Abstract
Background: Patients with major burns lose the normal thermoregulatory function of their skin. They exhibit profound changes in metabolism which aim to compensate for the heat loss associated with water loss through burnt skin. Although these changes in physiology are well documented, the optimal methods for temperature management in both the Operating Theatre and Intensive Care Unit are less clear. Methods: We distributed a survey consisting of 19 questions to all burn units and centres in the United Kingdom with the aim of ascertaining perception of both hypo and hyperthermia, as well as methods used to manage both of these scenarios. Results: In the Operating Theatre, most respondents stated that they measured core temperature (82%); either alone (33%) or in conjunction with peripheral temperature (49%). In the Intensive Care Unit, most respondents measured both core and peripheral temperature (67%), with only a small minority not measuring core temperature (13%). Taking into consideration all professional groups, patients were considered hypothermic if their body temperature was less than 36.2°C (+/-0.7°C). On average, a patient was considered hyperthermic if their body temperature was above 38.8°C (+/-0.6°C). Conclusion: Differences in perception between the professional groups surveyed did not reach clinical or statistical significance. In both the Operating Theatre and Intensive Care Unit, hypothermia was most often managed by increasing the ambient room temperature whereas hyperthermia was most often managed by giving paracetamol. As far as we are aware, this is the first study of the management of altered thermoregulation in major burn patients in the United Kingdom.
Keywords: Major burns, hypothermia, hyperthermia, hypermetabolism, temperature management
Introduction
Patients who have sustained major burns (more than 30% of total body surface area) often present a complex problem to those managing their injuries regarding how best to control body temperature. This is due to the profound hypermetabolic state they exhibit and the loss of the thermoregulatory role of the damaged skin [1].
Following the burn injury, they are extremely prone to hypothermia in the pre-hospital environment due to the nature of presentation and the initial emergency management which may involve cooling. Those undergoing pre-hospital anesthesia are reported to be at greatest risk [2]. As with polytrauma patients, the risks associated with hypothermia in burn patients are partly due to coagulopathy from several mechanisms. These effects include altered platelet function, impaired coagulation factors (a 1°C drop in temperature is associated with a 10% drop in function) and fibrinolysis [3].
Data from a retrospective single-centre study showed an increase in mortality linked to a lower body temperature at admission from 5% mortality in normothermic burn patients to 38% mortality in severely hypothermic patients (<34.5°C). There was also a significant increase in length of Intensive Care Unit (ICU) stay in patients admitted with hypothermia [4].
Within 72 hours, patients with major burns characteristically develop an inflammatory response which is characterized by hypotension, tachycardia, leukocytosis and hyperthermia (often over 40°C) [5]. The ability to regulate core body temperature is lost in these severely burned patients and leaving such high temperatures untreated is not without consequences. It will add to the hypermetabolic state as well as impacting on cellular function resulting in cell death and potentially multi-organ failure.
Wilmore et al showed that the hypermetabolic response can be attenuated by increasing the ambient temperature to a thermal neutral level of 33°C [6]. At this temperature, the energy required for water vaporization will be derived from the environment rather than from the patient. By maintaining ambient temperature between 28°C and 33°C, resting energy expenditure can be decreased from a magnitude of 2.0 to 1.4 in patients with severe burn injury. This leads to a reduction in protein and muscle catabolism and improved survival [6,7].
The practices in monitoring and management of extremes of temperature in burn patients often vary, as do the perceptions by clinicians of what should be regarded as abnormal. Additionally, there is a paucity of literature regarding thermoregulation in the burn patient [8]. A recent survey of temperature management practices carried out in burn centres in North America considered core temperature goals in the operating theatre and ICU as well as the methods used to achieve them [9].
Given the similarities between the United Kingdom (UK) and North America in terms of population profile, nature of burn injuries seen and health care provision we thought it would be useful to gauge the perception and understanding of individuals delivering care in UK burn centres.
Materials and methods
Survey
This descriptive study consisted of an internet-based, cross-sectional, anonymous survey distributed electronically to burn professionals working in the UK. The survey consisted of 19 questions grouped in four domains: professional status and affiliation, burn service population (adult/paediatric), management of patient temperature in the Operating Theatre/ICU and professionals’ perception of clinically relevant hypo and hyperthermia in burn patients. The survey utilised a range of responses including a dichotomous yes/no scale as well as categorical scales. Several questions allowed respondents to select more than one answer, therefore totals for these questions could sum to more than 100%.
Gaps in current knowledge were identified using a mini-Delphi technique during multidisciplinary regional burn centre meetings. After reaching agreement amongst the working group, a final version of the study protocol inclusive of survey questions was developed. A local feasibility pilot was conducted before the survey was distributed nationally.
Participants
Burn services in the UK are centralised as part of the National Health Service framework. We surveyed all 19 hospitals that care for major burn patients in the UK. Approval to distribute the survey was obtained from the Research and Development Department at University Hospitals Birmingham NHS Foundation Trust although formal ethical approval was not required for this survey based study. Approval was also obtained from the Burns Research Group within the hospital on 15th May 2019.
Inclusion criteria for the study were any staff members working in a UK Burn Centre or Burn Unit who were members of the British Burn Association. Exclusion criteria were any staff working in a UK Burn Facility; these are services which care for patients with smaller burns, usually below the resuscitation threshold, and therefore the survey about temperature management in major burns would not be applicable to them.
The survey was distributed by email via the British Burn Association (BBA) using their member mailing list. Following the first round of invitations, several burn services were identified as non-responders so a reminder was sent a month later via email. The data was collected electronically between 3rd of June 2019 and 5th of August 2019. Participation was on a voluntary basis with no incentive for completion.
Statistical analysis
Descriptive statistics were used to present data on professional affiliation, structure of burn services (adult or paediatric) and methods available for management of hypo and hyperthermia. Categorical data were analyzed using Fisher’s exact tests. The one-way analysis of variance (ANOVA) was used to determine differences between the perceptions of hypo and hyperthermia among different professional groups. A p-value of less than 0.05 was used to determine statistical significance. All statistical analyses were performed using: Survey Monkey (SurveyMonkey, SVMK Inc., San Mateo, CA, USA) and IBM SPSS Statistics for Windows, version 26 (IBMCorp., Armonk, N.Y., USA).
Results
Professional status and affiliation
In total, 74 responses were received from burn services (centres and units) in the UK. A single response pertinent to the Republic of Ireland was omitted for the purpose of the study as it fell outside the target geographical area. Respondents consisted of physicians (n = 46), registered and advanced practice burn nurses (n = 24) and other burn allied health professionals, namely physiotherapists (n = 4). The physicians identified themselves as burn surgeons (n = 19), burn anaesthetists (n = 16), and burn intensivists (n = 18), with some overlap between anaesthetists and intensivists due to dual certifications (Figure 1: Professional distribution of responders).
Figure 1.
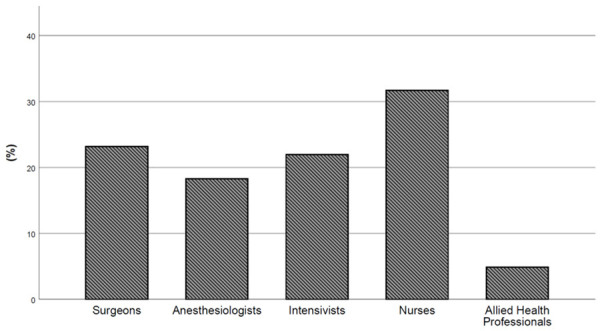
Professional distribution of responders.
Burn service population (adult or paediatric)
Forty percent of respondents worked exclusively within adult burn services, 18% within paediatric burn services and 42% within both adult and paediatric services. The majority of respondents indicated that they had access to dedicated burn operating theatres in their institution (n = 64, 85%), however, fewer respondents (n = 56, 75%) had access to a dedicated burn anaesthetic service. A similar number of respondents (n = 58, 77%) specified that they had dedicated burn ICU beds.
Temperature monitoring
Respondents were asked about their practices for temperature monitoring (core vs. peripheral) in both the operating theatre and ICU, with follow up questions exploring available methods. In theatres, most respondents indicated that they measured core temperature (82%); either alone (33%) or in conjunction with peripheral temperature (49%). A minority of respondents measured peripheral temperature alone (4%), with a significant number of respondents not sure about actual practices (14%) (Figure 2: Practice of temperature monitoring in the Operating Theatre).
Figure 2.
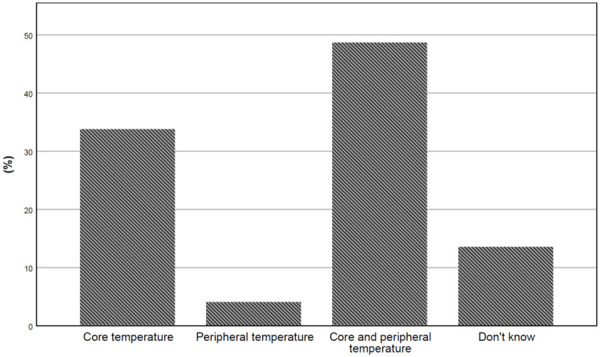
Practice of temperature monitoring in the Operating Theatre.
In the ICU, most respondents measured both core and peripheral temperature (67%), with only a small minority not utilizing core temperature measurement (13%). Some respondents stated that the actual measurement used was dependent upon the time since burn injury, with initial dual (core and peripheral) measurement used in the first 48-72 hours followed by core temperature only. Again, a small proportion of respondents stated that they were unsure about the actual practices undertaken (7%) (Figure 3: Practice of temperature monitoring in the Intensive Care Unit).
Figure 3.
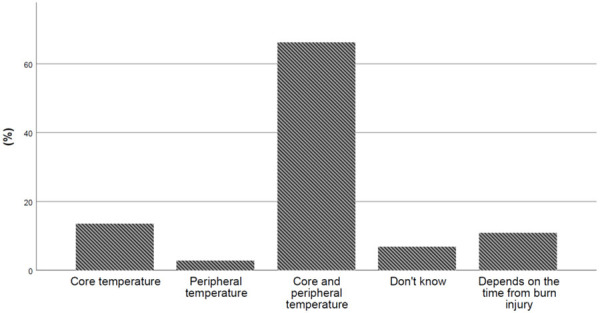
Practice of temperature monitoring in the Intensive Care Unit.
The oesophageal probe and bladder thermometer (49% and 47% respectively) were the most commonly used core temperature devices in the operating theatre followed by the tympanic and nasal probes (both 31%). Similar results were obtained in the ICU where the bladder thermometer was the most commonly used (59%), followed by the tympanic and oesophageal probes (34% and 33% respectively).
In regards to peripheral temperature monitoring, the most frequently used device was the skin probe in both the operating theatre and the ICU (49% and 74% respectively). The axillary thermometer was used by 11% of respondents in the operating theatre and 28% in the ICU. 17% of respondents did not measure peripheral temperature in the operating theatre.
Another aspect of patient care explored in the survey was the methods used to manage body temperature of patients in both the operating theatre and the ICU. The survey explored scenarios of both hypo and hyperthermia. Hypothermia was most often managed by increasing the ambient room temperature in both theatre and ICU settings (84% vs. 90% respectively). The next most common approaches were infusion of warmed intravenous fluids (78% in the operating theatre and 72% in the ICU) and forced air warming blankets. Warming blankets were more often preferred by ICU staff (88% of respondents) than by practitioners in the operating theatre (73%). Warmed mattresses were commonly used in the operating theatre (64%) whereas hemofiltration was more frequently used in the ICU (18%) (Table 1).
Table 1.
Hypothermia management strategies in the Operating Room and Intensive Care Unit (N = number of respondents, statistically significant differences: P<0.05 in bold)
| Hypothermia management methods | Operating theatre | Intensive Care Unit (ICU) | p value | ||
|---|---|---|---|---|---|
|
|
|
||||
| N | % | N | % | ||
| Increase of the ambient theatre temperature | 62 | 84% | 67 | 91% | 0.32 |
| Warmed intravenous fluids | 58 | 78% | 53 | 72% | 0.44 |
| Forced air warming blanket | 54 | 73% | 65 | 88% | 0.03 |
| Warmed mattress | 47 | 64% | 22 | 30% | <0.0001 |
| Overhead heating device | 24 | 32% | 20 | 27% | 0.59 |
| Don’t know | 12 | 16% | 5 | 7% | 0.12 |
| Warming pads | 12 | 16% | 10 | 14% | 0.82 |
| Intravascular targeted temperature management device | 10 | 14% | 7 | 10% | 0.61 |
| Other | 5 | 7% | 4 | 5% | 1.00 |
| Hemofiltration | 4 | 5% | 13 | 18% | 0.037 |
If the focus of practice was to prevent hyperthermia, different methods were used to manage body temperature depending on the location. The most common approach was to administer pharmacological treatment, typically an infusion of paracetamol (65% of respondents in the operating theatre vs. 81% in the ICU), followed closely again by a reduction in ambient room temperature (60% of respondents in the operating theatre vs. 76% in the ICU). A similar percentage of respondents in both settings used cooled intravenous fluids (36% in operating theatres and 46% in ICU). In the ICU, 56% of staff preferred to use hemofiltration as their method to manage hyperthermia. Other methods used in both theatres and ICU include non-steroidal anti-inflammatory drugs, forced air cooling blankets, bladder or gastric lavages and targeted temperature management devices (Table 2).
Table 2.
Hyperthermia management strategies in the Operating Room and Intensive Care Unit (statistically significant differences: P<0.05 in bold)
| Hyperthermia management methods | Operating Theatre | Intensive Care Unit (ICU) | p value | ||
|---|---|---|---|---|---|
|
|
|
||||
| N | % | N | % | ||
| Administration of paracetamol | 48 | 65% | 60 | 81% | 0.041 |
| Reduction of ambient room temperature | 44 | 60% | 56 | 76% | 0.055 |
| Cooled intravenous fluids | 26 | 35% | 34 | 46% | 0.2 |
| Forced air cooling blanket | 19 | 26% | 31 | 42% | <0.001 |
| Don’t know | 18 | 24% | 5 | 7% | 0.2 |
| Tepid sponging of patient | 13 | 18% | 34 | 46% | 0.2 |
| Administration of a non-steroidal anti-inflammatory | 13 | 18% | 20 | 27% | <0.001 |
| Hemofiltration | 12 | 16% | 40 | 54% | 0.006 |
| Other | 10 | 14% | 11 | 15% | 0.031 |
| Cooled nasogastric feed | 8 | 11% | 25 | 34% | 1 |
| Intravascular targeted temperature management device | 7 | 10% | 13 | 18% | <0.001 |
| Bladder lavage | 6 | 8% | 25 | 34% | 0.001 |
| Gastric lavage | 2 | 3% | 11 | 15% | 0.017 |
Perception of hypothermia and hyperthermia
Another aspect explored in the survey was the perception of both hypo and hyperthermia between different professional groups directly involved in clinical care of the burn patient. Taking into consideration all groups, patients were considered hypothermic if their body temperature was less than 36.2°C (+/-0.7°C). Difference in perceptions between the professional groups did not reach clinical or statistical significance (P = 0.65). Burn nurses’ perception of hypothermia was a body temperature below 36.0°C (+/-0.7°C). This was followed by the perception of burn surgeons and burn intensivists (below 36.2°C (+/-0.7°C)) and burn anaesthetists (below 36.3°C (+/-0.8°C)) (Figure 4: Perception of hypothermia between different professional groups (mean and 95% CI)).
Figure 4.
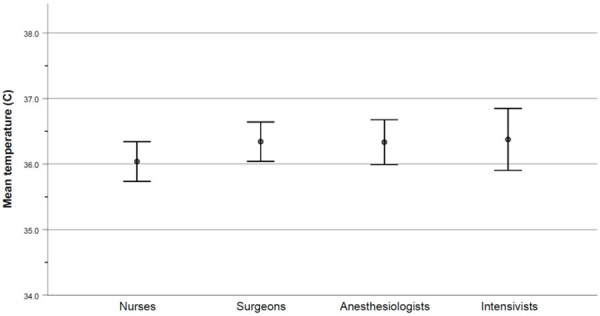
Perception of hypothermia between different professional groups (mean and 95% CI).
Interestingly, there were also no significant differences between the groups in the perception of what constituted hyperthermia. On average, a patient was considered hyperthermic if their body temperature was above 38.8°C (+/-0.6°C). Surgeons reported the lowest temperature value constituting hyperthermia, (just above 38.6°C (+/-0.5°C)), followed by nurses (38.7°C (+/-0.6°C)) and anaesthetists (38.8°C (+/-0.6°C)). As a group, intensivists reported the highest temperature as constituting hyperthermia (39.1°C (+/-0.5°C)). None of the differences reached either clinical or statistical significance (P = 0.08) (Figure 5: Perception of hyperthermia between different professional groups (mean and 95% CI)).
Figure 5.
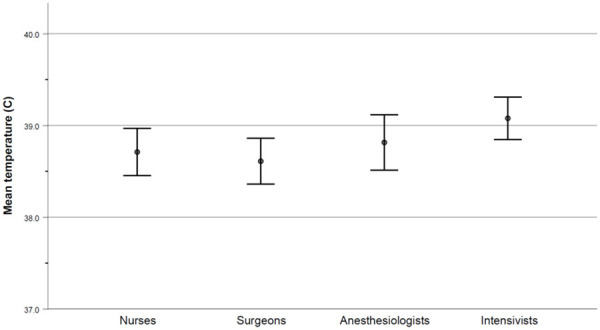
Perception of hyperthermia between different professional groups (mean and 95% CI).
Discussion
What this study adds to current literature
There has been no previous study, to our knowledge, of the management of altered thermoregulation in major burn patients in the UK. We felt it was important to carry out a national survey to establish perceptions of temperature management across different staff groups as well as the extent of consistency in practice across the surveyed area.
Current literature and guidelines regarding temperature management practices
Pruskowski and colleagues carried out a survey of temperature management practices among burn centers in North America [9]. The majority of respondents, who came mainly from a medical background, stated that they targeted core temperatures between 36 and 38°C in the Operating Room (OR). On the ICU, ambient temperatures were maintained between 75 and 95°F. They found that most respondents agreed that increasing ambient temperature benefited patients in both the OR and ICU but that this also had a negative effect on staff performance and concentration. The negative effect of increased temperature on cognitive performance [10,11] and manual dexterity [12] has also been reported in other studies. The authors of the North American study also reported concerns about the risk of staff sweating and causing contamination of a sterile field during a procedure. This concern has been studied and confirmed previously during mock total hip joint surgery performed by surgeons who were actively sweating under conditions of heat stress [13]. In addition, Pruskowski et al found that the commonest methods for maintaining core temperature in the OR and ICU were by increasing the ambient temperature, forced air devices and warmed intravenous fluids [9]. Their study did not discuss the issues of managing hyperthermia in burn patients.
There is no uniform guidance about what constitutes a ‘normal’ temperature range in the burn patient. In addition, advice regarding methods of temperature management varies, with a recent review advocating that the patient’s room temperature be set at around 18°C to reduce metabolic demand [14]. National standards produced by the British Burn Association (BBA) do not specify a particular target core temperature although they do suggest that burns of greater than 20% total body surface area (TBSA) should be cared for in a single-bedded temperature controlled cubicle [15]. The International Society for Burn Injuries (ISBI) guidelines suggest that core temperature should be maintained above 36°C [16].
Survey distribution within the UK
Burn patients in the UK are cared for within burn networks which are organized on a geographical basis. Each network contains burn facilities, units and centres which each treat patients of increasing burn size and complexity. Our survey was sent to all members of the BBA. Responses from burns facilities were excluded from this study as they treat smaller, less complex burns which would not be expected to be associated with altered thermoregulation. Data from burn centres and units were analyzed together as they both provide ICU level care for resuscitation burns. Excluding burns facilities, there are 19 burns services treating major burns in the UK. We received responses from 14 services giving a response rate of 74%. Multiple responses from each service were permitted in order to capture responses from different staff groups. We did not receive any responses from services in Scotland or from the single burn service in Northern Ireland. The responses to our survey therefore represented all burns centres and units within England and Wales.
Study limitations
There were limitations to our study. We are aware that our survey may have been affected by non-response bias. Surveys were sent to members of the BBA, who are predominantly from a medical rather than nursing background, and this may have affected the diversity of responses received. We aimed to maximize our response rate, and therefore minimize non-response bias, by discussing and advertising our survey at the annual National UK Burns Mortality Meeting, that is held in July of each year and is widely attended by staff from all burn services. A survey reminder was also sent one month after the initial invitation. The reason we received no responses from Scotland is not entirely clear. It may have been that contacting Scottish burn services via the Care of Burns in Scotland group (COBIS) would have yielded more responses.
Some multiple choice questions were answered with additional free text stating that the respondent’s answer would depend on the size of the burn. For this reason we realized, with hindsight, that our survey should have clearly specified that the questions referred to patients with major burns of greater than 30% TBSA. Similarly, there were a number of “Don’t Know” responses to several questions, which may have been because questions weren’t applicable to particular staff groups. A “Not Applicable” answer was included as an option but respondents might have felt that “Don’t Know” would capture the same information. For example, practitioners in the ICU are unlikely to be able to answer questions about temperature monitoring in the operating theatre and vice versa.
Our survey did not include an option for pre or perioperative measures used to reduce the risk of hypothermia in the operating theatre as we were focusing on management rather than prevention of these cases. However, a Canadian study has described the use of a forced air warming blanket used pre operatively to reduce the risk of intra operative hypothermia in major burns [17]. Including a question on pre operative measures used to prevent hypo or hyperthermia may have been beneficial in our survey.
Temperature management practices in our survey
Our survey found that perceptions of what constituted an abnormally high or low temperature were consistent across staff groups. Our survey was sent to a range of burn professionals and we received responses from across the multi-disciplinary burn team. Most respondents were physicians, followed by nurses, and this reflects the membership of the BBA which consists of approximately 46% physicians with a smaller number of nurses and allied health professionals including therapists.
To manage hypothermia, our survey showed that increasing ambient temperature was the most common method used in the operating theatre and ICU. This was followed by the use of forced air warming blankets and warmed intravenous fluid in keeping with the findings from Pruskowski et al. Warming blankets were possibly used less frequently in the operating theatre due to concerns over their inability to clear airborne contaminants from the surgical site [18]. They can also restrict surgical access to both the burn area and to the donor site.
To manage hyperthermia, commonly used methods included the administration of antipyretics and the reduction of ambient temperature. Hemofiltration was used in just over half of the ICUs surveyed due to its ready availability in contrast with in the operating theatre. A range of other methods were used, including cooled fluids via intravenous, nasogastric or intravesical routes but none were used consistently across the majority of services. A minority of services described the use of invasive devices for both increasing and reducing temperature but this was reported by less than 15% of respondents for both situations. This may be due to perceived concerns around the invasive nature and potential complications of intravascular devices despite previous literature reporting their use [19-21].
Conclusion
This is the first study to examine both the perceptions of altered thermoregulation in major burns and the methods used to manage both hypo and hyperthermia. Our findings are similar to a previous survey from North America but extend on those findings by also asking about management of hyperthermia. We have found that adjusting ambient temperature is the most common method of managing temperature control in major burn patients in the UK. Use of warmed intravenous fluids and forced air devices are also consistently used to maintain temperature and manage hypothermia. A range of other methods are available to manage hyperthermia but none of these are used consistently and this is likely to reflect the lack of available evidence for them. Further research is required into the various methods of temperature control that are available, especially novel or invasive techniques. In addition, controlled studies are needed to determine the optimal target temperature for the burn patient in both the operating theatre and ICU. Consideration should be given to incorporating advice on temperature management into national standards or guidelines to increase consistency between services and optimize patient management and outcome.
Acknowledgements
We would like to thank the British Burn Association for the help provided with distribution of the survey to burn centres and units within the UK. We would also like to acknowledge Alina Torlinska (University of Cardiff) for her help with statistical analysis of the data.
Disclosure of conflict of interest
None.
References
- 1.Williams FN, Herndon DN. Metabolic and endocrine considerations after burn injury. Clin Plast Surg. 2017;44:541–53. doi: 10.1016/j.cps.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 2.Lönnecker S, Schoder V. Hypothermie bei brandverletzten Patienten--Einflüsse der präklinischen Behandlung [Hypothermia in patients with burn injuries: influence of prehospital treatment] . Chirurg. 2001;72:164–167. doi: 10.1007/s001040051286. [DOI] [PubMed] [Google Scholar]
- 3.Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Filipescu D, Hunt BJ, Komadina R, Nardi G, Neugebauer EA, Ozier Y, Riddez L, Schultz A, Vincent JL, Spahn DR. The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition. Crit Care. 2016;20:100. doi: 10.1186/s13054-016-1265-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ziegler B, Kenngott T, Fischer S, Hundeshagen G, Hartmann B, Horter J, Münzberg M, Kneser U, Hirche C. Early hypothermia as risk factor in severely burned patients: a retrospective outcome study. Burns. 2019;45:1895–1900. doi: 10.1016/j.burns.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 5.Jeschke MG, Mlcak RP, Finnerty CC, Norbury WB, Gauglitz GG, Kulp GA, Herndon DN. Burn size determines the inflammatory and hypermetabolic response. Crit Care. 2007;11:R90. doi: 10.1186/cc6102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilmore DW, Mason AD Jr, Johnson DW, Pruitt BA Jr. Effect of ambient temperature on heat production and heat loss in burn patients. J Appl Physiol. 1975;38:593–597. doi: 10.1152/jappl.1975.38.4.593. [DOI] [PubMed] [Google Scholar]
- 7.Herndon DN. Mediators of metabolism. J Trauma. 1981;21:701–704. [Google Scholar]
- 8.Rizzo JA, Rowan MP, Driscoll IR, Chan RK, Chung KK. Perioperative temperature management during burn care. J Burn Care Res. 2017;38:e277–e283. doi: 10.1097/BCR.0000000000000371. [DOI] [PubMed] [Google Scholar]
- 9.Pruskowski KA, Rizzo JA, Shields BA, Chan RK, Driscoll IR, Rowan MP, Chung KK. A survey of temperature management practices among burn centers in North America. J Burn Care Res. 2018;39:612–617. doi: 10.1093/jbcr/irx034. [DOI] [PubMed] [Google Scholar]
- 10.Wyon DP, Andersen I, Lundqvist GR. The effects of moderate heat stress on mental performance. Scand J Work Environ Health. 1979;5:352–361. doi: 10.5271/sjweh.2646. [DOI] [PubMed] [Google Scholar]
- 11.Hancock PA, Vasmatzidis I. Effects of heat stress on cognitive performance: the current state of knowledge. Int J Hyperthermia. 2003;19:355–372. doi: 10.1080/0265673021000054630. [DOI] [PubMed] [Google Scholar]
- 12.Palejwala Z, Wallman K, Ward MK, Yam C, Maroni T, Parker S, Wood F. Effects of a hot ambient theatre on manual dexterity, psychological and physiological parameters in staff during a simulated burn surgery. PLoS One. 2019;14:e0222923. doi: 10.1371/journal.pone.0222923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mills SJ, Holland DJ, Hardy AE. Operative field contamination by the sweating surgeon. Aust N Z J Surg. 2000;70:837–839. doi: 10.1046/j.1440-1622.2000.01999.x. [DOI] [PubMed] [Google Scholar]
- 14.Greenhalgh DG. Management of burns. N Engl J Med. 2019;380:2349–59. doi: 10.1056/NEJMra1807442. [DOI] [PubMed] [Google Scholar]
- 15.British Burn Association. National Standards for Provisional and Outcomes in Adult and Paediatric Burn Care. https://www.britishburnassociation. org/wp-content/uploads/2018/11/BCSO-2018-FINAL-v28.pdf. Accessed 26/6/20.
- 16.ISBI Practice Guidelines Committee; Steering Subcommittee; Advisory Subcommittee. ISBI Practice guidelines for Burn Care. Burns. 2016;42:953–1021. doi: 10.1016/j.burns.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 17.Rogers AD, Saggaf M, Ziolkowski N. A quality improvement project incorporating preoperative warming to prevent perioperative hypothermia in major burns. Burns. 2018;44:1279–86. doi: 10.1016/j.burns.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 18.Dasari KB, Albrecht M, Harper M. Effect of forced-air warming on the performance of operating theatre laminar flow ventilation. Anaesthesia. 2012;67:244–249. doi: 10.1111/j.1365-2044.2011.06983.x. [DOI] [PubMed] [Google Scholar]
- 19.Corallo JP, King B, Pizano LR, Namias N, Schulman CI. Core warming of a burn patient during excision to prevent hypothermia. Burns. 2008;34:418–20. doi: 10.1016/j.burns.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 20.Prunet B, Asencio Y, Lacroix G, Bordes J, Montcriol A, D’Aranda E, Pradier JP, Dantzer E, Meaudre E, Goutorbe P, Kaiser E. Maintenance of normothermia during burn surgery with an intravascular temperature control system: a non-randomised controlled trial. Injury. 2012;43:648–652. doi: 10.1016/j.injury.2010.08.032. [DOI] [PubMed] [Google Scholar]
- 21.Davis JS, Rodriguez LI, Quintana OD, Varas R, Pizano LR, Namias N, Varon AJ, Schulman CI. Use of a warming catheter to achieve normothermia in large burns. J Burn Care Res. 2013;34:191–5. doi: 10.1097/BCR.0b013e31826c32a2. [DOI] [PubMed] [Google Scholar]


