Abstract
Background: Despite the surgical advances, obtaining the desired outcome in osteoporotic intertrochanteric femur fractures is still a tough row to hoe for the surgeons. Consequently, the interest of the researchers has shifted towards establishing a holistic approach for managing such injuries. Teriparatide, a recombinant form of human parathyroid hormone, is a novel drug that has been proved to hasten fracture healing and in both animals and humans. We attempted to evaluate the influence of Teriparatide therapy in surgically fixed osteoporotic intertrochanteric femur fractures and provide the groundwork for further research in this area. Methods: The results of osteoporotic patients who underwent only Proximal Femur Nailing [PFN] for intertrochanteric femur fractures were prospectively compared to the patients who received an additional Teriparatide therapy. We aimed to identify the effect of Teriparatide on the time to fracture union, bone mineral density [BMD], and other fracture related post-operative complications. The functional outcome was assessed using the Lower extremity functional scale [LEFS]. Results: All patients were followed up for 6 months by which time all the fractures united. However, in the Teriparatide group, time to fracture union was shortened by about 2 weeks and improvement in BMD and functional outcome were significantly better. The rate of migration of the helical, varus collapse, and femoral shortening did not show any relevant difference. Conclusion: Our preliminary attempt shows that early union coupled with better functional improvement and a substantial increase in BMD tips the balance in favour of the Teriparatide therapy in osteoporotic patients with intertrochanteric femur fractures. Well-designed clinical trials conducted in a similar vein are further required to support our claim.
Keywords: Intertrochanteric, fracture union, osteoporotic fractures, teriparatide
Introduction
The incidence of hip fractures in the geriatric population is increasing worldwide and the numbers are expected to reach approximately 6.26 million per year by 2050 [1]. The lifetime risk of sustaining a hip fracture has been reported to be as high as 5.6% for males and 20% for females at 50 years of age [2]. Trivial trauma has been the cause of these fractures in up to 53% of the population beyond 50 years of age, which increases to more than 80% of all fractures beyond 70 years of age [3].
Surgical fixation is the treatment of choice for pertrochanteric femur fractures. The stability of fixation and the success of the implant largely depend upon the bone quality and fracture comminution [4]. The incidence of implant failure and loss of reduction is significantly greater in osteoporotic patients. The subsequent evolution of the implant design is aimed at fixing the fracture and holding the fracture reduction with appropriate implant until union. However, even with the latest implant designs and surgical techniques, the problem is not fully resolved with significant failure rates [5].
There has been a recent shift towards multimodal treatment strategy targeting not only fracture fixation but also improving the overall bone quality. As a result, the pharmacological agents meant for treating osteoporosis are also being tried as adjuncts in fragility fractures to improve clinical outcome.
Teriparatide, a recombinant form of human parathyroid hormone, was approved by the Food and Drug Administration (FDA) for the treatment of patients with osteoporosis, in the year 2002 [6]. Apart from this well-established indication in osteoporosis, some research has shown its ability to hasten fracture union, improve callus volume, bone mineralization and strength in various animal trials [7]. Some promising results in animals have inspired human trials, which have also demonstrated similar results in agreement with animal model data [8-10].
We conceptualized this study to evaluate the effect of Teriparatide on the time to fracture healing in the elderly patients with osteoporotic intertrochanteric fractures. Additionally, functional outcome, improvement in bone mineral density, implant migration, and complications were also analyzed.
Material and methods
Study design
After institutional ethics committee clearance (INT/IEC/2017/1214) we conducted a prospective randomized controlled open label study, designed to learn if Teriparatide affects fracture union in osteoporotic intertrochanteric femur fractures. A written informed consent was obtained from all the participants. Best efforts were made to meet the required ethical standards [11].
Patient enrolment
This study was conducted from December 2016 to June 2017 at the Post Graduate Institute of Medical Education and Research, Chandigarh. All the patients above the age of 50 presenting to our advanced trauma centre with isolated intertrochanteric femur fracture were considered for inclusion. The surgical plan and choice of implant was not influenced by the study. We only included the patients who had established osteoporosis on DEXA scan and were planned for surgical fixation using Proximal Femoral Nailing (intramedullary nail with a single helical blade made of titanium).
Osteoporosis was defined as T Score <-2.5 at both lumbar spine and opposite hip on DEXA scan. Routine blood investigations and work up to rule out metabolic bone disease was also done. The exclusion criteria were: 1) any other associated fracture; 2) developmental anomaly of hip; 3) history of previous surgery around of the injured hip; 4) previous history of taking Teriparatide, bisphosphonates, calcitonin or any hormonal therapy for osteoporosis; 5) planned for dynamic hip screw, arthroplasty, or any other extramedullary surgical fixation; 6) unacceptable fracture reduction; 7) conditions like hypercalcemia, hyperparathyroidism, metabolic bone disease other than osteoporosis, and osteosarcoma, where Teriparatide is contraindicated; 8) unable to complete six months of follow up according to the study protocol.
The fractures were classified individually according to AO/OTA classification of fracture proximal femur. Type 31A1 fractures were considered stable while type 31A2 and 31A3 were considered unstable [12]. All the cases were operated by trained surgeons. The intraoperative quality of reduction was considered acceptable if the fracture gap was <5 mm and varus/valgus and/or anteversion/retroversion was <10°. The helical blade was considered to be adequately placed if it was central/central, inferior/central, or central/posterior in anteroposterior/lateral views.
Randomisation
A computer software generated random sequence was used to randomise the patients into two groups. In group A, patients received calcium and vitamin D supplementation postoperatively while in group B, patients received Teriparatide at a dose of 20 mcg/day subcutaneously from the first post-operative day, in addition to the standard treatment protocol. The correct method of drug administration using a pen type delivery system was taught to the patients and their caretakers. The procedure was supervised as long as the patient was admitted in the hospital and the compliance after the discharge was assessed by the history and empty refills returned during subsequent follow ups.
Follow up and rehabilitation
The patient’s physiotherapy and toe touch weight-bearing mobilization was started from the first postoperative day. After discharge, patients were followed up after two weeks for suture removal and thereafter every four weeks for a total period of six months. Partial weight-bearing was started at two weeks and full weight-bearing was allowed subsequently depending upon the appearance of cortical bridging on plain radiographs. A repeat DEXA scan for the opposite hip and lumbar spine was done at the final follow up at six months.
Radiological assessment
All patients underwent radiographic examination on the first post-operative day and then subsequently at four weekly interval till six months to assess for fracture union. Fracture union was defined as the radiological bridging of fracture site at a minimum of two cortices in two orthogonal views and clinical absence of pain or tenderness at the fracture site on bearing weight [13]. Other secondary outcome measures like the migration of the helical blade, femur neck shortening, and varus collapse were measured at three and six months of follow up. Tip apex distance was defined as the sum of the distance between the tip of the PFN blade and the apex of the femoral head after adjusting for magnification in an anteroposterior and a lateral view using Baumgaertner’s method [14]. The migration of the hip screw was assessed according to the serial changes in the tip apex distance. Varus collapse was measured by the change in neck-shaft angle, in an anteroposterior (AP) view (Figure 1). Femoral neck shortening was measured using the method given by Hélin et al [15]. A true AP view was ensured by using PFN as a reference. Malunion was defined as a varus collapse of >10°. Non-union was defined as the absence of radiological evidence of healing by 6 months.
Figure 1.
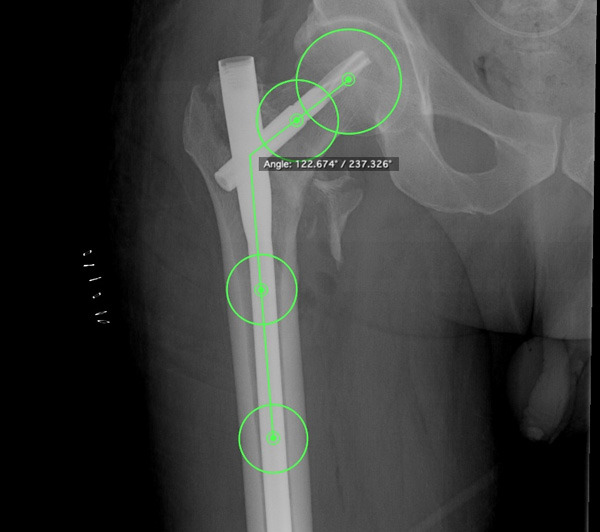
Technique used for measuring neck shaft angle. Largest fitting cricles were drawn in the head, neck, femur shaft just distal to lesser trochanter, and in the distal most part of the shaft at 100% image magnification. Centres of all the circles were joined to get the final neck shaft angle.
Clinical outcome
The functional outcome was evaluated as a secondary outcome measure using the Lower Extremity Functional Scale (LEFS) [16], a self-reported questionnaire taking into account 20 different everyday activities with a maximum score of 80. The pre trauma score was calculated by questioning the patient at the time of admission. The follow up scores were assessed using the questionnaire at three and six months. The recovery of the patient with respect to pre trauma activity level was assessed by calculating the change in depreciation of LEFS scores. This depreciation was recorded as a percentage reduction from pre trauma score, therefore a lesser depreciation indicated greater recovery. Additionally, we also recorded complications during the post-operative and follow up period.
Statistical analysis
The SPSS program for Windows, version 17.0 (SPSS, Chicago, Illinois) was used for statistical analysis. The power of the study was aimed to be 80% with a 0.05 alpha error. The effect size was taken as two weeks and the standard deviation was taken as 1.9 weeks. The minimum sample size was calculated to be 28. To account for the attrition (20%), the final sample size was decided to be 32.
Continuous variables are recorded as mean ± SD and were analysed using student T test. And Categorical variables were analyzed using either the chi-square test or Fisher’s exact test. For all statistical tests, a ‘P’ value less than 0.05 was taken to indicate a significant difference.
Results
Demographics
After applying the initial exclusion criteria, 32 osteoporotic patients were included in the study. They were randomly allocated into two groups: group A (non Teriparatide) and group B (Teriparatide). Two patients, one from each group died during the follow up and hence were excluded from the study and the final analysis included 30 patients. Both the groups were comparable in terms of age, gender, body mass index, and duration of hospital stay. The distribution of individual fracture types according to AO classification was variable in both groups; however, considering the broader subdivision of AO classification into the stable and unstable type (12), both groups were matched (Table 1).
Table 1.
Comparison of the demographic data of the study population
| PARAMETERS | GROUP A | GROUP B | P VALUE |
|---|---|---|---|
| Age at the time of surgery [years] | 74.87 ± 9.33 | 72.33 ± 9.92 | 0.477 |
| Gender | |||
| Males | 6 | 5 | |
| Females | 9 | 10 | |
| Body Mass Index [kg/m2] | 23.63 ± 3.52 | 24.98 ± 4.60 | 0.375 |
| Duration of hospital stay [days] | 13.13 ± 7.14 | 14.27 ± 7.17 | 0.334 |
| Bone Mineral Density [g/cm2] | |||
| Contralateral hip | 0.537 ± 0.073 | 0.561 ± 0.081 | 0.410 |
| Spine | 0.595 ± 0.123 | 0.650 ± 0.936 | 0.181 |
| Fracture classification | |||
| Stable [AO/OTA 31-A1.1 to 31-A2.1] | 7 | 5 | 0.456 |
| Unstable [AO/OTA 31-A2.1 to 31-A3.3] | 8 | 10 | 0.456 |
AO/OTA = AO; Foundation/Orthopaedic Trauma Association.
Radiological outcome
All 30 patients achieved fracture union. There was a significantly shorter mean healing time of 13.33 ± 1.95 weeks in group B as compared to 15.47 ± 1.41 weeks in group A (P = 0.001). By 12 weeks, only two patients (13.33%) in group A and eight patients (53.33%) in group B had achieved fracture union (P = 0.02). Subsequently, 8 patients (53.33%) in group B and 12 patients in group A (80%) attained complete fracture healing by 16 weeks (P = 0.04), and all the fractures united by the end of 20 weeks. However, the healing was noted to be faster in the Teriparatide group (Table 2).
Table 2.
Comparison of union time in the two groups
| TIME TO FRACTURE UNION | GROUP A | GROUP B | P VALUE |
|---|---|---|---|
| By 8 WEEKS | 0 | 0 | |
| By 12 WEEKS | 2 (13.33%) | 8 (53.33%) | 0.02 |
| By 16 WEEKS | 8 (53.33%) | 12 (80%) | 0.04 |
| By 20 WEEKS | 15 (100%) | 15 (100%) |
The tip apex distance and neck shaft angle were similar in both groups in the immediate post-operative period. The secondary radiographic outcome measures like the migration of the helical blade, femoral shortening, and varus collapse did not differ significantly in both the groups at 3 months. At 6 months of follow up, varus collapse at the neck was 3.04 ± 1.46° in the Teriparatide group as opposed to 4.59 ± 2.03° in the patients who did not receive Teriparatide (P = 0.01). Although statistically significant, the difference was numerically too small to make any clinical impact. Similarly, the intergroup difference in the migration of the helical blade and femoral shortening was not remarkable at the final follow up (Table 3).
Table 3.
Comparison of tip apex distance, neck shaft angle, union time, migration of helical blade, varus collapse and femoral shortening between the two groups
| PARAMETERS | GROUP A | GROUP B | P VALUE |
|---|---|---|---|
| Tip Apex Distance [mm] | 25.46 ± 5.36 | 26.29 ± 7.87 | 0.371 |
| Neck Shaft angle [degrees] | 134.85 ± 6.21 | 134.05 ± 8.91 | 0.389 |
| Union time [weeks] | 15.47 ± 1.41 | 13.33 ± 1.95 | 0.001 |
| Migration of helical blade [mm] | |||
| 3 months | 0.92 ± 0.84 | 0.82 ± 0.73 | 0.363 |
| 6 months | 1.74 ± 0.82 | 1.39 ± 1.21 | 0.232 |
| Varus collapse [degrees] | |||
| 3 months | 2.14 ± 1.01 | 1.79 ± 0.72 | 0.140 |
| 6 months | 4.59 ± 2.03 | 3.04 ± 1.46 | 0.01 |
| Femoral shortening [mm] | |||
| 3 months | 3.86 ± 3.12 | 3.61 ± 2.91 | 0.41 |
| 6 months | 6.04 ± 4.31 | 5.29 ± 4.1 | 0.31 |
The baseline BMD was matched in both the groups at both the lumbar spine and the opposite hip. The BMD at the lumbar spine increased by 7.59 ± 1.37% in the Teriparatide group as compared to 4.77 ± 1.78% in the non-Teriparatide group (P<0.05) after 6 months of follow up. Similarly, BMD at hip increased by 1.81 ± 1.39% in Teriparatide group as compared to 0.97 ± 1.14% in non-Teriparatide group (P<0.05). This increase in BMD was considerably more at the lumbar spine than hip at the final follow up (Table 4).
Table 4.
Comparison of increase in BMD in both groups at 6 months
| REGION | PRE OPERATIVE BMD [g/cm2] | Percentage change in BMD at 6 months follow up | P VALUE | ||
|---|---|---|---|---|---|
|
|
|
||||
| GROUP A | GROUP B | GROUP A | GROUP B | ||
| Hip | 0.549 ± 0.077 | 0.565 ± 0.082 | 0.97 ± 1.14% | 1.81 ± 1.39% | 0.0001 |
| Spine | 0.623 ± 0.111 | 0.652 ± 0.119 | 4.77 ± 1.78% | 7.59 ± 1.37% | 0.00001 |
BMD = Bone mineral density.
Clinical outcome
The mean pre injury LEFS was 33.73 ± 1.49 and 34.46 ± 2.90 (P = 0.377) in group A and B, respectively. After 3 months, depreciation in LEFS was 32.83 ± 1.00% in group A and 32.17 ± 1.20% in group B (P = 0.110). This difference became significant at final follow up when group A showed depreciation of 26.17 ± 1.1% compared to 24.83 ± 1.24% depreciation in group B (P = 0.04), indicating a better recovery in the Teriparatide group (Table 5).
Table 5.
Comparison of depreciation of LEFS in both groups
| MEAN PRE TRAUMA LEFS | MEAN LEFS AT 3 MONTHS | MEAN LEFS AT 6 MONTHS | PERCENTAGE DEPRECIATION FROM PRE TRAUMA SCORE | ||
|---|---|---|---|---|---|
|
| |||||
| 3 MONTHS | 6 MONTHS | ||||
| Group A | 33.73 ± 1.49 | 7.47 ± 0.88 | 12.8 ± 1.6 | 32.83 ± 1.00 | 26.17 ± 1.1 |
| Group B | 34.46 ± 2.90 | 7.73 ± 2.20 | 13.6 ± 2.85 | 32.17 ± 1.20 | 24.83 ± 1.24 |
| P-Value | 0.377 | 0.34 | 0.18 | 0.110 | 0.004 |
LEFS = Lower extremity functional scale.
No patient developed malunion, non-union, or any implant related complications. There were two cases of superficial wound infection. The wound cultures were sterile and the suture line healed with empirical antibiotics and daily dressings. One patient in the Teriparatide group developed a grade two bedsore in the sacral area which healed subsequently.
In conclusion, patients receiving additional Teriparatide therapy demonstrated earlier union, better functional outcome, and considerably greater improvement in their BMD. Although Teriparatide does not seem to alter the course of recovery in the terms of major complications like migration of the helical blade, femoral neck shortening, varus collapse, non-union, and malunion, it might increase the patient’s susceptibility to developing some minor problems.
Discussion
Hip fractures in the elderly are globally considered a major public health concern affecting not only the quality of life but also posing a major economic burden on both the families and the health care systems. Although surgical fixation has been the standard treatment in intertrochanteric femur fractures, the outcome depends upon the fracture patterns, reduction, stability, and bone quality [4]. The outcome in an adequately fixed fracture may be often compromised due to poor bone quality [4]. Lately, the research focus is shifting towards improving the overall bone structure using pharmacotherapy, and Teriparatide has shown promising results in animal and human trials [7-10]. Studies have also demonstrated a faster healing and better functional outcome associated with the use of Teriparatide in osteoporotic distal end radius and pubic fractures [8,9].
As far as the effects of Teriparatide on osteoporotic hip fractures are concerned, the present literature is contradictory. PubMed search reveals only a handful of studies of which most are retrospective, and consider “elderly patients” as osteoporotic instead of following a definitive criteria [17-25]. A few authors reported faster fracture union [17-19], while others did not find any improvement in fracture healing with Teriparatide therapy [20-22]. Han et al [23] conducted a metanalysis and concluded that Teriparatide decreases time to union in hip fractures. They however highlighted the need for well-designed studies to further substantiate the evidence. The published data on the role of Teriparatide in proximal femur fractures is detailed in Table 6.
Table 6.
A few studies in current literature pertaining to the role of Teriparatide in hip fractures
| Author | Year | Type of study | Type of fracture | Subset of patient | Surgery | Pharmacotherapy | Radiological outcome | Functional outcome | Follow up | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Group 1 | Group 2 | Group 3 | |||||||||
| Huang et al [17] | 2015 | Retrospective | Unstable intertrochanteric fracture | Elderly [>65 years] | Dynamic Hip Screw | Calcium and vitamin D | Daily subcutaneous Teriparatide (20 μg) + Calcium and vitamin D | - | Significantly faster union and reduced varus collapse, sliding of lag screw and femoral shortening in Teriparatide group [2] | Better Mobility score and hip pain score at 3 and 6 months in Teriparatide group [2] | 40.1 months |
| Huang et al [18] | 2016 | Retrospective | Stable intertrochanteric fracture | Osteoporotic patients [no definitive criteria] | Dynamic Hip Screw | Calcium and vitamin D | Daily subcutaneous Teriparatide (20 μg) + Calcium and vitamin D | On prior alendronate therapy + Daily subcutaneous Teriparatide (20 μg) + Calcium and vitamin D | Significantly faster union and decreased varus collapse, sliding of lag screw and femoral shortening in Teriparatide groups 2 and 3 | Better Mobility score and hip pain score at 3 and 6 months in group 2 and 3. Health related quality of life similar in all the groups | 12 months |
| Aspenberg et al [20] | 2016 | Prospective randomized controlled trial | Pertrochanteric fracture | Elderly [≥50 years], T score ≤2 | Sliding compression hip screw or trochanteric intramedullary nail | Daily subcutaneous Teriparatide (20 μg) + Calcium and vitamin D + oral placebo weekly | Daily subcutaneous Placebo + Calcium and vitamin D + oral risedronate weekly | - | No statistical difference in union time, loss of reduction and implant failure in both groups | TUG and VAS pain score were better but Charnley hip pain score and SF 36 was similar in Teriparatide group at 6, 12, 18 and 26 weeks | 26 weeks |
| Bhandari et al [21] | 2016 | Prospective randomized controlled trial | Femoral neck fracture | Elderly [≥50 years], T score ≤2 | Internal fixation [no definitive surgery defined] | Calcium and vitamin D | Daily subcutaneous Teriparatide (20 μg) + Calcium and vitamin D | - | No statistical difference in union time in both groups | No difference revision surgeries, pain scores, gait speed and weight bearing | 12 months |
| Chesser et al [24] | 2016 | Prospective randomized pilot study | Trochanteric fractures | Elderly [≥60 years] | Sliding hip screw and cephalomedullary nail | Calcium and vitamin D | Daily subcutaneous Teriparatide (20 μg) + Calcium and vitamin D | Defined the challenges that would present while conducting a randomized control trial | 3 months | ||
| Sierra et al [25] | 2016 | Prospective randomized controlled trial | Pertrochanteric fracture | Elderly [≥50 years], T score ≤2 | Sliding compression hip screw or trochanteric intramedullary nail | Daily subcutaneous Teriparatide (20 μg) + Calcium and vitamin D + oral placebo weekly | Daily subcutaneous Placebo + Calcium and vitamin D + oral risedronate weekly | - | No statistical difference in union time, loss of reduction and implant failure in both groups | Significant improvement of BMD at lumbar spine at 26 weeks and hip at 72 weeks in Teriparatide group | 78 weeks |
| Kim et al [22] | 2018 | Retrospective | Unstable intertrochanteric fracture | Elderly [>65 years], T score ≤2.5 | Dynamic Hip Screw | Calcium and vitamin D | Weekly subcutaneous Teriparatide (56.5 μg) + Calcium and vitamin D | - | No statistical difference in union time in both groups | No statistical difference in HHS, VAS pain score and VAS stiffness score in both groups | 6 months |
| Kim et al [19] | 2019 | Retrospective | Unstable intertrochanteric fracture | Elderly [>65 years], T score ≤2.5 | Dynamic Hip Screw | Calcium and vitamin D | Daily subcutaneous Teriparatide (20 μg) + Calcium and vitamin D | - | Significantly faster union in Teriparatide group | Better HHS, VAS pain score and VAS stiffness score at 2 and 4 months in Teriparatide group | 19 months |
| Han et al [23] | 2020 | Systematic review and meta analysis | Hip fractures | Calcium and vitamin D | Daily subcutaneous Teriparatide (20 μg) + Calcium and vitamin D | No statistical difference in union time in both groups at 3 and 6 months | No difference revision surgeries, complication and HHS | ||||
| Rana et al | Present study | Prospective randomized controlled trial | Intertrochanteric femur fractures | T score ≤2.5 | Proximal femur nail with a helical blade | Calcium and vitamin D | Daily subcutaneous Teriparatide (20 μg) + Calcium and vitamin D | Significantly faster union, decreased varus collapse in Teriparatide group at 6 months. No difference in migration of lag screw and femoral shortening in both groups | Better LEFS score and significant improvement in BMD at hip and spine at 6 months in Teriparatide group in all the groups | 6 months | |
TUG = Timed up and go test; VAS = Visual analogue scale; HHS = Harris hip score; BMD = Bone mineral density; LEFS = Lower extremity functional scale.
Chesser et al [24] recently conducted a pilot study, administering Teriparatide therapy in the trochanteric fractures in the elderly for six weeks to assess the feasibility of conducting a large scale randomised control trial. They highlighted the difficulties that would present to a researcher planning a large scale study following similar protocols. Though they did not statistically analyse their data in detail, all their fractures united within 12 weeks of surgery. Our study, looking prospectively at the effect of the Teriparatide therapy specifically in osteoporotic intertrochanteric femur fractures noticed that it reduces the time to fracture union by approximately two weeks and also improves fracture healing rate at 12 and 16 weeks.
The effects of Teriparatide are not only limited to accelerating bone healing. The new bone formed has greater density, osseous tissue volume, bone mineral content, and ultimate load to failure [7]. The pathophysiology behind this action of Teriparatide seems to be multimodal. Intermittent administration of the drug has been shown to decrease the volume and number of adipocytes in the bone marrow thereby indicating that it promotes osteoblastogenesis and reduces adipogenesis at the site of fracture healing. Moreover, no change in osteoclast density has been noted indicating that it enhances bone formation but not resorption [26].
Huang et al reported better functional outcome with the use of Teriparatide in osteoporotic pertrochanteric femur fractures at 3 months and 6 months of therapy [18]. Although Kim et al have reported conflicting results with Teriparatide therapy in two different studies [19,22], their study with a larger sample size found a significant improvement in Harris hip score and Visual analogue scale for pain as soon as two months after Teriparatide therapy [19]. In our experience we did not find any significant functional improvement at three months. However, at six months the Teriparatide group performed considerably better.
The majority of LEFS is based on the patient’s ability to mobilise [16]. The higher scores in the current study point towards better pain free mobilisation of the patient and higher activity level in the Teriparatide group. This may be attributed to faster fracture union and improved overall BMD in patients with Teriparatide therapy enabling them to bear weight earlier on the fractured limb, thereby improving the general functional status of the patient.
Previous studies have shown that Teriparatide therapy significantly improves BMD at both hip and spine after 12-24 months [27,28]. Sierra et al [25] found that daily subcutaneous administration of 20 micrograms Teriparatide improves BMD at the lumbar spine as early as six months compared to the hip, where a significant increase was reported after almost 12 months. Surprisingly, in our study, the Teriparatide group demonstrated significant improvement in BMD at both the lumbar spine and hip after six months of therapy. We suspect that this unexpected increase of BMD at the hip just after six months can be due to a possible alteration in the bone mineral deposition at the hip of osteoporotic patients with contralateral hip fracture. This may further be explained by increased loading of the contralateral hip or the effect of fracture healing process that might act as a stimulus for bone formation at distant sites. Nevertheless, we acknowledge that our sample size is very small and studies with a bigger patient cohort might produce different results.
The successful outcome after an osteoporotic intertrochanteric fracture treatment depends on the ability of the implant to hold the fracture until it unites. The poor bone quality often complicates the results in the form of varus collapse, screw migration, or excessive femoral neck shortening. As opposed to Huang et al (20), our study did not find any significant difference in medial migration of the blade and femoral neck shortening. Although varus collapse was significantly greater in the non-Teriparatide group at the end of 6 months, we believe that difference of approximately 1.5° between the two groups would hardly make any clinical impact. A few other complications like bedsore and superficial wound infection were higher in the Teriparatide group, but we believe that our sample size was too small to make any conclusions and further studies are required to investigate it better.
Teriparatide therapy significantly increases the cost of management which is an important consideration against which all the benefits of the therapy are assessed, especially in developing countries. Although a gain of approximately two weeks may not be convincing enough to use Teriparatide therapy routinely in osteoporotic per trochanteric fractures, the additional benefits in the form of greater improvement in overall BMD and functional outcome tips the balance in its favour. A significant improvement in overall bone health [26] and reduction in the incidence of new and subsequent fragility fractures [29] reported in the literature further substantiate our claims.
Despite the projected advantages, there are several limitations associated with this study that must be acknowledged. Firstly, this was a preliminary attempt with small sample size and short follow up, which makes it difficult to make any definitive conclusion regarding secondary outcomes. Secondly, our study was not blinded due to ethical considerations. Although our criteria for outcome assessment were objective, some bias might still have come into play while recording the data. Thirdly, we did not compare the outcome of Teriparatide therapy with bisphosphonates, which are cheaper alternatives for osteoporosis management. Lastly, the radiology was done at four weekly intervals so the exact time of union could not be assessed precisely.
Conclusion
Teriparatide treatment seems to expedite fracture union and improve bone mineral density in osteoporotic patients with intertrochanteric femur fractures. Although, the gain in union time is overshadowed by the cost of therapy but considering the overall improvement in functional outcome and BMD, we recommend the use of Teriparatide in osteoporotic intertrochanteric femur fractures. However, we also realise that studies with greater sample size are required to further substantiate our findings.
Disclosure of conflict of interest
None.
References
- 1.Kannus P, Parkkari J, Sievänen H, Heinonen A, Vuori I, Järvinen M. Epidemiology of hip fractures. Bone. 1996;18:S57–S63. doi: 10.1016/8756-3282(95)00381-9. [DOI] [PubMed] [Google Scholar]
- 2.Hagino H, Furukawa K, Fujiwara S, Okano T, Katagiri H, Yamamoto K, Teshima R. Recent trends in the incidence and lifetime risk of hip fracture in Tottori, Japan. Osteoporos Int. 2009;20:543–548. doi: 10.1007/s00198-008-0685-0. [DOI] [PubMed] [Google Scholar]
- 3.Bergström U, Björnstig U, Stenlund H, Jonsson H, Svensson O. Fracture mechanisms and fracture pattern in men and women aged 50 years and older: a study of a 12-year population-based injury register, Umeå, Sweden. Osteoporos Int. 2008;19:1267–1273. doi: 10.1007/s00198-007-0549-z. [DOI] [PubMed] [Google Scholar]
- 4.Saudan M, Lübbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P. Pertrochanteric fractures: is there an advantage to an intramedullary nail? A randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma. 2002;16:386–393. doi: 10.1097/00005131-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Gardner MJ, Lorich DG, Lane JM. Osteoporotic femoral neck fractures: management and current controversies. Instr Course Lect. 2004;53:427–439. [PubMed] [Google Scholar]
- 6.“Approval Letter”. https://www.Accessdata.Fda.Gov/Drugsatfda_docs/Nda/2002/21-318_FORTEO_Approv.Pdf. FDA 2002. 21-318_FORTEO_Approv.pdf.
- 7.Komatsubara S, Mori S, Mashiba T, Nonaka K, Seki A, Akiyama T, Miyamoto K, Cao Y, Manabe T, Norimatsu H. Human parathyroid hormone (1-34) accelerates the fracture healing process of woven to lamellar bone replacement and new cortical shell formation in rat femora. Bone. 2005;36:678–687. doi: 10.1016/j.bone.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Aspenberg P, Genant HK, Johansson T, Nino AJ, See K, Krohn K, García-Hernández PA, Recknor CP, Einhorn TA, Dalsky GP, Mitlak BH, Fierlinger A, Lakshmanan MC. Teriparatide for acceleration of fracture repair in humans: a prospective, randomized, double-blind study of 102 postmenopausal women with distal radial fractures. J Bone Miner Res. 2010;25:404–414. doi: 10.1359/jbmr.090731. [DOI] [PubMed] [Google Scholar]
- 9.Peichl P, Holzer LA, Maier R, Holzer G. Parathyroid hormone 1-84 accelerates fracture-healing in pubic bones of elderly osteoporotic women. J Bone Joint Surg Am. 2011;93:1583–1587. doi: 10.2106/JBJS.J.01379. [DOI] [PubMed] [Google Scholar]
- 10.Andreassen TT, Ejersted C, Oxlund H. Intermittent parathyroid hormone (1-34) treatment increases callus formation and mechanical strength of healing rat fractures. J Bone Miner Res. 1999;14:960–968. doi: 10.1359/jbmr.1999.14.6.960. [DOI] [PubMed] [Google Scholar]
- 11.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal. Basic principles and recommendations in clinical and field science research. Muscles Ligaments Tendons J. 2014;3:250–2. [PMC free article] [PubMed] [Google Scholar]
- 12.Baird RP, O’Brien P, Cruickshank D. Comparison of stable and unstable pertrochanteric femur fractures managed with 2- and 4-hole side plates. Can J Surg. 2014;57:327–30. doi: 10.1503/cjs.026113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Corrales LA, Morshed S, Bhandari M, Miclau T 3rd. Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008;90:1862–8. doi: 10.2106/JBJS.G.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–64. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Hélin M, Pelissier A, Boyer P, Delory T, Estellat C, Massin P. Does the PFNATM nail limit impaction in unstable intertrochanteric femoral fracture? A 115 case-control series. Orthop Traumatol Surg Res. 2015;101:45–49. doi: 10.1016/j.otsr.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 16.Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999;79:371–383. [PubMed] [Google Scholar]
- 17.Huang TW, Yang TY, Huang KC, Peng KT, Lee MS, Hsu RW. Effect of teriparatide on unstable pertrochanteric fractures. Biomed Res Int. 2015;2015:568390. doi: 10.1155/2015/568390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang TW, Chuang PY, Lin SJ, Lee CY, Huang KC, Shih HN, Lee MS, Hsu RW, Shen WJ. Teriparatide improves fracture healing and early functional recovery in treatment of osteoporotic intertrochanteric fractures. Medicine (Baltimore) 2016;95:e3626. doi: 10.1097/MD.0000000000003626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim SJ, Park HS, Lee DW, Lee JW. Short-term daily teriparatide improve postoperative functional outcome and fracture healing in unstable intertrochanteric fractures. Injury. 2019;50:1364–1370. doi: 10.1016/j.injury.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Aspenberg P, Malouf J, Tarantino U, García-Hernández PA, Corradini C, Overgaard S, Stepan JJ, Borris L, Lespessailles E, Frihagen F, Papavasiliou K. Effects of teriparatide compared with risedronate on recovery after pertrochanteric hip fracture: results of a randomized, active-controlled, double-blind clinical trial at 26 weeks. J Bone Joint Surg Am. 2016;98:1868–1878. doi: 10.2106/JBJS.15.01217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhandari M, Jin L, See K, Burge R, Gilchrist N, Witvrouw R, Krohn KD, Warner MR, Ahmad QI, Mitlak B. Does teriparatide improve femoral neck fracture healing: results from a randomized placebo-controlled trial. Clin Orthop Relat Res. 2016;474:1234–1244. doi: 10.1007/s11999-015-4669-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim SJ, Park HS, Lee DW, Lee JW. Does short-term weekly teriparatide improve healing in unstable intertrochanteric fractures? J Orthop Surg (Hong Kong) 2018;26:2309499018802485. doi: 10.1177/2309499018802485. [DOI] [PubMed] [Google Scholar]
- 23.Han S, Wen SM, Zhao QP, Huang H, Wang H, Cong YX, Shang K, Ke C, Zhuang Y, Zhang BF. The efficacy of teriparatide in improving fracture healing in hip fractures: a systematic review and meta-analysis. Biomed Res Int. 2020;2020:5914502. doi: 10.1155/2020/5914502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chesser TJ, Fox R, Harding K, Halliday R, Barnfield S, Willett K, Lamb S, Yau C, Javaid MK, Gray AC, Young J. The administration of intermittent parathyroid hormone affects functional recovery from trochanteric fractured neck of femur: a randomised prospective mixed method pilot study. Bone Joint J. 2016;98:840–845. doi: 10.1302/0301-620X.98B6.36794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Malouf-Sierra J, Tarantino U, García-Hernández PA, Corradini C, Overgaard S, Stepan JJ, Borris L, Lespessailles E, Frihagen F, Papavasiliou K, Petto H. Effect of teriparatide or risedronate in elderly patients with a recent pertrochanteric hip fracture: final results of a 78-week randomized clinical trial. J Bone Miner Res. 2017;32:1040–1451. doi: 10.1002/jbmr.3067. [DOI] [PubMed] [Google Scholar]
- 26.Babu S, Sandiford NA, Vrahas M. Use of teriparatide to improve fracture healing: what is the evidence? World J Orthop. 2015;6:457. doi: 10.5312/wjo.v6.i6.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eriksen EF, Keaveny TM, Gallagher ER, Krege JH. Literature review: the effects of teriparatide therapy at the hip in patients with osteoporosis. Bone. 2014;67:246–256. doi: 10.1016/j.bone.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 28.Chen P, Miller PD, Delmas PD, Misurski DA, Krege JH. Change in lumbar spine BMD and vertebral fracture risk reduction in teriparatide-treated postmenopausal women with osteoporosis. J Bone Miner Res. 2006;21:1785–1790. doi: 10.1359/jbmr.060802. [DOI] [PubMed] [Google Scholar]
- 29.Langdahl BL, Rajzbaum G, Jakob F, Karras D, Ljunggren Ö, Lems WF, Fahrleitner-Pammer A, Walsh JB, Barker C, Kutahov A, Marin F. Reduction in fracture rate and back pain and increased quality of life in postmenopausal women treated with teriparatide: 18-month data from the European Forsteo Observational Study (EFOS) Calcif Tissue Int. 2009;85:484. doi: 10.1007/s00223-009-9299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


