Abstract
Background:
Atrial Fibrillation (AF) has been associated with various behavioral risk factors such as tobacco, alcohol, and/or substances abuse.
Objective:
The main objective is to describe the national trends and burden of tobacco and substance abuse in AF hospitalizations. Also, this study identifies potential population who are more vulnerable to these substance abuse among AF hospitalizations.
Methods:
The National Inpatient Sample database from 2007 to 2015 was utilized and the hospitalizations with AF were identified using the international classification of disease, Ninth Revision, Clinical Modification code. They were stratified into without abuse, tobacco use disorder (TUD), substance use disorder (SUD), alcohol use disorder (AUD) and drug use disorder (DUD).
Results:
Of 3,631,507 AF hospitalizations, 852,110 (23.46%) had TUD, 1,851,170 (5.1%) had SUD, 155,681 (4.29%) had AUD and 42,667 (1.17%) had DUD. The prevalence of TUD, SUD, AUD, and DUD was substantially increased across all age groups, races, and gender during the study period. Female sex was associated with lower odds TUD, SUD, AUD, and DUD. Among AF hospitalizations, the black race was associated with higher odds of SUD, and DUD. The younger age group (18–35 years), male, Medicare/Medicaid as primary insurance, and lower socioeconomic status were associated with increased risk of both TUD and SUDs.
Conclusion:
TUD and SUD among AF hospitalizations in the United States mainly affects males, younger individuals, white more than black, and those of lower socioeconomic status which demands for the development of preventive strategies to address multilevel influences.
Keywords: Atrial fibrillation, Tobacco abuse, Substance abuse, Trends, Drug abuse
Introduction
Atrial fibrillation (AF) is one of the most common arrhythmias in the U.S. and the prevalence of AF continue to rise secondary to the increased detection rate and population aging.1, 2 AF is predominantly associated with hypertension, heart failure, coronary artery disease, diabetes mellitus, and valvular heart disease.3 AF has also been associated with various behavioral risk factors such as tobacco abuse,4 alcohol abuse5, 6 and substances abuse.6 Tobacco abuse has been shown to increase the risk of AF in the Framingham Heart Study (FHS) and Rotterdam study.7, 8 Alcohol has been strongly associated with the risk of AF and reducing intake was shown to be associated with reduction in AF recurrences.9, 10 Similarly, various substances such as cocaine, amphetamine and other illicit drugs have been shown to have cardiotoxic effects resulting in cardiac arrhythmias.11, 12 Furthermore, rates of tobacco, alcohol and illegal drug use in the U.S. continue to increase, especially in the young adults, which may add to the incidence and prevalence of AF.13–15 Prior studies on substance use and AF in the U.S. are not nationally representative. National tobacco abuse and substance abuse rates among heart failure hospitalizations have been studied.16 The national burden of tobacco and other substance use disorders among AF hospitalizations is not well described.
Nationally representative data helps to understand the prevalence and influence of tobacco and substance use disorders on health outcomes among AF hospitalizations. Identifying AF hospitalizations with tobacco, alcohol or other substance use disorders is critical in developing preventive policies. This study describes the national burden and trend of tobacco and substance abuse in AF hospitalizations. Also, this study identifies potential population who are more vulnerable to these substance abuse among AF hospitalizations. Moreover, we stratified these trends by age, race, and sex to observe predominant group characteristics in AF hospitalizations.
Methods
Data source
The National Inpatient Sample (NIS) was used for the present analysis. The NIS is created and maintained by the Agency for Healthcare Research and Quality and is developed for the Healthcare Cost and Utilization Project (HCUP). The NIS contains data from more than 7 million unweighted hospital discharges each year and weighted, and the NIS estimates more than 35 million hospitalizations nationally. The design of the NIS was changed after the year 2012. The NIS included all inpatient discharges from a random 20% sample of hospitalizations from 2007 to 2011. From 2012 onwards, the database was built using a systematic sampling of 20% of discharges from all the hospitals. Additionally, we used “trend weights” for the database prior to the year 2011, as recommended. These trend weights help facilitate comparison of estimates from the year prior to 2012. These changes in the NIS database structure has been described previously.17, 18 Since, the NIS uses de-identified hospital discharges as samples with prior ethical committee approval, no additional ethical committee approval was required for the present analysis.
Study population
AF hospitalizations were identified using the international classification of disease, Ninth Revision, Clinical Modification (ICD-9-CM) code 427.31 in the primary diagnosis column. We included the database from January 2007 to September 2015 since the coding system changed to ICD-10-CM after September 2015. These codes for identifying AF hospitalizations from the NIS have been utilized in previous studies.19–21 Hospitalizations under 18 years of age were excluded from the present analysis. Demographic data including age, sex, race, co-morbidities, region of hospital, location of the hospital, hospital size, payment type and median household income category for hospitalization’s zip code were retrieved for each of the included hospitalizations. Tobacco, alcohol and drug use disorders were defined using ICD-9-CM codes (Supplementary Table 1), as described previously.16 Substance use disorder (SUD) was defined as any drug or alcohol use disorder excluding tobacco. This method has been utilized previously for heart failure hospitalization using the same database.16 Finally, Charlson’s comorbidity index score has been explained in the Supplementary Table 2. This was later stratified by 0, 1, 2 or ≥3.
Statistical analysis
AF hospitalizations were stratified into without abuse, tobacco use disorder (TUD), SUD, alcohol use disorder (AUD) and drug use disorder (DUD). Descriptive statistics of hospitalizations in each stratum with in-hospital outcomes were reported. AF hospitalizations were later stratified based on sex. All analyses in the present study accounted for NIS clustering, survey nature, stratification, and weights per recommendations (Supplementary Table 3).22 Continuous variables were expressed as mean (standard deviations [SD]) or median (interquartile range [IQR]) depending on the data distribution and analyzed using the Student t-test or Wilcoxon rank sum test, as appropriate. Categorical data were expressed in frequency and percentages and analyzed using the Pearson’s chi-square test. We used the Jonckheere-Terpstra trend test to analyze the trend of the frequency of substance use percentage combined, stratified into five age groups (18–35, 36–50, 51–65, 66- 80 and more than 80), sex and race. Statistical significance was set at a P-value of <0.05. The cost was calculated by multiplying the total cost with the cost-to-charge ratio provided by the sponsor for each given year and adjusted for inflation to year 2011. Finally, we performed multivariable logistic regression analysis to analyze demographic factors associated with TUD, SUD, AUD and DUD. We included age, sex, race, hospital region, median household income, primary payor, hospital bedsize and hospital location in this model. SAS, version 9.4 (SAS Institute Inc.) was used for all statistical analyses.
Results
A total of 3,631,507 AF hospitalizations from 2007 - 2015 over 18 years of age were included in the present analysis. Of the hospitalizations, 852,110 (23.46%) had TUD, 1,851,170 (5.1%) had SUD, 155,681 (4.29%) had AUD and 42,667 (1.17%) had DUD. 2,689,315 (74.06%) had no documented history of any abuse.
Atrial fibrillation hospitalization without a history of abuse
Hospitalizations without a history of abuse had a mean age of 71.8 ± 30.1 years. Majority of the hospitalizations without drug abuse were between 66 and 80 years (38.7%), females (57.4%) and whites (72.6%). Hypertension (67.6%) and dyslipidemia (43.3%) were the most frequently occurring co-morbidities. Most of the AF hospitalizations without a history of drug abuse had CHA2DS2VASc score ≥3 (62%) (CHA2DS2VASc scores are used in AF patients to stratify the risk of stroke). The majority of the hospitalizations were at large hospitals by bed-size (60.1%) and urban teaching locations (44.3%) with Medicare/Medicaid (72.5%) being the most common primary payment type among AF hospitalizations with drug abuse (Table 1).
Table 1.
Demographics, baseline characteristics and in-hospital outcomes of patients admitted with atrial fibrillation and substance abuse.
| Variable | Without Abuse (2,689,315) | TUD (852,110) | SUD (185,170) | AUD (155,681) | DUD (42,667) |
|---|---|---|---|---|---|
| Age, years (Mean±SD) | 71.8 ± 30.1 | 67±29.5 | 58.4 ± 29.9 | 58.7 ± 28.4 | 55±34.2 |
| 18–35 | 36,563 (1.4) | 18,501 (2.2) | 11,213 (6.1) | 7717 (5) | 5194 (12.17) |
| 36–50 | 145,669 (5.4) | 655,012 (7.7) | 30,297 (16.4) | 24,838 (16) | 8833 (20.7) |
| 51–65 | 558,193 (20.8) | 256,048 (30.1) | 84,068 (45.4) | 72,562 (46.7) | 18,261 (42.8) |
| 66–80 | 1,040,383 (38.7) | 353,048 (41.4) | 48,255 (26.1) | 42,391 (27.2) | 7121 (16.7) |
| >80 | 908,560 (33.8) | 159,011 (18.7) | 11,338 (6.1) | 8172 (5.3) | 3258 (7.6) |
| Sex | |||||
| Male | 1,146,283 (42.6) | 519,812 (61) | 152,287 (82.2) | 132,378 (85) | 31,569 (74) |
| Female | 1,543,032 (57.4) | 332,290 (39) | 32,880 (17.8) | 23,299 (15) | 11,098 (26) |
| Race | |||||
| White | 1,952,137 (72.6) | 653,703 (76.7) | 129,093 (70) | 110,263 (70.8) | 27,259 (63.9) |
| Black | 168,472 (6.3) | 58,933 (6.9) | 19,759 (10/7) | 14,708 (9.5) | 7200 (16.9) |
| Other | 568,498 (21.1) | 139,428 (16.36) | 36,319 (20) | 30,710 (19.7) | 8208 (19.2) |
| Comorbidities | |||||
| Hypertension | 1,817,966 (67.6) | 582,136 (68.32) | 112,540 (60.8) | 95,368 (61.3) | 24,327 (57) |
| Diabetes Mellitus | 675,975 (25.1) | 209,941 (24.64) | 30,737 (16.6) | 24,325 (15.6) | 8106 (19) |
| Chronic Lung Disease | 465,053 (17.3) | 314,874 (40) | 49,966 (30) | 41,160 (26.4) | 12,284 (28.8) |
| Congestive Heart Failure | 10,335 (0.38) | 2422 (0.28) | 727 (0.4) | 565 (0.4) | 192 (0.45) |
| Dyslipidemia | 1,164,022 (43.3) | 409,553 (48) | 55,868 (30.2) | 46,912 (30.1) | 11,811 (27.7) |
| Chronic Kidney Disease | 355,061 (13.2) | 102,391 (12) | 13,632 (7.4) | 9965 (6.4) | 4351 (10.2) |
| Chronic Liver Disease | 27,935 (1) | 20,258 (2.38) | 19,619 (10.6) | 18,184 (11.7) | 3387 (7.9) |
| Cancer with or without metastasis | 103,601 (3.9) | 46,776 (5.5) | 4586 (2.5) | 3578 (2.3) | 1195 (2.8) |
| Obesity | 355,338 (13.2) | 143,394 (16.8) | 27,414 (14.8) | 22,128 (14.2) | 7153.2 (16.8) |
| Thyroid Dysfunction | 495,453 (18.4) | 121,424 (14.25) | 14,882 (8) | 11,480 (7.4) | 4149 (9.72) |
| Obstructive sleep apnea | 195,427 (7.3) | 84,731.2 (9.9) | 14,430 (7.8) | 11,565 (7.4) | 3673 (8.6) |
| Electrical cardioversion | 386,458 (14.4) | 132,616 (15.6) | 22,537 (12.2) | 19,051 (12.2) | 4837 (11.3) |
| CHA2DS2VASc Score | |||||
| 0 | 168,234 (6.3) | 80,497 (9.5) | 41,160 (22.2) | 34,745 (22.3) | 10,941 (25.6) |
| 1 | 354,086 (13.2) | 160,896 (18.9) | 62,612 (33.8) | 54,124 (34.8) | 13,722 (32.16) |
| 2 | 499,746 (18.6) | 198,084 (23.3) | 42,936 (23.2) | 36,650 (23.5) | 8705 (20) |
| >=3 | 1,667,302 (62) | 412,633 (48.4) | 38,463 (20.8) | 30,161 (19.4) | 9299 (21.8) |
| Charlson’s Comorbidity Index | |||||
| 0 | 998,579 (37.1) | 239,955 (26.2) | 70,618 (38.1) | 60,977 (39.2) | 15,332 (36) |
| 1 | 755,457 (28.1) | 248,203 (29.1) | 55,835 (30.2) | 47,664.3 (30.6) | 12,117 (28.4) |
| 2 | 436,110 (16.2) | 167,244 (19.6) | 30,350 (16.4) | 24,944.3 (16.0) | 7315 (17.1) |
| >=3 | 499,221 (18.6) | 196,707 (23.1) | 28,368 (15.3) | 22,096 (14.2) | 7903 (18.5) |
| Hospital-level Characteristics | |||||
| Region of the Hospital | |||||
| Northeast | 588,634 (21.9) | 157,460 (18.5) | 40,140 (21.7) | 34,797 (22.3) | 8036 (18.8) |
| Midwest | 661,976 (24.6) | 230,076 (27) | 40,074 (21.6) | 34,048 (21.9) | 8734 (20.4) |
| South | 1,045,666 (38.9) | 328,662 (38.6) | 67,163 (36.3) | 56,466 (36.2) | 15,208 (35.6) |
| West | 392,903 (14.6) | 135,787 (15.9) | 37,773 (20.4) | 30,350 (20) | 10,690 (25) |
| Hospital Bed Size | |||||
| Small | 398,144 (14.9) | 117,024 (13.8) | 26,754 (14.5) | 22,727 (14.7) | 5933 (14) |
| Medium | 668,824 (25) | 220,502 (26) | 49,723 (27) | 42,011 (27.1) | 11,278 (26.6) |
| Large | 1,607,656 (60.1) | 510,336 (60.1) | 107,666 (58.5) | 90,071 (58.2) | 25,263 (59.5) |
| Location of the Hospital | |||||
| Rural | 389,364 (14.6) | 106,388 (12.6) | 20,677 (11.2) | 17,624 (11.4) | 4346 (10.2) |
| Urban, Nonteaching | 1,100,741 (41.2) | 339,788 (40.1) | 75,276 (40.9) | 63,937 (41.3) | 16,231 (38.2) |
| Urban, Teaching | 1,184,520 (44.3) | 401,685 (47.4) | 88,190 (47.9) | 73,247 (47.31) | 21,895 (51.6) |
| Median household income category for patient’s zip code | |||||
| 1. 0–25th percentile | 669,952 (25.4) | 228,195 (27.3) | 54,488 (30.5) | 44,264 (29.4) | 14,866 (36.1) |
| 2. 26–50th percentile | 709,693 (27) | 224,826 (27) | 45,751 (25.6) | 38,426 (25.5) | 10,650 (25.9) |
| 3. 51–75th percentile | 651,437 (25) | 207,050 (24.9) | 42,771 (23.9) | 36,452 (24.2) | 9168 (22.3) |
| 4. 76–100th percentile | 604,831 (23) | 175,363 (22) | 35,913 (20.1) | 31,320 (20.8) | 6452 (15.7) |
| Payment Type | |||||
| Medicare/Medicaid | 1,947,167 (72.5) | 567,002 (66.7) | 98,681 (53.4) | 80,383 (51.8) | 24,598 (57.8) |
| Private insurance | 630,849 (23.5) | 215,899 (25.4) | 52,650 (28.5) | 46,832 (30.2) | 8830 (20.8) |
| Self pay/no charge/others | 107,154 (4) | 67,743 (8) | 33,317 (18) | 28,005 (18) | 9131 (21.5) |
| In-hospital Outcomes | |||||
| Stroke | 35,355 (1.3) | 8924 (1.1) | 1762 (1) | 1472 (1) | 374 (0.9) |
| In-hospital Mortality | 26,753 (1) | 5953 (0.7) | 1530 (0.8) | 1166 (0.75) | 438 (1.0) |
| Discharge to Home | 1,971,907 (73.4) | 668,381 (78.5) | 142,544 (77) | 121,483 (78.1) | 31,368 (73.6) |
| Length of Stay (Median, IQR) | 3 (1–4) | 3 (1–4) | 3 (2–5) | 3 (2–5) | 3 (1–5) |
| Cost, $$ (Median, IQR) | 5409 (3366–9363) | 5637 (3551–9532) | 6037 (3855–9920) | 6008 (3848–9790) | 6083 (3871–10,226) |
SD-Standard Deviation; IQR: Interquartile range; TUD-tobacco use disorder; SUD-substance use disorders; AUD-alcohol use disorders, DUD-drug use disorders.
Tobacco use disorder in AF hospitalizations
AF hospitalizations with TUD had a mean age of 67±29.5 years. The majority of the hospitalizations in TUD were between 51 and 65 years of age (41.4%), male (61%), and white (76.7%). Most of the AF hospitalizations with TUD had CHA2DS2VASc score ≥ 3 (48.4%). Like AF hospitalizations without drug abuse, AF hospitalizations with TUD were predominantly admitted to a large bed-sized hospital (60.1%), urban teaching hospitals (47.4%) with Medicare/Medicaid being the primary payor in AF hospitalizations with TUD (66.7%). Among AF hospitalizations, 1.1% had a stroke, 0.7% died in hospital, and 78.5% were discharged to home (Table 1). TUD was most common in age groups >50 years, the majority were whites, and Medicare/Medicaid was the primary payor for AF hospitalizations with TUD in both sexes (Table 2).
Table 2.
Atrial fibrillation patient characteristics by substance abuse disorders stratified by sex.
| MALE | |||||
|---|---|---|---|---|---|
| Variable | TUD (519,812) | SUD (152,287) | AUD (132,378) | DUD (31,486) | |
| 18–35 | 15,617 (3) | 10,136 (6.7) | 7118 (5.3) | 4601 (14.6) | |
| 36–50 | 51,076 (9.8) | 26,902 (17.7) | 22,563 (170 | 7295 (23.1) | |
| 51–65 | 179,858 (34.6) | 73,038 (48) | 64,416 (48.7) | 14,687 (46.5) | |
| 66–80 | 200,661 (38.6) | 36,078 (23.7) | 33,038 (24.9) | 4032 (12.8) | |
| >80 | 72,601 (13.8) | 6132 (4) | 5241 (4) | 953 (3) | |
| Race | |||||
| White | 393,822 (75.8) | 105,250 (69.1) | 93,178 (70.4) | 19,597 (62) | |
| Black | 35,107 (6.8) | 15,916 (10.5) | 12,152 (9.2) | 5561 (17.6) | |
| Other | 90,870 (17.5) | 31,121 (20.4) | 27,049 (20.4) | 6410 (20.3) | |
| Hospital-level Characteristics | |||||
| Region of the Hospital | |||||
| Northeast | 95,692 (18.4) | 33,139 (21.8) | 29,390 (22.2) | 6104 (19.3) | |
| Midwest | 139,362 (26.8) | 33,261 (21.8) | 29,170 (22) | 6504 (20.6) | |
| South | 202,783 (39) | 55,542 (36.5) | 48,474 (36.6) | 11,056 (35) | |
| West | 81,910 (15.8) | 30,324 (20) | 25,324 (19.1) | 7903 (25) | |
| Hospital Bed Size | |||||
| Small | 69,796 (13.5) | 22,019 (14.5) | 19,286 (14.7) | 4422 (14) | |
| Medium | 132,635 (25.7) | 40,772 (26.9) | 35,641 (27.1) | 8344 (26.5) | |
| Large | 314,700 (60.9) | 88,646 (58.5) | 76,692 (58.3) | 18,679 (59.4) | |
| Location of the Hospital | |||||
| Rural | 64,939 (12.6) | 16,848 (11.1) | 14,946 (11.4) | 3053 (9.7) | |
| Urban, Nonteaching | 204,953 (39.6) | 61,447 (40.6) | 54,055 (41.1) | 11,726 (37.3) | |
| Urban, Teaching | 247,239 (47.8) | 73,142 (48.3) | 62,618 (47.6) | 16,666 (53) | |
| Median household income category for patient’s zip code | |||||
| 1. 0–25th percentile | 138,746 (27.3) | 45,111 (30.7) | 38,041 (29.8) | 11,155 (36.8) | |
| 2. 26–50th percentile | 137,480 (27.1) | 37,570 (25.6) | 32,768 (25.7) | 7726 (25.5) | |
| 3. 51–75th percentile | 125,988 (24.8) | 35,178 (24) | 30,968 (24.2) | 6721 (22.1) | |
| 4. 76–100th percentile | 106,077 (20.9) | 28,932 (20) | 25,859 (20.3) | 4740 (15.6) | |
| Payment Type | |||||
| Medicare/Medicaid | 312,469 (60.2) | 75,498 (49.7) | 64,836 (49.13) | 16,070 (51) | |
| Private insurance | 154,280 (29.7) | 46,218 (30.4) | 41,520 (31.5) | 7458 (23.7) | |
| Self-pay/no charge/others | 52,010 (10) | 30,107 (19.8) | 25,600 (19.4) | 7957 (25.3) | |
| FEMALE | |||||
| Variable | TUD (332,290) | SUD (32,880) | AUD (23,299) | DUD (11,074) | |
| 18–35 | 2884 (0.9) | 1077 (3.3) | 599 (2.6) | 593 (5.4) | |
| 36–50 | 14,426 (4.3) | 3395 (10.3) | 2275 (9.8) | 1539 (13.9) | |
| 51–65 | 76,190 (23) | 11,025 (33.5) | 8142 (35) | 3573 (32.2) | |
| 66–80 | 152,383 (45.9) | 12,177 (37) | 9353 (40.1) | 3088 (27.8) | |
| >80 | 86,406 (26) | 5205 (15.8) | 2931 (12.6) | 2304 (20.8) | |
| Race | |||||
| White | 259,881 (78.2) | 23,843 (72.5) | 17,085 (73.3) | 7661 (69) | |
| Black | 23,828 (7.2) | 3843 (11.7) | 2556 (11) | 1639 (14.8) | |
| Other | 48,550 (14.6) | 5194 (15.80 | 3657 (15.7) | 1797 (16.2) | |
| Hospital-level Characteristics | |||||
| Region of the Hospital | |||||
| Northeast | 61,768 (18.6) | 7001 (21.3) | 5408 (23.2) | 1931 (17.4) | |
| Midwest | 90,706 (27.3) | 6808 (20.7) | 4874 (21) | 2229 (20.1) | |
| South | 125,879 (37.9) | 11,621 (35.3) | 7991 (34.3) | 4152 (37.4) | |
| West | 53,877 (16.2) | 7449 (22.3) | 5026 (21.6) | 2786 (25.1) | |
| Hospital Bed Size | |||||
| Small | 47,219 (14.30) | 4731 (14.5) | 3437 (14.8) | 1511 (13.7) | |
| Medium | 87,867 (26.6) | 8951 (27.4) | 6370 (27.5) | 2934 (26.6) | |
| Large | 195,635 (59.2) | 19,020 (58.2) | 13,379 (57.7) | 6584 (59.7) | |
| Location of the Hospital | |||||
| Rural | 41,449 (12.5) | 3829 (11.7) | 2678 (11.6) | 1293 (11.7) | |
| Urban, Nonteaching | 134,827 (40.8) | 13,825 (42.3) | 9878 (42.6) | 4506 (40.8) | |
| Urban, Teaching | 154,446 (46.7) | 15,048 (46) | 10,629 (45.8) | 5229 (47.4) | |
| Median household income category for patient’s zip code | |||||
| 1. 0–25th percentile | 89,445 (27.3) | 9377 (29.2) | 6223 (27.2) | 3711 (34.4) | |
| 2. 26–50th percentile | 87,342 (26.7) | 8177 (25.5) | 5653 (24.8) | 2923 (27.1) | |
| 3. 51–75th percentile | 81,062 (24.8) | 7593 (23.6) | 5484 (24) | 2446 (22.7) | |
| 4. 76–100th percentile | 69,285 (21.2) | 6980 (21.7) | 5460 (24) | 1712 (15.9) | |
| Payment Type | |||||
| Medicare/Medicaid | 254,525 (76.7) | 23,179 (70.6) | 15,544 (66.8) | 8528 (77) | |
| Private insurance | 61,620 (18.6) | 6432 (19.6) | 5311 (22.8) | 1372 (12.4) | |
| Self-pay/no charge/others | 15,733 (4.7) | 3210 (9.8) | 2404 (10.3) | 1174 (10.6) | |
Substance use disorder in AF hospitalizations
AF hospitalizations with SUD had a mean age of 58.4 ± 29.9 years, with the majority in the age group of 51–65 (45.4%). Majority of the hospitalizations were male (82.2%) and whites (70%), at a large bed-sized hospital (58.5%) and urban teaching hospitals (47.9%) with Medicare/Medicaid being the primary payor. Among AF hospitalization with SUD, 1% had a stroke, 0.8% died in hospital, and 77% were discharged to home. (Table 1) Among males, the most common age group was 51–65 years, while it was 66–80 years in females, with whites being majority among both sexes. (Table 2)
Alcohol use disorder in AF hospitalizations
AF hospitalizations with AUD had a mean age of 58.7 ± 28.4 years, with the majority in the age group of 51–65 years (46.7%). The majority of the hospitalizations were male (85%), whites (70.8%), at a large bed-sized hospital (58.2%), urban teaching settings (47.31%) with Medicare/Medicaid being a significant payor for AF hospitalizations with AUD. Among AF hospitalizations with AUD, 1% had a stroke, 0.75% died in the hospital, and 78.1% were discharged to home (Table 1). Among males, the most common age group was 50–65 years, while it was 66–80 years in females. (Table 2)
Drug use disorder in AF hospitalizations
AF hospitalizations with DUD had a mean age of 55±34.2 years, and the majority were in the age group of 51–65 (42.8%). The majority of the hospitalizations were male (74%), whites (63.9%), at a large bed-sized hospital (59.5%), urban teaching settings (51.6%) with Medicare/Medicaid (57.8%) being the primary payor. Hypertension (57%) and chronic lung disease (28.8%) were the most prevalent comorbidities. Among AF hospitalization with DUD, 0.9% had a stroke, 1% died in the hospital, and 73.6% were discharged to home (Table 1). DUD among AF hospitalizations was most common in the 51–65 years age group in both sexes (Table 2).
Associated demographic factors
Among AF hospitalizations, compared to the age group of 18–35 years, all the other age groups had lower odds of TUD, SUD, AUD, and DUD. The exception to this was the age group of 51–65 years, which had an increased odds of TUD as compared with the age group 18–35 years (1.05 (1.03–1.07), P-value <0.001). Female sex was associated with lower odds of TUD (0.57 (0.56–0.57), P-value <0.001), SUD (0.27 (0.26–0.27), P-value <0.001), AUD (0.22 (0.22–0.22), P-value <0.001), and DUD (0.51 (0.5–0.52), P-value <0.001). Among AF hospitalizations, the black race was associated with higher odds of SUD (1.12 (1.1–1.14), P-value <0.001), and DUD (1.42 (1.38–1.47), P-value <0.001). Midwest (1.45 (1.44–1.46), P-value <0.001), south (1.16 (1.15–1.17), P-value <0.001) and west (1.34 (1.33–1.35), P-value <0.001) hospital regions had a higher odds of TUD as compared with northeast region. The hospitalizations in the lower percentile median household income category had higher odds of TUD and SUDs. Private insured patients had the lowest odds of TUD, and SUDs and self-pay/no charge patients had the highest odds of TUD and SUDs (Table 3).
Table 3.
Demographic factors associated with Tobacco or Substance use disorders Among Hospitalized Atrial Fibrillation Patients.
| TUD | SUD | AUD | DUD | |
|---|---|---|---|---|
| Variable | ||||
| Age groups | ||||
| 18–35 | Reference | Reference | Reference | Reference |
| 36–50 | 0.96 (0.94–0.98)# | 0.74 (0.72–0.75) # | 0.93 (0.9–0.95) # | 0.46 (0.44–0.48) # |
| 51–65 | 1.05 (1.03–1.07) # | 0.59 (0.57–0.6) # | 0.8 (0.78–0.82) # | 0.27 (0.26–0.28) # |
| 66–80 | 0.76 (0.75–0.78) # | 0.17 (0.16–0.17) # | 0.25 (0.25–0.26) # | 0.04 (0.04–0.05) # |
| >80 | 0.42 (0.42–0.44) # | 0.06 (0.06–0.06) # | 0.08 (0.07–0.08) # | 0.03 (0.01–0.01) # |
| Female vs. Male | 0.57 (0.56–0.57) # | 0.27 (0.26–0.27) # | 0.22 (0.22–0.22) # | 0.51 (0.5–0.52) # |
| Black vs. White | 0.85 (0.84–0.86) # | 1.12 (1.1–1.14) # | 1 (0.99–1.02)$ | 1.42 (1.38–1.47) # |
| Region of the Hospital | ||||
| Northeast | Reference | Reference | Reference | Reference |
| Midwest | 1.45 (1.44–1.46) # | 0.88 (0.87–0.9) # | 0.86 (0.84–0.87) # | 1.01 (0.98–1.04)£ |
| South | 1.16 (1.15–1.17) # | 0.83 (0.82–0.85) # | 0.81 (0.8–0.83) # | 0.93 (0.9–0.96) # |
| West | 1.34 (1.33–1.35) # | 1.36 (1.34–1.38) # | 1.22 (1.2–1.23) # | 2.05 (1.99–2.1) # |
| Median household income category for patient’s zip code | ||||
| 1. 0–25th percentile | Reference | Reference | Reference | Reference |
| 2. 26–50th percentile | 0.93 (0.92–0.93) # | 0.85 (0.84–0.86) # | 0.87 (0.85–0.88) # | 0.8 (0.78–0.83) # |
| 3.51 –75th percentile | 0.91 (0.91–0.92) # | 0.85 (0.83–0.86) # | 0.87 (0.86–0.89) # | 0.75 (0.73–0.77) # |
| 4. 76–100th percentile | 0.84 (0.83–0.85) # | 0.78 (0.77–0.79) # | 0.82 (0.8–0.83) # | 0.63 (0.61–0.65)# |
| Payment Type | ||||
| Medicare/Medicaid | Reference | Reference | Reference | Reference |
| Private insurance | 0.71 (0.71–0.71) # | 0.45 (0.45–0.46) # | 0.52 (0.51–0.52) # | 0.27 (0.26–0.27) # |
| Self-pay/no charge/others | 1.2 (1.19–1.2) # | 1.36 (1.34–1.38) # | 1.46 (1.43–1.48) # | 1.03 (1.01–1.06) # |
| Hospital Bed Size | ||||
| Small | Reference | Reference | Reference | Reference |
| Medium | 1.08 (1.07–1.09) # | 0.99 (0.97–1) β | 0.99 (0.97–1)& | 0.99 (0.96–1.02) ¥ |
| Large | 1.02 (1.02–1.04) # | 0.85 (0.84–0.86) # | 0.84 (0.83–0.85) # | 0.89 (0.87–0.92) # |
| Location of the Hospital | ||||
| Rural | Reference | Reference | Reference | Reference |
| Urban, Nonteaching | 1.15 (1.14–1.16) # | 1.19 (1.17–1.21) # | 1.17 (1.15–1.2) # | 1.22 (1.18–1.27) # |
| Urban, Teaching | 1.25 (1.24–1.26) # | 1.15 (1.13–1.17) # | 1.09 (1.08–1.12) # | 1.39 (1.34–1.44) # |
P <0.001.
P = 0.124.
P = 0.034.
P = 0.1.
P = 0.521.
P = 0.078.
The trend of tobacco, substance, alcohol and drug use disorder from 2007 to 2015 among AF hospitalizations
There was a significant increase in trend of AF hospitalizations with TUD, SUD, AUD, and DUD from 2007 to 2015 combined, stratified gender, and race (Fig. 1, Fig. 2). TUD has the highest prevalence of hospital admissions as shown in the Fig. 1. DUD has the lowest prevalence of hospital admission for Afib as explained in the Fig. 1. In males (Fig. 2A) and in females (Fig. 2B), TUD had highest prevalence throughout the study period. The prevalence of TUD consistently increases during the study period in males and as well in females. Similarly, TUD had the highest prevalence in whites as well as African Americans (Fig. 2C and 2D). Further, TUD, SUD, AUD and DUD increased significantly in all age groups; 18–35 years, 36–50 years, 51–65 years, 66–80 years and >80 years (Fig. 3). Prevalence of TUD was highest in the younger population (below 35 years of age) as shown in Fig. 3A. Additionally, prevalence of SUD, AUD and DUD is also highest compared to other population (Fig. 3 panel B-D).
Fig. 1.
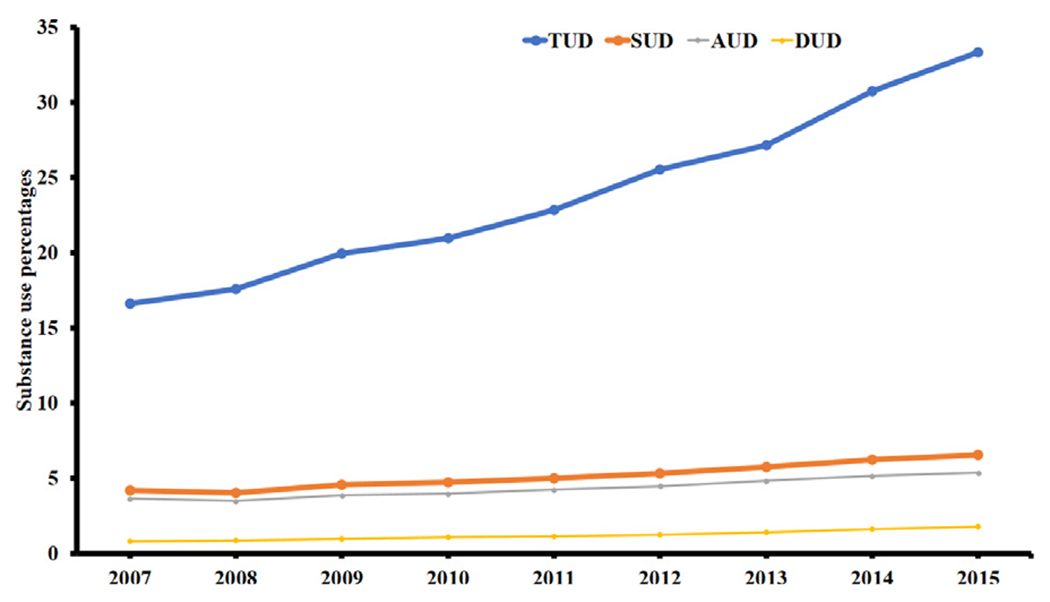
Temporal trend of TUD, SUD, AUD and DUD.
Panel A represent overall hospitalizations included in the study. X-axis represents timeline in years, and Y-axis represents frequency of substance use disorder in percentages.
Abbreviations: TUD: Tobacco Use Disorder; SUD: Substance Use Disorder; AUD: Alcohol Use Disorder; and DUD: Drug Use Disorder.
Fig. 2.
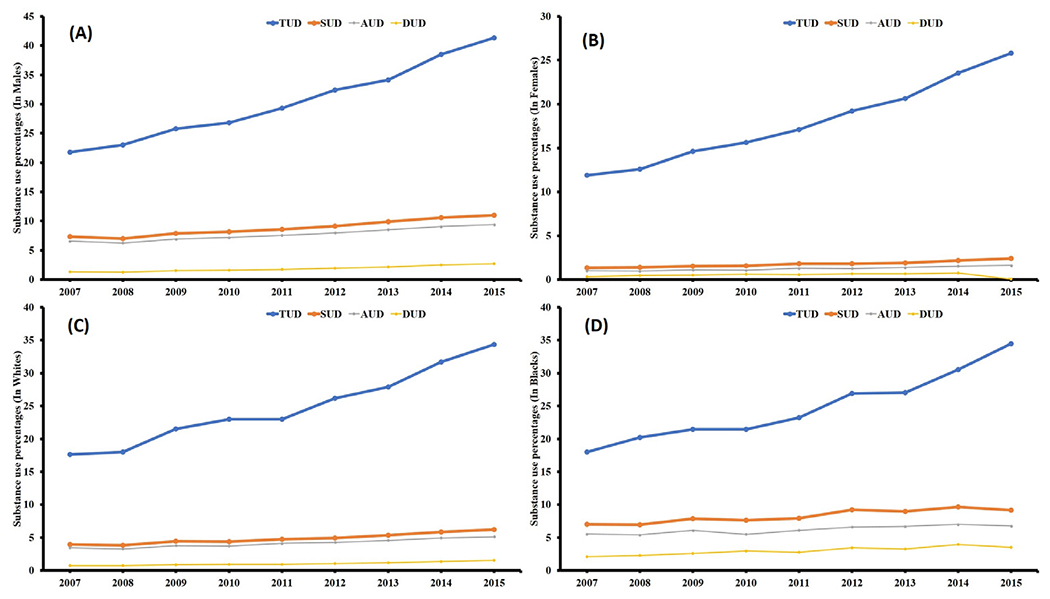
Trend plots for TUD, SUD, AUD and DUD stratified based on gender and race.
Panel A represents temporal trends in males and Panel B represented temporal trends in females. Panel C represents temporal trends in white race and Panel D represents temporal trends in black race. X-axis represents timeline in years, and Y-axis represents frequency of substance use disorder in percentages.
Abbreviations: TUD: Tobacco Use Disorder; SUD: Substance Use Disorder; AUD: Alcohol Use Disorder; and DUD: Drug Use Disorder.
Fig. 3.
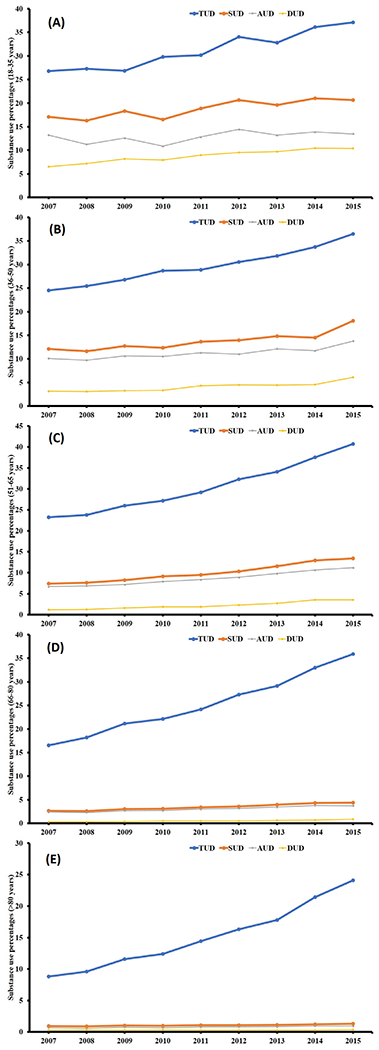
Trend plots for TUD, SUD, AUD and DUD stratified based on age groups.
(Panel A is for 18–35 years, Panel B is for 36–50 years, Panel C is for 51–65 years, Panel D is for 66–80 and Panel E is for >80 years). X-axis represents timeline in years and Y-axis represents frequency of substance use disorder.
Abbreviations: TUD: Tobacco Use Disorder; SUD: Substance Use Disorder; AUD: Alcohol Use Disorder; and DUD: Drug Use Disorder.
Discussion
This current nationwide research of ~3.6 million hospitalizations for AF from 2007 to 2015 demonstrated the rates and temporal trends of AF hospitalizations with TUD, AUD, DUD, or SUD. Of ~3.6 million hospitalizations with AF, 23.46% had TUD, which was the most commonly associated disorder followed by 5.1% had SUD, 4.3% had AUD, and 1.2% had DUD. Among AF hospitalizations, the prevalence of TUD, SUD, AUD, and DUD was substantially up trended across all age groups, races, and gender during the study period. The younger age group (18–35 years), male, and lower socioeconomic status were associated with increased risk of both TUD and SUDs. Patients with private insurance were associated with lower odds of all types of substance abuse compared with Medicare/Medicaid. All AF hospitalizations were more likely to be admitted to urban teaching hospitals. While white race and Midwest regional hospitals were associated with increased risk of TUD, the black race, and west regional hospitals were associated with higher rates of SUD, AUD, and DUD in AF hospitalizations.
Several former studies showed an association between tobacco and the incidence of AF.4, 8, 23 This study showed an increasing trend of TUD among hospitalization with AF, consistent with the most recent report by Wang et al.14 Several mechanisms may explain an association between smoking and AF. Nicotine has sympathomimetic activity leading to tachycardia and elevated blood pressure from catecholamine release.24 Nicotine also has a profibrotic response leading to atrial structural and electric remodeling in the animal study.25 All these point towards a causal pathway between tobacco and AF as evidenced in the former literature depicting the role of nicotine in atrial fibrosis leading to AF.26 Few small studies showed that alcohol and opioid use are independently associated with AF.6, 12, 27, 28 Literature showed an increasing trend of alcohol use from 2000 to 201615, opioid use disorder, opioid overdose from 2006 to 2016,29 and increasing trend of AF among opioid overdose hospitalizations from 2005 to 2015, consistent with our results.28 Three large observational studies documented a dose-dependent relationship between alcohol consumption and the risk of AF.30–32 Furthermore, as explained above, cessation of alcohol was associated with reduction in the trends of AF in a previous study.10 Several mechanism have also been proposed for a strong association between alcohol and AF which may include, but not limited to sympathetic activation, direct myocardial injury and inflammation, and increasing oxidative stress.9 Alcohol also has indirect effects such as increasing blood pressure, causing obstructive sleep apnea and left ventricular cardiomyopathy which can eventually lead to AF.9 Additionally, substance abuse has been strongly associated with heart failure which can eventually lead to AF.16, 33
In the general population, TUD and SUDs are continually on the rise without discriminating against age. Across the age strata, young adults were more predilected towards the TUD and SUDs, as shown in this study. Among the young adults, depression, peer pressure, desire to be among the ‘cool’, whereas, among old adults, psychiatric illness, stress, social factors like divorce, life events, and prescription medications misuse could be the contributing factors towards abuse.34 The TUD and SUD would have a different magnitude of impact among the younger as compared with older patients with AF hospitalization due to differences in the prevalence of comorbidities. Among the AF hospitalizations, the TUD and SUDs had a high prevalence of male that goes with a similar trend of TUD and SUD in the general population.35 Noticeably, the up-trend in the male was steeper as compared to the female in this study. The difference in trend and prevalence by gender could be explained by the neurobiological mechanism.36
This study reported that white and black were associated with an increased risk of TUD and SUDs, respectively. A national survey reported the maximum prevalence of TUD and DUD among the American Indians and whites.35 However, the authors categorized the race by white, black, and others. There is no substantial research revealing the disparity by race in the past. However, certain factors such as multiple peers, family (poor parenting), school (location), community domain (neighborhood deterioration), culture-specific risk (greater acculturation), protective correlates (cultural pride) might influence the difference.37 In the general population, AUD was more prevalent among the higher socioeconomic status (SES), but TUD and DUD were more prevalent among lower SES.38 Among AF hospitalizations, our study showed that the prevalence of TUD and SUDs was higher for patients with lower socioeconomic status as represented by payor status (Medicaid/Medicare, self-pay, or no other charge) and median household income quartiles. These are consistent with the results of previous studies.39, 40 This result can be attributed to the possible “downward drift” of substance users into disadvantaged neighborhood overtime.41 This could also explain the higher odds of TUD, SUD, AUD, and DUD reported among hospitalizations, where the primary payor was Medicare/Medicaid. The results in the study were not adjusted for other complex community factors predisposing to TUD or SUD. Geographically, the Midwest, west region stood out for high rates of TUD and SUD among AF hospitalizations, which mirror the data from NSDUH reporting a high prevalence of illicit drug use by individuals 18 years or older in the west region.35
TUD and SUD in the AF hospitalizations have broader implications on the healthcare system. The REGARDS study demonstrated that environmental tobacco smoke exposure is associated with a higher prevalence of AF,42 and childhood second-hand smoke exposure predicts the increased risk for adulthood AF.43 The Rotterdam Study reported a similar risk of AF in former smokers as it is current smokers.8 In general, substance use leads to increased costs from decreased productivity, healthcare expenditure, and crime.44 SUDs have a lasting impact on social, economic, health, and legal consequences. Screening for TUD and SUDs is inadequate in primary care, emergency room, and hospital settings for a long time.45 Considering the effect of tobacco, alcohol, and drugs (cocaine, opioids, marijuana, amphetamine, and others) on AF and its rising trend among AF hospitalizations across the age, gender, and race demands for the development of preventive strategies to address multilevel influences. Additional education must be provided to the patients during clinic visit or hospital admission to explain the preventable behavioral risk factor, which may be contributing to their AF risk.
The limitations of this study are as following: The NIS database is prone to inherent miscoding among diagnoses and procedural codes. However, the authors used authenticated codes from literature laid out by HCUP/AHRQ to recognize the ICD-9-CM codes for diagnosis or procedure. Occasionally, patients with recent history of tobacco or substance use but presently under abstinence may not be coded as TUD and SUDs that might have led to under-coding of conditions. The authors could not quantify the amount and duration of tobacco, alcohol, or illicit substance use disorder due to the nature of the NIS dataset where such information is unavailable. However, these codes have been utilized previously.16 The unmeasured factors related to lifestyle or cardiovascular risk factors not measured may influence some of these associations, primarily as related to socioeconomic status or race. This study is only focused on hospitalized AF and did not include any patients who were diagnosed in the clinic, given the nature of the database. This affects the actual rates of substance abuse. The frequency for opioid abuse, amphetamine abuse and other drug abuse was low and hence, were not reported in this study. We have not adjusted out trend analysis with demographics. Finally, one hospitalization can have more than one substance abuse which was not accounted for in this study given the complex nature of the combinations. However, the NIS is a large and nationally representative database that allows us to generalize findings and utilize it as a reference tool for potential implications on healthcare policy.
In nationally representative data, despite these limitations, the authors highlighted the rising trend of the TUD, AUD, DUD and SUD among hospitalized AF patients. To our knowledge, this is the most extensive study of its kind that reveals that TUD and SUD among AF hospitalizations in the U.S. affects more males, younger individuals, white individuals, and those of lower socioeconomic status. An AF hospitalization is an opportunity to screen for and treat TUD, AUD or SUD. Further research on the prevalence of TUD and SUD, its impact on outcomes such as readmission, mortality, and the intervention that reduces rates of TUD or SUD among discharged AF are imminent.
Supplementary Material
Funding Source
Dr. Saraschandra Vallabhajosyula is supported by the Clinical and Translational ScienceAward (CTSA) Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Abbreviations and Acronyms:
- AF
Atrial Fibrillation
- AUD
Alcohol Use Disorder
- DUD
Drug Use Disorder
- FHS
Framingham Heart Study
- HCUP
Healthcare Cost and Utilization Project
- ICD-9-CM
International classification of disease, Ninth Revision, Clinical Modification
- NIS
National Inpatient Sample
- SUD
Substance Use Disorder
- TUD
Tobacco Use Disorder
- US
United States
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.hrtlng.2020.12.009.
References
- 1.Patel NJ, Deshmukh A, Pant S, et al. Contemporary trends of hospitalization for atrial fibrillation in the United States, 2000 through 2010: implications for healthcare planning. Circulation. 2014;129(23):2371–2379. [DOI] [PubMed] [Google Scholar]
- 2.Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114(2):119–125. [DOI] [PubMed] [Google Scholar]
- 3.Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271(11):840–844. [PubMed] [Google Scholar]
- 4.Chamberlain AM, Agarwal SK, Folsom AR, et al. Smoking and incidence of atrial fibrillation: results from the Atherosclerosis Risk in Communities (ARIC) study. Heart Rhythm. 2011;8(8):1160–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Samokhvalov AV, Irving HM, Rehm J. Alcohol consumption as a risk factor for atrial fibrillation: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil. 2010;17(6):706–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krishnamoorthy S, Lip GY, Lane DA. Alcohol and illicit drug use as precipitants of atrial fibrillation in young adults: a case series and literature review. Am J Med. 2009;122(9). 851–856 e3. [DOI] [PubMed] [Google Scholar]
- 7.Schnabel RB, Sullivan LM, Levy D, et al. Development of a risk score for atrial fibrillation (Framingham Heart Study): a community-based cohort study. Lancet. 2009;373(9665):739–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heeringa J, Kors JA, Hofman A, van Rooij FJ, Witteman JC. Cigarette smoking and risk of atrial fibrillation: the Rotterdam Study. Am Heart J. 2008;156(6):1163–1169. [DOI] [PubMed] [Google Scholar]
- 9.Voskoboinik A, Prabhu S, Ling LH, Kalman JM, Kistler PM. Alcohol and atrial fibrillation: a sobering review. J Am Coll Cardiol. 2016;68(23):2567–2576. [DOI] [PubMed] [Google Scholar]
- 10.Voskoboinik A, Kalman JM, De Silva A, et al. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med. 2020;382(1):20–28. [DOI] [PubMed] [Google Scholar]
- 11.Huang MC, Yang SY, Lin SK, et al. Risk of cardiovascular diseases and stroke events in methamphetamine users: a 10-Year Follow-Up Study. J Clin Psychiatry. 2016;77 (10):1396–1403. [DOI] [PubMed] [Google Scholar]
- 12.Doshi R, Majmundar M, Kansara T, et al. Frequency of cardiovascular events and in-hospital mortality with opioid overdose hospitalizations. Am J Cardiol. 2019;124(10):1528–1533. [DOI] [PubMed] [Google Scholar]
- 13.Mack KA, Jones CM, Ballesteros MF. Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan areas-United States. Am J Transplant. 2017;17(12):3241–3252. [DOI] [PubMed] [Google Scholar]
- 14.Wang TW, Gentzke AS, Creamer MR, et al. Tobacco product use and associated factors among middle and high school students - United States, 2019. MMWR Surveill Summ. 2019;68(12):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grucza RA, Sher KJ, Kerr WC, et al. Trends in adult alcohol use and binge drinking in the early 21st-Century United States: a meta-analysis of 6 national survey series. Alcohol Clin Exp Res. 2018;42(10):1939–1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Snow SC, Fonarow GC, Ladapo JA, Washington DL, Hoggatt KJ, Ziaeian B. National rate of tobacco and substance use disorders among hospitalized heart failure patients. Am J Med. 2019;132(4). 478–488 e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thakkar S, Majmundar M, Kumar A, et al. Comparison of management and outcomes of acute heart failure hospitalization in medicaid beneficiaries versus privately insured individuals. Am J Cardiol. 2020;125(7):1063–1068. [DOI] [PubMed] [Google Scholar]
- 18.Khera R, Cram P, Lu X, et al. Trends in the use of percutaneous ventricular assist devices: analysis of national inpatient sample data, 2007 through 2012. JAMA Intern Med.2015;175(6):941–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah J, Kumar A, Majmundar M, et al. Prevalence of cardiovascular risk factors and financial burden in younger adults hospitalized with atrial fibrillation. Heart Lung. 2020. [DOI] [PubMed] [Google Scholar]
- 20.Doshi R, Al-Khafaji JF, Dave M, et al. Comparison of baseline characteristics and in-hospital outcomes in medicaid versus private insurance hospitalizations for atrial fibrillation. Am J Cardiol. 2019;123(5):776–781. [DOI] [PubMed] [Google Scholar]
- 21.Doshi R, Pisipati S, Taha M, et al. Incidence, 30-day readmission rates and predictors of readmission after new onset atrial fibrillation who underwent transcatheter aortic valve replacement. Heart Lung. 2020;49(2):186–192. [DOI] [PubMed] [Google Scholar]
- 22.Khera R, Angraal S, Couch T, et al. Adherence to methodological standards in research using the national inpatient sample. JAMA. 2017;318(20):2011–2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Staerk L, Sherer JA, Ko D, Benjamin EJ, Helm RH. Atrial fibrillation: epidemiology, pathophysiology, and clinical outcomes. Circ Res. 2017;120(9):1501–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haass M, Kubler W. Nicotine and sympathetic neurotransmission. Cardiovasc Drugs Ther. 1997;10(6):657–665. [DOI] [PubMed] [Google Scholar]
- 25.Shan H, Zhang Y, Lu Y, et al. Downregulation of miR-133 and miR-590 contributes to nicotine-induced atrial remodelling in canines. Cardiovasc Res. 2009;83(3):465–472. [DOI] [PubMed] [Google Scholar]
- 26.Goette A. Nicotine, atrial fibrosis, and atrial fibrillation: do microRNAs help to clear the smoke? Cardiovasc Res. 2009;83(3):421–422. [DOI] [PubMed] [Google Scholar]
- 27.Qureshi WT, O’Neal WT, Khodneva Y, et al. Association between opioid use and atrial fibrillation: the reasons for geographic and racial differences in stroke (REGARDS) study. JAMA Intern Med. 2015;175(6):1058–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Doshi R, Shah J, Desai R, Gullapalli N. Burden of arrhythmia in hospitalizations with opioid overdose. Int J Cardiol. 2019;286:73–75. [DOI] [PubMed] [Google Scholar]
- 29.Wei YJ, Chen C, Fillingim R, Schmidt SO, Winterstein AG. Trends in prescription opioid use and dose trajectories before opioid use disorder or overdose in US adults from 2006 to 2016: a cross-sectional study. PLoS Med. 2019;16:(11)e1002941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ruigomez A, Johansson S, Wallander MA, Rodriguez LA. Incidence of chronic atrial fibrillation in general practice and its treatment pattern. J Clin Epidemiol. 2002;55(4):358–363. [DOI] [PubMed] [Google Scholar]
- 31.Djousse L, Levy D, Benjamin EJ, et al. Long-term alcohol consumption and the risk of atrial fibrillation in the Framingham Study. Am J Cardiol. 2004;93(6):710–713. [DOI] [PubMed] [Google Scholar]
- 32.Krahn AD, Manfreda J, Tate RB, Mathewson FA, Cuddy TE. The natural history of atrial fibrillation: incidence, risk factors, and prognosis in the Manitoba Follow-Up Study. Am J Med. 1995;98(5):476–484. [DOI] [PubMed] [Google Scholar]
- 33.Nishimura M, Bhatia H, Ma J, et al. The impact of substance abuse on heart failure hospitalizations. Am J Med. 2020;133(2). 207–213 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kuerbis A, Sacco P, Blazer DG, Moore AA. Substance abuse among older adults. Clin Geriatr Med. 2014;30(3):629–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Results from the 2017 National Survery on Drug Use and Health: Detailed Tables https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDetailedTabs2017.pdf Accessed on June 1, 2020.
- 36.Becker JB, Hu M. Sex differences in drug abuse. Front Neuroendocrinol. 2008;29(1):36–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu LT, Woody GE, Yang C, Pan JJ, Blazer DG. Racial/ethnic variations in substance-related disorders among adolescents in the United States. Arch Gen Psychiatry. 2011;68(11):1176–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Patrick ME, Wightman P, Schoeni RF, Schulenberg JE. Socioeconomic status and substance use among young adults: a comparison across constructs and drugs. J Stud Alcohol Drugs. 2012;73(5):772–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Galea S, Ahern J, Tracy M, Vlahov D. Neighborhood income and income distribution and the use of cigarettes, alcohol, and marijuana. Am J Prev Med. 2007;32(6 Suppl):S195–S202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Karriker-Jaffe KJ. Neighborhood socioeconomic status and substance use by U.S. adults. Drug Alcohol Depend. 2013;133(1):212–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buu A, Mansour M, Wang J, Refior SK, Fitzgerald HE, Zucker RA. Alcoholism effects on social migration and neighborhood effects on alcoholism over the course of 12 years. Alcohol Clin Exp Res. 2007;31(9):1545–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O’Neal WT, Qureshi WT, Judd SE, et al. Environmental Tobacco Smoke and Atrial Fibrillation: the REasons for Geographic And Racial Differences in Stroke (REGARDS) Study. J Occup Environ Med. 2015;57(11):1154–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Groh CA, Vittinghoff E, Benjamin EJ, Dupuis J, Marcus GM. Childhood tobacco smoke exposure and risk of atrial fibrillation in adulthood. J Am Coll Cardiol. 2019;74(13):1658–1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the U.S., 2006. Am J Prev Med. 2011;41(5):516–524. [DOI] [PubMed] [Google Scholar]
- 45.Pilowsky DJ, Wu LT. Screening for alcohol and drug use disorders among adults in primary care: a review. Subst Abuse Rehabil. 2012;3(1):25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


