Abstract
Objective: To explore the clinical effect of acupuncture combined with nerve block treatment on Grade I lumbar spondylolisthesis. Methods: Seventy patients with Grade I lumbar spondylolisthesis were randomly divided into a control group (n=70) treated with merely nerve block and an observation group (n=70) treated with acupuncture based on the nerve block treatment in the control group. The clinical efficacy rate, pain severity evaluated by VAS (on the 3rd day and in one week after treatment), recovery of spinal functions evaluated by Oswestry Dysfunction Index (ODI) and the quality of life reflected by the 36-Item Short Form Health Survey (SF-36) were compared between the two groups. Results: The overall efficacy rate (94.29% vs 77.14%, P=0.036) and SF-36 score of the observation group were higher than those of the control group (both P<0.05). The VAS and ODI scores of the two groups after treatment were decreased and the observation group had lower scores (all P<0.05). Conclusion: Acupuncture combined with nerve block can improve the efficacy rate of treatment of Grade I lumbar spondylolisthesis, relieve the pain of patients, restore their spinal functions and improve their quality of life, which is worthy of clinical promotion.
Keywords: Grade I lumbar spondylolisthesis, pain treatment, nerve block, acupuncture therapy, clinical effect
Introduction
Lumbar spondylolisthesis includes spondylolisthesis caused by external force and degenerative lumbar spondylolisthesis generated by degenerative diseases of the vertebra itself. Clinically, the latter one is more common. As a disease of spine, degenerative lumbar spondylolisthesis occurs generally in middle-aged and elderly groups, which is mainly caused by degenerative diseases of the lumbar intervertebral disc and the joint [1,2]. It may be associated with age, obesity, local anatomy of the spine, bad habits, living environment and lack of exercise and it is more likely to be occurred in females [3]. The clinical symptoms mainly include low back pain caused by nerve root compression resulting from spondylolisthesis, claudication, difficulty in walking, neurological dysfunction, which seriously affects the quality of life of patients. It has been reported that with the progress of aging, the incidence of lumbar spondylolisthesis is increasing year by year. Therefore, the treatment for lumbar spondylolisthesis is rather important for improvement in the quality of life of such patients [4,5].
Lumbar spondylolisthesis can be divided into Grade I-IV based on different degrees, and the severity is aggravated from I to IV. Patients with Grade I-II lumbar spondylolisthesis mostly treated with non-surgical treatment, which consists of nerve block, acupuncture, analgesic drug therapy, bone-setting therapy of Traditional Chinese Medicine (TCM) and drug therapy of TCM. Grade II and above rely on surgical treatment, but due to the high cost, long hospital stay, potential complications and other factors, patients with lumbar spondylolisthesis mostly would be treated with non-surgical treatment [6]. Previous studies have shown that local nerve root block has a good therapeutic effect on patients with lumbar spondylolisthesis, which blocks pain transmission through effective nerve block. Meanwhile, hormone injection can relieve nerve edema and provide vitamins for nerves which helps to reach a positive therapeutic effect [7]. Although lumbar spondylolisthesis is a bone disease, it can still be regarded as lumbar arthralgia and improved by dialectical treatment. Besides, TCM therapies such as acupuncture and bone-setting have good clinical effects on the treatment of orthopedic diseases, but there are few studies on the treatment of lumbar spondylolisthesis by acupuncture combined with nerve block [8]. This study applied acupuncture combined with nerve block to the treatment of lumbar spondylolisthesis and comprehensively assessed its clinical value in order to provide more research directions for improving the overall diagnosis and treatment of lumbar spondylolisthesis.
Materials and methods
General information
A total of 70 patients with lumbar spondylolisthesis admitted to our hospital from June 2019 to June 2020 were prospectively selected and randomly divided into an observation group (n=35, treated with nerve block) and a control group (n=35, treated with acupuncture combined with nerve block) according to patients’ number for hospitalization. Patients in both groups were informed of this study and signed the informed consent. This study has been approved by the Ethics Committee of our hospital.
Inclusion criteria: Patients who had lumbar spondylolisthesis diagnosed by MRI; patients who aged from 20 to 70 years old; patients who had the treatment of lumbar spondylolisthesis for the first time; patients who was diagnosed as Meyerding type I lumbar spondylolisthesis. Exclusion criteria: Patients who had heart, liver and kidney and other major organ dysfunction; patients who had other fractures; patients who had tuberculosis infection or tumors; patients who were unable to cooperate to finish this study; patients who had severe spinal deformity or osteoporosis.
Methods
After admission, patients in both groups were treated with nerve block therapy [9]. The specific procedures are as follows. Sacral block therapy was given to the patients. Be sure that there were no any other abnormal tissues around the sacrum according to the CT image. After disinfection and draping, a 9-gauge lumbar puncture needle was selected and slowly inserted into the sacral hiatus at 45° to the skin. A sense of falling would be perceived when the fibrous septum was punctured. Then, the negative pressure was drawn. After no cerebrospinal fluid or blood was found anymore, some drugs would be injected: 20 mL of 0.9% normal saline, 5 mL of 2% lidocaine (Shiyao Yinhu Pharmaceutical Co., Ltd., 5 mL/vial); 200 mg of vitamin B6, 1 mg of vitamin B12 for nerves (CR Double-crane Pharmaceutical Co., Ltd., 10 mg/vial) and 10 mg of triamcinolone acetonide to reduce edema and limit the production of inflammatory substances (Hubei Zhongshanfengxing Medical Technology Co., Ltd., 100 mg/vial). The whole therapy was conducted once a week with three times as a course. The patients in the observation group were treated with acupuncture based on the nerve block therapy of the control group [10]. Yaoyangguan, Jiaji, Weizhong, Huanqiao and Kunlun were chosen as the targeted acupoints. After routine disinfection, needles of 1-1.5 inch were taken to quickly insert into the above acupoints. During the whole process, we focused on patients’ senses and made some adjustment accordingly. The needles were remained for half an hour. The acupuncture therapy was applied once a day with ten times as a course of treatment.
Outcome measures
Main outcome measures: Visual analogue scale (VAS) was used to evaluate the pain changes before and after treatment in both groups: 0 point for no pain, 1-3 points for mild pain, 4-6 points for moderate pain, 7-9 points for severe pain, and 10 points for worst pain imaginable. Oswestr Disability Index (ODI) was applied to compare the spinal functions of patients in the two groups. It has a total score of 45 points for 9 items, 6 options for each item, with the maximum score of 5 points and the minimum score of 0 points. After accumulating scores of the 9 items, divided the sum by 45 and got the ODI scores. 0% is normal and the higher percentage represents the more severe dysfunction [11]. Clinical efficacy was evaluated: Cured indicated that the pain and lumbar discomfort were completely disappeared and the ability of daily activity was restored; significantly effective showed that the pain was relieved and the range of motion improved significantly; effective represented that the pain was relieved and functions of diseased parts were partially recovered; ineffective suggested that the pain was not relieved and diseased parts were not improved. Overall efficacy rate equaled (cured cases + significantly effective cases + effective cases)/35 × 100%.
Secondary outcome measures: The quality of life after treatment was assessed by the 36-Item Short Form Health Survey (SF-36) [12]. It consists of eight dimensions: general health, physical functioning, social functioning, role emotional, bodily pain, role physical, mental health and vitality. Except mental health score, the other scores were positively corelated with the corresponding dimensions.
Statistical analysis
SPSS 25.0 statistical software was used for analysis. Count data were expressed as n (%) and Chi-square test was conducted for comparison of count data; measurement data were expressed as (x̅ ± s); paired t test was utilized for comparison in the same group; independent t test was performed for comparison between groups. P<0.05 was considered statistically significant.
Results
Comparison of general information of patients between the two groups
The results showed that there was no significant difference in age, gender, disease course and causes between the two groups (all P>0.05) and they are comparable. See Table 1 for details.
Table 1.
Comparison of general information between the two groups (x̅ ± sd)
| Index | Observation group | Control group | t/χ2 | P |
|---|---|---|---|---|
| Age (years) | 68.2±12.3 | 69.0±11.8 | 0.278 | 0.782 |
| Gender (Male/Female) | 20/15 | 23/12 | 0.241 | 0.623 |
| Smoking history | 12 | 9 | 0.272 | 0.602 |
| Diabetes | 4 | 7 | 0.431 | 0.511 |
| Hypertension | 11 | 14 | 0.249 | 0.618 |
| Causes of disease | 0.089 | 0.765 | ||
| Osteoporosis | 27 | 29 | ||
| Injury from external force | 8 | 6 | ||
| Course of the disease (days) | 3.8±1.2 | 4.1±1.3 | 1.003 | 0.319 |
| BMI (kg.m-2) | 26.8±3.94 | 27.1±4.03 | 0.318 | 0.752 |
| Slipped parts | 0.589 | 0.963 | ||
| L4-5 | 18 | 20 | ||
| L5-S1 | 17 | 15 |
Note: BMI: body mass index.
Comparison of clinical efficacy of patients between the two groups
The results showed that in the observation group, 33 cases were effective and 2 cases were ineffective; while in the control group, 27 cases were overall effective and 8 cases were ineffective. The statistics showed that the overall efficacy rate in the observation group was higher than that in the control group (94.29% vs 77.14%, P=0.036), the difference had statistical significance. See Table 2 for details.
Table 2.
Comparison of clinical efficacy of different treatments on patients with Grade I lumbar spondylolisthesis (n, %)
| Groups | Cured | Significantly effective | effective | Ineffective | Overall efficacy rate |
|---|---|---|---|---|---|
| Observation group | 21 (60.00) | 8 (22.86) | 4 (11.43) | 2 (5.71) | 33/35 (94.29) |
| Control group | 15 (42.86) | 6 (17.14) | 6 (17.14) | 8 (22.86) | 27/35 (77.14) |
| t/χ2 | 4.375 | ||||
| P | 0.036 | ||||
Comparison of ODI scores for spinal function before and after treatment
The statistical results showed that there was no difference in ODI scores between the two groups before treatment (30.73±4.24 vs 29.39±4.92, P=0.264). After treatment, the spinal functions of patients in both groups were improved compared with those before treatment and the recovery of patients in the observation group was better than that of patients in the control group after the addition of acupuncture treatment (P<0.05). See Figure 1 for details.
Figure 1.
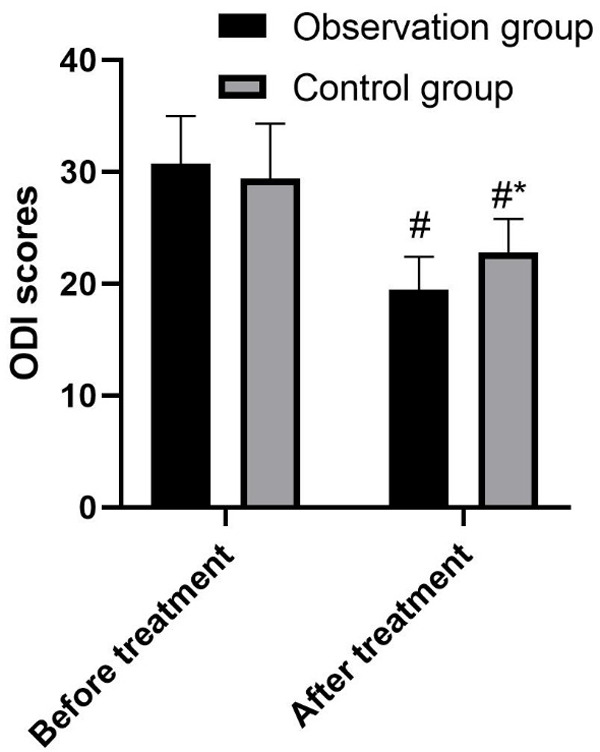
Comparison of ODI scores before and after treatment. # means comparison of ODI scores after treatment with those before treatment between the two groups, P<0.05; * indicates comparison of ODI scores in the observation group with those in the control group after treatment, P<0.05.
Comparison of VAS scores on the days 3 and 7 after treatment between the two groups
It showed that there was no statistical difference in the VAS score for preoperative pain between the two groups (9.51±1.43 vs 9.34±1.34, P=0.374). After conducting nerve block therapy, the VAS scores on the days 3 and 7 in both groups were lower than those before treatment, and the observation group had lower scores (P<0.05). See Figure 2 for details.
Figure 2.
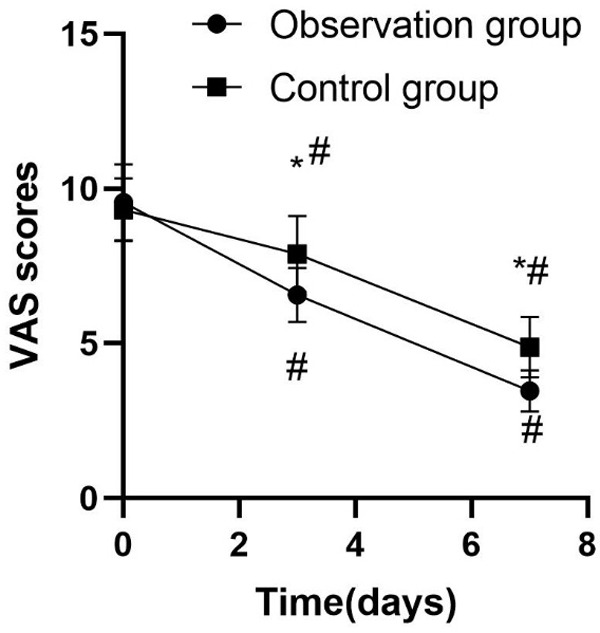
Comparison of VAS scores between two groups before and after treatment. * means comparison of VAS scores between the observation group and the control group, P<0.05; # indicates comparison of VAS scores after treatment with those before treatment at different time points, P<0.05.
Comparison of SF-36 scores before and after treatment
The results showed that after acupuncture combined with nerve block treatment, the score of mental health in the observation group was lower than that in the control group while scores of other 7 dimensions in the observation group were higher than those in the control group (all P<0.05), as shown in Table 3.
Table 3.
Comparison of SF-36 scores between the two groups after treatment (x̅ ± sd, point)
| Groups | General health | Physical functioning | Social functioning | Role emotional | Bodily pain | Role physical | Mental health | Vitality |
|---|---|---|---|---|---|---|---|---|
| Control group | 65.32±3.78 | 65.14±4.32 | 76.37±3.30 | 64.65±5.49 | 69.94±3.42 | 68.49±4.57 | 78.70±8.19 | 62.57±8.80 |
| Observation group | 78.18±3.29 | 78.43±4.18 | 82.64±3.46 | 72.59±4.75 | 81.69±4.23 | 79.47±5.29 | 71.26±7.64 | 68.53±7.39 |
| t | 15.182 | 13.221 | 7.758 | 6.471 | 12.779 | 9.292 | 3.930 | 3.068 |
| P | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.003 |
Note: SF-36: 36-Item Short Form Health Survey.
Discussion
The forward or backward slipping of a vertebral body reflected by CT images is called lumbar spondylolisthesis. Current studies suggest that lumbar spondylolisthesis is caused by chronic strain or injury from external force, which changes the normal structure of vertebral body and destroys the stability of vertebrae. The vertebral body which slipped forward and the posterior edge of adjacent pyramid form a “ladder” in shape, thus compressing the cauda equina and causing lumbar pain and nerve paralysis of lower limbs. Meanwhile, the forward movement of superior articular process of the slipped vertebral body leads to foraminal stenosis, which aggravates the nerve compression [13,14]. At present, the spondylolisthesis is divided into four degrees based on spondylolisthesis happened to four equal parts of the articular surface of the lower vertebral body. Conservative treatment is mostly taken for Grade I lumbar spondylolisthesis, including basic lumbar immobilization, exercises, and analgesic treatment with drugs, which will have local therapeutic effects on reconstructing the spine [15,16].
At present, local nerve block can reach immediate pain relief and it has become a common treatment for lumbar spondylolisthesis [17,18]. The results of this study showed that after nerve block therapy for patients with Grade I spondylolisthesis, the VAS score of patients in both groups were decreased. It may be because the drugs blocked the nerve roots and reduced the pain. In addition, vitamins and hormones can nourish nerves, reduce inflammatory substances, local nerve edema and they also have positive analgesic effect. Previous studies have reported that injection of hormones and vitamins to the nerve roots reduces nerve edema and nourishes nerves which meanwhile promotes the therapeutic effect of nerve block [19]. In this study, we found that after acupuncture treatment, the pain relief of patients with lumbar spondylolisthesis in the observation group was better than that in the control group, which may be because acupuncture relaxed spastic muscles around the diseased lumbar vertebra, reduced the chronic extrusion to nerves from soft tissues, reduced the aseptic inflammatory response caused by local nerve chemical stimulation and traction while at the same time improved the local microcirculation. It supports the previous study conclusion that acupuncture can reduce the aseptic response, local stimulation and improve the clinical treatment effect [20,21].
From the results of this study, we found that the clinical treatment effect of the observation group was better than that of the control group and so did the Oswestr dysfunction index, which may be attribute to the relief of soft tissue adhesions, contractures and scars through acupuncture, effectively reducing the internal pressure of the diseased tissue and improving the local blood circulation and lymphatic reflux. It finally facilitated the muscle reconstruction of the diseased tissue, stimulated the rehabilitation mechanism and compensatory ability of the body, promoted the recovery of lumbar function and improved the corresponding motor function. The results were similar with those of the previous studies [22,23].
The SF-36 was the most recognized method for evaluating the quality of life of patients with lumbar spondylolisthesis after treatment. After acupuncture treatment, the spinal function of patients was recovered, and the motor ability was also regained to a certain extent. Besides, the lumbar pain was reduced, which promoted patients to participate in rehabilitation exercises to the maximum extent, thereby improving the quality of life of patients with lumbar spondylolisthesis. Our study showed that after treatment, the SF-36 scores of patients in the observation group were significantly higher than those of patients in the control group, confirming that acupuncture combined with nerve block could significantly improve the quality of life of patients with lumbar spondylolisthesis, which was consistent with the conclusions of other studies abroad [24].
However, this study has some limitations. The sample of this study is small and it is a single-centered study. More multi-centered researches with large samples are required. Meanwhile, the specific biological approach of acupuncture needs to be studied further. Besides, the complications of acupuncture treatment should also be explored for comprehensive study on its clinical effect.
In summary, acupuncture combined with nerve block treatment can relieve pain, help to recover the spinal functions, and improve the quality of life of patients with lumbar spondylolisthesis. It is worthy of clinical application and promotion.
Disclosure of conflict of interest
None.
References
- 1.Pinter ZW, Kolz JM, Elder BD, Sebastian AS. Is reduction and fusion required for high-grade spondylolisthesis? Clin Spine Surg. 2020 doi: 10.1097/BSD.0000000000001029. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Alvi MA, Sebai A, Yolcu Y, Wahood W, Elder BD, Kaufmann T, Bydon M. Assessing the differences in measurement of degree of spondylolisthesis between supine MRI and erect X-ray: an institutional analysis of 255 cases. Oper Neurosurg (Hagerstown) 2020;18:438–443. doi: 10.1093/ons/opz180. [DOI] [PubMed] [Google Scholar]
- 3.Duan PG, Mummaneni PV, Guinn JMV, Rivera J, Berven SH, Chou D. Is the Goutallier grade of multifidus fat infiltration associated with adjacent-segment degeneration after lumbar spinal fusion? J Neurosurg Spine. 2020:1–6. doi: 10.3171/2020.6.SPINE20238. [DOI] [PubMed] [Google Scholar]
- 4.Aoki Y, Takahashi H, Nakajima A, Kubota G, Watanabe A, Nakajima T, Eguchi Y, Orita S, Fukuchi H, Yanagawa N, Nakagawa K, Ohtori S. Prevalence of lumbar spondylolysis and spondylolisthesis in patients with degenerative spinal disease. Sci Rep. 2020;10:6739. doi: 10.1038/s41598-020-63784-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sebaaly A, El Rachkidi R, Grobost P, Burnier M, Labelle H, Roussouly P. L5 incidence: an important parameter for spinopelvic balance evaluation in high-grade spondylolisthesis. Spine J. 2018;18:1417–1423. doi: 10.1016/j.spinee.2018.01.014. [DOI] [PubMed] [Google Scholar]
- 6.Bydon M, Alvi MA, Goyal A. Degenerative lumbar spondylolisthesis: definition, natural history, conservative management, and surgical treatment. Neurosurg Clin N Am. 2019;30:299–304. doi: 10.1016/j.nec.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Du JP, Fan Y, Liu JJ, Zhang JN, Chang Liu S, Hao D. Application of gelatin sponge impregnated with a mixture of 3 drugs to intraoperative nerve root block combined with robot-assisted minimally invasive transforaminal lumbar interbody fusion surgery in the treatment of adult degenerative scoliosis: a clinical observation including 96 patients. World Neurosurg. 2017;108:791–797. doi: 10.1016/j.wneu.2017.09.075. [DOI] [PubMed] [Google Scholar]
- 8.Sun K, Liang L, Yin H, Yu J, Feng M, Zhan J, Jin Z, Yin X, Wei X, Zhu L. Manipulation for treatment of degenerative lumbar spondylolisthesis: a protocol of systematic review and meta-analysis. Medicine (Baltimore) 2019;98:e18135. doi: 10.1097/MD.0000000000018135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Takami M, Nagatal K, Yamada H. Microendoscopic surgery with an ultrasonic bone curette for a patient with intraforaminal stenosis of the lumbar spine due to an ossification lesion: a technical case report. J Orthop Case Rep. 2018;8:57–60. doi: 10.13107/jocr.2250-0685.998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yuan S, Huang C, Xu Y, Chen D, Chen L. Acupuncture for lumbar disc herniation: protocol for a systematic review and meta-analysis. Medicine (Baltimore) 2020;99:e19117. doi: 10.1097/MD.0000000000019117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin CT, Yaszemski AK, Ledonio CGT, Barrack TC, Polly DW Jr. Oswestry disability index: is telephone administration valid? Iowa Orthop J. 2019;39:92–94. [PMC free article] [PubMed] [Google Scholar]
- 12.Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016;4:2050312116671725. doi: 10.1177/2050312116671725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of guidelines for the treatment of lumbar spondylolisthesis. Neurosurg Clin N Am. 2019;30:353–364. doi: 10.1016/j.nec.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 14.Caelers IJMH, Rijkers K, van Hemert WLW, de Bie RA, van Santbrink H. Lumbar spondylolisthesis; common, but surgery is rarely needed. Ned Tijdschr Geneeskd. 2019;163:D3769. [PubMed] [Google Scholar]
- 15.Gagnet P, Kern K, Andrews K, Elgafy H, Ebraheim N. Spondylolysis and spondylolisthesis: a review of the literature. J Orthop. 2018;15:404–407. doi: 10.1016/j.jor.2018.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.M L V SK, Sharma D, Menon J. Prognostic importance of spinopelvic parameters in the assessment of conservative treatment in patients with spondylolisthesis. Asian Spine J. 2018;12:277–284. doi: 10.4184/asj.2018.12.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Canturk M. Ultrasound-guided bilateral lumbar erector spinae plane block for postoperative analgesia after spondylolisthesis correction surgery. J Clin Anesth. 2019;57:77–78. doi: 10.1016/j.jclinane.2019.03.015. [DOI] [PubMed] [Google Scholar]
- 18.Takeuchi M, Chikawa T, Hibino N, Takahashi Y, Yamasaki Y, Momota K, Henmi T, Maeda T, Sairyo K. An elite triathlete with high-grade isthmic spondylolisthesis treated by lumbar decompression surgery without fusion. NMC Case Rep J. 2020;7:167–171. doi: 10.2176/nmccrj.cr.2019-0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greher M, Moriggl B, Peng PW, Minella CE, Zacchino M, Eichenberger U. Ultrasound-guided approach for L5 dorsal ramus block and fluoroscopic evaluation in unpreselected cadavers. Reg Anesth Pain Med. 2015;40:713–717. doi: 10.1097/AAP.0000000000000314. [DOI] [PubMed] [Google Scholar]
- 20.Lee HJ, Seo JC, Kwak MA, Park SH, Min BM, Cho MS, Shin I, Jung JY, Roh WS. Acupuncture for low back pain due to spondylolisthesis: study protocol for a randomized controlled pilot trial. Trials. 2014;15:105. doi: 10.1186/1745-6215-15-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song G, Fiocchi C, Achkar JP. Acupuncture in inflammatory bowel disease. Inflamm Bowel Dis. 2019;25:1129–1139. doi: 10.1093/ibd/izy371. [DOI] [PubMed] [Google Scholar]
- 22.Zhuang Y, Xing JJ, Li J, Zeng BY, Liang FR. History of acupuncture research. Int Rev Neurobiol. 2013;111:1–23. doi: 10.1016/B978-0-12-411545-3.00001-8. [DOI] [PubMed] [Google Scholar]
- 23.Lu L, Zhang XG, Zhong LL, Chen ZX, Li Y, Zheng GQ, Bian ZX. Acupuncture for neurogenesis in experimental ischemic stroke: a systematic review and meta-analysis. Sci Rep. 2016;6:19521. doi: 10.1038/srep19521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brinkhaus B, Roll S, Jena S, Icke K, Adam D, Binting S, Lotz F, Willich SN, Witt CM. Acupuncture in patients with allergic asthma: a randomized pragmatic trial. J Altern Complement Med. 2017;23:268–277. doi: 10.1089/acm.2016.0357. [DOI] [PubMed] [Google Scholar]


