–7% more likely to have a discrepancy between the two reporting methods (higher sex frequency in daily reports compared with equal frequency reports: AOR=1.06, 95% CI (1.01 to 1.12); higher sex frequency in recall reports compared with equal frequency reports: AOR=1.07, 95% CI (1.01 to 1.13)) (see table 2).
Table 2.
Significant correlates of differential sex frequency reporting between daily and recall reports
| Covariate | Equal reporting in daily and recall | Higher report in daily* | Higher report in recall* | ||
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | AOR (95% CI) | Mean (SD) | AOR (95% CI) | |
| Age† | 30.01 (11.08) | 33.70 (11.96) | 1.11 (0.98 to 1.25) | 28.47 (10.74) | 0.88 (0.79 to 0.99) |
| Female—n (%) | 47 (12.91) | 100 (27.47) | 2.37 (1.34 to 4.20) | 217 (59.62) | 1.11 (0.69 to 1.81) |
| Male—n (%) | 40 (15.15) | 46 (17.42) | - | 178 (67.42) | - |
| Lifetime sexual partnerst | 20.57 (24.45) | 31.87 36.53() | 1.06 (1.01 to 1.12) | 28.97 (38.24) | 1.07 (1.01 to 1.13) |
Model with equal reporting as the reference group.
Adjusted OR and corresponding CI for 5 unit increase.
AOR: adjusted OR from generalised logit model.
Race, ethnicity, income, education, lifetime and current STI status and race/gender participant–interviewer match were not significantly associated with sex frequency reporting concordance between the two methods. A generalised logits model was fit with level of agreement between daily and recall reporting of condom-unprotected penile–vaginal sex as the outcome, but none of the tested covariates had significant association.
DISCUSSION
This study provides new insights regarding discrepancies between two modes of computer-based reporting of penile-vaginal events, both overall and condom unprotected, among a large sample of persons at elevated risk for STIs. Overall, there was a tendency toward greater reporting of events and condom-unprotected events via recall than daily report. This is consistent with findings reported from a review study published in 2014.8 Recall of sex frequency elicited a mean number of 38 events over 3 months, compared with 24 events over 3 months with daily report. Without a gold standard measure that is not reliant on self-report, the extent of over- and under-reporting cannot be determined and it cannot be known which data collection approach yielded estimates closer to the ‘truth’. Therefore, the focus of this analysis is on the discrepancy between the two methods rather than on either method’s accuracy. One plausible explanation for the discrepancy identified (ie, fewer sex events reported via daily reporting vs recall) could be diary completeness; that is, without 100% coverage of the days included in the 3-month recall surveys, the diary data would naturally indicate less frequent sex. Although diary incompleteness is frequently acknowledged as a limitation in estimates generated from daily reports, empirical data quantifying and examining correlates with the discrepancy between diary-based data collection and recall has been relatively limited. Additionally, demonstrating this discrepancy in a high-risk sample such as that used in the current study is certainly a strength. Of note, because the unprotected sex measure was based on a proportion rather than a count, diary incompleteness would not explain why daily report provided a significantly lower proportion (0.31) of unprotected sex acts than recall (0.47).
Beyond revealing that more events were documented by recall than via daily reports, the present study also identified circumstances under which such discrepancies were greater. Interestingly, in reporting unprotected sex acts, this tendency to over report with recall compared with daily was not significantly associated with age, gender, STI history and other covariates. However, in reporting sex acts in general, age, gender and number of lifetime partners were significant covariates. Although research has shown younger individuals may be more comfortable disclosing sexual behaviours and less inclined to under-report,15 we found they were more likely to have discrepant reports than older participants. Women were more than twice as likely as men to report a higher number of partners in daily compared with recall. This is not surprising given the sexual double standard that persists in US culture and prior research indicating that women may underreport sexual behaviours.6 Consistent with prior research,9–11,26 participants reporting more lifetime sexual partners exhibited greater discrepancy; most likely due to the decreased ability to accurately keep track of sexual events as occurrences increase. Daily reporting allows the capture of considerably more detail about individual events than is practicable via recall. This point is vital when event-level analyses are necessitated by research questions.
Interestingly, our findings indicate that individuals may think they are using condoms more often than they are. This finding has clinical implications since individuals may be underestimating their risk. Additionally, other demographic factors and race/gender participant–interviewer match were not significantly associated with sex frequency or condom-unprotected reporting concordance between the two methods. Of note, emphasis is often placed on gender/race matching in study design for sensitive behaviour elicitation,27 but our findings may indicate this emphasis is unwarranted. However, our participants were completing their reports on an electronic device and perhaps this indirect interaction contributed to a difference in effect.
These findings should be taken in the context of the limitations of the study. The data were collected several years ago when smartphones and data collection apps were not as widely available, hence the use of PDAs. Temporal trends in technology use could affect current generalisability of the findings; however, given the increased use of smartphones to collect behavioural data in sexual health research,8 the study remains highly relevant as methodological issues surrounding dairy-based reporting and recall will be critical to understand as technology evolves. Our field faces the absence of a practicable ‘gold standard’ for quantifying sexual behaviours. Precisely because there is no such gold standard, a study such as this is useful for understanding discrepancies between computer-based methods for reporting sexual behaviours. Although beyond the scope of the present study, additional research is needed to investigate whether and how reporting discrepancies relate to subsequent STI acquisition. Moreover, if such a relationship is discovered, then a practical question about how to use it will arise since STI clinic attenders do not ordinarily furnish daily reports. What is clear for now, however, is that sexual behaviour researchers should take steps to enhance compliance with data collection procedures. Additionally, shifting focus to methodological considerations of sexual behavioural research can help ensure better investment of resources into sex research.
Supplementary Material
Key messages.
There is a need for attention to be paid to methodological issues in sexual behavioural research.
Concordance between daily and 3-month recall of sexual behaviour is low to moderate.
Younger female participants and participants with more lifetime sexual partners are particularly likely to have discordant reports in daily versus recall of sexual behaviour.
Individuals may think they are using condoms more often than they are, indicating an underestimation of risk that should be considered in clinical practice.
Acknowledgments
Funding Data were from a project funded by NIH grant R01AI068119.
Footnotes
Handling editor Jackie A Cassell
Twitter Follow Kristen Mark at @Kristen_Mark
Competing interests None declared.
Patient consent Obtained.
Ethics approval University of Kentucky Institutional Review Board.
Provenance and peer review Not commissioned; externally peer reviewed.
Additional material is published online only. To view please visit the journal online (http://dx.doi.org/10.1136/sextrans-2016-052556).
REFERENCES
- 1.Crosby R, DiClemente RJ, Holtgrave DR, et al. Design, measurement, and analytical considerations for testing hypotheses relative to condom effectiveness against non-viral STIs. Sex Transm Infect 2002;78:228–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Graham CA, Crosby RA, Sanders SA, et al. Assessment of condom use in men and women. Ann Rev Sex Research 2005;16:20–52. [PubMed] [Google Scholar]
- 3.Fenton KA, Johnson AM, McManus S, et al. Measuring sexual behaviour: Methodological challenges in survey research. Sex Transm Infect 2001;77:84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brener ND, Billy JO, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behaviour among adolescents: evidence from the scientific literature. J Adoles Health 2003;33:436–57. [DOI] [PubMed] [Google Scholar]
- 5.McFarlane M, St Lawrence JS. Adolescents’ recall of sexual behaviour: Consistency of self-report and effect of variations in recall duration. J Adoles Health 1999;25:199–206. [DOI] [PubMed] [Google Scholar]
- 6.Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behaviour: II. Accuracy of self-reports. Annals of Behav Med 2003;26:104–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carey MP, Carey KB, Maisto SA, et al. Assessing sexual risk behaviour with the Timeline Followback (TLFB) approach: Continued development and psychometric evaluation with psychiatric outpatients. Int J STD & AIDS 2001;12:365–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stalgaitis C, Glick SX. The use of web-based diaries in sexual risk behavior research: a systematic review. Sex Tranms Infect 2014;90:374–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tourangeau R, Smith TW. Asking sensitive questions the impact of data collection mode, question format, and question context. Pub Opin Q 1996;60:275–304. [Google Scholar]
- 10.Downey L, Ryan R, Roffman R, et al. How could I forget? Inaccurate memories of sexually intimate moments. J Sex Res 1995;32:177–91. [Google Scholar]
- 11.Durant LE, Carey MP. Self-administered questionnaires versus face-to-face interviews in assessing sexual behaviour in young women. Arch Sex Behav 2000;29:309–22. [DOI] [PubMed] [Google Scholar]
- 12.Rose E, Diclemente RJ, Wingood GM, et al. The validity of teens’ and young adults’ self-reported condom use. Arch Ped Adoles Med 2009;163:61–4. [DOI] [PubMed] [Google Scholar]
- 13.Kissinger P, Rice J, Farley T, et al. Application of computer-assisted interviews to sexual behaviour research. Am J Epi 1999;149:950–4. [DOI] [PubMed] [Google Scholar]
- 14.Turner CF, Ku L, Rogers SM, et al. Adolescent sexual behaviour, drug use, and violence: increased reporting with computer survey technology. Science 1998;280:867–73. [DOI] [PubMed] [Google Scholar]
- 15.Newman JC, Des Jarlais DC, Turner CF, et al. The differential effects of face-to-face and computer interview modes. Am J Public Health 2002;92:294–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Catania JA, Gibson DR, Chitwood DD, et al. Methodological problems in AIDS behavioural research: Influences on measurement error and participation bias in studies of sexual behaviour. Psych Bulletin 1990;108:339–62. [DOI] [PubMed] [Google Scholar]
- 17.Catania JA, Binson D, Dolcini MM, et al. Risk factors for HIV and other sexually transmitted diseases and prevention practices among US heterosexual adults: Changes from 1990 to 1992. Am J Public Health 1995;85:1492–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garry M, Sharman SJ, Feldman J, et al. Examining memory for heterosexual college students’ sexual experiences using an electronic mail diary. Health Psyc 2002;21:629–34. [DOI] [PubMed] [Google Scholar]
- 19.Langhaug LF, Sherr L, Cowan FM. How to improve the validity of sexual behaviour reporting: systematic review of questionnaire delivery modes in developing countries. Trop Med Int Health 2010;15:362–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.James NJ, Bignell CJ, Gillies PA. The reliability of self-reported sexual behaviour. AIDS 1991;5:333–6. [DOI] [PubMed] [Google Scholar]
- 21.Zimmerman RS, Atwood KA, Cupp PK. Improving validity of self-reports for sensitive behaviours. In: Crosby RA, DiClemente RJ, Salazar LF, eds. Research methods in health promotion. CA: Jossey-Bass, 2006;269. [Google Scholar]
- 22.Allen CF, Lees SS, Desmond NA, et al. Validity of coital diaries in a feasibility study for the Microbicides Development Programme trial among women at high risk of HIV/AIDS in Mwanza, Tanzania. Sex Transm Infect 2007;83:490–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lees S, Cook C, Vallely A, et al. Comparison of sexual behaviour data collected using a coital diary and a clinic-based interview during a microbicide pilot study in Mwanza, Tanzania. Sex Transm Dis 2010;37:497–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Graham CA, Catania JA, Brand R, et al. Recalling sexual behaviour: a methodological analysis of memory recall bias via interview using the diary as the gold standard. J Sex Res 2003;40:325–32. [DOI] [PubMed] [Google Scholar]
- 25.Shrier LA, Shih MC, Beardslee WR. Affect and sexual behaviour in adolescents: a review of the literature and comparison of momentary sampling with diary and retrospective self-report methods of measurement. Pediatrics 2005;115:e573–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCallum EB, Peterson ZD. Investigating the impact of inquiry mode on self-reported sexual behaviour: Theoretical considerations and review of the literature. J Sex Res 2012;49:212–26. [DOI] [PubMed] [Google Scholar]
- 27.Crosby RA, Charnigo RA, Weathers C, et al. Condom effectiveness against non-viral sexually transmitted infections: a prospective study using electronic daily diaries. Sex Transm Inf 2012;88:484–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.